Bamlanivimab Use in a Military Treatment Facility
et al., Military Medicine, doi:10.1093/milmed/usab188, May 2021
25th treatment shown to reduce risk in
May 2021, now with p = 0.00049 from 22 studies, recognized in 11 countries.
Efficacy is variant dependent.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
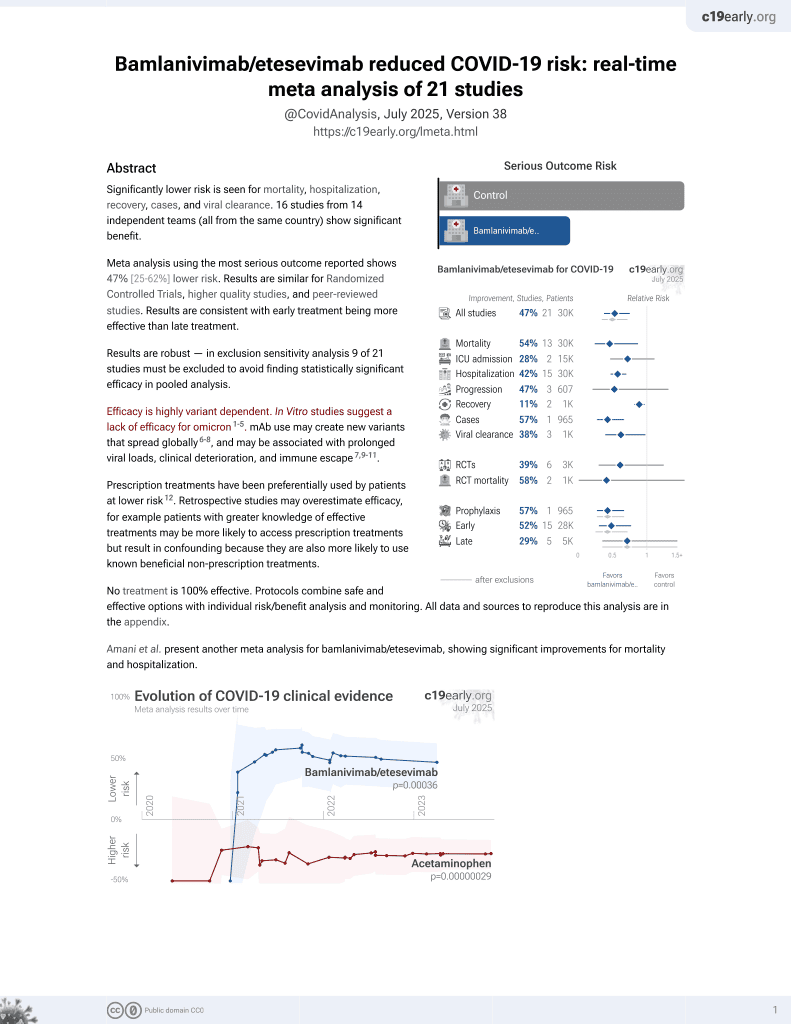
Retrospective 40 outpatients showing improvement in symptoms and lower risk of hospitalization/ER visits with bamlanivimab, without statistical significance.
Different counts for hospitalization are provided in the abstract and text: "Three of 40 (7.5%) patients in the treatment group required inpatient admission" and "In the treatment group, 4 of 40 (10%) patients were hospitalized after infusion."
Although the 40% lower hospitalization is not statistically significant, it is consistent with the significant 42% lower hospitalization [30‑53%] from meta-analysis of the 15 hospitalization results to date.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments6.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of hospitalization, 40.0% lower, RR 0.60, p = 0.52, treatment 4 of 40 (10.0%), control 1 of 6 (16.7%), NNT 15, day 30.
|
|
risk of hospitalization/ER, 62.5% lower, RR 0.38, p = 0.22, treatment 5 of 40 (12.5%), control 2 of 6 (33.3%), NNT 4.8, day 30.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Liu et al., Striking Antibody Evasion Manifested by the Omicron Variant of SARS-CoV-2, bioRxiv, doi:10.1101/2021.12.14.472719.
2.
Sheward et al., Variable loss of antibody potency against SARS-CoV-2 B.1.1.529 (Omicron), bioRxiv, doi:10.1101/2021.12.19.473354.
3.
VanBlargan et al., An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by several therapeutic monoclonal antibodies, bioRxiv, doi:10.1101/2021.12.15.472828.
