Vitamin B12 effectiveness in the management of hospitalized COVID‐19 and its clinical outcomes and complications: A randomized clinical trial
et al., Health Science Reports, doi:10.1002/hsr2.1509, Sep 2023
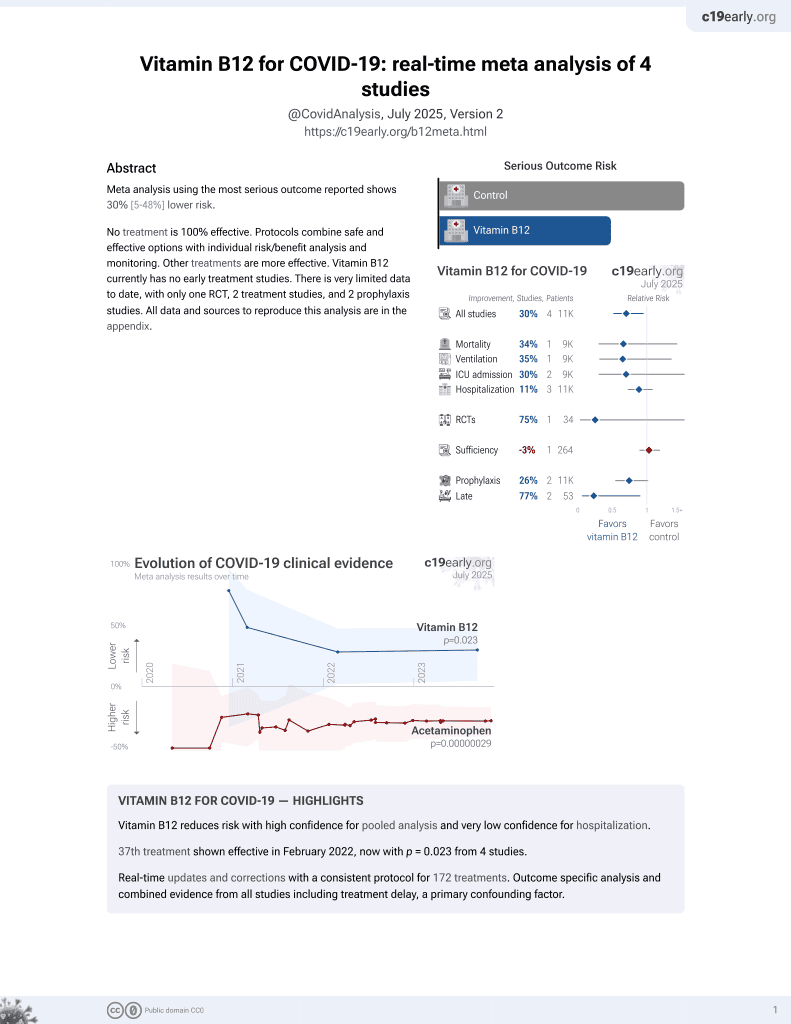
38th treatment shown to reduce risk in
February 2022, now with p = 0.023 from 4 studies.
Lower risk for recovery.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Small RCT 34 hospitalized patients in Iran showing improved imflammatory markers and lower ICU admission with vitamin B12 treatment, without statistical significance. There was no mortality.
|
risk of ICU admission, 75.0% lower, RR 0.25, p = 0.34, treatment 1 of 17 (5.9%), control 4 of 17 (23.5%), NNT 5.7.
|
|
hospitalization time, 0.8% higher, relative time 1.01, p = 0.97, treatment mean 7.47 (±2.93) n=17, control mean 7.41 (±4.88) n=17.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Erfani et al., 14 Sep 2023, Randomized Controlled Trial, placebo-controlled, Iran, peer-reviewed, median age 52.6, 4 authors.
Contact: nafisehalizadeh@yahoo.com.
