Efficacy and safety of ultra-short wave diathermy on COVID-19 pneumonia: a pioneering study
et al., Frontiers in Medicine, doi:10.3389/fmed.2023.1149250, ChiCTR2000029972, Feb 2021 (preprint)
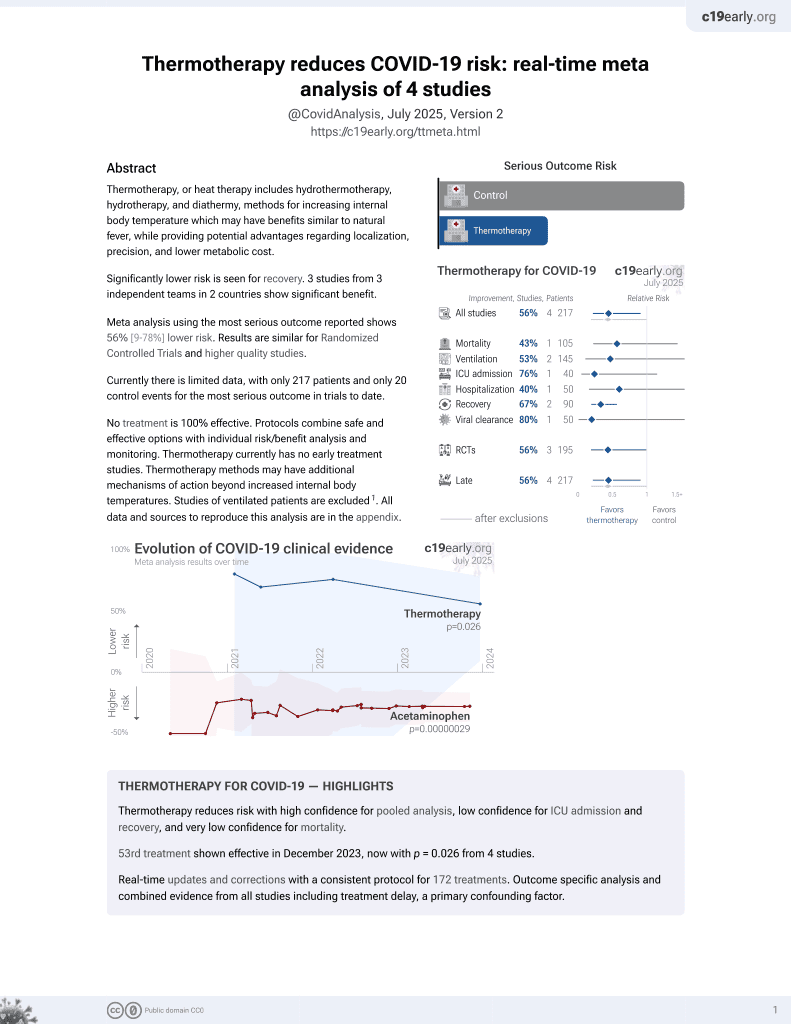
54th treatment shown to reduce risk in
December 2023, now with p = 0.026 from 4 studies.
Lower risk for recovery.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
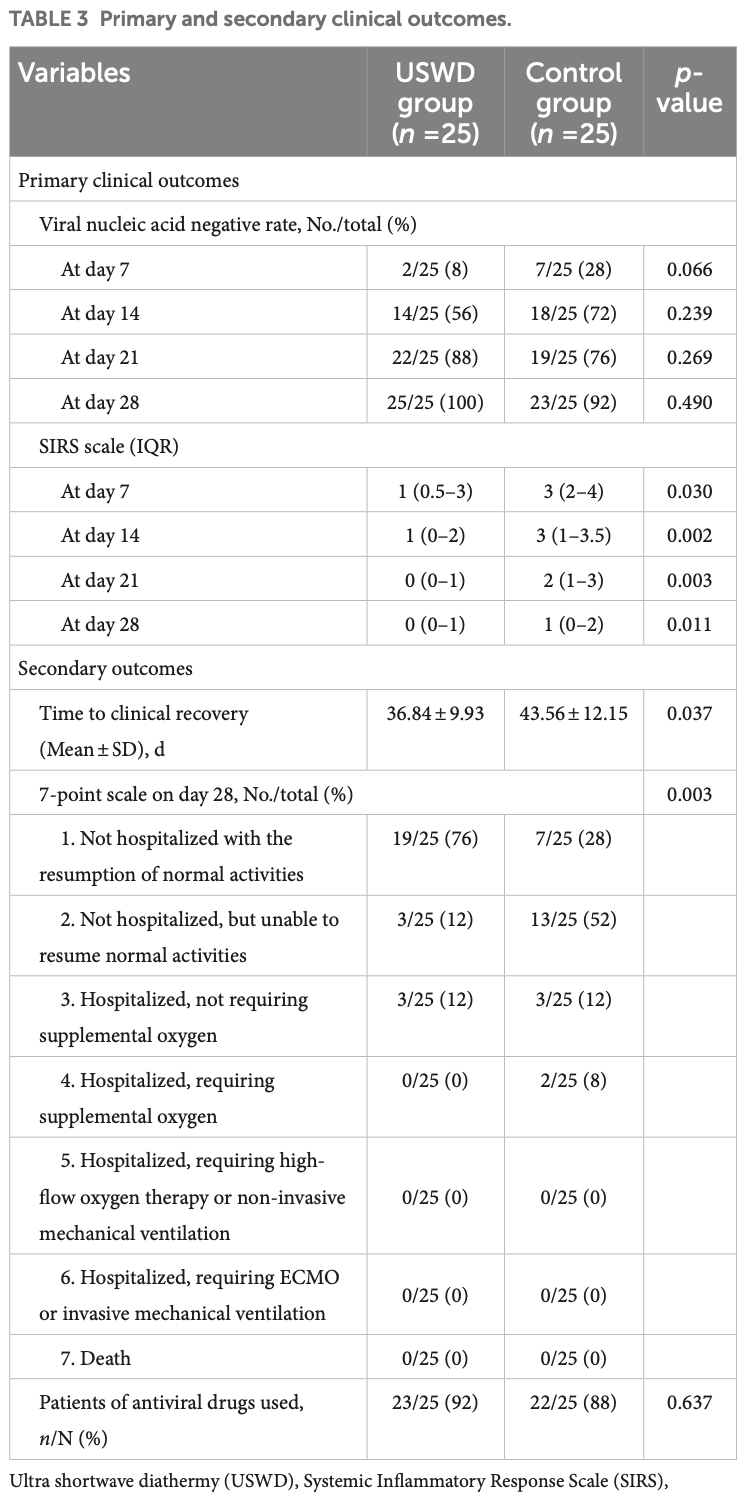
RCT 50 hospitalized COVID-19 pneumonia patients showing faster recovery with ultra-short wave diathermy (USWD). The USWD group received standard treatment plus USWD applied to the chest for 10 minutes twice daily for 12 days. The USWD group had significantly faster clinical recovery by 6.7 days, lower systemic inflammation, and better outcomes on the 7-point clinical status scale on days 21 and 28 compared to the control group receiving only standard treatment. There was no significant difference in SARS-CoV-2 viral clearance. Pulmonary fibrosis observed prior to treatment was recovered in most patients in both groups, alleviating concerns over potential harms of USWD.
Baseline severe cases were more common in the treatment group, 52 vs. 28%.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
|
risk of oxygen therapy, 80.0% lower, RR 0.20, p = 0.49, treatment 0 of 25 (0.0%), control 2 of 25 (8.0%), NNT 12, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), day 28.
