Cross-Section of Neurological Manifestations Among SARS-CoV-2 Omicron Subvariants—Single-Center Study
et al., Brain Sciences, doi:10.3390/brainsci14111161, Nov 2024
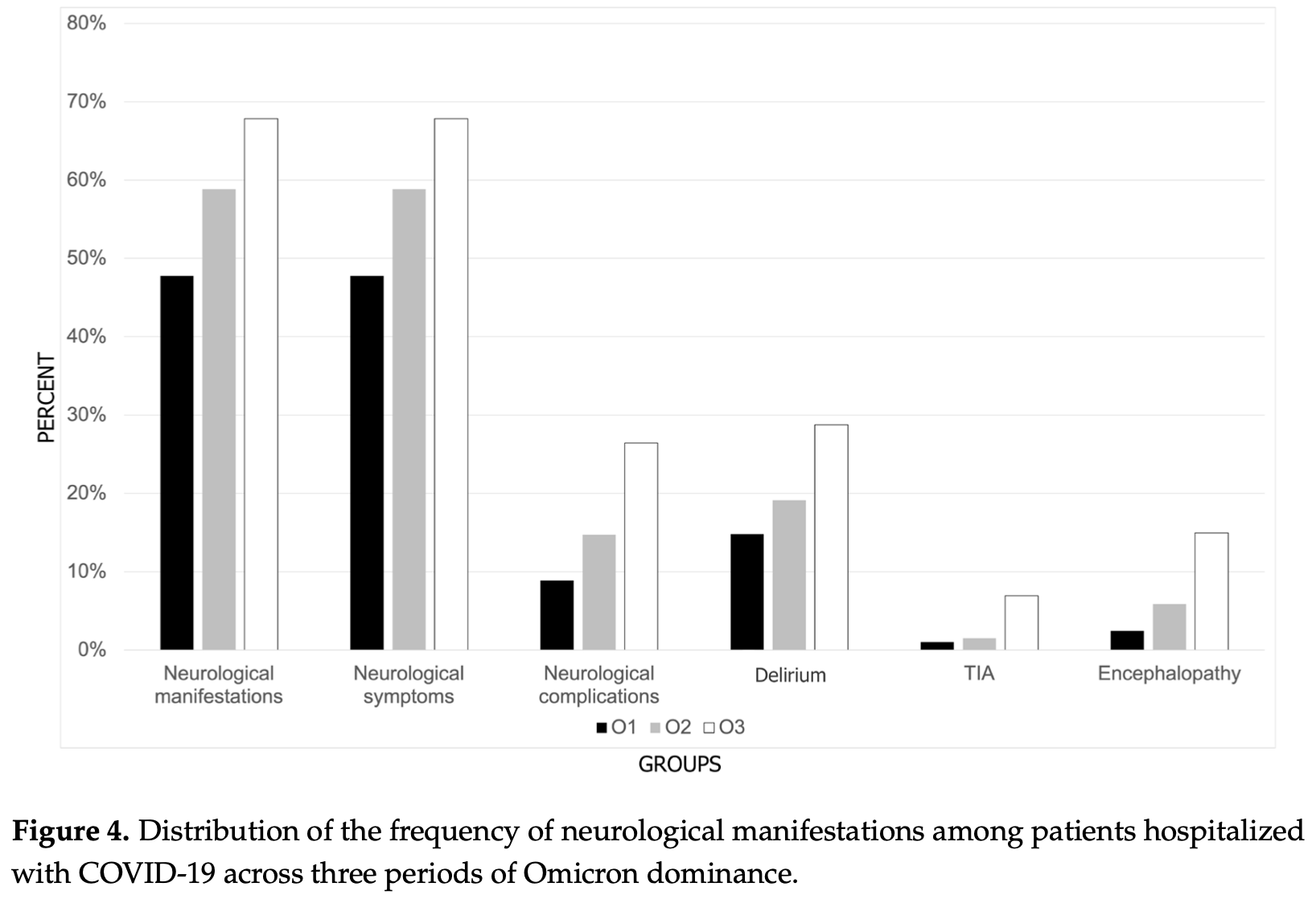
Retrospective 426 hospitalized COVID-19 patients in Poland during Omicron dominance, showing increasing neurological manifestations over time across three Omicron subvariant periods despite improving overall survival. Authors hypothesize that different Omicron subvariants have varying neuropathogenicity, with later subvariants potentially causing stronger immune suppression and neurodegeneration while simultaneously becoming less systemically severe.
Jachman-Kapułka et al., 20 Nov 2024, retrospective, Poland, peer-reviewed, 4 authors.
Contact: justyna.jachman@gmail.com (corresponding author), alek.zinczuk@gmail.com, krzysimon@gmail.com, marta.rorat@gmail.com.
Cross-Section of Neurological Manifestations Among SARS-CoV-2 Omicron Subvariants—Single-Center Study
Brain Sciences, doi:10.3390/brainsci14111161
Background/Objectives: The Omicron variant of SARS-CoV-2 is undergoing constant mutation. New strains vary in neuropathogenicity and the neurological spectrum of disease. The aim of this study was to assess the frequency and clinical characteristics of neurological manifestations during the Omicron dominance among hospitalized patients, including the differences between three subsequent periods. Methods: This retrospective single-center study included 426 hospitalized adults with confirmed COVID-19 divided into three periods (O1, O2, and O3) dependent on the dominance of Omicron subvariants in Poland. Demographic and clinical data, in particular neurological manifestations, were collected and compared. Results: The median age of the group was 74, older in subsequent (later) periods. The number of patients with a history of previous SARS-CoV-2 infection or vaccination increased with the duration of the pandemic. The severity of COVID-19 became lower in successive periods. Neurological manifestations were observed in 55.4% of patients, and the most frequent were delirium, headache, myalgia, dizziness, cerebrovascular diseases, and encephalopathy. In subsequent periods of Omicron dominance, a higher frequency of neurological manifestations such as delirium, transient ischemic attack (TIA), and encephalopathy was observed. Headache or myalgia was related to a shorter hospitalization while delirium, cerebrovascular diseases, and ischemic stroke were linked with an increased risk of death. Conclusions: The Omicron variant of SARS-CoV-2 presents a wide spectrum of neurological manifestations. Although there is an improvement in the survival rate of patients with COVID-19, the frequency of neurological manifestations increases. The occurrence of delirium, cerebrovascular diseases, and ischemic stroke results in higher mortality.