Vitamin B12 effectiveness in the management of hospitalized COVID‐19 and its clinical outcomes and complications: A randomized clinical trial
Health Science Reports, doi:10.1002/hsr2.1509
Background and Aims: Since 2019, severe acute respiratory syndrome coronavirus 2, has spread and challenged the health care system for treatment which is mainly limited to supportive care. It is well-established that malnutrition impedes the immunity in human bodies, and makes it vulnerable to microorganisms. Vitamin B12 is one of the agents that has critical roles in body systems. Thus, the following clinical trial was conducted to assess its possible therapeutic value in COVID-19 patients. Method: The present randomized clinical trial was carried out in Baharlou Hospital, and patients with confirmed COVID-19 infection within 24 h of admission were included. We used quadruple blocks randomization to divide patients into groups of case and control. The case group received 1000 mg of vitamin B12, daily for 7 day while the patients in control group were administered distilled water as placebo. The studied outcomes were duration of hospitalization, need for intensive care unit (ICU), mechanical ventilation, mortality rate and laboratory findings. The statistical analysis was done via SPSS version 22. Results: After implementing inclusion and exclusion criteria, 34 participants were included in the study, 20 of which were male. Serum levels of creatinine, LDH (Lactate dehydrogenase), Ferritin, and CRP (C-reactive protein) had decreased in both groups. The improving changes of CRP, LDH, ferritin and creatinine was higher in case group. The increase of Alanine Transaminase and D-dimer was higher in control group. however there was no statistically significant difference. More patients were admitted to ICU in the control group but the difference was not statistically significant. Duration of hospitalization did not differ statistically between the groups. No in hospital mortality has been recorded.
Conclusion: Our study suggests that vitamin B12 supplementation seem to have curative effect in COVID-19. Nutritious diet is necessary for proper functioning of the immune system. Since malnutrition is associated with poor prognosis in COVID-19 patients, and limited number of participants in this study, we suggest performing meta-analysis on similar studies to reach reliable result.
References
Ali, Kunugi, Approaches to nutritional screening in patients with coronavirus disease 2019 (Covid-19), Int J Environ Res Public Health
Alizadeh, Tabatabaei, Azimi, Lactate dehydrogenase to albumin ratio as a predictive factor of COVID-19 patients' outcome; a cross-sectional study, Arch Acad Emerg Med
Allard, Ouedraogo, Molleville, Malnutrition: percentage and association with prognosis in patients hospitalized for coronavirus disease 2019, Nutrients
Annweiler, Corvaisier, Gautier, Vitamin d supplementation associated to better survival in hospitalized frail elderly covid-19 patients: the geria-covid quasi-experimental study, Nutrients
Anwar, Raut, Kanwal, Yahia, Vitamin B 12 deficiency and increased susceptibility and severity of Covid-19: a review, Int J Creat Res Thoughts
Azimi, Faramarzi, Sarbakhsh, Ostadrahimi, Somi et al., Folate and vitamin B12 status and their relation to hematological indices in healthy adults of Iranians: Azar cohort study, doi:10.1177/0260106018815392
Bedock, Couffignal, Lassen, Evolution of nutritional status after early nutritional management in covid-19 hospitalized patients, Nutrients
Bourbour, Dahka, Gholamalizadeh, Nutrients in prevention, treatment, and management of viral infections; special focus on Coronavirus
Camp, Bai, Gonullu, Nayak, Hm, Melatonin interferes with COVID-19 at several distinct ROS-related steps, J Inorg Biochem
Corcoran, Neill, Webb, Ho, Prevalence of vitamin deficiencies on admission: relationship to hospital mortality in critically ill patients, Anaesth Intensive Care
Darand, Hassanizadeh, Martami, Shams, Mirzaei et al., The association between B vitamins and the risk of COVID-19, Br J Nutr, doi:10.1017/s0007114522003075
Fathizadeh, Afshar, Masoudi, SARS-CoV-2 (Covid-19) vaccines structure, mechanisms and effectiveness: a review, Int J Biol Macromol
Galmés, Serra, Palou, Current state of evidence: influence of nutritional and nutrigenetic factors on immunity in the COVID-19 pandemic framework, Nutrients
Kien, Wee, COVID-19's toll on the elderly and those with diabetes mellitus-is vitamin B12 deficiency an accomplice?