|
|
risk of hospitalization, 40.0% lower, RR 0.60, p = 0.70, treatment 3 of 25 (12.0%), control 5 of 25 (20.0%), NNT 12, day 28.
|
|
clinical scale >1, 66.7% lower, RR 0.33, p = 0.002, treatment 6 of 25 (24.0%), control 18 of 25 (72.0%), NNT 2.1, day 28.
|
|
recovery time, 15.4% lower, relative time 0.85, p = 0.04, treatment 25, control 25.
|
|
SIRS, 66.7% lower, RR 0.33, p = 0.03, treatment 25, control 25, inverted to make RR<1 favor treatment, day 7.
|
|
SIRS, 66.7% lower, RR 0.33, p = 0.002, treatment 25, control 25, inverted to make RR<1 favor treatment, day 14.
|
|
risk of no viral clearance, 80.0% lower, RR 0.20, p = 0.49, treatment 0 of 25 (0.0%), control 2 of 25 (8.0%), NNT 12, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), day 28.
|
|
risk of no viral clearance, 50.0% lower, RR 0.50, p = 0.46, treatment 3 of 25 (12.0%), control 6 of 25 (24.0%), NNT 8.3, day 21.
|
|
risk of no viral clearance, 57.1% higher, RR 1.57, p = 0.38, treatment 11 of 25 (44.0%), control 7 of 25 (28.0%), day 14.
|
|
risk of no viral clearance, 27.8% higher, RR 1.28, p = 0.14, treatment 23 of 25 (92.0%), control 18 of 25 (72.0%), day 7.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Huang et al., 1 Feb 2021, Randomized Controlled Trial, China, peer-reviewed, 8 authors, study period 18 February, 2020 - 20 April, 2020, diathermy, trial ChiCTR2000029972.
Contact: chenhong1129@hotmail.com, chenhong1129@hust.edu.cn.