Author Contributions: Conceptualization, J.J.-K. and M.R.; investigation and data collection, J.J.-K. and A.Z.; writing-original draft preparation, J.J.-K.; writing-review and editing, J.J.-K., M.R. and K.S.; supervision, K.S. and M.R.; final approval, M.R. All authors have read and agreed to the published version of the manuscript. Declaration of Helsinki, and approved by the Ethics Committee of Lower Silesian Medical Chamber (protocol code 02/BNR/2024 from 12 March 2024). Informed Consent Statement: Patient consent was waived due to the retrospective nature of this work.
Conflicts of Interest: The authors declare no conflicts of interest.
References
Albitar, Ballouze, Ooi, Sheikh Ghadzi, Risk factors for mortality among COVID-19 patients, Diabetes Res. Clin. Pract, doi:10.1016/j.diabres.2020.108293
Amanat, Rezaei, Roozbeh, Shojaei, Tafakhori et al., Neurological manifestations as the predictors of severity and mortality in hospitalized individuals with COVID-19: A multicenter prospective clinical study, BMC Neurol, doi:10.1186/s12883-021-02152-5
Anscombe, Lissauer, Thole, Rylance, Dula et al., A comparison of four epidemic waves of COVID-19 in Malawi; an observational cohort study, BMC Infect. Dis, doi:10.1186/s12879-022-07941-y
Bauer, Laksono, De Vrij, Kushner, Harschnitz et al., The neuroinvasiveness, neurotropism, and neurovirulence of SARS-CoV-2, Trends Neurosci, doi:10.1016/j.tins.2022.02.006
Bauer, Van Riel, Do SARS-CoV-2 Variants Differ in Their Neuropathogenicity?, mBio, doi:10.1128/mbio.02920-22
Brola, Wilski, Neurological consequences of COVID-19, Pharmacol. Rep, doi:10.1007/s43440-022-00424-6
Callaway, Heavily mutated Omicron variant puts scientists on alert, Nature, doi:10.1038/d41586-021-03552-w
Cao, Yisimayi, Jian, Song, Xiao et al., 2.12.1, BA.4 and BA.5 escape antibodies elicited by Omicron infection, Nature, doi:10.1038/s41586-022-04980-y
Caronna, Ballvé, Llauradó, Gallardo, Ariton et al., Headache: A striking prodromal and persistent symptom, predictive of COVID-19 clinical evolution, Cephalalgia, doi:10.1177/0333102420965157
Chang, Huang, Shie, Lin, Chen, Clinical features and virologic lineages of COVID-19-associated encephalitis in Taiwanese children during early epidemic wave of omicron in 2022: Report from a medical center, J. Microbiol. Immunol. Infect, doi:10.1016/j.jmii.2023.10.005
Chatterjee, Bhattacharya, Nag, Dhama, Chakraborty, A Detailed Overview of SARS-CoV-2 Omicron: Its Sub-Variants, Mutations and Pathophysiology, Clinical Characteristics, Immunological Landscape, Immune Escape, and Therapies, Viruses, doi:10.3390/v15010167
Cojocaru, Cojocaru, Turcanu, Zaharia, Clinical challenges of SARS-CoV-2 variants (Review), Exp. Ther. Med, doi:10.3892/etm.2022.11343
De Rioja, Basile, Perramon-Malavez, Martínez-Solanas, López et al., Severity of Omicron Subvariants and Vaccine Impact in Catalonia, Spain, Vaccines, doi:10.3390/vaccines12050466
Dhama, Nainu, Frediansyah, Yatoo, Mohapatra et al., Global emerging Omicron variant of SARS-CoV-2: Impacts, challenges and strategies, J. Infect. Public Health, doi:10.1016/j.jiph.2022.11.024
Di Giorgio, Mirijello, De Gennaro, Fontana, Alboini et al., Factors Associated with Delirium in COVID-19 Patients and Their Outcome: A Single-Center Cohort Study, Diagnostics, doi:10.3390/diagnostics12020544
Diaconu, Irimie-Bălut, Vâţă, Avadanei, Vasilescu et al., COVID-19 neurological manifestations-The experience of a tertiary hospital from Northeastern Romania, Med. Surg. J. Rev. Med. Chir. Soc. Med. Nat. Iaşi, doi:10.22551/MSJ.2024.01.03
Drabik, Derbisz, Chatys-Bogacka, Mazurkiewicz, Sawczynska et al., Neurological Prognostic Factors in Hospitalized Patients with COVID-19, Brain Sci, doi:10.3390/brainsci12020193
Ellul, Benjamin, Singh, Lant, Michael et al., Neurological associations of COVID-19, Lancet Neurol, doi:10.1016/S1474-4422(20)30221-0
Flisiak, Zarębska-Michaluk, Dobrowolska, Rorat, Rogalska et al., Change in the Clinical Picture of Hospitalized Patients with COVID-19 between the Early and Late Period of Dominance of the Omicron SARS-CoV-2 Variant, J. Clin. Med, doi:10.3390/jcm12175572
Forero, Buqaileh, Sunderman, Aboualaiwi, COVID-19 and Neurological Manifestations, Brain Sci, doi:10.3390/brainsci13081137
Goller, Ziemann, Kohler, Becker, Hübner, Clinical Manifestations of Infections with the Omicron Sub-Lineages BA.1, BA.2, and BA.5: A Retrospective Follow-Up Analysis of Public Health Data from Mecklenburg-Western Pomerania, Viruses, doi:10.3390/v16030454
Griggs, Mitchell, Lazariu, Gaglani, Mcevoy et al., Clinical Epidemiology and Risk Factors for Critical Outcomes Among Vaccinated and Unvaccinated Adults Hospitalized With COVID-19-VISION Network, 10 States, Clin. Infect. Dis, doi:10.1093/cid/ciad505
Hawkins, Sockalingam, Bonato, Rajaratnam, Ravindran et al., A rapid review of the pathoetiology, presentation, and management of delirium in adults with COVID-19, J. Psychosom. Res, doi:10.1016/j.jpsychores.2020.110350
Hoteit, Yassine, Biological Properties of SARS-CoV-2 Variants: Epidemiological Impact and Clinical Consequences, Vaccines, doi:10.3390/vaccines10060919
Jachman-Kapułka, Zi Ńczuk, Szyma Ński, Simon, Rorat, Complexity and Diversity of the Neurological Spectrum of SARS-CoV-2 over Three Waves of COVID-19, J. Clin. Med, doi:10.3390/jcm13123477
Jagst, Pottkämper, Gömer, Pitarokoili, Steinmann, Neuroinvasion and neurotropism of severe acute respiratory syndrome coronavirus 2 infection, Curr. Opin. Microbiol, doi:10.1016/j.mib.2024.102474
Jung, Kmiec, Koepke, Zech, Jacob et al., Omicron: What Makes the Latest SARS-CoV-2 Variant of Concern So Concerning?, J. Virol, doi:10.1128/jvi.02077-21
