Association of anti-diabetic drugs and covid-19 outcomes in patients with diabetes mellitus type 2 and chronic kidney disease: Nationwide registry analysis
et al., PLOS ONE, doi:10.1371/journal.pone.0301056, Mar 2024
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
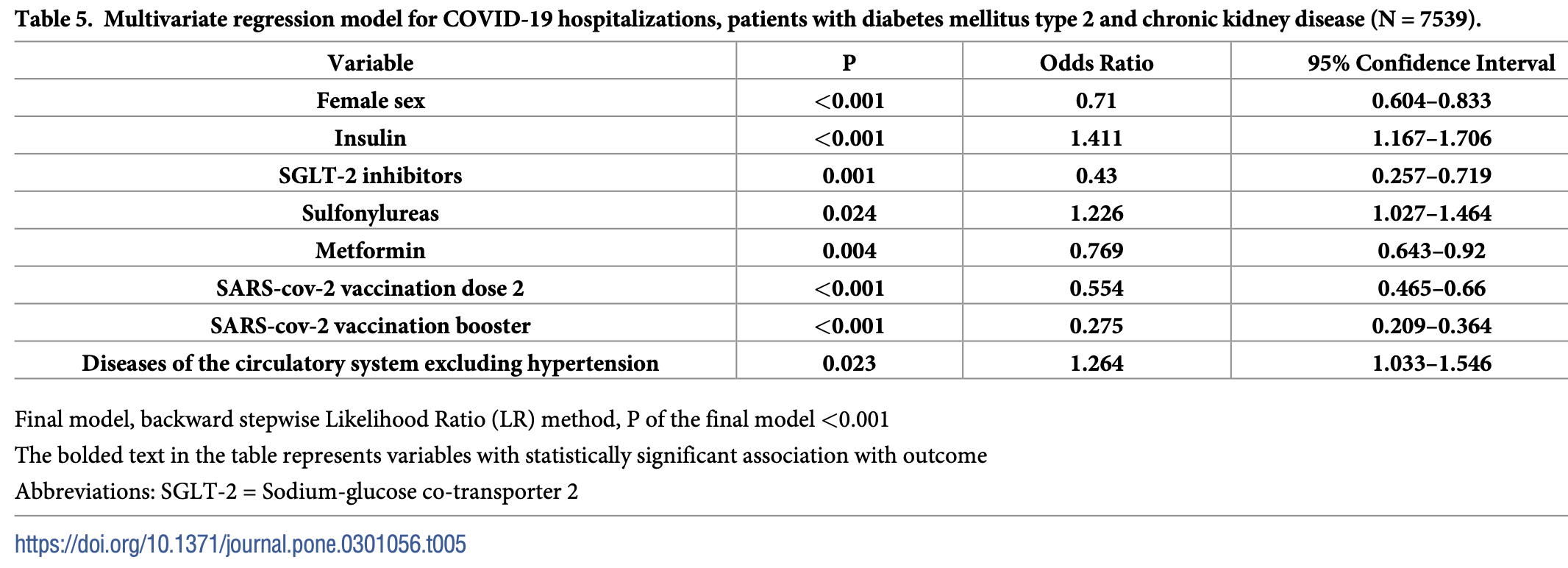
Retrospective 7,539 patients with diabetes mellitus type 2 and chronic kidney disease in Croatia showing lower risk of SARS-CoV-2 infection with SGLT-2 inhibitors, metformin, and repaglinide use, and lower risk of COVID-19 hospitalization with SGLT-2 inhibitors and metformin use.
|
risk of hospitalization, 23.1% lower, OR 0.77, p = 0.004, treatment 2,843, control 4,475, adjusted per study, multivariable, RR approximated with OR.
|
|
risk of case, 12.5% lower, OR 0.88, p = 0.04, treatment 2,843, control 4,475, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Dimnjaković et al., 27 Mar 2024, retrospective, Croatia, peer-reviewed, 7 authors.
Contact: hana.brborovic@gmail.com.
Association of anti-diabetic drugs and covid-19 outcomes in patients with diabetes mellitus type 2 and chronic kidney disease: Nationwide registry analysis
PLOS ONE, doi:10.1371/journal.pone.0301056
Introduction Patients with diabetes mellitus type 2 and chronic kidney disease (T2DM-CKD) have a 5 times higher risk of developing severe SARS-CoV-2 infection than those without these 2 diseases. The goal of this study is to provide information on T2DM-CKD and COVID-19 outcomes, with an emphasis on the association with anti-diabetic medications.
Methodology Study is designed as a retrospective cohort analysis covering the years 2020 and 2021. Data from the National Diabetes Registry (CroDiab) were linked to hospital data, primary healthcare data, Causes of Death Registry data, the SARS-CoV-2 vaccination database, and the SARS-CoV-2 test results database. Study outcomes were cumulative incidence of SARS-CoV-2 positivity, COVID-19 hospitalizations, and COVID-19 deaths. For outcome predictors, logistic regression models were developed.