Efficacy and safety of ultra-short wave diathermy on COVID-19 pneumonia: a pioneering study
Frontiers in Medicine, doi:10.3389/fmed.2023.1149250
Background: The ultra-short wave diathermy (USWD) is widely used to ameliorate inflammation of bacterial pneumonia, however, for COVID-19 pneumonia, USWD still needs to be verified. This study aimed to investigate the efficacy and safety of USWD in COVID-19 pneumonia patients. Methods: This was a single-center, evaluator-blinded, randomized controlled trial. Moderate and severe COVID-19 patients were recruited between 18 February and 20 April 2020. Participants were randomly allocated to receive USWD + standard medical treatment (USWD group) or standard medical treatment alone (control group). The negative conversion rate of SARS-CoV-2 and Systemic Inflammatory Response Scale (SIRS) on days 7, 14, 21, and 28 were assessed as primary outcomes. Secondary outcomes included time to clinical recovery, the 7-point ordinal scale, and adverse events. Results: Fifty patients were randomized (USWD, 25; control, 25), which included 22 males (44.0%) and 28 females (56.0%) with a mean (SD) age of 53 ± 10.69. The rates of SARS-CoV-2 negative conversion on day 7 (p = 0.066), day 14 (p = 0.239), day 21 (p = 0.269), and day 28 (p = 0.490) were insignificant. However, systemic inflammation by SIRS was ameliorated with significance on day 7 (p = 0.030), day 14 (p = 0.002), day 21 (p = 0.003), and day 28 (p = 0.011). Time to clinical recovery (USWD 36.84 ± 9.93 vs. control 43.56 ± 12.15, p = 0.037) was significantly shortened with a between-group difference of 6.72 ± 3.14 days. 7-point ordinal scale on days 21 and 28 showed significance (p = 0.002, 0.003), whereas the difference on days 7 and 14 was insignificant (p = 0.524, 0.108). In addition, artificial intelligenceassisted CT analysis showed a greater decrease in the infection volume in the USWD group, without significant between-group differences. No treatmentassociated adverse events or worsening of pulmonary fibrosis were observed in either group. Conclusion: Among patients with moderate and severe COVID-19 pneumonia, USWD added to standard medical treatment could ameliorate systemic inflammation and shorten the duration of hospitalization without causing any adverse effects.
Ethics statement The studies involving human participants were reviewed and approved by The ethics committee of the Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China (certificate of approval number: TJ-C20200127). The patients/participants provided their written informed consent to participate in this study.
Author contributions HC contributed to the supervision, drafting, and finalizing of the study. LH, QL, and SS equally contributed to compiling and describing the results. Moreover, authors LH and QL contributed to designing the CRF, medical history forms development, data collection, and interpretation. SS and MN contributed to writing and formatting the manuscript. LX designed the USWD treatment protocol, while BC did the CT scan analysis. IA contributed to data analysis. All authors contributed to the article and approved the submitted version.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary..
References
Bedford, Enria, Giesecke, Heymann, Ihekweazu et al., COVID-19: towards controlling of a pandemic, Lancet, doi:10.1016/S0140-6736(20)30673-5
Cucinotta, Vanelli, WHO declares COVID-19 a pandemic, Acta Biomed, doi:10.23750/abm.v91i1.9397
Dantas, Barreto, Ferreira, Digital physical therapy in the COVID-19 pandemic, Braz J Phys Ther, doi:10.1016/j.bjpt.2020.04.006
Du, Nan, Lv, Ye, Lv et al., Benefits of adjuvant therapy with transcutaneous ion introduction of traditional Chinese medicine by using microcomputer control intermediate frequency stimulator and ultrashort wave therapy on 112 cases of infantile pneumonia, Chin J Gen Pract, doi:10.16766/j.cnki.issn.1674-4152.2012.08.063
Goats, Continuous short-wave (radio-frequency) diathermy, Br J Sports Med, doi:10.1136/bjsm.23.2.123
Gorbunov, Vinnikov, Strelkova, Krupennikov, The use of pulsed and continuous UHF electrical fields in the rehabilitation of patients with the Guillain-Barre syndrome and other peripheral myelinopathies, Zh Nevrol Psikhiatr Im S S Korsakova
He, Ruan, Chang, Zhu, Changes of serum cytokines in children with bronchopneumonia treated with ultrashort wave diathermy, J Appl Clin Pediatr, doi:10.3760/cma.j.issn.0254-1424.2003.06.005
Hill, Lewis, Mills, Kielty, Pulsed short-wave diathermy effects on human fibroblast proliferation, Arch Phys Med Rehabil, doi:10.1053/apmr.2002.32823
Hu, Fu, Xue, Association of the proliferation of lung fibroblasts with the ERK1/2 signaling pathway in neonatal rats with hyperoxia-induced lung fibrosis, Exp Ther Med, doi:10.3892/etm.2018.6999
Hu, Luo, Yang, Xiang, The effect of ultrashort wave adjuvant therapy on adult mycoplasma pneumoniae pneumonia and serum cytokines, Chin J Phys Med Rehabil, doi:10.3760/cma.j.issn.0254-1424.2012.01.020
