Admission Rothman Index, Aspirin, and Intermediate Dose Anticoagulation Effects on Outcomes in COVID-19: A Multi-Site Propensity Matched Analysis
et al., Blood, doi:10.1182/blood-2020-143349, Nov 2020
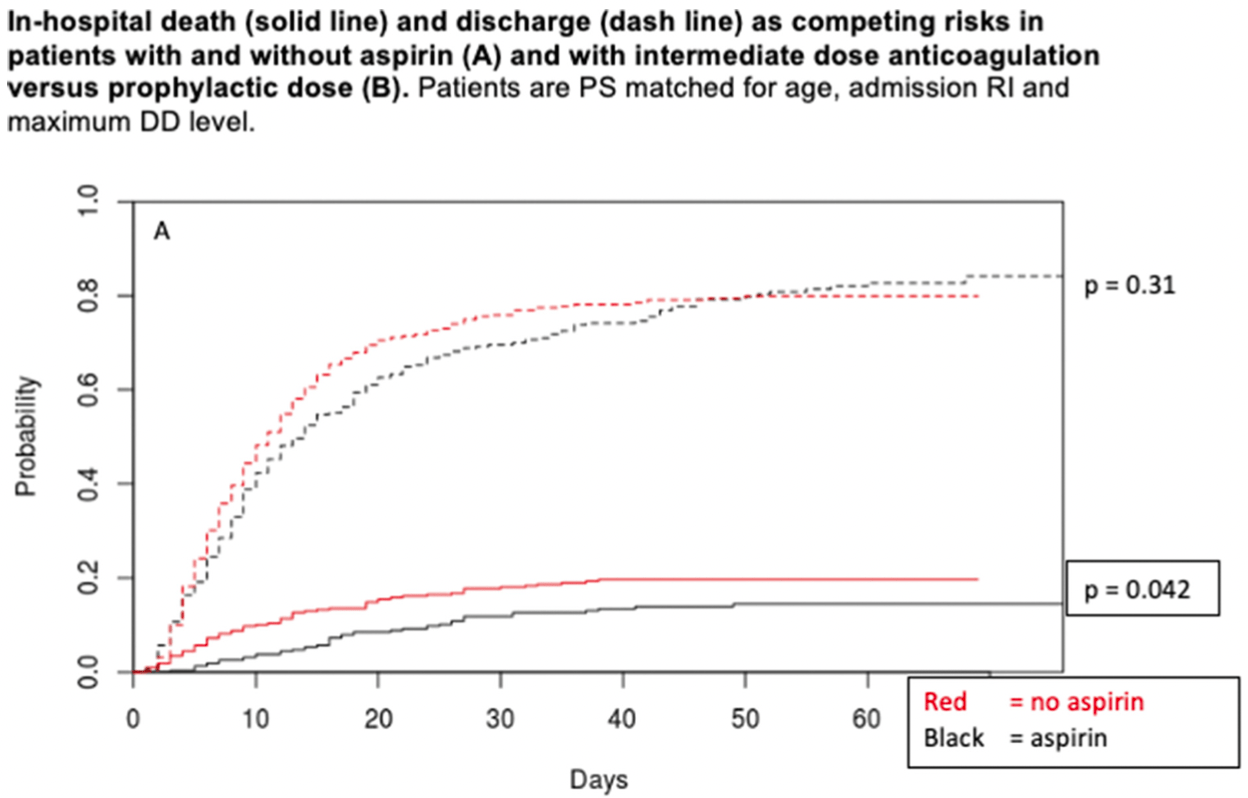
PSM retrospective 2,785 hospitalized patients in the USA, showing lower mortality and higher ventilation and ICU admission with aspirin treatment.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 35.0% lower, OR 0.65, p = 0.04, treatment 319, control 319, propensity score matching, RR approximated with OR.
|
|
risk of mechanical ventilation, 49.0% higher, OR 1.49, p = 0.04, treatment 319, control 319, propensity score matching, RR approximated with OR.
|
|
risk of ICU admission, 45.0% higher, OR 1.45, p = 0.02, treatment 319, control 319, propensity score matching, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Goshua et al., 5 Nov 2020, retrospective, USA, peer-reviewed, 15 authors.