Results Of 231 796 patients with diabetes mellitus type 2 in the database, 7 539 were T2DM-CKD (3.25%). The 2-year cumulative incidences of all three studies' outcomes were higher in T2DM-CKD than in diabetes patients without CKD (positivity 18.1% vs. 14.4%; hospitalization 9.7% vs. 4.2%; death 3.3% vs. 1.1%, all p<0.001). For COVID-19 hospitalization, protective factors were SGLT-2 inhibitors use (OR 0.430; 95%CI 0.257-0.719) and metformin use (OR 0.769; 95% CI 0.643-0.920), risk factors were insulin use (1.411;) and sulfonylureas use (OR 1.226;. For SARS-CoV-2 positivity
Supporting information
S1
References
Agrawal, Azcoaga-Lorenzo, Fagbamigbe, Vasileiou, Henery et al., Association between multimorbidity and mortality in a cohort of patients admitted to hospital with COVID-19 in Scotland, J R Soc Med, doi:10.1177/01410768211051715
Antoljak, Erceg, Značaj digitalizacije podataka prijave uzroka smrti za unapređenje kvalitete epidemiolos ˇkog nadzora [Role of digitalized death reports in epidemiological surveillance quality, Med. inform
Astrazeneca, Forxiga approved in the EU for the treatment of chronic kidney disease in patients with and without type-2 diabetes
Banerjee, Stoian, Silva-Nunes, Sonmez, Rizvi et al., The role of GLP-1 receptor agonists during COVID-19 pandemia: a hypothetical molecular mechanism, Expert Opin Drug Saf, doi:10.1080/14740338.2021.1970744
Belančić, Kresović, Dijan, Glucagon-like peptide-1 receptor agonists in the era of COVID-19: Friend or foe?, Clin Obes, doi:10.1111/cob.12439
Bornstein, Rubino, Khunti, Mingrone, Hopkins et al., Practical recommendations for the management of diabetes in patients with COVID-19, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587%2820%2930152-2
Cai, Liu, Sun, He, Zheng et al., Prediabetes and the risk of heart failure: A metaanalysis, Diabetes Obes Metab, doi:10.1111/dom.14388
Capak, Kopal, Benjak, Cerovečki, Draus ˇnik Z ˇ et al., Surveillance system for coronavirus disease 2019 epidemiological parameters in Croatia, Croat Med J, doi:10.3325/cmj.2020.61.481
Ceriello, Catrinoiu, Chandramouli, Cosentino, Dombrowsky et al., Heart failure in type 2 diabetes: current perspectives on screening, diagnosis and management, Cardiovasc Diabetol, doi:10.1186/s12933-021-01408-1
Ceriello, Schnell, COVID-19: Considerations of Diabetes and Cardiovascular Disease Management, J Diabetes Sci Technol, doi:10.1177/1932296820930025
Ceriello, Stoian, Rizzo, COVID-19 and diabetes management: What should be considered?, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108151
Cerovečki, COVID-19 Pandemic Influence on Diabetes Management in Croatia, Front Clin Diabetes Healthc, doi:10.3389/fcdhc.2021.704807
Chen, Chen, Chen, Chen, Yang et al., Judicious use of sodium-glucose cotransporter 2 inhibitors in patients with diabetes on coronavirus-19 pandemic, J Chin Med Assoc, doi:10.1097/JCMA.0000000000000354
Chen, Lv, Lin, Arshad, Dai, The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis, Front Endocrinol, doi:10.3389/fendo.2022.895458
Chudasama, Zaccardi, Gillies, Razieh, Yates et al., Patterns of multimorbidity and risk of severe SARS-CoV-2 infection: an observational study in the U.K, BMC Infect Dis, doi:10.1186/s12879-021-06600-y
Clark, Jit, Warren-Gash, Guthrie, Wang et al., Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study, Lancet Glob Health, doi:10.1016/S2214-109X%2820%2930264-3
Cunningham, Carinci, Brillante, Leese, Mcalpine et al., Core Standards of the EUBIROD Project. Defining a European Diabetes Data Dictionary for Clinical Audit and Healthcare Delivery, Methods Inf Med
Dalan, Ang, Tan, Fong, Tay et al., The association of hypertension and diabetes pharmacotherapy with COVID-19 severity and immune signatures: an observational study, Eur Heart J Cardiovasc Pharmacother, doi:10.1093/ehjcvp/pvaa098
Emami, Javanmardi, Pirbonyeh, Akbari, Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: a Systematic Review and Meta-Analysis, Arch Acad Emerg Med
Extance, Covid-19 and long term conditions: what if you have cancer, diabetes, or chronic kidney disease?, BMJ, doi:10.1136/bmj.m1174
Ferrannini, Lund, Benson, Rizzo, Almahmeed et al., Association between use of novel glucose-lowering drugs and COVID-19 hospitalization and death in patients with type 2 diabetes: a nationwide registry analysis, Eur Heart J Cardiovasc Pharmacother, doi:10.1093/ehjcvp/pvac044
Fried, Schmedt, Folkerts, Bowrin, Raad et al., High unmet treatment needs in patients with chronic kidney disease and type 2 diabetes: real-world evidence from a US claims database, Nephrol Dial Transplant, doi:10.1093/ndt/gfac140
Ganesh, Randall, Does metformin affect outcomes in COVID-19 patients with new or pre-existing diabetes mellitus? A systematic review and meta-analysis, Br J Clin Pharmacol, doi:10.1111/bcp.15258