Huang, Han, Ai, Yu, Kang et al., Serial quantitative chest CT assessment of COVID-19: a deep learning approach, Radiol Cardiothorac Imaging, doi:10.1148/ryct.2020200075
Huang, Zhang, Zhou, Liu, Wang et al., Effect of radial extracorporeal shock wave combined with ultrashort wave diathermy on fibrosis and contracture of muscle, Am J Phys Med Rehabil, doi:10.1097/PHM.0000000000001599
Lamina, Hanif, Gagarawa, Short wave diathermy in the symptomatic management of chronic pelvic inflammatory disease pain: a randomized controlled trial, Physiother Res Int, doi:10.1002/pri.473
Laufer, Zilberman, Porat, Nahir, Effect of pulsed short-wave diathermy on pain and function of subjects with osteoarthritis of the knee: a placebo-controlled double-blind clinical trial, Clin Rehabil, doi:10.1191/0269215505cr864oa
Lazzeri, Lanza, Bellini, Bellofiore, Cecchetto et al., Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a position paper of the Italian Association of Respiratory Physiotherapists (ARIR), Monaldi Arch Chest Dis, doi:10.4081/monaldi.2020.1285
Li, Guan, Wu, Wang, Zhou et al., Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia, N Engl J Med, doi:10.1056/NEJMoa2001316
Li, Qu, Yang, Liu, Wang et al., Effects of ultrashort wave therapy on inflammation and macrophage polarization after acute lung injury in rats, Bioelectromagnetics, doi:10.1002/bem.22353
Luo, Yuan, Wu, Tan, Effect of ultrashort wave in the treatment of children with Mycoplasma pneumonia and serum inflammatory factors, Chin J Phys Med Rehabil, doi:10.3760/cma.j.issn.0254-1424.2020.06.019
Ma, Li, Liu, Short wave diathermy for small spontaneous pneumothorax, Thorax, doi:10.1136/thx.52.6.561
Ma, Shang, Effect of ultrashort wave and magnetic therapy on serum inflammatory factors in children with bronchial pneumonia, Chin J Phys Med Rehabil, doi:10.3760/cma.j.issn.0254-1424.2018.07.010
Martin, Erickson, Medical diathermy, J Am Med Assoc, doi:10.1001/jama.1950.72910190003007
Na, Wang, Liu, Zhang, Ultrashort wave combined with human umbilical cord mesenchymal stem cell (HUC-MSC) transplantation inhibits NLRP3 inflammasome and improves spinal cord injury via MK2/TTP signalling pathway, Biomed Res Int, doi:10.1155/2020/3021750
Olaiz-Fernandez, Vicuna, Diaz-Ramirez, Fajardo, Bautista-Carbajal et al., Effect of omicron on the prevalence of COVID-19 in TABLE 5 The laboratory values and complications in USWD and control groups, doi:10.1016/j.tmaid.2022.102361
Paterson, The treatment of nasal sinus infection by ultra-short wave diathermy, Can Med Assoc J
Peeri, Shrestha, Rahman, Zaki, Tan et al., The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned?, Int J Epidemiol, doi:10.1093/ije/dyaa033
Pekarek, Treatment of peptic ulcer by ultra-short-wave diathermy, Br J Phys Med
Rost, Schlink, Uneven field in ultra-short-wave diathermy: its application for sinusitis, Br J Phys Med, doi:10.1080/00218469408026647
Shah, Nasb, Lu, Huang, Wang et al., Scaling the need, benefits, and risks associated with COVID-19 acute and postacute care rehabilitation: a review, Rehabil Res Pract, doi:10.1155/2020/3642143
Shields, Gormley, Hare, Short-wave diathermy: current clinical and safety practices, Physiother Res Int, doi:10.1002/pri.259
Shields, Hare, Boyle, Gormley, Development and application of a quality control procedure for short-wave diathermy units, Med Biol Eng Comput, doi:10.1007/BF02343540
Strzelecki, The second worldwide wave of interest in coronavirus since the COVID-19 outbreaks in South Korea, Italy and Iran: a Google trends study, Brain Behav Immun, doi:10.1016/j.bbi.2020.04.042
Thomas, Baldwin, Bissett, Boden, Gosselink et al., Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations, J Physiother, doi:10.1016/j.jphys.2020.03.011
Vardhanabhuti, CT scan AI-aided triage for patients with COVID-19 in China, Lancet Digit Health, doi:10.1016/S2589-7500(20)30222-3
Vardiman, Moodie, Siedlik, Kudrna, Graham et al., Shortwave diathermy pretreatment and inflammatory myokine response after high-intensity eccentric exercise, J Athl Train, doi:10.4085/1062-6050-50.1.12
Wang, Jia, Cao, Feng, Na et al., HUCMSCs transplantation combined with ultrashort wave therapy attenuates neuroinflammation in spinal cord injury through NUR77/NF-kappaB pathway, Life Sci, doi:10.1016/j.lfs.2020.118958
Wang, Xia, Huang, Xu, Qin et al., Deep learning-based triage and analysis of lesion burden for COVID-19: a retrospective study with external validation, Lancet Digit Health, doi:10.1016/S2589-7500(20)30199-0
Welliver, Temperature, humidity, and ultraviolet B radiation predict community respiratory syncytial virus activity, Pediatr Infect Dis J, doi:10.1097/INF.0b013e318157da59
Yang, Effects of ultra-short wave diathermy on chronic pneumonia in children, Chin Med J
Yang, Yang, Pulmonary rehabilitation for patients with coronavirus disease 2019 (COVID-19), Chronic Dis Transl Med, doi:10.1016/j.cdtm.2020.05.002