Li, Zhang, Gong, Prevalence of malnutrition and analysis of related factors in elderly patients with COVID-19 in Wuhan, China, Eur J Clin Nutr
Manzanares, Hardy, Vitamin B12 pharmaconutrition for COVID-19, Rev Nutr Clínica y Metab
Monyck, Dos Santos, Can vitamin B12 be an adjuvant to COVID-19 treatment?, GSC Biolo Pharmaceut Sci
Ochani, Asad, Yasmin, Covid-19 pandemic: from origins to outcomes. A comprehensive review of viral pathogenesis, clinical manifestations, diagnostic evaluation, and management, Infez Med
Panahibakhsh, Amiri, Doroudi, The association between micronutrients and the SARS-CoV-2-specific antibodies in convalescent patients, Infection
Richardson, Lovegrove, Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: A UK perspective, Br J Nutr
Robert, Darmstadt, Brown, Vitamin B 12 deficiency, Va Med Mon
Sepandi, Taghdir, Alimohamadi, Afrashteh, Hosamirudsari, Factors associated with mortality in COVID-19 patients: A systematic review and meta-analysis, Iran J Public Health
Shakeri, Azimian, Ghasemzadeh-Moghaddam, Evaluation of the relationship between serum levels of zinc, vitamin B12, vitamin D, and clinical outcomes in patients with COVID-19, J Med Virol
Silva, Lima, Sena-Evangelista, Marchioni, Cobucci et al., Nutritional risk screening tools for older adults with covid-19: a systematic review, Nutrients
Tan, Ho, Kalimuddin, Cohort study to evaluate the effect of vitamin D, magnesium, and vitamin B12 in combination on progression to severe outcomes in older patients with coronavirus (COVID-19), Nutrition
Thibault, Coëffier, Joly, Bohé, Schneider et al., How the Covid-19 epidemic is challenging our practice in clinical nutrition-feedback from the field, Eur J Clin Nutr
Vj, Ramos-Campo, Mielgo-Ayuso, Nutrition in the actual covid-19 pandemic. A narrative review, Nutrients
Wee, COVID-19's toll on the elderly and those with diabetes mellitus -is vitamin B12 deficiency an accomplice?, Med Hypotheses
DOI record:
{
"DOI": "10.1002/hsr2.1509",
"ISSN": [
"2398-8835",
"2398-8835"
],
"URL": "http://dx.doi.org/10.1002/hsr2.1509",
"abstract": "<jats:title>Abstract</jats:title><jats:sec><jats:title>Background and Aims</jats:title><jats:p>Since 2019, severe acute respiratory syndrome coronavirus 2, has spread and challenged the health care system for treatment which is mainly limited to supportive care. It is well‐established that malnutrition impedes the immunity in human bodies, and makes it vulnerable to microorganisms. Vitamin B12 is one of the agents that has critical roles in body systems. Thus, the following clinical trial was conducted to assess its possible therapeutic value in COVID‐19 patients.</jats:p></jats:sec><jats:sec><jats:title>Method</jats:title><jats:p>The present randomized clinical trial was carried out in Baharlou Hospital, and patients with confirmed COVID‐19 infection within 24 h of admission were included. We used quadruple blocks randomization to divide patients into groups of case and control. The case group received 1000 mg of vitamin B12, daily for 7 day while the patients in control group were administered distilled water as placebo. The studied outcomes were duration of hospitalization, need for intensive care unit (ICU), mechanical ventilation, mortality rate and laboratory findings. The statistical analysis was done via SPSS version 22.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>After implementing inclusion and exclusion criteria, 34 participants were included in the study, 20 of which were male. Serum levels of creatinine, LDH (Lactate dehydrogenase), Ferritin, and CRP (C‐reactive protein) had decreased in both groups. The improving changes of CRP, LDH, ferritin and creatinine was higher in case group. The increase of Alanine Transaminase and D‐dimer was higher in control group. however there was no statistically significant difference. More patients were admitted to ICU in the control group but the difference was not statistically significant. Duration of hospitalization did not differ statistically between the groups. No in hospital mortality has been recorded.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>Our study suggests that vitamin B12 supplementation seem to have curative effect in COVID‐19. Nutritious diet is necessary for proper functioning of the immune system. Since malnutrition is associated with poor prognosis in COVID‐19 patients, and limited number of participants in this study, we suggest performing meta‐analysis on similar studies to reach reliable result.</jats:p></jats:sec>",
"alternative-id": [