4.
Pochtovyi et al., In Vitro Efficacy of Antivirals and Monoclonal Antibodies against SARS-CoV-2 Omicron Lineages XBB.1.9.1, XBB.1.9.3, XBB.1.5, XBB.1.16, XBB.2.4, BQ.1.1.45, CH.1.1, and CL.1, Vaccines, doi:10.3390/vaccines11101533.
Karr et al., 16 May 2021, retrospective, USA, peer-reviewed, 5 authors, study period 3 December, 2020 - 12 January, 2021.
Bamlanivimab Use in a Military Treatment Facility
Military Medicine, doi:10.1093/milmed/usab188
Background: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease 2019 (COVID-19), was first identified in 2019 in Wuhan, China, and has rapidly spread across the world. As of April 2021, SARS-CoV-2 has infected more than 140,000,000 and caused more than 3,000,000 deaths globally. In November 2020, the monoclonal antibody bamlanivimab was approved by the FDA for non-hospitalized patients with SARS-CoV-2 (COVID-19) who possessed risk factors for progression to severe COVID-19. This provided a treatment option that may help prevent hospitalization.
Methods: Patients who regularly received ambulatory care at a military treatment facility and who were diagnosed with mildto-moderate COVID-19 and possessed risk factors for progression to severe COVID-19 were treated with a single, intravenous infusion (700 mg) of the virus-neutralizing monoclonal antibody bamlanivimab. The primary outcome was improvement of self-reported symptoms within 24 to 72 hours of receiving the infusion. The secondary outcome was prevention of disease progression requiring emergency department (ED) utilization or hospitalization related to COVID-19 within 30 days of infusion. Bamlanivimab was administered in accordance with the FDA's approval and Defense Health Agency's guidance, including follow-up within 72 hours of administration. Institutional Review Board (IRB) approval was obtained.
Results: Of the COVID-19 patients who were given the option of a bamlanivimab infusion, 40 accepted and 6 did not (40/46, 86.9%). Thirty-six of 40 patients in the treatment group were contacted within 72 hours. ED/hospitalization information was available for all 46 patients. In the treatment group, 94.4% (34/36) reported global improvement. Three of 40 (7.5%) patients in the treatment group required inpatient admission, and 2 of 40 patients (5%) required ED evaluation within 30 days of infusion. Therefore, 5 of 40 (12.5%) patients required evaluation shortly after infusion, while 2 of 6 (33.3%) patients who declined treatment required hospital evaluation or admission related to COVID-19 within 30 days of infusion (P = .15).
Conclusions: Global improvement of symptoms within 24 to 72 hours of infusion was reported by 94.4% of patients receiving bamlanivimab; however, statistical significance could not be determined due to the small sample size and lack of placebo group due to study design. Furthermore, ED visits and hospital admissions were analyzed, but with only six patients in the comparison group, the relative risk was not statistically significant and could not be precisely estimated. In the future, this study can be replicated with both larger control/treatment arms to validate the initial results of this small, retrospective, cohort study.
CONFLICT OF INTEREST STATEMENT None declared.