Ye, Chen, Wang, Shen, Short-wave therapy for spontaneous pneumothorax: a case report, Bioelectromagnetics, doi:10.1002/bem.22013
Yu, Jones, Dean, Liisa, Ultra-shortwave diathermy -a new purported treatment for management of patients with COVID-19, Physiother Theory Pract, doi:10.1080/09593985.2020.1757264
Zhang, Zheng, Liu, Zhao, Fu et al., Application of ultrashort wave diathermy in treatment of severe acute respiratory syndrome, Chin J Rehabil Med Rehabil, doi:10.3760/cma.j.issn.0254-1424.2003.06.005
Zhang, Zhou, Zhong, Liu, Effect of stretching combined with ultrashort wave diathermy on joint function and its possible mechanism in a rabbit knee contracture model, Am J Phys Med Rehabil, doi:10.1097/PHM.0000000000000873
Zhou, Jiang, Yang, Effect of Ultrashortwave diathermy on experimental pulmonary interstitial fibrosis, Chin J Phys Med Rehabil, doi:10.3760/cma.j.issn.0254-1424.2002.09.007
Zhu, Sun, Zhao, Li, Effect of ultrashort wave and medications on pulmonary function of pneumonia patients, Chin J Phys Ther, doi:10.1016/B978-008043005-8/50012-3
DOI record:
{
"DOI": "10.3389/fmed.2023.1149250",
"ISSN": [
"2296-858X"
],
"URL": "http://dx.doi.org/10.3389/fmed.2023.1149250",
"abstract": "<jats:sec><jats:title>Background</jats:title><jats:p>The ultra-short wave diathermy (USWD) is widely used to ameliorate inflammation of bacterial pneumonia, however, for COVID-19 pneumonia, USWD still needs to be verified. This study aimed to investigate the efficacy and safety of USWD in COVID-19 pneumonia patients.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>This was a single-center, evaluator-blinded, randomized controlled trial. Moderate and severe COVID-19 patients were recruited between 18 February and 20 April 2020. Participants were randomly allocated to receive USWD + standard medical treatment (USWD group) or standard medical treatment alone (control group). The negative conversion rate of SARS-CoV-2 and Systemic Inflammatory Response Scale (SIRS) on days 7, 14, 21, and 28 were assessed as primary outcomes. Secondary outcomes included time to clinical recovery, the 7-point ordinal scale, and adverse events.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Fifty patients were randomized (USWD, 25; control, 25), which included 22 males (44.0%) and 28 females (56.0%) with a mean (SD) age of 53 ± 10.69. The rates of SARS-CoV-2 negative conversion on day 7 (<jats:italic>p</jats:italic> = 0.066), day 14 (<jats:italic>p</jats:italic> = 0.239), day 21 (<jats:italic>p</jats:italic> = 0.269), and day 28 (<jats:italic>p</jats:italic> = 0.490) were insignificant. However, systemic inflammation by SIRS was ameliorated with significance on day 7 (<jats:italic>p</jats:italic> = 0.030), day 14 (<jats:italic>p</jats:italic> = 0.002), day 21 (<jats:italic>p</jats:italic> = 0.003), and day 28 (<jats:italic>p</jats:italic> = 0.011). Time to clinical recovery (USWD 36.84 ± 9.93 vs. control 43.56 ± 12.15, <jats:italic>p</jats:italic> = 0.037) was significantly shortened with a between-group difference of 6.72 ± 3.14 days. 7-point ordinal scale on days 21 and 28 showed significance (<jats:italic>p</jats:italic> = 0.002, 0.003), whereas the difference on days 7 and 14 was insignificant (<jats:italic>p</jats:italic> = 0.524, 0.108). In addition, artificial intelligence-assisted CT analysis showed a greater decrease in the infection volume in the USWD group, without significant between-group differences. No treatment-associated adverse events or worsening of pulmonary fibrosis were observed in either group.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>Among patients with moderate and severe COVID-19 pneumonia, USWD added to standard medical treatment could ameliorate systemic inflammation and shorten the duration of hospitalization without causing any adverse effects.</jats:p><jats:p><jats:bold>Clinical Trial Registration</jats:bold>: <jats:ext-link>chictr.org.cn</jats:ext-link>, identifier ChiCTR2000029972.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fmed.2023.1149250"
],
"author": [
{
"affiliation": [],
"family": "Huang",
"given": "Liangjiang",
"sequence": "first"
},
{
"affiliation": [],
"family": "Li",
"given": "Qian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shah",
"given": "Sayed Zulfiqar Ali",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nasb",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ali",
"given": "Iftikhar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Bin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xie",
"given": "Lingfeng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Hong",
"sequence": "additional"
}
],
"container-title": "Frontiers in Medicine",
"container-title-short": "Front. Med.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2023,
6,
5
]
],
"date-time": "2023-06-05T05:22:26Z",
"timestamp": 1685942546000
},
"deposited": {
"date-parts": [
[
2023,
6,
5