Kim, Choi, Kim, Cho, Kim et al., Severe Neurological Manifestation Associated With Coronavirus Disease 2019 in Children During the Omicron Variant-Predominant Period, Pediatr. Neurol, doi:10.1016/j.pediatrneurol.2024.04.004
Kulkarni, Gupta, Pujari, Deshpande, Naphade et al., Neurological Manifestations in COVID-19 in Three Waves of the Pandemic: An Inpatient Study from India, Ann. Indian Acad. Neurol, doi:10.4103/aian.aian_204_22
Liu, Xie, Wang, Xiong, Chen et al., A comparative overview of COVID-19, MERS and SARS: Review article, Int. J. Surg, doi:10.1016/j.ijsu.2020.07.032
Lu, Chen, Wang, Qi, Chen et al., Neurological complications during the Omicron COVID-19 wave in China: A cohort study, Eur. J. Neurol, doi:10.1111/ene.16096
Mao, Jin, Wang, Hu, Chen et al., Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China, JAMA Neurol, doi:10.1001/jamaneurol.2020.1127
Markov, Ghafari, Beer, Lythgoe, Simmonds et al., The evolution of SARS-CoV-2, Nat. Rev. Microbiol, doi:10.1038/s41579-023-00878-2
Marron, Mateo-Urdiales, O'donnell, Robinson, Domegan, The impact of the COVID-19 vaccination programme on symptomatic and severe SARS-CoV-2 infection during a period of Omicron variant dominance in Ireland, December 2021 to March 2023, Euro Surveill, doi:10.2807/1560-7917.ES.2024.29.28.2300697
Mekkawy, Hamdy, Abdel-Naseer, Shehata, Halfawy et al., Neurological Manifestations in a Cohort of Egyptian Patients with COVID-19: A Prospective, Multicenter, Observational Study, Brain Sci, doi:10.3390/brainsci12010074
Mohapatra, Kandi, Sarangi, Verma, Tuli et al., The recently emerged BA.4 and BA.5 lineages of Omicron and their global health concerns amid the ongoing wave of COVID-19 pandemic-Correspondence, Int. J. Surg, doi:10.1016/j.ijsu.2022.106698
Morris, Eldesouki, Sachithanandham, Fall, Norton et al., Omicron Subvariants: Clinical, Laboratory, and Cell Culture Characterization, Clin. Infect. Dis, doi:10.1093/cid/ciac885
Ng, Sun, Je, Tan, Unravelling Pathophysiology of Neurological and Psychiatric Complications of COVID-19 Using Brain Organoids, Neuroscientist, doi:10.1177/10738584211015136
Ong, Chiew, Ang, Mak, Cui et al., Clinical and Virological Features of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Variants of Concern: A Retrospective Cohort Study Comparing B.1.1.7 (Alpha), B.1.351 (Beta), and B.1.617, Clin. Infect. Dis, doi:10.1093/cid/ciab721
Pather, Madhi, Cowling, Moss, Kamil et al., SARS-CoV-2 Omicron variants: Burden of disease, impact on vaccine effectiveness and need for variant-adapted vaccines, Front. Immunol, doi:10.3389/fimmu.2023.1130539
Pavel, Moroti, Spataru, Popescu, Panaitescu et al., Neurological Manifestations of SARS-CoV2 Infection: A Narrative Review, Brain Sci, doi:10.3390/brainsci12111531
Proust, Queval, Harvey, Adams, Bennett et al., Differential effects of SARS-CoV-2 variants on central nervous system cells and blood-brain barrier functions, J. Neuroinflamm, doi:10.1186/s12974-023-02861-3
Ramesh, Govindarajulu, Parise, Neel, Shankar et al., Emerging SARS-CoV-2 Variants: A Review of Its Mutations, Its Implications and Vaccine Efficacy, Vaccines, doi:10.3390/vaccines9101195
Sahin, Karadag-Oncel, Buyuksen, Ekemen-Keles, Ustundag et al., 1.1.7), Delta (B.1.617.2, and Omicron (B.1.1.529) variant periods of SARS CoV-2: Caution for neurological symptoms in Omicron variant, J. Med. Virol, doi:10.1002/jmv.28628
Sanjuán, Domingo-Calap, Mechanisms of viral mutation, Cell. Mol. Life Sci, doi:10.1007/s00018-016-2299-6
Seehusen, Clark, Sharma, Bentley, Kirby et al., Neuroinvasion and Neurotropism by SARS-CoV-2 Variants in the K18-hACE2 Mouse, Viruses, doi:10.3390/v14051020
Seyler, Van Nedervelde, De Cock, Mann, Pien et al., Surfing the Waves: Differences in Hospitalised COVID-19 Patients across 4 Variant Waves in a Belgian University Hospital, Viruses, doi:10.3390/v15030618
Shapiro, Gallardo, Caronna, Pozo-Rosich, The impact of headache disorders on COVID-19 survival: A world population-based analysis, medRxiv, doi:10.1101/2021.03.10.21253280
Shen, Wang, Shen, Jiang, Wu et al., Neurological Manifestations of hospitalized patients with mild to moderate infection with SARS-CoV-2 Omicron variant in Shanghai, China, J. Infect. Public Health, doi:10.1016/j.jiph.2022.12.005
Sureshbabu, Joseph, Haseena, Basheer, Srutha Keerthi et al., Comparison of Neurological Manifestations in the Two Waves of COVID-19 Infection: A Cross-Sectional Study, Ann. Indian Acad. Neurol, doi:10.4103/aian.aian_1048_21
Syahrul, Maliga, Ilmawan, Fahriani, Mamada et al., Hemorrhagic and ischemic stroke in patients with coronavirus disease 2019: Incidence, risk factors, and pathogenesis-A systematic review and meta-analysis, Research, doi:10.12688/f1000research.42308.1
Tetsuhara, Akamine, Matsubara, Fujii, Kashimada et al., Severe encephalopathy associated with SARS-CoV-2 Omicron BA.1 variant infection in a neonate, Brain Dev, doi:10.1016/j.braindev.2022.06.010
Wang, Yang, Xu, Zou, Long et al., Differential pathogenic and molecular features in neurological infection of SARS-CoV-2 Omicron BA.5.2 and BA.2.75 and Delta, J. Med. Virol, doi:10.1002/jmv.29357
Wang, Yu, Shi, Zhang, Huo et al., Retrospective study about clinical severity and epidemiological analysis of the COVID-19 Omicron subvariant lineage-infected patients in Hohhot, China, BMC Infect. Dis, doi:10.1186/s12879-024-09084-8
Wnuk, Sawczy Ńska, Kęsek, Wrona, Chatys-Bogacka et al., Neurological symptoms in hospitalised patients with COVID-19 and their association with in-hospital mortality, Neurol. Neurochir. Pol, doi:10.5603/PJNNS.a2021.0039
Wu, Li, Zhang, Liang, Zhang et al., Risk factors for mortality of coronavirus disease 2019 (COVID-19) patients during the early outbreak of COVID-19: A systematic review and meta-analysis, Ann. Palliat. Med, doi:10.21037/apm-20-2557