Gerdes, Mu ¨ller, Wolf, Busch, Nephroprotective Properties of Antidiabetic Drugs, J Clin Med, doi:10.3390/jcm12103377
Gibertoni, Reno, Rucci, COVID-19 incidence and mortality in non-dialysis chronic kidney disease patients, PLoS ONE, doi:10.1371/journal.pone.0254525
Girgin, Aksun, Tu ¨zen As, Şencan, Şanlı et al., Effects of comorbidities associated with COVID-19 cases in Intensive Care Unit on mortality and disease progression, Eur Rev Med Pharmacol Sci, doi:10.26355/eurrev%5F202304%5F32174
Gupta, Marzook, Ahmad, Comorbidities and clinical complications associated with SARS-CoV-2 infection: an overview, Clin Exp Med, doi:10.1007/s10238-022-00821-4
Hariyanto, Intan, Hananto, Putri, Kurniawan, Pre-admission glucagon-like peptide-1 receptor agonist (GLP-1RA) and mortality from coronavirus disease 2019 (Covid-19): A systematic review, meta-analysis, and meta-regression, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2021.109031
Henry, Lippi, Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection, Int Urol Nephrol, doi:10.1007/s11255-020-02451-9
Kan, Zhang, Han, Xu, Ye et al., Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis, Front Endocrinol, doi:10.3389/fendo.2021.708494
Katsiki, Ferrannini, Anti-inflammatory properties of antidiabetic drugs: A "promised land" in the COVID-19 era?, J Diabetes Complications, doi:10.1016/j.jdiacomp.2020.107723
Khunti, Aroda, Bhatt, Bozkurt, Buse et al., Re-examining the widespread policy of stopping sodium-glucose cotransporter-2 inhibitors during acute illness: A perspective based on the updated evidence, Diabetes Obes Metab, doi:10.1111/dom.14805
Khunti, Knighton, Zaccardi, Bakhai, Barron et al., Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587%2821%2900050-4
Koncar, Gvozdanović, Primary healthcare information system-the cornerstone for the next generation healthcare sector in Republic of Croatia, Int J Med Inform, doi:10.1016/j.ijmedinf.2005.08.007
Lai, Gigante, Pellicano, Mariani, Iannazzo et al., Kidney dysfunction is associated with adverse outcomes in internal medicine COVID-19 hospitalized patients, Eur Rev Med Pharmacol Sci, doi:10.26355/eurrev%5F202303%5F31809
Lamprea-Montealegre, Madden, Tummalapalli, Chu, Peralta et al., Prescription Patterns of Cardiovascular-and Kidney-Protective Therapies Among Patients With Type 2 Diabetes and Chronic Kidney Disease, Diabetes Care, doi:10.2337/dc22-0614
Machado-Duque, Gaviria-Mendoza, Valladales-Restrepo, Franco, De et al., Treatment patterns of antidiabetic and kidney protective therapies among patients with type 2 diabetes mellitus and chronic kidney disease in Colombia. The KDICO descriptive study, Diabetol Metab Syndr, doi:10.1186/s13098-023-01126-6
Martı ´n Sa ´nchez, ´nez-Selle ´s, Garcı ´a, Guille ´n, ´guez-Artalejo et al., Insights for COVID-19 in 2023, Rev Esp Quimioter, doi:10.37201/req/122.2022
Narayanan, Naik, Sahoo, Kamalanathan, Dipeptidyl peptidase 4 inhibitors in COVID-19: Beyond glycemic control, World J Virol, doi:10.5501/wjv.v11.i6.399
Nassar, Abosheaishaa, Singh, Misra, Bloomgarden, Noninsulin-based antihyperglycemic medications in patients with diabetes and COVID-19: A systematic review and meta-analysis, J Diabetes, doi:10.1111/1753-0407.13359
Nguyen, Ho, Nguyen, Ho, Li et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196
Pang, Liu, Friend or foe? ACE2 inhibitors and GLP-1R agonists in COVID-19 treatment, Obes Med, doi:10.1016/j.obmed.2020.100312
Perez-Gomez, Bartsch, Castillo-Rodriguez, Fernandez-Prado, Fernandez-Fernandez et al., Clarifying the concept of chronic kidney disease for non-nephrologists, Clin Kidney J, doi:10.1093/ckj/sfz007
Permana, Yanto, Hariyanto, Pre-admission use of sodium glucose transporter-2 inhibitor (SGLT-2i) may significantly improves Covid-19 outcomes in patients with diabetes: A systematic review, meta-analysis, and meta-regression, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2022.110205
Poljicanin, Lang, Mach, Svajda, Croatian diabetes registry (CroDiab) and implementation of standardised diabetes checklists using Joint Action CHRODIS Recommendations and Criteria, Ann Ist Super Sanita, doi:10.4415/ANN%5F21%5F01%5F12
Poljicanin, Pavlić-Renar, Metelko, CroDiab NET-registar osoba sa s ˇećernom bolesti [CroDiab NET-electronic diabetes registry, Acta Med Croatica
Poljičanin, Pristas, National public health information system in Croatia
Qu, Zheng, Wang, Li, Liu et al., The potential effects of clinical antidiabetic agents on SARS-CoV-2, J Diabetes, doi:10.1111/1753-0407.13135
Russell, Lone, Baillie, Comorbidities, multimorbidity and COVID-19, Nat Med, doi:10.1038/s41591-022-02156-9