]
],
"date-time": "2023-06-05T05:22:36Z",
"timestamp": 1685942556000
},
"indexed": {
"date-parts": [
[
2023,
12,
22
]
],
"date-time": "2023-12-22T05:25:29Z",
"timestamp": 1703222729477
},
"is-referenced-by-count": 2,
"issued": {
"date-parts": [
[
2023,
6,
5
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
5
]
],
"date-time": "2023-06-05T00:00:00Z",
"timestamp": 1685923200000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2023.1149250/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2023,
6,
5
]
]
},
"published-online": {
"date-parts": [
[
2023,
6,
5
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.23750/abm.v91i1.9397",
"article-title": "WHO declares COVID-19 a pandemic",
"author": "Cucinotta",
"doi-asserted-by": "publisher",
"first-page": "157",
"journal-title": "Acta Biomed",
"key": "ref1",
"volume": "91",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2001316",
"article-title": "Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "1199",
"journal-title": "N Engl J Med",
"key": "ref2",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30673-5",
"article-title": "COVID-19: towards controlling of a pandemic",
"author": "Bedford",
"doi-asserted-by": "publisher",
"first-page": "1015",
"journal-title": "Lancet",
"key": "ref3",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1093/ije/dyaa033",
"article-title": "The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned?",
"author": "Peeri",
"doi-asserted-by": "publisher",
"first-page": "717",
"journal-title": "Int J Epidemiol",
"key": "ref4",
"volume": "49",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2020.04.042",
"article-title": "The second worldwide wave of interest in coronavirus since the COVID-19 outbreaks in South Korea, Italy and Iran: a Google trends study",
"author": "Strzelecki",
"doi-asserted-by": "publisher",
"first-page": "950",
"journal-title": "Brain Behav Immun",
"key": "ref5",
"volume": "88",
"year": "2020"
},
{
"DOI": "10.1016/j.tmaid.2022.102361",
"article-title": "Effect of omicron on the prevalence of COVID-19 in international travelers at the Mexico city international airport. December 16th, 2021 to January 31st, 2022",
"author": "Olaiz-Fernandez",
"doi-asserted-by": "publisher",
"first-page": "102361",
"journal-title": "Travel Med Infect Dis",
"key": "ref6",
"volume": "49",
"year": "2022"
},
{
"DOI": "10.1016/j.cdtm.2020.05.002",
"article-title": "Pulmonary rehabilitation for patients with coronavirus disease 2019 (COVID-19)",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "79",
"journal-title": "Chronic Dis Transl Med",
"key": "ref7",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1016/j.jphys.2020.03.011",
"article-title": "Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations",
"author": "Thomas",
"doi-asserted-by": "publisher",
"first-page": "73",
"journal-title": "J Physiother",
"key": "ref8",
"volume": "66",
"year": "2020"
},
{
"DOI": "10.4081/monaldi.2020.1285",
"article-title": "Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a position paper of the Italian Association of Respiratory Physiotherapists (ARIR)",
"author": "Lazzeri",
"doi-asserted-by": "publisher",
"first-page": "163",
"journal-title": "Monaldi Arch Chest Dis",
"key": "ref9",
"volume": "90",
"year": "2020"
},
{
"DOI": "10.1016/j.bjpt.2020.04.006",
"article-title": "Digital physical therapy in the COVID-19 pandemic",
"author": "Dantas",
"doi-asserted-by": "publisher",
"first-page": "381",
"journal-title": "Braz J Phys Ther",
"key": "ref10",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1002/pri.259",
"article-title": "Short-wave diathermy: current clinical and safety practices",
"author": "Shields",
"doi-asserted-by": "publisher",
"first-page": "191",
"journal-title": "Physiother Res Int",
"key": "ref11",
"volume": "7",
"year": "2002"
},
{
"DOI": "10.1136/thx.52.6.561",
"article-title": "Short wave diathermy for small spontaneous pneumothorax",
"author": "Ma",
"doi-asserted-by": "publisher",
"first-page": "561",
"journal-title": "Thorax",
"key": "ref12",
"volume": "52",
"year": "1997"
},
{
"DOI": "10.1002/bem.22013",
"article-title": "Short-wave therapy for spontaneous pneumothorax: a case report",
"author": "Ye",
"doi-asserted-by": "publisher",
"first-page": "78",
"journal-title": "Bioelectromagnetics",
"key": "ref13",
"volume": "38",
"year": "2017"
},
{
"DOI": "10.1191/0269215505cr864oa",
"article-title": "Effect of pulsed short-wave diathermy on pain and function of subjects with osteoarthritis of the knee: a placebo-controlled double-blind clinical trial",
"author": "Laufer",
"doi-asserted-by": "publisher",
"first-page": "255",
"journal-title": "Clin Rehabil",
"key": "ref14",
"volume": "19",
"year": "2005"
},
{
"article-title": "Treatment of peptic ulcer by ultra-short-wave diathermy",
"author": "Pekarek",
"first-page": "267",
"journal-title": "Br J Phys Med",
"key": "ref15",
"volume": "15",
"year": "1952"
},
{