Xiong, Lu, Zhang, Luo, Li et al., Association of consciousness impairment and mortality in people with COVID-19, Acta Neurol. Scand, doi:10.1111/ane.13471
Xue, Zeng, He, Xu, Ren, Autoimmune encephalitis in COVID-19 patients: A systematic review of case reports and case series, Front. Neurol, doi:10.3389/fneur.2023.1207883
Yang, Yang, Kim, Kim, Tark et al., B1.617.2) variant of SARS-CoV-2 induces severe neurotropic patterns in K18-hACE2 mice, Sci. Rep, doi:10.1038/s41598-023-29909-x
Zhang, Wu, He, Liu, Liu et al., Age-Related Risk Factors and Complications of Patients With COVID-19: A Population-Based Retrospective Study, Front. Med, doi:10.3389/fmed.2021.757459
DOI record:
{
"DOI": "10.3390/brainsci14111161",
"ISSN": [
"2076-3425"
],
"URL": "http://dx.doi.org/10.3390/brainsci14111161",
"abstract": "<jats:p>Background/Objectives: The Omicron variant of SARS-CoV-2 is undergoing constant mutation. New strains vary in neuropathogenicity and the neurological spectrum of disease. The aim of this study was to assess the frequency and clinical characteristics of neurological manifestations during the Omicron dominance among hospitalized patients, including the differences between three subsequent periods. Methods: This retrospective single-center study included 426 hospitalized adults with confirmed COVID-19 divided into three periods (O1, O2, and O3) dependent on the dominance of Omicron subvariants in Poland. Demographic and clinical data, in particular neurological manifestations, were collected and compared. Results: The median age of the group was 74, older in subsequent (later) periods. The number of patients with a history of previous SARS-CoV-2 infection or vaccination increased with the duration of the pandemic. The severity of COVID-19 became lower in successive periods. Neurological manifestations were observed in 55.4% of patients, and the most frequent were delirium, headache, myalgia, dizziness, cerebrovascular diseases, and encephalopathy. In subsequent periods of Omicron dominance, a higher frequency of neurological manifestations such as delirium, transient ischemic attack (TIA), and encephalopathy was observed. Headache or myalgia was related to a shorter hospitalization while delirium, cerebrovascular diseases, and ischemic stroke were linked with an increased risk of death. Conclusions: The Omicron variant of SARS-CoV-2 presents a wide spectrum of neurological manifestations. Although there is an improvement in the survival rate of patients with COVID-19, the frequency of neurological manifestations increases. The occurrence of delirium, cerebrovascular diseases, and ischemic stroke results in higher mortality.</jats:p>",
"alternative-id": [
"brainsci14111161"
],
"author": [
{
"affiliation": [
{
"name": "6th Department of Internal Medicine, J. Gromkowski Specialist Regional Hospital, 51-149 Wroclaw, Poland"
}
],
"family": "Jachman-Kapułka",
"given": "Justyna",
"sequence": "first"
},
{
"ORCID": "https://orcid.org/0000-0003-4725-123X",
"affiliation": [
{
"name": "1st Department of Infectious Diseases, J. Gromkowski Specialist Regional Hospital, 51-149 Wroclaw, Poland"
}
],
"authenticated-orcid": false,
"family": "Zińczuk",
"given": "Aleksander",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "1st Department of Infectious Diseases, J. Gromkowski Specialist Regional Hospital, 51-149 Wroclaw, Poland"
},
{
"name": "Clinical Department of Infectious Diseases and Hepatology, Wroclaw Medical University, 50-369 Wroclaw, Poland"
}
],
"family": "Simon",
"given": "Krzysztof",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-5318-4945",
"affiliation": [
{
"name": "Department of Social Sciences and Infectious Diseases, Medical Faculty, Wroclaw University of Science and Technology, 50-370 Wroclaw, Poland"
}
],
"authenticated-orcid": false,
"family": "Rorat",
"given": "Marta",
"sequence": "additional"
}
],
"container-title": "Brain Sciences",
"container-title-short": "Brain Sciences",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
11,
20
]
],
"date-time": "2024-11-20T15:37:35Z",
"timestamp": 1732117055000
},
"deposited": {
"date-parts": [
[
2024,
11,
22
]
],
"date-time": "2024-11-22T05:26:43Z",
"timestamp": 1732253203000
},
"indexed": {
"date-parts": [
[
2025,
2,
21
]
],
"date-time": "2025-02-21T17:49:56Z",
"timestamp": 1740160196589,
"version": "3.37.3"
},
"is-referenced-by-count": 0,
"issue": "11",
"issued": {
"date-parts": [
[
2024,
11,
20
]
]
},
"journal-issue": {
"issue": "11",
"published-online": {
"date-parts": [
[
2024,
11
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
11,
20
]
],
"date-time": "2024-11-20T00:00:00Z",
"timestamp": 1732060800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2076-3425/14/11/1161/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1161",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
11,
20
]
]
},
"published-online": {
"date-parts": [
[
2024,
11,
20
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1007/s00018-016-2299-6",
"article-title": "Mechanisms of viral mutation",
"doi-asserted-by": "crossref",
"first-page": "4433",
"journal-title": "Cell. Mol. Life Sci.",
"key": "ref_1",
"volume": "73",
"year": "2016"
},
{
"DOI": "10.1001/jamaneurol.2020.1127",
"article-title": "Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China",
"author": "Mao",
"doi-asserted-by": "crossref",
"first-page": "683",
"journal-title": "JAMA Neurol.",
"key": "ref_2",
"volume": "77",
"year": "2020"
},
{
"DOI": "10.3390/vaccines10060919",
"doi-asserted-by": "crossref",
"key": "ref_3",
"unstructured": "Hoteit, R., and Yassine, H.M. (2022). Biological Properties of SARS-CoV-2 Variants: Epidemiological Impact and Clinical Consequences. Vaccines, 10."