Salmen, Pietroșel, Mihai, Bica, Teodorescu et al., Non-Insulin Novel Antidiabetic Drugs Mechanisms in the Pathogenesis of COVID-19, Biomedicines, doi:10.3390/biomedicines10102624
Schernthaner, Shehadeh, Ametov, Bazarova, Ebrahimi et al., Worldwide inertia to the use of cardiorenal protective glucose-lowering drugs (SGLT2i and GLP-1 RA) in high-risk patients with type 2 diabetes, Cardiovasc Diabetol, doi:10.1186/s12933-020-01154-w
The, The COVID-19 pandemic in 2023: far from over, Lancet, doi:10.1016/S0140-6736%2823%2900050-8
Vergara, Rossi, Biagi, Falasconi, Pannone et al., Role of comorbidities on the mortality in patients with SARS-CoV-2 infection: an Italian cohort study, Minerva Med, doi:10.23736/S0026-4806.21.07187-1
DOI record:
{
"DOI": "10.1371/journal.pone.0301056",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0301056",
"abstract": "<jats:sec id=\"sec001\">\n<jats:title>Introduction</jats:title>\n<jats:p>Patients with diabetes mellitus type 2 and chronic kidney disease (T2DM-CKD) have a 5 times higher risk of developing severe SARS-CoV-2 infection than those without these 2 diseases. The goal of this study is to provide information on T2DM-CKD and COVID-19 outcomes, with an emphasis on the association with anti-diabetic medications.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec002\">\n<jats:title>Methodology</jats:title>\n<jats:p>Study is designed as a retrospective cohort analysis covering the years 2020 and 2021. Data from the National Diabetes Registry (CroDiab) were linked to hospital data, primary healthcare data, Causes of Death Registry data, the SARS-CoV-2 vaccination database, and the SARS-CoV-2 test results database. Study outcomes were cumulative incidence of SARS-CoV-2 positivity, COVID-19 hospitalizations, and COVID-19 deaths. For outcome predictors, logistic regression models were developed.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec003\">\n<jats:title>Results</jats:title>\n<jats:p>Of 231 796 patients with diabetes mellitus type 2 in the database, 7 539 were T2DM-CKD (3.25%). The 2-year cumulative incidences of all three studies’ outcomes were higher in T2DM-CKD than in diabetes patients without CKD (positivity 18.1% vs. 14.4%; hospitalization 9.7% vs. 4.2%; death 3.3% vs. 1.1%, all p<0.001). For COVID-19 hospitalization, protective factors were SGLT-2 inhibitors use (OR 0.430; 95%CI 0.257–0.719) and metformin use (OR 0.769; 95% CI 0.643–0.920), risk factors were insulin use (1.411; 95%CI 1.167–1.706) and sulfonylureas use (OR 1.226; 95% CI 1.027–1.464). For SARS-CoV-2 positivity protective factors were SGLT-2 inhibitors (0.607; 95% CI 0.448–0.823), repaglinide use (OR 0.765; 95% CI 0.593–0.986) and metformin use (OR 0.857; 95% CI 0.770–0.994). DPP-4 inhibitors showed a non-significant decrease in risk for COVID-19 death (OR 0.761; 95% CI 0.568–1.019).</jats:p>\n</jats:sec>\n<jats:sec id=\"sec004\">\n<jats:title>Conclusion</jats:title>\n<jats:p>T2DM-CKD are heavily burdened by COVID-19 disease. Our results suggest no association between antidiabetic drugs and COVID-19 death outcome while SGLT-2 and metformin show to be protective against COVID-19 hospitalization and infection, repaglinide against infection, and insulin and sulfonylureas show to be risk factors for COVID-19 hospitalization and infection. Further research in T2DM-CKD is needed.</jats:p>\n</jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3115-0186",
"affiliation": [],
"authenticated-orcid": true,
"family": "Dimnjaković",
"given": "Jelena",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-1356-4166",
"affiliation": [],
"authenticated-orcid": true,
"family": "Buble",
"given": "Tamara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ivanko",
"given": "Pero",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2336-0861",
"affiliation": [],
"authenticated-orcid": true,
"family": "Poljičanin",
"given": "Tamara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Karanović Štambuk",
"given": "Sandra",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0844-0054",
"affiliation": [],
"authenticated-orcid": true,
"family": "Brborović",
"given": "Hana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Brborović",
"given": "Ognjen",
"sequence": "additional"
}
],
"container-title": "PLOS ONE",
"container-title-short": "PLoS ONE",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2024,
3,
27
]
],
"date-time": "2024-03-27T17:48:05Z",
"timestamp": 1711561685000
},
"deposited": {
"date-parts": [
[
2024,
3,
27
]
],
"date-time": "2024-03-27T17:48:41Z",
"timestamp": 1711561721000
},
"editor": [
{
"affiliation": [],
"family": "Hariyanto",
"given": "Timotius Ivan",
"sequence": "first"
}
],
"indexed": {
"date-parts": [
[
2024,
3,
28
]
],
"date-time": "2024-03-28T01:13:23Z",