"article-title": "The use of pulsed and continuous UHF electrical fields in the rehabilitation of patients with the Guillain-Barre syndrome and other peripheral myelinopathies",
"author": "Gorbunov",
"first-page": "22",
"journal-title": "Zh Nevrol Psikhiatr Im S S Korsakova",
"key": "ref16",
"volume": "95",
"year": "1995"
},
{
"DOI": "10.1097/PHM.0000000000000873",
"article-title": "Effect of stretching combined with ultrashort wave diathermy on joint function and its possible mechanism in a rabbit knee contracture model",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "357",
"journal-title": "Am J Phys Med Rehabil",
"key": "ref17",
"volume": "97",
"year": "2018"
},
{
"DOI": "10.1002/bem.22353",
"article-title": "Effects of ultrashort wave therapy on inflammation and macrophage polarization after acute lung injury in rats",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "464",
"journal-title": "Bioelectromagnetics",
"key": "ref18",
"volume": "42",
"year": "2021"
},
{
"article-title": "Effects of ultra-short wave diathermy on chronic pneumonia in children",
"author": "Yang",
"first-page": "109",
"journal-title": "Chin Med J",
"key": "ref19",
"volume": "81",
"year": "1962"
},
{
"DOI": "10.1080/00218469408026647",
"article-title": "Uneven field in ultra-short-wave diathermy: its application for sinusitis",
"author": "Rost",
"doi-asserted-by": "publisher",
"first-page": "243",
"journal-title": "Br J Phys Med",
"key": "ref20",
"volume": "16",
"year": "1953"
},
{
"article-title": "The treatment of nasal sinus infection by ultra-short wave diathermy",
"author": "Paterson",
"first-page": "454",
"journal-title": "Can Med Assoc J",
"key": "ref21",
"volume": "42",
"year": "1940"
},
{
"DOI": "10.1155/2020/3642143",
"article-title": "Scaling the need, benefits, and risks associated with COVID-19 acute and postacute care rehabilitation: a review",
"author": "Shah",
"doi-asserted-by": "publisher",
"first-page": "3642143",
"journal-title": "Rehabil Res Pract",
"key": "ref22",
"volume": "2020",
"year": "2020"
},
{
"DOI": "10.1016/j.lfs.2020.118958",
"article-title": "HUCMSCs transplantation combined with ultrashort wave therapy attenuates neuroinflammation in spinal cord injury through NUR77/NF-kappaB pathway",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "118958",
"journal-title": "Life Sci",
"key": "ref23",
"volume": "267",
"year": "2021"
},
{
"DOI": "10.1155/2020/3021750",
"article-title": "Ultrashort wave combined with human umbilical cord mesenchymal stem cell (HUC-MSC) transplantation inhibits NLRP3 inflammasome and improves spinal cord injury via MK2/TTP signalling pathway",
"author": "Na",
"doi-asserted-by": "publisher",
"first-page": "3021750",
"journal-title": "Biomed Res Int",
"key": "ref24",
"volume": "2020",
"year": "2020"
},
{
"DOI": "10.1136/bjsm.23.2.123",
"article-title": "Continuous short-wave (radio-frequency) diathermy",
"author": "Goats",
"doi-asserted-by": "publisher",
"first-page": "123",
"journal-title": "Br J Sports Med",
"key": "ref25",
"volume": "23",
"year": "1989"
},
{
"DOI": "10.1080/09593985.2020.1757264",
"article-title": "Ultra-shortwave diathermy - a new purported treatment for management of patients with COVID-19",
"author": "Yu",
"doi-asserted-by": "publisher",
"first-page": "559",
"journal-title": "Physiother Theory Pract",
"key": "ref26",
"volume": "36",
"year": "2020"
},
{
"DOI": "10.1002/pri.473",
"article-title": "Short wave diathermy in the symptomatic management of chronic pelvic inflammatory disease pain: a randomized controlled trial",
"author": "Lamina",
"doi-asserted-by": "publisher",
"first-page": "50",
"journal-title": "Physiother Res Int",
"key": "ref27",
"volume": "16",
"year": "2011"
},
{
"DOI": "10.4085/1062-6050-50.1.12",
"article-title": "Short-wave diathermy pretreatment and inflammatory myokine response after high-intensity eccentric exercise",
"author": "Vardiman",
"doi-asserted-by": "publisher",
"first-page": "612",
"journal-title": "J Athl Train",
"key": "ref28",
"volume": "50",
"year": "2015"
},
{
"DOI": "10.1007/BF02343540",
"article-title": "Development and application of a quality control procedure for short-wave diathermy units",
"author": "Shields",
"doi-asserted-by": "publisher",
"first-page": "62",
"journal-title": "Med Biol Eng Comput",
"key": "ref29",
"volume": "41",
"year": "2003"
},
{
"DOI": "10.1097/INF.0b013e318157da59",
"article-title": "Temperature, humidity, and ultraviolet B radiation predict community respiratory syncytial virus activity",
"author": "Welliver",
"doi-asserted-by": "publisher",
"first-page": "S29",
"journal-title": "Pediatr Infect Dis J",
"key": "ref30",
"volume": "26",
"year": "2007"
},
{
"DOI": "10.3760/cma.j.issn.0254-1424.2003.06.005",
"article-title": "Application of ultrashort wave diathermy in treatment of severe acute respiratory syndrome",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "332",
"journal-title": "Chin J Rehabil Med Rehabil",
"key": "ref31",
"volume": "6",