"10.1002/hsr2.1509"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2023-04-06"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2023-08-07"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2023-09-14"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-7071-5103",
"affiliation": [
{
"name": "School of Medicine Tehran University of Medical Sciences Tehran Iran"
}
],
"authenticated-orcid": false,
"family": "Erfani",
"given": "Zahra",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Baharlou Hospital Research Center Tehran University of Medical Sciences Tehran Iran"
},
{
"name": "Pharmaceutical Care Department Baharlou Hospital Tehran University of Medical Sciences Tehran Iran"
}
],
"family": "Alizadeh",
"given": "Nafiseh",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9599-4575",
"affiliation": [
{
"name": "School of Medicine Tehran University of Medical Sciences Tehran Iran"
},
{
"name": "Baharlou Hospital Research Center Tehran University of Medical Sciences Tehran Iran"
}
],
"authenticated-orcid": false,
"family": "Faraji",
"given": "Neda",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6739-1876",
"affiliation": [
{
"name": "School of Medicine Tehran University of Medical Sciences Tehran Iran"
}
],
"authenticated-orcid": false,
"family": "Teymouri",
"given": "Alireza",
"sequence": "additional"
}
],
"container-title": "Health Science Reports",
"container-title-short": "Health Science Reports",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2023,
9,
14
]
],
"date-time": "2023-09-14T13:31:17Z",
"timestamp": 1694698277000
},
"deposited": {
"date-parts": [
[
2023,
9,
14
]
],
"date-time": "2023-09-14T13:31:26Z",
"timestamp": 1694698286000
},
"indexed": {
"date-parts": [
[
2023,
9,
15
]
],
"date-time": "2023-09-15T15:14:37Z",
"timestamp": 1694790877058
},
"is-referenced-by-count": 0,
"issue": "9",
"issued": {
"date-parts": [
[
2023,
9
]
]
},
"journal-issue": {
"issue": "9",
"published-print": {
"date-parts": [
[
2023,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 13,
"start": {
"date-parts": [
[
2023,
9,
14
]
],
"date-time": "2023-09-14T00:00:00Z",
"timestamp": 1694649600000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/hsr2.1509",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"prefix": "10.1002",
"published": {
"date-parts": [
[
2023,
9
]
]
},
"published-online": {
"date-parts": [
[
2023,
9,
14
]
]
},
"published-print": {
"date-parts": [
[
2023,
9
]
]
},
"publisher": "Wiley",
"reference": [
{
"article-title": "Covid‐19 pandemic: from origins to outcomes. A comprehensive review of viral pathogenesis, clinical manifestations, diagnostic evaluation, and management",
"author": "Ochani R",
"first-page": "20",
"journal-title": "Infez Med",
"key": "e_1_2_11_2_1",
"volume": "29",
"year": "2021"
},
{
"key": "e_1_2_11_3_1",
"unstructured": "World Health Organization.WHO coronavirus (COVID-19) dashboard.https://covid19.who.int"
},
{
"DOI": "10.30574/gscbps.2020.11.3.0155",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_4_1"
},
{
"article-title": "Factors associated with mortality in COVID‐19 patients: A systematic review and meta‐analysis",
"author": "Sepandi M",
"first-page": "1211",
"journal-title": "Iran J Public Health",
"key": "e_1_2_11_5_1",
"volume": "49",
"year": "2020"
},
{
"article-title": "Lactate dehydrogenase to albumin ratio as a predictive factor of COVID‐19 patients' outcome; a cross‐sectional study",
"author": "Alizadeh N",
"first-page": "63",
"journal-title": "Arch Acad Emerg Med",
"key": "e_1_2_11_6_1",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.3390/ijerph18052772",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_7_1"
},
{
"DOI": "10.1017/S000711452000330X",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_8_1"
},
{
"DOI": "10.3390/nu13061924",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_9_1"
},
{
"DOI": "10.3390/nu12102956",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_10_1"
},
{
"DOI": "10.3390/nu12092738",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_11_1"
},
{
"DOI": "10.3390/nu12113377",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_12_1"
},
{
"DOI": "10.1016/j.mehy.2020.110374",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_13_1"
},
{
"DOI": "10.1002/jmv.27277",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_14_1"
},
{
"DOI": "10.1016/j.mehy.2020.110374",
"doi-asserted-by": "crossref",
"key": "e_1_2_11_15_1",
"unstructured": "KienA WeeH. COVID‐19's toll on the elderly and those with diabetes mellitus—is vitamin B12 deficiency an accomplice? 2020."