"timestamp": 1711588403069
},
"is-referenced-by-count": 0,
"issue": "3",
"issued": {
"date-parts": [
[
2024,
3,
27
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2024,
3,
27
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
3,
27
]
],
"date-time": "2024-03-27T00:00:00Z",
"timestamp": 1711497600000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0301056",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0301056",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2024,
3,
27
]
]
},
"published-online": {
"date-parts": [
[
2024,
3,
27
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"DOI": "10.37201/req/122.2022",
"article-title": "Insights for COVID-19 in 2023.",
"author": "FJ Martín Sánchez",
"doi-asserted-by": "crossref",
"first-page": "114",
"issue": "2",
"journal-title": "Rev Esp Quimioter.",
"key": "pone.0301056.ref001",
"volume": "36",
"year": "2023"
},
{
"article-title": "With the international public health emergency ending, WHO/Europe launches its transition plan for COVID-19",
"author": "World Health Organization",
"key": "pone.0301056.ref002",
"year": "2023"
},
{
"DOI": "10.1016/S0140-6736(23)00050-8",
"article-title": "The COVID-19 pandemic in 2023: far from over",
"author": "The Lancet",
"doi-asserted-by": "crossref",
"first-page": "79",
"issue": "10371",
"journal-title": "Lancet",
"key": "pone.0301056.ref003",
"volume": "401",
"year": "2023"
},
{
"DOI": "10.1177/1932296820930025",
"article-title": "COVID-19: Considerations of Diabetes and Cardiovascular Disease Management.",
"author": "A Ceriello",
"doi-asserted-by": "crossref",
"first-page": "723",
"issue": "4",
"journal-title": "J Diabetes Sci Technol",
"key": "pone.0301056.ref004",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1186/s12933-021-01408-1",
"article-title": "Heart failure in type 2 diabetes: current perspectives on screening, diagnosis and management.",
"author": "A Ceriello",
"doi-asserted-by": "crossref",
"first-page": "218",
"issue": "1",
"journal-title": "Cardiovasc Diabetol.",
"key": "pone.0301056.ref005",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.23736/S0026-4806.21.07187-1",
"article-title": "Role of comorbidities on the mortality in patients with SARS-CoV-2 infection: an Italian cohort study.",
"author": "P Vergara",
"doi-asserted-by": "crossref",
"first-page": "185",
"issue": "2",
"journal-title": "Minerva Med.",
"key": "pone.0301056.ref006",
"volume": "114",
"year": "2023"
},
{
"DOI": "10.1007/s10238-022-00821-4",
"article-title": "Comorbidities and clinical complications associated with SARS-CoV-2 infection: an overview.",
"author": "A Gupta",
"doi-asserted-by": "crossref",
"first-page": "313",
"issue": "2",
"journal-title": "Clin Exp Med.",
"key": "pone.0301056.ref007",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.1093/ndt/gfaa314",
"article-title": "Chronic kidney disease is a key risk factor for severe COVID-19: a call to action by the ERA-EDTA.",
"author": "European Renal Association–European Dialysis and Transplantation Association (ERA-EDTA Council); ERACODA Working Group",
"doi-asserted-by": "crossref",
"first-page": "87",
"issue": "1",
"journal-title": "Nephrol Dial Transplant.",
"key": "pone.0301056.ref008",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.1016/S2214-109X(20)30264-3",
"article-title": "Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study",
"author": "A Clark",
"doi-asserted-by": "crossref",
"first-page": "e1003",
"journal-title": "Lancet Glob Health 2020",
"key": "pone.0301056.ref009",
"volume": "8",
"year": "2020"
},
{
"article-title": "Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: a Systematic Review and Meta-Analysis.",
"author": "A Emami",
"first-page": "e35",
"issue": "1",
"journal-title": "Arch Acad Emerg Med.",
"key": "pone.0301056.ref010",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1007/s11255-020-02451-9",
"article-title": "Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection.",
"author": "BM Henry",
"doi-asserted-by": "crossref",
"first-page": "1193",
"issue": "6",
"journal-title": "Int Urol Nephrol.",
"key": "pone.0301056.ref011",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1174",
"article-title": "Covid-19 and long term conditions: what if you have cancer, diabetes, or chronic kidney disease?",
"author": "A. Extance",
"doi-asserted-by": "crossref",
"first-page": "m1174",
"journal-title": "BMJ",
"key": "pone.0301056.ref012",
"volume": "368",
"year": "2020"
},
{
"article-title": "Kidney dysfunction is associated with adverse outcomes in internal medicine COVID-19 hospitalized patients.",
"author": "S Lai",
"first-page": "2706",
"issue": "6",
"journal-title": "Eur Rev Med Pharmacol Sci.",
"key": "pone.0301056.ref013",
"volume": "27",
"year": "2023"
},
{