Admission Rothman Index, Aspirin, and Intermediate Dose Anticoagulation Effects on Outcomes in COVID-19: A Multi-Site Propensity Matched Analysis
Blood, doi:10.1182/blood-2020-143349
Introduction: Venous thromboembolism and in-situ small vessel thrombosis are increased in hospitalized patients with COVID-19 in several patient cohorts. Endotheliopathy and activation of both platelets and coagulation predict critical illness and death. For these reasons the use of anti-platelet agents and increased-intensity anticoagulation in the care of hospitalized patients with COVID-19 is under
Disclosures Neuberg: Pharmacyclics: Research Funding; Madrigak Pharmaceuticals: Current equity holder in publicly-traded company; Celgene: Research Funding.
Author notes * Asterisk with author names denotes non-ASH members.
© 2020 by the American Society of Hematology
DOI record:
{
"DOI": "10.1182/blood-2020-143349",
"ISSN": [
"0006-4971",
"1528-0020"
],
"URL": "http://dx.doi.org/10.1182/blood-2020-143349",
"abstract": "<jats:p>Introduction: Venous thromboembolism and in-situ small vessel thrombosis are increased in hospitalized patients with COVID-19 in several patient cohorts. Endotheliopathy and activation of both platelets and coagulation predict critical illness and death. For these reasons the use of anti-platelet agents and increased-intensity anticoagulation in the care of hospitalized patients with COVID-19 is under intense study in several clinical trials. We sought to examine the impact of aspirin and anticoagulation on hospitalization outcomes.</jats:p>\n <jats:p>Methods: We examined outcomes in a large multi-site cohort of consecutive, hospitalized, COVID-19 laboratory confirmed patients under a risk-stratified treatment algorithm from March 13 through June 18, with a focus on efficacy of aspirin and/or increased-intensity anticoagulation. Out of 4150 identified hospitalized patients with COVID-19, we created 3 study cohorts. The overall cohort (2785 patients) excluded pediatric patients, those with incomplete electronic data, and those with multiple admissions. The aspirin (1956 patients) and anticoagulation (1623 patients) cohorts were nested within the overall cohort; the former excluded patients on any home anti-platelet therapy or those who received non-aspirin anti-platelet therapy in the hospital, while the latter excluded patients who did not receive prophylactic or intermediate dose anticoagulation in the hospital. The primary outcome was in-hospital death. Secondary outcomes were time-to-death with a competing risk (time-to-hospital-discharge), escalation to ICU, length-of-stay and use of mechanical ventilation. Variables examined included age, gender, BMI, race, Rothman Index (RI), D-dimer (DD) and patient co-morbidities including cardiovascular disease, chronic kidney disease, and prior VTE. The aspirin and anticoagulation cohorts underwent propensity score (PS) matching utilizing variables found to be significant in multivariable regression modeling in the overall cohort with 638 and 386 patients, respectively.</jats:p>\n <jats:p>Results: Univariate followed by multivariable regression modeling in the 2785 patient overall cohort established a novel role for RI, and independent roles for age, BMI, and maximum DD, in predicting severity of illness. In all cohorts the 50th and lower percentile of admission RI was predictive of mortality in multivariable modeling (i.e. aspirin: 3rd and 4th admission RI quartiles with HR = 0.18 for both, p&lt;0.001 for both). In PS matched patients, aspirin was associated with a significant decrease in mortality (OR 0.65 [0.42, 0.98], p=0.044) and a significant increase in mechanical ventilation (OR 1.49 [1.03, 2.18], p=0.037) and ICU status (OR = 1.45 [1.06, 1.98], p=0.021). In PS matched patients in the anticoagulation cohort, intermediate versus prophylactic dose anticoagulation was associated with a marginal decrease in mortality (OR 0.60, p=0.053). In the aspirin cohort examining in-hospital death and discharge as competing risks, the use of aspirin was associated with decreased mortality (p=0.042) and had no effect on discharge (p=0.31). In the anticoagulation cohort a similar competing risk model showed the use of intermediate rather than prophylactic anticoagulation decreased mortality (p=0.046) and had no effect on discharge (p = 0.21).</jats:p>\n <jats:p>Conclusion: We show in a large cohort of consecutively hospitalized patients with COVID-19 treated under a risk-stratified algorithm the prognostic utility of the admission RI in assessing outcomes in hospitalized patients with COVID-19 and a potential benefit of aspirin therapy on in-hospital death from COVID-19. A potential albeit marginal benefit of intermediate dose anticoagulation over prophylactic dose anticoagulation merits further study with results of clinical trials awaited.</jats:p>\n <jats:p>Figure</jats:p>\n <jats:sec>\n <jats:title>Disclosures</jats:title>\n <jats:p>Neuberg: Pharmacyclics: Research Funding; Madrigak Pharmaceuticals: Current equity holder in publicly-traded company; Celgene: Research Funding.</jats:p>\n </jats:sec>",