},
{
"DOI": "10.35454/rncm.v4n1.187",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_16_1"
},
{
"DOI": "10.1080/13813455.2020.1791188",
"doi-asserted-by": "crossref",
"key": "e_1_2_11_17_1",
"unstructured": "BourBourF DahkaSM GholamalizadehM et al. Nutrients in prevention treatment and management of viral infections; special focus on Coronavirus.2020."
},
{
"article-title": "Vitamin B 12 deficiency",
"author": "Robert C",
"first-page": "167",
"journal-title": "Va Med Mon (1918)",
"key": "e_1_2_11_18_1",
"volume": "69",
"year": "2003"
},
{
"key": "e_1_2_11_19_1",
"unstructured": "FathizadehH AfsharS MasoudiMR et al.SARS‐CoV‐2 (Covid‐19) vaccines structure mechanisms and effectiveness: a review.Int J Biol Macromol.2021."
},
{
"DOI": "10.1016/j.jinorgbio.2021.111546",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_20_1"
},
{
"DOI": "10.1177/0260106018815392",
"doi-asserted-by": "crossref",
"key": "e_1_2_11_21_1",
"unstructured": "AzimiS FaramarziE SarbakhshP OstadrahimiA SomiMH GhayourM. Folate and vitamin B12 status and their relation to hematological indices in healthy adults of Iranians: Azar cohort study. 2018.doi:10.1177/0260106018815392"
},
{
"article-title": "Vitamin B 12 deficiency and increased susceptibility and severity of Covid‐19: a review",
"author": "Anwar S",
"first-page": "623",
"journal-title": "Int J Creat Res Thoughts",
"key": "e_1_2_11_22_1",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.3390/nu12123679",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_23_1"
},
{
"article-title": "Cohort study to evaluate the effect of vitamin D, magnesium, and vitamin B12 in combination on progression to severe outcomes in older patients with coronavirus (COVID‐19)",
"author": "Tan CW",
"first-page": "1",
"journal-title": "Nutrition",
"key": "e_1_2_11_24_1",
"volume": "79",
"year": "2020"
},
{
"DOI": "10.1038/s41430-020-0642-3",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_25_1"
},
{
"DOI": "10.3390/nu13072276",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_26_1"
},
{
"DOI": "10.1038/s41430-020-00757-6",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_27_1"
},
{
"DOI": "10.1017/S0007114522003075",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_28_1"
},
{
"DOI": "10.1177/0310057X0903700215",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_29_1"
},
{
"DOI": "10.1007/s15010-022-01774-2",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_30_1"
}
],
"reference-count": 29,
"references-count": 29,
"relation": {},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1002/hsr2.1509"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Vitamin B12 effectiveness in the management of hospitalized COVID‐19 and its clinical outcomes and complications: A randomized clinical trial",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy",
"volume": "6"
}