},
{
"DOI": "10.3390/vaccines9101195",
"doi-asserted-by": "crossref",
"key": "ref_4",
"unstructured": "Ramesh, S., Govindarajulu, M., Parise, R.S., Neel, L., Shankar, T., Patel, S., Lowery, P., Smith, F., Dhanasekaran, M., and Moore, T. (2021). Emerging SARS-CoV-2 Variants: A Review of Its Mutations, Its Implications and Vaccine Efficacy. Vaccines, 9."
},
{
"DOI": "10.1038/s41579-023-00878-2",
"article-title": "The evolution of SARS-CoV-2",
"author": "Markov",
"doi-asserted-by": "crossref",
"first-page": "361",
"journal-title": "Nat. Rev. Microbiol.",
"key": "ref_5",
"volume": "21",
"year": "2023"
},
{
"key": "ref_6",
"unstructured": "World Health Organization (WHO) (2024, January 18). Tracking SARS-CoV-2 Variants. Available online: https://www.who.int/activities/tracking-SARS-CoV-2-variants."
},
{
"DOI": "10.1128/jvi.02077-21",
"article-title": "Omicron: What Makes the Latest SARS-CoV-2 Variant of Concern So Concerning?",
"author": "Jung",
"doi-asserted-by": "crossref",
"first-page": "e0207721",
"journal-title": "J. Virol.",
"key": "ref_7",
"volume": "96",
"year": "2022"
},
{
"DOI": "10.1016/j.ijsu.2022.106698",
"article-title": "The recently emerged BA.4 and BA.5 lineages of Omicron and their global health concerns amid the ongoing wave of COVID-19 pandemic—Correspondence",
"author": "Mohapatra",
"doi-asserted-by": "crossref",
"first-page": "106698",
"journal-title": "Int. J. Surg.",
"key": "ref_8",
"volume": "103",
"year": "2022"
},
{
"DOI": "10.3390/v15010167",
"doi-asserted-by": "crossref",
"key": "ref_9",
"unstructured": "Chatterjee, S., Bhattacharya, M., Nag, S., Dhama, K., and Chakraborty, C. (2023). A Detailed Overview of SARS-CoV-2 Omicron: Its Sub-Variants, Mutations and Pathophysiology, Clinical Characteristics, Immunological Landscape, Immune Escape, and Therapies. Viruses, 15."
},
{
"DOI": "10.3389/fimmu.2023.1232965",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Pather, S., Madhi, S.A., Cowling, B.J., Moss, P., Kamil, J.P., Ciesek, S., Muik, A., and Türeci, Ö. (2023). SARS-CoV-2 Omicron variants: Burden of disease, impact on vaccine effectiveness and need for variant-adapted vaccines. Front. Immunol., 14."
},
{
"DOI": "10.1016/j.ijsu.2020.07.032",
"article-title": "A comparative overview of COVID-19, MERS and SARS: Review article",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Int. J. Surg.",
"key": "ref_11",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1186/s12879-022-07941-y",
"doi-asserted-by": "crossref",
"key": "ref_12",
"unstructured": "Anscombe, C., Lissauer, S., Thole, H., Rylance, J., Dula, D., Menyere, M., Kutambe, B., van der Veer, C., Phiri, T., and Banda, N.P. (2023). A comparison of four epidemic waves of COVID-19 in Malawi; an observational cohort study. BMC Infect. Dis., 23."
},
{
"DOI": "10.1093/cid/ciab721",
"article-title": "Clinical and Virological Features of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Variants of Concern: A Retrospective Cohort Study Comparing B.1.1.7 (Alpha), B.1.351 (Beta), and B.1.617.2 (Delta)",
"author": "Ong",
"doi-asserted-by": "crossref",
"first-page": "e1128",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_13",
"volume": "75",
"year": "2022"
},
{
"DOI": "10.3390/v15030618",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Seyler, L., Van Nedervelde, E., De Cock, D., Mann, C., Pien, K., Allard, S.D., and Demuyser, T. (2023). Surfing the Waves: Differences in Hospitalised COVID-19 Patients across 4 Variant Waves in a Belgian University Hospital. Viruses, 15."
