Effects of acetaminophen on outcomes in patients hospitalized with COVID-19
et al., Chest, doi:10.1016/j.chest.2021.07.992, Oct 2021
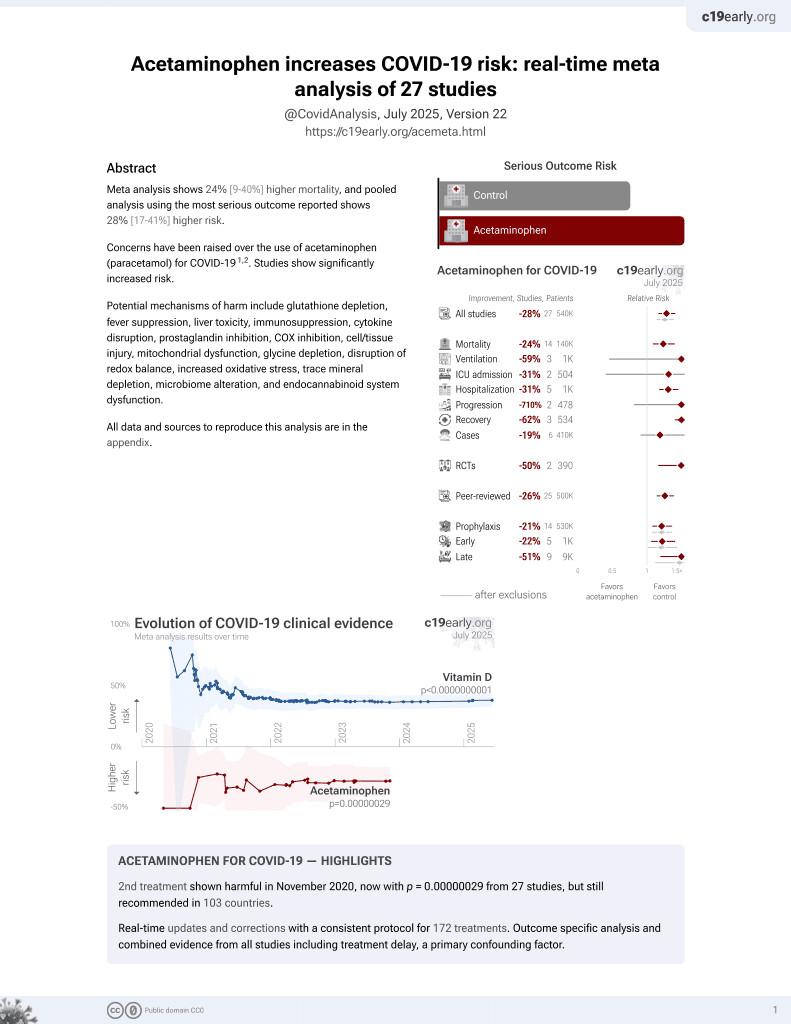
2nd treatment shown to increase risk in
November 2020, now with p = 0.00000029 from 27 studies, but still recommended in 103 countries.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 524 hospitalized patients in the USA, showing higher mortality and progression with acetaminophen use.
Acetaminophen is also known as paracetamol, Tylenol, Panadol, Calpol, Tempra, Calprofen, Doliprane, Efferalgan, Grippostad C, Dolo, Acamol, Fevadol, Crocin, and Perfalgan.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 220.5% higher, RR 3.20, p = 0.001, treatment 64 of 388 (16.5%), control 7 of 136 (5.1%).
|
|
risk of mechanical ventilation, 434.5% higher, RR 5.34, p < 0.001, treatment 388, control 136.
|
|
risk of progression, 244.0% higher, OR 3.44, p < 0.005, treatment 132, control 136, triaged to higher level of care, high exposure, RR approximated with OR.
|
|
risk of progression, 201.0% higher, OR 3.01, p < 0.007, treatment 256, control 136, triaged to higher level of care, moderate exposure, RR approximated with OR.
|
|
hospitalization time, 100% higher, relative time 2.00, p < 0.001, treatment 388, control 136.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Manjani et al., 31 Oct 2021, retrospective, USA, peer-reviewed, 6 authors, study period February 2020 - June 2020.