References
Baum, Ajithdoss, Copin, REGN-COV2 antibodies prevent and treat SARS-CoV-2 infection in rhesus macaques and hamsters, Science
Bhimraj, Morgan, Shumaker, Infectious Diseases Society of America guidelines on the treatment and management of patients with COVID-19, Clin Infect Dis
Chan, Yuan, Kok, A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-toperson transmission: a study of a family cluster, Lancet
Cummings, Baldwin, Abrams, Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study, Lancet
Farooqi, Dhawan, Morgan, Dinh, Nedd et al., Treatment of severe COVID-19 with tocilizumab mitigates cytokine storm and averts mechanical ventilation during acute respiratory distress: a case report and literature review, Trop Med Infect Dis
Goldman, Lye, Hui, Remdesivir for 5 or 10 days in patients with severe Covid-19, N Engl J Med
Gottlieb, Nirula, Chen, Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial, JAMA
Hoffmann, Kleine-Weber, Schroeder, SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cell
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Jehi, Ji, Milinovich, Development and validation of a model for individualized prediction of hospitalization risk in 4,536 patients with COVID-19, PLoS One
Li, Zhang, Hu, Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial, JAMA
Liu, Yan, Wan, Viral dynamics in mild and severe cases of COVID-19, Lancet Infect Dis
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.1093/milmed/usab188",
"ISSN": [
"0026-4075",
"1930-613X"
],
"URL": "http://dx.doi.org/10.1093/milmed/usab188",
"abstract": "<jats:title>ABSTRACT</jats:title>\n <jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease 2019 (COVID-19), was first identified in 2019 in Wuhan, China, and has rapidly spread across the world. As of April 2021, SARS-CoV-2 has infected more than 140,000,000 and caused more than 3,000,000 deaths globally. In November 2020, the monoclonal antibody bamlanivimab was approved by the FDA for non-hospitalized patients with SARS-CoV-2 (COVID-19) who possessed risk factors for progression to severe COVID-19. This provided a treatment option that may help prevent hospitalization.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>Patients who regularly received ambulatory care at a military treatment facility and who were diagnosed with mild-to-moderate COVID-19 and possessed risk factors for progression to severe COVID-19 were treated with a single, intravenous infusion (700 mg) of the virus-neutralizing monoclonal antibody bamlanivimab. The primary outcome was improvement of self-reported symptoms within 24 to 72 hours of receiving the infusion. The secondary outcome was prevention of disease progression requiring emergency department (ED) utilization or hospitalization related to COVID-19 within 30 days of infusion. Bamlanivimab was administered in accordance with the FDA’s approval and Defense Health Agency’s guidance, including follow-up within 72 hours of administration. Institutional Review Board (IRB) approval was obtained.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Of the COVID-19 patients who were given the option of a bamlanivimab infusion, 40 accepted and 6 did not (40/46, 86.9%). Thirty-six of 40 patients in the treatment group were contacted within 72 hours. ED/hospitalization information was available for all 46 patients. In the treatment group, 94.4% (34/36) reported global improvement. Three of 40 (7.5%) patients in the treatment group required inpatient admission, and 2 of 40 patients (5%) required ED evaluation within 30 days of infusion. Therefore, 5 of 40 (12.5%) patients required evaluation shortly after infusion, while 2 of 6 (33.3%) patients who declined treatment required hospital evaluation or admission related to COVID-19 within 30 days of infusion (P = .15).</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>Global improvement of symptoms within 24 to 72 hours of infusion was reported by 94.4% of patients receiving bamlanivimab; however, statistical significance could not be determined due to the small sample size and lack of placebo group due to study design. Furthermore, ED visits and hospital admissions were analyzed, but with only six patients in the comparison group, the relative risk was not statistically significant and could not be precisely estimated. In the future, this study can be replicated with both larger control/treatment arms to validate the initial results of this small, retrospective, cohort study.</jats:p>\n </jats:sec>",
"author": [
{
"affiliation": [
{
"name": "Wright-Patterson Medical Center, Wright-Patterson AFB , OH 45433, USA"
},
{
"name": "Boonshoft School of Medicine, Wright State University , Fairborn, OH 45324, USA"
}
],
"family": "Karr",
"given": "Eric",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Wright-Patterson Medical Center, Wright-Patterson AFB , OH 45433, USA"
},
{
"name": "Boonshoft School of Medicine, Wright State University , Fairborn, OH 45324, USA"
}
],
"family": "Chung",
"given": "Theodore",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Wright-Patterson Medical Center, Wright-Patterson AFB , OH 45433, USA"
},
{
"name": "Boonshoft School of Medicine, Wright State University , Fairborn, OH 45324, USA"
}
],
"family": "Burtson",
"given": "Kathryn",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Boonshoft School of Medicine, Wright State University , Fairborn, OH 45324, USA"
}
],
"family": "Markert",
"given": "Ronald",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Wright-Patterson Medical Center, Wright-Patterson AFB , OH 45433, USA"