"year": "2003"
},
{
"DOI": "10.1148/ryct.2020200075",
"article-title": "Serial quantitative chest CT assessment of COVID-19: a deep learning approach",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "e200075",
"journal-title": "Radiol Cardiothorac Imaging",
"key": "ref32",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.3760/cma.j.issn.0254-1424.2003.06.005",
"article-title": "Changes of serum cytokines in children with bronchopneumonia treated with ultrashort wave diathermy",
"author": "He",
"doi-asserted-by": "publisher",
"first-page": "323",
"journal-title": "J Appl Clin Pediatr",
"key": "ref33",
"volume": "21",
"year": "2006"
},
{
"DOI": "10.16766/j.cnki.issn.1674-4152.2012.08.063",
"article-title": "Benefits of adjuvant therapy with transcutaneous ion introduction of traditional Chinese medicine by using microcomputer control intermediate frequency stimulator and ultrashort wave therapy on 112 cases of infantile pneumonia",
"author": "Du",
"doi-asserted-by": "publisher",
"first-page": "1232",
"journal-title": "Chin J Gen Pract",
"key": "ref34",
"volume": "10",
"year": "2012"
},
{
"DOI": "10.1016/B978-008043005-8/50012-3",
"article-title": "Effect of ultrashort wave and medications on pulmonary function of pneumonia patients",
"author": "Zhu",
"doi-asserted-by": "publisher",
"first-page": "75",
"journal-title": "Chin J Phys Ther",
"key": "ref35",
"volume": "22",
"year": "1999"
},
{
"DOI": "10.1001/jama.1950.72910190003007",
"article-title": "Medical diathermy",
"author": "Martin",
"doi-asserted-by": "publisher",
"first-page": "27",
"journal-title": "J Am Med Assoc",
"key": "ref36",
"volume": "142",
"year": "1950"
},
{
"DOI": "10.1053/apmr.2002.32823",
"article-title": "Pulsed short-wave diathermy effects on human fibroblast proliferation",
"author": "Hill",
"doi-asserted-by": "publisher",
"first-page": "832",
"journal-title": "Arch Phys Med Rehabil",
"key": "ref37",
"volume": "83",
"year": "2002"
},
{
"DOI": "10.3892/etm.2018.6999",
"article-title": "Association of the proliferation of lung fibroblasts with the ERK1/2 signaling pathway in neonatal rats with hyperoxia-induced lung fibrosis",
"author": "Hu",
"doi-asserted-by": "publisher",
"first-page": "701",
"journal-title": "Exp Ther Med",
"key": "ref38",
"volume": "17",
"year": "2019"
},
{
"DOI": "10.3760/cma.j.issn.0254-1424.2002.09.007",
"article-title": "Effect of Ultrashortwave diathermy on experimental pulmonary interstitial fibrosis",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "533",
"journal-title": "Chin J Phys Med Rehabil.",
"key": "ref39",
"volume": "24",
"year": "2002"
},
{
"DOI": "10.1097/PHM.0000000000001599",
"article-title": "Effect of radial extracorporeal shock wave combined with ultrashort wave diathermy on fibrosis and contracture of muscle",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "643",
"journal-title": "Am J Phys Med Rehabil",
"key": "ref40",
"volume": "100",
"year": "2021"
},
{
"DOI": "10.3760/cma.j.issn.0254-1424.2020.06.019",
"article-title": "Effect of ultrashort wave in the treatment of children with Mycoplasma pneumonia and serum inflammatory factors",
"author": "Luo",
"doi-asserted-by": "publisher",
"first-page": "559",
"journal-title": "Chin J Phys Med Rehabil.",
"key": "ref41",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.3760/cma.j.issn.0254-1424.2018.07.010",
"article-title": "Effect of ultrashort wave and magnetic therapy on serum inflammatory factors in children with bronchial pneumonia",
"author": "Ma",
"doi-asserted-by": "publisher",
"first-page": "519",
"journal-title": "Chin J Phys Med Rehabil",
"key": "ref42",
"volume": "40",
"year": "2018"
},
{
"DOI": "10.3760/cma.j.issn.0254-1424.2012.01.020",
"article-title": "The effect of ultrashort wave adjuvant therapy on adult mycoplasma pneumoniae pneumonia and serum cytokines",
"author": "Hu",
"doi-asserted-by": "publisher",
"first-page": "61",
"journal-title": "Chin J Phys Med Rehabil.",
"key": "ref43",
"volume": "34",
"year": "2012"
},
{
"DOI": "10.1016/S2589-7500(20)30222-3",
"article-title": "CT scan AI-aided triage for patients with COVID-19 in China",
"author": "Vardhanabhuti",
"doi-asserted-by": "publisher",
"first-page": "e494",
"journal-title": "Lancet Digit Health",
"key": "ref44",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1016/S2589-7500(20)30199-0",
"article-title": "Deep learning-based triage and analysis of lesion burden for COVID-19: a retrospective study with external validation",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "e506",
"journal-title": "Lancet Digit Health",
"key": "ref45",
"volume": "2",
"year": "2020"
}
],
"reference-count": 45,
"references-count": 45,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2023.1149250/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Efficacy and safety of ultra-short wave diathermy on COVID-19 pneumonia: a pioneering study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "10"
}