EFFECTS OF ACETAMINOPHEN ON OUTCOMES IN PATIENTS HOSPITALIZED WITH COVID-19
Chest, doi:10.1016/j.chest.2021.07.992
Acetaminophen acts as an antipyretic agent, inhibiting prostaglandin production in the brain. This may, in turn, lead to loss of a negative feedback loop allowing increased production of pro-inflammatory cytokines such as interleukin 6 (IL-6). Given that elevated IL-6 levels have been associated with worse outcomes in COVID-19 patients, we hypothesized that a clinical correlation exists between acetaminophen dose and outcomes in COVID-19 patients.
METHODS: We conducted a retrospective analysis of patients admitted at Washington Hospital Center between February 2020 and-June 2020. Patients older than 18 years of age, diagnosed with COVID-19 were included in the study. Those who were directly admitted to the ICU were excluded. Acetaminophen exposure was calculated using a formula for average adjusted daily acetaminophen: total acetaminophen divided by number of day's medication was administered. Groups were stratified to nonexposed and exposed. Within the exposed groups, we further divided them into moderate (100-1000 mg/day) or high exposure(>1000 mg/day). Comparison between groups for continuous variables was conducted using Kruskal Wallis test. Association between two categorical variables was tested using Fisher's exact test.
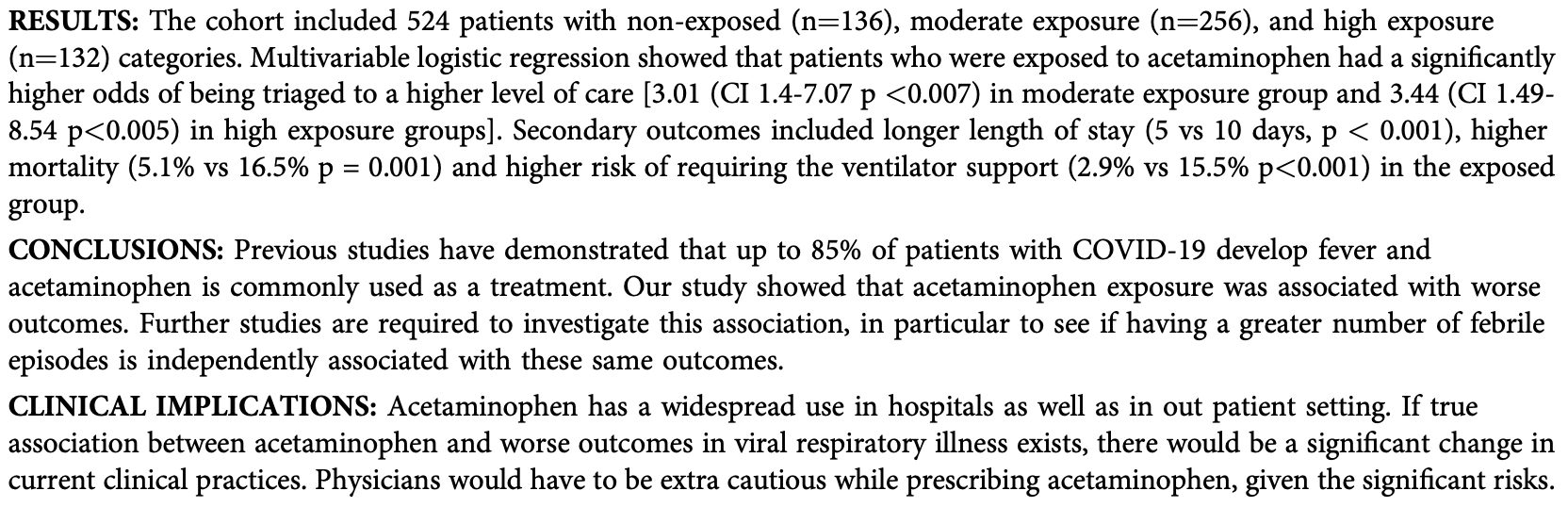
RESULTS: The cohort included 524 patients with non-exposed (n¼136), moderate exposure (n¼256), and high exposure (n¼132) categories. Multivariable logistic regression showed that patients who were exposed to acetaminophen had a significantly higher odds of being triaged to a higher level of care [3.01 (CI 1.4-7.07 p <0.007) in moderate exposure group and 3.44 (CI 1.49-8.54 p<0.005) in high exposure groups]. Secondary outcomes included longer length of stay (5 vs 10 days, p < 0.001), higher mortality (5.1% vs 16.5% p = 0.001) and higher risk of requiring the ventilator support (2.9% vs 15.5% p<0.001) in the exposed group. CONCLUSIONS: Previous studies have demonstrated that up to 85% of patients with COVID-19 develop fever and acetaminophen is commonly used as a treatment. Our study showed that acetaminophen exposure was associated with worse outcomes. Further studies are required to investigate this association, in particular to see if having a greater number of febrile episodes is independently associated with these same outcomes. CLINICAL IMPLICATIONS: Acetaminophen has a widespread use in hospitals as well as in out patient setting. If true association between acetaminophen and worse outcomes in viral respiratory