},
{
"DOI": "10.3892/etm.2022.11343",
"article-title": "Clinical challenges of SARS-CoV-2 variants (Review)",
"author": "Cojocaru",
"doi-asserted-by": "crossref",
"first-page": "416",
"journal-title": "Exp. Ther. Med.",
"key": "ref_15",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1038/d41586-021-03552-w",
"article-title": "Heavily mutated Omicron variant puts scientists on alert",
"author": "Callaway",
"doi-asserted-by": "crossref",
"first-page": "21",
"journal-title": "Nature",
"key": "ref_16",
"volume": "600",
"year": "2021"
},
{
"DOI": "10.1016/j.jiph.2022.11.024",
"article-title": "Global emerging Omicron variant of SARS-CoV-2: Impacts, challenges and strategies",
"author": "Dhama",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "J. Infect. Public Health",
"key": "ref_17",
"volume": "16",
"year": "2023"
},
{
"DOI": "10.1093/cid/ciac885",
"article-title": "Omicron Subvariants: Clinical, Laboratory, and Cell Culture Characterization",
"author": "Morris",
"doi-asserted-by": "crossref",
"first-page": "1276",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_18",
"volume": "76",
"year": "2023"
},
{
"DOI": "10.1186/s12879-024-09084-8",
"doi-asserted-by": "crossref",
"key": "ref_19",
"unstructured": "Wang, Y., Yu, G., Shi, J., Zhang, X., Huo, J., Li, M., Chen, J., Yu, L., Li, Y., and Han, Z. (2024). Retrospective study about clinical severity and epidemiological analysis of the COVID-19 Omicron subvariant lineage-infected patients in Hohhot, China. BMC Infect. Dis., 24."
},
{
"DOI": "10.3390/v16030454",
"doi-asserted-by": "crossref",
"key": "ref_20",
"unstructured": "Goller, K.V., Ziemann, J., Kohler, C., Becker, K., Hübner, N.-O., and on behalf of the CoMV-Gen Study Group (2024). Clinical Manifestations of Infections with the Omicron Sub-Lineages BA.1, BA.2, and BA.5: A Retrospective Follow-Up Analysis of Public Health Data from Mecklenburg-Western Pomerania, Germany. Viruses, 16."
},
{
"DOI": "10.3390/vaccines12050466",
"doi-asserted-by": "crossref",
"key": "ref_21",
"unstructured": "De Rioja, V.L., Basile, L., Perramon-Malavez, A., Martínez-Solanas, É., López, D., Medina Maestro, S., Coma, E., Fina, F., Prats, C., and Mendioroz Peña, J. (2024). Severity of Omicron Subvariants and Vaccine Impact in Catalonia, Spain. Vaccines, 12."
},
{
"DOI": "10.3390/jcm12175572",
"doi-asserted-by": "crossref",
"key": "ref_22",
"unstructured": "Flisiak, R., Zarębska-Michaluk, D., Dobrowolska, K., Rorat, M., Rogalska, M., Kryńska, J.A., Moniuszko-Malinowska, A., Czupryna, P., Kozielewicz, D., and Jaroszewicz, J. (2023). Change in the Clinical Picture of Hospitalized Patients with COVID-19 between the Early and Late Period of Dominance of the Omicron SARS-CoV-2 Variant. J. Clin. Med., 12."
},
{
"DOI": "10.3390/brainsci12111531",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "Pavel, B., Moroti, R., Spataru, A., Popescu, M.R., Panaitescu, A.M., and Zagrean, A.-M. (2022). Neurological Manifestations of SARS-CoV2 Infection: A Narrative Review. Brain Sci., 12."
},
{
"DOI": "10.1016/j.mib.2024.102474",
"doi-asserted-by": "crossref",
"key": "ref_24",
"unstructured": "Jagst, M., Pottkämper, L., Gömer, A., Pitarokoili, K., and Steinmann, E. (2024). Neuroinvasion and neurotropism of severe acute respiratory syndrome coronavirus 2 infection. Curr. Opin. Microbiol., 79."
},
{
"DOI": "10.1016/S1474-4422(20)30221-0",
"article-title": "Neurological associations of COVID-19",
"author": "Ellul",
"doi-asserted-by": "crossref",
"first-page": "767",
"journal-title": "Lancet Neurol.",
"key": "ref_25",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1007/s43440-022-00424-6",
"article-title": "Neurological consequences of COVID-19",
"author": "Brola",
"doi-asserted-by": "crossref",
"first-page": "1208",
"journal-title": "Pharmacol. Rep.",
"key": "ref_26",
"volume": "74",
"year": "2022"
},
{
"DOI": "10.1177/10738584211015136",
"article-title": "Unravelling Pathophysiology of Neurological and Psychiatric Complications of COVID-19 Using Brain Organoids",
"author": "Ng",
"doi-asserted-by": "crossref",
"first-page": "30",
"journal-title": "Neuroscientist",
"key": "ref_27",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.3389/fneur.2023.1207883",
"doi-asserted-by": "crossref",
"key": "ref_28",
"unstructured": "Xue, H., Zeng, L., He, H., Xu, D., and Ren, K. (2023). Autoimmune encephalitis in COVID-19 patients: A systematic review of case reports and case series. Front. Neurol., 14."
},
{
"DOI": "10.1016/j.tins.2022.02.006",
"article-title": "The neuroinvasiveness, neurotropism, and neurovirulence of SARS-CoV-2",
"author": "Bauer",
"doi-asserted-by": "crossref",
"first-page": "358",
"journal-title": "Trends Neurosci.",
"key": "ref_29",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.1128/mbio.02920-22",
"doi-asserted-by": "crossref",
"key": "ref_30",
"unstructured": "Bauer, L., and van Riel, D. (2023). Do SARS-CoV-2 Variants Differ in Their Neuropathogenicity?. mBio, 14."
},
{
"DOI": "10.3390/brainsci13081137",
"doi-asserted-by": "crossref",
"key": "ref_31",
"unstructured": "Forero, K., Buqaileh, R., Sunderman, C., and AbouAlaiwi, W. (2023). COVID-19 and Neurological Manifestations. Brain Sci., 13."