"author": [
{
"affiliation": [
{
"name": "Section of Hematology, Yale University School of Medicine, New Haven, CT"
}
],
"family": "Goshua",
"given": "George",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Data Science, Dana-Farber Cancer Institute, Boston, MA"
}
],
"family": "Liu",
"given": "Yiwen",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Yale University School of Medicine, New Haven,"
}
],
"family": "Meizlish",
"given": "Matthew L.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Yale University School of Medicine, New Haven,"
}
],
"family": "Fine",
"given": "Rebecca",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy, Yale-New Haven Hospital, New Haven,"
}
],
"family": "Amin",
"given": "Kejal",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Section of Hematology, Yale University School of Medicine, New Haven,"
}
],
"family": "Chang",
"given": "Eric",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Yale University, New Haven, CT"
}
],
"family": "Liu",
"given": "Yuxin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy, Yale University School of Medicine, New Havem,"
}
],
"family": "McManus",
"given": "Dayna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy, Yale New Haven Hospital, New Haven,"
}
],
"family": "Petrosan",
"given": "Adina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Yale School of Medicine, New Haven, CT"
}
],
"family": "Ochoa Chaar",
"given": "Cassius Ilya",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Section of Cardiovascular Medicine, Yale University School of Medicine, New Haven, CT"
}
],
"family": "Chun",
"given": "Hyung J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "University of Connecticut, Storrs,"
}
],
"family": "Defilippo",
"given": "Nicholas A.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Data Science, Dana-Farber Cancer Institute, Boston, MA"
}
],
"family": "Neuberg",
"given": "Donna S.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Yale New Haven Hospital, New Haven, CT"
}
],
"family": "Owusu",
"given": "Kent A.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Section of Hematology, Department of Internal Medicine, Yale University School of Medicine and Yale Cancer Center, New Haven, CT"
}
],
"family": "Lee",
"given": "Alfred Ian",
"sequence": "additional"
}
],
"container-title": "Blood",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"ashpublications.org"
]
},
"created": {
"date-parts": [
[
2021,
2,
6
]
],
"date-time": "2021-02-06T16:25:58Z",
"timestamp": 1612628758000
},
"deposited": {
"date-parts": [
[
2021,
2,
6
]
],
"date-time": "2021-02-06T16:26:00Z",
"timestamp": 1612628760000
},
"indexed": {
"date-parts": [
[
2022,
4,
3
]
],
"date-time": "2022-04-03T17:07:27Z",
"timestamp": 1649005647309
},
"is-referenced-by-count": 3,
"issue": "Supplement 1",
"issued": {
"date-parts": [
[
2020,
11,
5
]
]
},
"journal-issue": {
"issue": "Supplement 1",
"published-print": {
"date-parts": [
[
2020,
11,
5
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://ashpublications.org/blood/article/136/Supplement%201/23/470342/Admission-Rothman-Index-Aspirin-and-Intermediate",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://ashpublications.org/blood/article/136/Supplement%201/23/470342/Admission-Rothman-Index-Aspirin-and-Intermediate",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "234",
"original-title": [],
"page": "23-24",
"prefix": "10.1182",
"published": {
"date-parts": [
[
2020,
11,
5
]
]
},
"published-print": {
"date-parts": [
[
2020,
11,
5
]
]
},
"publisher": "American Society of Hematology",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://ashpublications.org/blood/article/136/Supplement%201/23/470342/Admission-Rothman-Index-Aspirin-and-Intermediate"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cell Biology",
"Hematology",
"Immunology",
"Biochemistry"
],
"subtitle": [],
"title": "Admission Rothman Index, Aspirin, and Intermediate Dose Anticoagulation Effects on Outcomes in COVID-19: A Multi-Site Propensity Matched Analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1182/blood.2019cm0000",
"volume": "136"
}