illness exists, there would be a significant change in current clinical practices. Physicians would have to be extra cautious while prescribing acetaminophen, given the significant risks. DISCLOSURES: No relevant relationships by Radhika Arya, source¼Web Response No relevant relationships by Neerja Desai, source¼Web Response No relevant relationships by Sameer Desale, source¼Web Response No relevant relationships by Akshay Kohli, source¼Web Response No relevant relationships by lokesh..
DOI record:
{
"DOI": "10.1016/j.chest.2021.07.992",
"ISSN": [
"0012-3692"
],
"URL": "http://dx.doi.org/10.1016/j.chest.2021.07.992",
"alternative-id": [
"S0012369221024430"
],
"author": [
{
"affiliation": [],
"family": "MANJANI",
"given": "LOKESH",
"sequence": "first"
},
{
"affiliation": [],
"family": "DESAI",
"given": "NEERJA",
"sequence": "additional"
},
{
"affiliation": [],
"family": "KOHLI",
"given": "AKSHAY",
"sequence": "additional"
},
{
"affiliation": [],
"family": "ARYA",
"given": "RADHIKA",
"sequence": "additional"
},
{
"affiliation": [],
"family": "WOODS",
"given": "CHRISTIAN",
"sequence": "additional"
},
{
"affiliation": [],
"family": "DESALE",
"given": "SAMEER",
"sequence": "additional"
}
],
"container-title": "Chest",
"container-title-short": "Chest",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
10,
11
]
],
"date-time": "2021-10-11T12:48:24Z",
"timestamp": 1633956504000
},
"deposited": {
"date-parts": [
[
2022,
2,
19
]
],
"date-time": "2022-02-19T06:08:29Z",
"timestamp": 1645250909000
},
"indexed": {
"date-parts": [
[
2022,
8,
10
]
],
"date-time": "2022-08-10T16:49:44Z",
"timestamp": 1660150184666
},
"is-referenced-by-count": 1,
"issue": "4",
"issued": {
"date-parts": [
[
2021,
10
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2021,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
10,
1
]
],
"date-time": "2021-10-01T00:00:00Z",
"timestamp": 1633046400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0012369221024430?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0012369221024430?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "A1072",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
10
]
]
},
"published-print": {
"date-parts": [
[
2021,
10
]
]
},
"publisher": "Elsevier BV",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0012369221024430"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cardiology and Cardiovascular Medicine",
"Critical Care and Intensive Care Medicine",
"Pulmonary and Respiratory Medicine"
],
"subtitle": [],
"title": "EFFECTS OF ACETAMINOPHEN ON OUTCOMES IN PATIENTS HOSPITALIZED WITH COVID-19",
"type": "journal-article",
"volume": "160"
}