},
{
"DOI": "10.1002/jmv.29357",
"article-title": "Differential pathogenic and molecular features in neurological infection of SARS-CoV-2 Omicron BA.5.2 and BA.2.75 and Delta",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "e29357",
"journal-title": "J. Med. Virol.",
"key": "ref_32",
"volume": "96",
"year": "2024"
},
{
"DOI": "10.1002/jmv.28628",
"article-title": "The diversity in the clinical features of children hospitalized with COVID-19 during the nonvariant, Alpha (B.1.1.7), Delta (B.1.617.2), and Omicron (B.1.1.529) variant periods of SARS CoV-2: Caution for neurological symptoms in Omicron variant",
"author": "Sahin",
"doi-asserted-by": "crossref",
"first-page": "e28628",
"journal-title": "J. Med. Virol.",
"key": "ref_33",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.1016/j.braindev.2022.06.010",
"article-title": "Severe encephalopathy associated with SARS-CoV-2 Omicron BA.1 variant infection in a neonate",
"author": "Tetsuhara",
"doi-asserted-by": "crossref",
"first-page": "743",
"journal-title": "Brain Dev.",
"key": "ref_34",
"volume": "44",
"year": "2022"
},
{
"article-title": "COVID-19 neurological manifestations—The experience of a tertiary hospital from Northeastern Romania",
"author": "Diaconu",
"first-page": "21",
"journal-title": "Med. Surg. J. Rev. Med. Chir. Soc. Med. Nat. Iaşi.",
"key": "ref_35",
"volume": "128",
"year": "2024"
},
{
"DOI": "10.4103/aian.aian_1048_21",
"article-title": "Comparison of Neurological Manifestations in the Two Waves of COVID-19 Infection: A Cross-Sectional Study",
"author": "Sureshbabu",
"doi-asserted-by": "crossref",
"first-page": "864",
"journal-title": "Ann. Indian Acad. Neurol.",
"key": "ref_36",
"volume": "25",
"year": "2022"
},
{
"DOI": "10.4103/aian.aian_204_22",
"article-title": "Neurological Manifestations in COVID-19 in Three Waves of the Pandemic: An Inpatient Study from India",
"author": "Kulkarni",
"doi-asserted-by": "crossref",
"first-page": "1047",
"journal-title": "Ann. Indian Acad. Neurol.",
"key": "ref_37",
"volume": "25",
"year": "2022"
},
{
"DOI": "10.3390/jcm13123477",
"doi-asserted-by": "crossref",
"key": "ref_38",
"unstructured": "Jachman-Kapułka, J., Zińczuk, A., Szymański, W., Simon, K., and Rorat, M. (2024). Complexity and Diversity of the Neurological Spectrum of SARS-CoV-2 over Three Waves of COVID-19. J. Clin. Med., 13."
},
{
"key": "ref_39",
"unstructured": "(2024, October 27). Genomic Epidemiology of SARS-CoV-2 with Subsampling Focused on Poland Since Pandemic Start. Available online: https://covariants.org/per-country?country=Poland."
},
{
"DOI": "10.1111/ene.16096",
"article-title": "Neurological complications during the Omicron COVID-19 wave in China: A cohort study",
"author": "Lu",
"doi-asserted-by": "crossref",
"first-page": "e16096",
"journal-title": "Eur. J. Neurol.",
"key": "ref_40",
"volume": "31",
"year": "2024"
},
{
"DOI": "10.1016/j.jiph.2022.12.005",
"article-title": "Neurological Manifestations of hospitalized patients with mild to moderate infection with SARS-CoV-2 Omicron variant in Shanghai, China",
"author": "Shen",
"doi-asserted-by": "crossref",
"first-page": "155",
"journal-title": "J. Infect. Public Health.",
"key": "ref_41",
"volume": "16",
"year": "2023"
},
{
"DOI": "10.3390/v14051020",
"doi-asserted-by": "crossref",
"key": "ref_42",
"unstructured": "Seehusen, F., Clark, J.J., Sharma, P., Bentley, E.G., Kirby, A., Subramaniam, K., Wunderlin-Giuliani, S., Hughes, G.L., Patterson, E.I., and Michael, B.D. (2022). Neuroinvasion and Neurotropism by SARS-CoV-2 Variants in the K18-hACE2 Mouse. Viruses, 14."
},
{
"DOI": "10.1038/s41598-023-29909-x",
"doi-asserted-by": "crossref",
"key": "ref_43",
"unstructured": "Yang, J.H., Yang, M.S., Kim, D.M., Kim, B., Tark, D., Kang, S.M., and Lee, G.H. (2023). Delta (B1.617.2) variant of SARS-CoV-2 induces severe neurotropic patterns in K18-hACE2 mice. Sci. Rep., 13."
},
{
"DOI": "10.1186/s12974-023-02861-3",
"article-title": "Differential effects of SARS-CoV-2 variants on central nervous system cells and blood-brain barrier functions",
"author": "Proust",
"doi-asserted-by": "crossref",
"first-page": "184",
"journal-title": "J. Neuroinflamm.",
"key": "ref_44",
"volume": "20",
"year": "2023"
},
{
"DOI": "10.1016/j.jmii.2023.10.005",
"article-title": "Clinical features and virologic lineages of COVID-19-associated encephalitis in Taiwanese children during early epidemic wave of omicron in 2022: Report from a medical center",
"author": "Chang",
"doi-asserted-by": "crossref",
"first-page": "48",
"journal-title": "J. Microbiol. Immunol. Infect.",
"key": "ref_45",
"volume": "57",
"year": "2024"
},
{
"DOI": "10.1016/j.pediatrneurol.2024.04.004",
"article-title": "Severe Neurological Manifestation Associated With Coronavirus Disease 2019 in Children During the Omicron Variant-Predominant Period",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "17",
"journal-title": "Pediatr. Neurol.",
"key": "ref_46",
"volume": "156",
"year": "2024"
},
{
"DOI": "10.1093/cid/ciad505",
"article-title": "Clinical Epidemiology and Risk Factors for Critical Outcomes Among Vaccinated and Unvaccinated Adults Hospitalized With COVID-19-VISION Network, 10 States, June 2021-March 2023",
"author": "Griggs",
"doi-asserted-by": "crossref",
"first-page": "338",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_47",
"volume": "78",
"year": "2024"
},
{
"DOI": "10.1016/j.diabres.2020.108293",
"article-title": "Risk factors for mortality among COVID-19 patients",
"author": "Albitar",
"doi-asserted-by": "crossref",
"first-page": "108293",
"journal-title": "Diabetes Res. Clin. Pract.",
"key": "ref_48",
"volume": "166",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2021.757459",
"doi-asserted-by": "crossref",
"key": "ref_49",
"unstructured": "Zhang, H., Wu, Y., He, Y., Liu, X., Liu, M., Tang, Y., Li, X., Yang, G., Liang, G., and Xu, S. (2022). Age-Related Risk Factors and Complications of Patients With COVID-19: A Population-Based Retrospective Study. Front. Med., 8."