"article-title": "Effects of comorbidities associated with COVID-19 cases in Intensive Care Unit on mortality and disease progression.",
"author": "S Girgin",
"first-page": "3753",
"issue": "8",
"journal-title": "Eur Rev Med Pharmacol Sci",
"key": "pone.0301056.ref014",
"volume": "27",
"year": "2023"
},
{
"DOI": "10.1038/s41591-022-02156-9",
"article-title": "Comorbidities, multimorbidity and COVID-19",
"author": "CD Russell",
"doi-asserted-by": "crossref",
"first-page": "334",
"issue": "2",
"journal-title": "Nat Med",
"key": "pone.0301056.ref015",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.1371/journal.pone.0254525",
"article-title": "COVID-19 incidence and mortality in non-dialysis chronic kidney disease patients.",
"author": "D Gibertoni",
"doi-asserted-by": "crossref",
"first-page": "e0254525",
"journal-title": "PLoS ONE",
"key": "pone.0301056.ref016",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1177/01410768211051715",
"article-title": "Association between multimorbidity and mortality in a cohort of patients admitted to hospital with COVID-19 in Scotland.",
"author": "U Agrawal",
"doi-asserted-by": "crossref",
"first-page": "22",
"issue": "1",
"journal-title": "J R Soc Med",
"key": "pone.0301056.ref017",
"volume": "115",
"year": "2022"
},
{
"article-title": "Patterns of multimorbidity and risk of severe SARS-CoV-2 infection: an observational study in the U.K. BMC Infect Dis.",
"author": "YV Chudasama",
"first-page": "908",
"issue": "1",
"key": "pone.0301056.ref018",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1111/dom.14388",
"article-title": "Prediabetes and the risk of heart failure: A meta-analysis",
"author": "X Cai",
"doi-asserted-by": "crossref",
"first-page": "1746",
"issue": "8",
"journal-title": "Diabetes Obes Metab",
"key": "pone.0301056.ref019",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(20)30152-2",
"article-title": "Practical recommendations for the management of diabetes in patients with COVID-19.",
"author": "SR Bornstein",
"doi-asserted-by": "crossref",
"first-page": "546",
"issue": "6",
"journal-title": "Lancet Diabetes Endocrinol.",
"key": "pone.0301056.ref020",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1097/JCMA.0000000000000354",
"article-title": "Judicious use of sodium-glucose cotransporter 2 inhibitors in patients with diabetes on coronavirus-19 pandemic.",
"author": "CF Chen",
"doi-asserted-by": "crossref",
"first-page": "809",
"issue": "9",
"journal-title": "J Chin Med Assoc.",
"key": "pone.0301056.ref021",
"volume": "83",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108151",
"article-title": "COVID-19 and diabetes management: What should be considered?",
"author": "A Ceriello",
"doi-asserted-by": "crossref",
"first-page": "108151",
"journal-title": "Diabetes Res Clin Pract",
"key": "pone.0301056.ref022",
"volume": "163",
"year": "2020"
},
{
"DOI": "10.1016/j.jdiacomp.2020.107723",
"article-title": "Anti-inflammatory properties of antidiabetic drugs: A \"promised land\" in the COVID-19 era?",
"author": "N Katsiki",
"doi-asserted-by": "crossref",
"first-page": "107723",
"issue": "12",
"journal-title": "J Diabetes Complications",
"key": "pone.0301056.ref023",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1080/14740338.2021.1970744",
"article-title": "The role of GLP-1 receptor agonists during COVID-19 pandemia: a hypothetical molecular mechanism.",
"author": "Y Banerjee",
"doi-asserted-by": "crossref",
"first-page": "1309",
"issue": "11",
"journal-title": "Expert Opin Drug Saf.",
"key": "pone.0301056.ref024",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.3390/biomedicines10102624",
"article-title": "Non-Insulin Novel Antidiabetic Drugs Mechanisms in the Pathogenesis of COVID-19.",
"author": "T Salmen",
"doi-asserted-by": "crossref",
"first-page": "2624",
"issue": "10",
"journal-title": "Biomedicines",
"key": "pone.0301056.ref025",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1093/ehjcvp/pvac044",
"article-title": "Association between use of novel glucose-lowering drugs and COVID-19 hospitalization and death in patients with type 2 diabetes: a nationwide registry analysis",
"author": "G Ferrannini",
"doi-asserted-by": "crossref",
"first-page": "10",
"issue": "1",
"journal-title": "Eur Heart J Cardiovasc Pharmacother",
"key": "pone.0301056.ref026",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1093/ehjcvp/pvaa098",
"article-title": "The association of hypertension and diabetes pharmacotherapy with COVID-19 severity and immune signatures: an observational study",
"author": "R Dalan",
"doi-asserted-by": "crossref",
"first-page": "e48",
"issue": "3",
"journal-title": "Eur Heart J Cardiovasc Pharmacother",
"key": "pone.0301056.ref027",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1111/dom.14805",