},
{
"name": "Boonshoft School of Medicine, Wright State University , Fairborn, OH 45324, USA"
}
],
"family": "Kelly",
"given": "Devin",
"sequence": "additional"
}
],
"container-title": "Military Medicine",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
5,
16
]
],
"date-time": "2021-05-16T12:09:59Z",
"timestamp": 1621166999000
},
"deposited": {
"date-parts": [
[
2022,
12,
15
]
],
"date-time": "2022-12-15T21:58:25Z",
"timestamp": 1671141505000
},
"indexed": {
"date-parts": [
[
2023,
5,
8
]
],
"date-time": "2023-05-08T07:50:53Z",
"timestamp": 1683532253753
},
"is-referenced-by-count": 4,
"issue": "Special Issue_13",
"issued": {
"date-parts": [
[
2021,
5,
16
]
]
},
"journal-issue": {
"issue": "Special Issue_13",
"published-online": {
"date-parts": [
[
2021,
5,
16
]
]
},
"published-print": {
"date-parts": [
[
2022,
12,
5
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://academic.oup.com/milmed/article-pdf/187/Special%20Issue_13/e1509/47913783/usab188.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/milmed/article-pdf/187/Special%20Issue_13/e1509/47913783/usab188.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "286",
"original-title": [],
"page": "e1509-e1512",
"prefix": "10.1093",
"published": {
"date-parts": [
[
2021,
5,
16
]
]
},
"published-online": {
"date-parts": [
[
2021,
5,
16
]
]
},
"published-other": {
"date-parts": [
[
2022,
11,
1
]
]
},
"published-print": {
"date-parts": [
[
2022,
12,
5
]
]
},
"publisher": "Oxford University Press (OUP)",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30154-9",
"article-title": "A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster",
"author": "Chan",
"doi-asserted-by": "publisher",
"first-page": "514",
"journal-title": "Lancet",
"key": "2022121510471705800_R1",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)31189-2",
"article-title": "Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study",
"author": "Cummings",
"doi-asserted-by": "publisher",
"first-page": "1763",
"issue": "10239",
"journal-title": "Lancet",
"key": "2022121510471705800_R2",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "497",
"issue": "10223",
"journal-title": "Lancet",
"key": "2022121510471705800_R3",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0237419",
"article-title": "Development and validation of a model for individualized prediction of hospitalization risk in 4,536 patients with COVID-19",
"author": "Jehi",
"doi-asserted-by": "publisher",
"issue": "8",
"journal-title": "PLoS One",
"key": "2022121510471705800_R4",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"issue": "10229",
"journal-title": "Lancet",
"key": "2022121510471705800_R5",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.10044",
"article-title": "Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "460",
"issue": "5",
"journal-title": "JAMA",
"key": "2022121510471705800_R6",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1056/nejmoa2015301",
"article-title": "Remdesivir for 5 or 10 days in patients with severe Covid-19",
"author": "Goldman",
"doi-asserted-by": "publisher",
"first-page": "1827",
"issue": "19",
"journal-title": "N Engl J Med",
"key": "2022121510471705800_R7",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.3390/tropicalmed5030112",
"article-title": "Treatment of severe COVID-19 with tocilizumab mitigates cytokine storm and averts mechanical ventilation during acute respiratory distress: a case report and literature review",
"author": "Farooqi",
"doi-asserted-by": "publisher",
"issue": "3",
"journal-title": "Trop Med Infect Dis",
"key": "2022121510471705800_R8",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1001/jama.2021.0202",
"article-title": "Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial",
"author": "Gottlieb",
"doi-asserted-by": "publisher",
"first-page": "632",
"issue": "7",
"journal-title": "JAMA",
"key": "2022121510471705800_R9",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor",
"author": "Hoffmann",
"doi-asserted-by": "publisher",
"first-page": "271",
"issue": "2",
"journal-title": "Cell",
"key": "2022121510471705800_R10",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(20)30232-2",
"article-title": "Viral dynamics in mild and severe cases of COVID-19",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "p656",
"issue": "6",
"journal-title": "Lancet Infect Dis",
"key": "2022121510471705800_R11",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1126/science.abe2402",
"article-title": "REGN-COV2 antibodies prevent and treat SARS-CoV-2 infection in rhesus macaques and hamsters",
"author": "Baum",
"doi-asserted-by": "publisher",
"first-page": "1110",
"issue": "6520",
"journal-title": "Science",
"key": "2022121510471705800_R12",
"volume": "370",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa478",
"article-title": "Infectious Diseases Society of America guidelines on the treatment and management of patients with COVID-19",
"author": "Bhimraj",
"doi-asserted-by": "publisher",
"journal-title": "Clin Infect Dis",
"key": "2022121510471705800_R13",
"volume": "ciaa478",
"year": "2020"
}
],
"reference-count": 13,
"references-count": 13,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/milmed/article/187/Special%20Issue_13/e1509/6276449"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Public Health, Environmental and Occupational Health",
"General Medicine"
],
"subtitle": [],
"title": "Bamlanivimab Use in a Military Treatment Facility",
"type": "journal-article",
"volume": "187"
}