},
{
"DOI": "10.2807/1560-7917.ES.2024.29.28.2300697",
"article-title": "The impact of the COVID-19 vaccination programme on symptomatic and severe SARS-CoV-2 infection during a period of Omicron variant dominance in Ireland, December 2021 to March 2023",
"author": "Marron",
"doi-asserted-by": "crossref",
"first-page": "2300697",
"journal-title": "Euro Surveill",
"key": "ref_50",
"volume": "29",
"year": "2024"
},
{
"DOI": "10.1038/s41586-022-04980-y",
"article-title": "BA.2.12.1, BA.4 and BA.5 escape antibodies elicited by Omicron infection",
"author": "Cao",
"doi-asserted-by": "crossref",
"first-page": "593",
"journal-title": "Nature",
"key": "ref_51",
"volume": "608",
"year": "2022"
},
{
"DOI": "10.3390/brainsci12020193",
"doi-asserted-by": "crossref",
"key": "ref_52",
"unstructured": "Drabik, L., Derbisz, J., Chatys-Bogacka, Z., Mazurkiewicz, I., Sawczynska, K., Kesek, T., Czepiel, J., Wrona, P., Szaleniec, J., and Wojcik-Bugajska, M. (2022). Neurological Prognostic Factors in Hospitalized Patients with COVID-19. Brain Sci., 12."
},
{
"DOI": "10.5603/PJNNS.a2021.0039",
"article-title": "Neurological symptoms in hospitalised patients with COVID-19 and their association with in-hospital mortality",
"author": "Wnuk",
"doi-asserted-by": "crossref",
"first-page": "314",
"journal-title": "Neurol. Neurochir. Pol.",
"key": "ref_53",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.12688/f1000research.42308.1",
"article-title": "Hemorrhagic and ischemic stroke in patients with coronavirus disease 2019: Incidence, risk factors, and pathogenesis—A systematic review and meta-analysis",
"author": "Syahrul",
"doi-asserted-by": "crossref",
"first-page": "34",
"journal-title": "F1000Research",
"key": "ref_54",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1111/ane.13471",
"article-title": "Association of consciousness impairment and mortality in people with COVID-19",
"author": "Xiong",
"doi-asserted-by": "crossref",
"first-page": "251",
"journal-title": "Acta Neurol. Scand.",
"key": "ref_55",
"volume": "144",
"year": "2021"
},
{
"DOI": "10.3390/brainsci12010074",
"doi-asserted-by": "crossref",
"key": "ref_56",
"unstructured": "Mekkawy, D.A., Hamdy, S., Abdel-Naseer, M., Shehata, H.S., Halfawy, A.A., Shalaby, N.M., Shehata, G.A., Ali, A.M., Elmazny, A., and Ahmed, S.M. (2022). Neurological Manifestations in a Cohort of Egyptian Patients with COVID-19: A Prospective, Multicenter, Observational Study. Brain Sci., 12."
},
{
"DOI": "10.3390/diagnostics12020544",
"doi-asserted-by": "crossref",
"key": "ref_57",
"unstructured": "Di Giorgio, A., Mirijello, A., De Gennaro, C., Fontana, A., Alboini, P.E., Florio, L., Inchingolo, V., Zarrelli, M., Miscio, G., and Raggi, P. (2022). Factors Associated with Delirium in COVID-19 Patients and Their Outcome: A Single-Center Cohort Study. Diagnostics, 12."
},
{
"DOI": "10.1016/j.jpsychores.2020.110350",
"article-title": "A rapid review of the pathoetiology, presentation, and management of delirium in adults with COVID-19",
"author": "Hawkins",
"doi-asserted-by": "crossref",
"first-page": "110350",
"journal-title": "J. Psychosom. Res.",
"key": "ref_58",
"volume": "141",
"year": "2021"
},
{
"DOI": "10.21037/apm-20-2557",
"article-title": "Risk factors for mortality of coronavirus disease 2019 (COVID-19) patients during the early outbreak of COVID-19: A systematic review and meta-analysis",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "5069",
"journal-title": "Ann. Palliat. Med.",
"key": "ref_59",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1186/s12883-021-02152-5",
"doi-asserted-by": "crossref",
"key": "ref_60",
"unstructured": "Amanat, M., Rezaei, N., Roozbeh, M., Shojaei, M., Tafakhori, A., Zoghi, A., Darazam, I.A., Salehi, M., Karimialavijeh, E., and Lima, B.S. (2021). Neurological manifestations as the predictors of severity and mortality in hospitalized individuals with COVID-19: A multicenter prospective clinical study. BMC Neurol., 21."
},
{
"DOI": "10.1101/2021.03.10.21253280",
"doi-asserted-by": "crossref",
"key": "ref_61",
"unstructured": "Shapiro, R., Gallardo, V.J., Caronna, E., and Pozo-Rosich, P. (2021). The impact of headache disorders on COVID-19 survival: A world population-based analysis. medRxiv."
},
{
"DOI": "10.1177/0333102420965157",
"article-title": "Headache: A striking prodromal and persistent symptom, predictive of COVID-19 clinical evolution",
"author": "Caronna",
"doi-asserted-by": "crossref",
"first-page": "1410",
"journal-title": "Cephalalgia",
"key": "ref_62",
"volume": "40",
"year": "2020"
}
],
"reference-count": 62,
"references-count": 62,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2076-3425/14/11/1161"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Cross-Section of Neurological Manifestations Among SARS-CoV-2 Omicron Subvariants—Single-Center Study",
"type": "journal-article",
"volume": "14"
}