"article-title": "Re-examining the widespread policy of stopping sodium-glucose cotransporter-2 inhibitors during acute illness: A perspective based on the updated evidence",
"author": "K Khunti",
"doi-asserted-by": "crossref",
"first-page": "2071",
"issue": "11",
"journal-title": "Diabetes Obes Metab",
"key": "pone.0301056.ref028",
"volume": "24",
"year": "2022"
},
{
"article-title": "Croatian diabetes registry (CroDiab) and implementation of standardised diabetes checklists using Joint Action CHRODIS Recommendations and Criteria.",
"author": "T Poljicanin",
"first-page": "74",
"issue": "1",
"journal-title": "Ann Ist Super Sanita.",
"key": "pone.0301056.ref029",
"volume": "57",
"year": "2021"
},
{
"article-title": "CroDiab NET—registar osoba sa šećernom bolesti [CroDiab NET—electronic diabetes registry].",
"author": "T Poljicanin",
"first-page": "185",
"issue": "3",
"journal-title": "Acta Med Croatica.",
"key": "pone.0301056.ref030",
"volume": "59",
"year": "2005"
},
{
"article-title": "National public health information system in Croatia",
"author": "T Poljičanin",
"journal-title": "International Public Health Conference \"Health indicators as an important tool for strengthening health information systems in the European Region\" Tirana, Albania",
"key": "pone.0301056.ref031",
"year": "2016"
},
{
"DOI": "10.1016/j.ijmedinf.2005.08.007",
"article-title": "Primary healthcare information system—the cornerstone for the next generation healthcare sector in Republic of Croatia.",
"author": "M Koncar",
"doi-asserted-by": "crossref",
"first-page": "306",
"issue": "3–4",
"journal-title": "Int J Med Inform",
"key": "pone.0301056.ref032",
"volume": "75",
"year": "2006"
},
{
"DOI": "10.3325/cmj.2020.61.481",
"article-title": "Surveillance system for coronavirus disease 2019 epidemiological parameters in Croatia.",
"author": "K Capak",
"doi-asserted-by": "crossref",
"first-page": "481",
"issue": "6",
"journal-title": "Croat Med J",
"key": "pone.0301056.ref033",
"volume": "61",
"year": "2020"
},
{
"article-title": "Značaj digitalizacije podataka prijave uzroka smrti za unapređenje kvalitete epidemiološkog nadzora [Role of digitalized death reports in epidemiological surveillance quality] Med.",
"author": "N Antoljak",
"first-page": "95",
"journal-title": "inform.",
"key": "pone.0301056.ref034",
"volume": "15",
"year": "2021"
},
{
"article-title": "National Registry of Patients with Diabetes (CroDiab).",
"author": "Croatian Institute of Public Health (CIPH).",
"journal-title": "Report for year",
"key": "pone.0301056.ref035",
"year": "2020"
},
{
"DOI": "10.1093/ckj/sfz007",
"article-title": "Clarifying the concept of chronic kidney disease for non-nephrologists.",
"author": "MV Perez-Gomez",
"doi-asserted-by": "crossref",
"first-page": "258",
"issue": "2",
"journal-title": "Clin Kidney J.",
"key": "pone.0301056.ref036",
"volume": "12",
"year": "2019"
},
{
"DOI": "10.1186/s13098-023-01126-6",
"article-title": "Treatment patterns of antidiabetic and kidney protective therapies among patients with type 2 diabetes mellitus and chronic kidney disease in Colombia.",
"author": "ME Machado-Duque",
"doi-asserted-by": "crossref",
"first-page": "150",
"issue": "1",
"journal-title": "The KDICO descriptive study. Diabetol Metab Syndr",
"key": "pone.0301056.ref037",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1093/ndt/gfac140",
"article-title": "High unmet treatment needs in patients with chronic kidney disease and type 2 diabetes: real-world evidence from a US claims database",
"author": "L Fried",
"doi-asserted-by": "crossref",
"first-page": "630",
"issue": "3",
"journal-title": "Nephrol Dial Transplant",
"key": "pone.0301056.ref038",
"volume": "38",
"year": "2023"
},
{
"DOI": "10.2337/dc22-0614",
"article-title": "Prescription Patterns of Cardiovascular- and Kidney-Protective Therapies Among Patients With Type 2 Diabetes and Chronic Kidney Disease",
"author": "JA Lamprea-Montealegre",
"doi-asserted-by": "crossref",
"first-page": "2900",
"issue": "12",
"journal-title": "Diabetes Care",
"key": "pone.0301056.ref039",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.1186/s12933-020-01154-w",
"article-title": "Worldwide inertia to the use of cardiorenal protective glucose-lowering drugs (SGLT2i and GLP-1 RA) in high-risk patients with type 2 diabetes.",
"author": "G Schernthaner",
"doi-asserted-by": "crossref",
"first-page": "185",
"issue": "1",
"journal-title": "Cardiovasc Diabetol",
"key": "pone.0301056.ref040",
"volume": "19",
"year": "2020"
},
{
"author": "AstraZeneca",
"journal-title": "Forxiga approved in the EU for the treatment of chronic kidney disease in patients with and without type-2 diabetes",
"key": "pone.0301056.ref041",
"year": "2021"
},
{
"author": "Boehringer Ingelheim",
"journal-title": "Jardiance® (empagliflozin) approved in the EU for the treatment of adults with chronic kidney disease",
"key": "pone.0301056.ref042",
"year": "2023"
},
{
"DOI": "10.3390/jcm12103377",
"article-title": "Nephroprotective Properties of Antidiabetic Drugs.",
"author": "C Gerdes",
"doi-asserted-by": "crossref",
"first-page": "3377",
"issue": "10",
"journal-title": "J Clin Med.",
"key": "pone.0301056.ref043",
"volume": "12",
"year": "2023"
},
{
"DOI": "10.1016/j.diabres.2022.110205",
"article-title": "Pre-admission use of sodium glucose transporter-2 inhibitor (SGLT-2i) may significantly improves Covid-19 outcomes in patients with diabetes: A systematic review, meta-analysis, and meta-regression.",
"author": "H Permana",
"doi-asserted-by": "crossref",
"first-page": "110205",
"journal-title": "Diabetes Res Clin Pract",
"key": "pone.0301056.ref044",
"volume": "195",
"year": "2023"
},
{
"DOI": "10.3389/fendo.2022.895458",
"article-title": "The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis.",
"author": "Y Chen",
"doi-asserted-by": "crossref",
"first-page": "895458",
"journal-title": "Front Endocrinol (Lausanne).",
"key": "pone.0301056.ref045",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1111/1753-0407.13135",
"article-title": "The potential effects of clinical antidiabetic agents on SARS-CoV-2",
"author": "H Qu",
"doi-asserted-by": "crossref",
"first-page": "243",
"issue": "3",
"journal-title": "J Diabetes",
"key": "pone.0301056.ref046",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2021.708494",
"article-title": "Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis.",
"author": "C Kan",
"doi-asserted-by": "crossref",
"first-page": "708494",
"journal-title": "Front Endocrinol (Lausanne).",
"key": "pone.0301056.ref047",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1111/1753-0407.13359",
"article-title": "Noninsulin-based antihyperglycemic medications in patients with diabetes and COVID-19: A systematic review and meta-analysis.",
"author": "M Nassar",
"doi-asserted-by": "crossref",
"first-page": "86",
"issue": "2",
"journal-title": "J Diabetes.",
"key": "pone.0301056.ref048",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1111/bcp.15258",
"article-title": "Does metformin affect outcomes in COVID-19 patients with new or pre-existing diabetes mellitus? A systematic review and meta-analysis",
"author": "A Ganesh",
"doi-asserted-by": "crossref",
"first-page": "2642",
"issue": "6",
"journal-title": "Br J Clin Pharmacol",
"key": "pone.0301056.ref049",
"volume": "88",
"year": "2022"
},
{
"DOI": "10.1016/j.diabres.2021.109031",
"article-title": "Pre-admission glucagon-like peptide-1 receptor agonist (GLP-1RA) and mortality from coronavirus disease 2019 (Covid-19): A systematic review, meta-analysis, and meta-regression.",
"author": "TI Hariyanto",
"doi-asserted-by": "crossref",
"first-page": "109031",
"journal-title": "Diabetes Res Clin Pract",
"key": "pone.0301056.ref050",
"volume": "179",
"year": "2021"
},
{
"DOI": "10.1016/j.obmed.2020.100312",
"article-title": "Friend or foe? ACE2 inhibitors and GLP-1R agonists in COVID-19 treatment.",
"author": "J Pang",
"doi-asserted-by": "crossref",
"first-page": "100312",
"journal-title": "Obes Med.",
"key": "pone.0301056.ref051",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1111/cob.12439",
"article-title": "Glucagon-like peptide-1 receptor agonists in the era of COVID-19: Friend or foe?",
"author": "A Belančić",
"doi-asserted-by": "crossref",
"first-page": "e12439",
"issue": "2",
"journal-title": "Clin Obes.",
"key": "pone.0301056.ref052",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.metabol.2022.155196",
"article-title": "Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis",
"author": "NN Nguyen",
"doi-asserted-by": "crossref",
"first-page": "155196",
"journal-title": "Metabolism",
"key": "pone.0301056.ref053",
"volume": "131",
"year": "2022"
},
{
"DOI": "10.5501/wjv.v11.i6.399",
"article-title": "Dipeptidyl peptidase 4 inhibitors in COVID-19: Beyond glycemic control",
"author": "N Narayanan",
"doi-asserted-by": "crossref",
"first-page": "399",
"issue": "6",
"journal-title": "World J Virol",
"key": "pone.0301056.ref054",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"article-title": "Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England.",
"author": "K Khunti",
"doi-asserted-by": "crossref",
"first-page": "293",
"issue": "5",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "pone.0301056.ref055",
"volume": "9",
"year": "2021"
},
{
"article-title": "Core Standards of the EUBIROD Project",
"author": "SG Cunningham",
"first-page": "166",
"issue": "2",
"journal-title": "Defining a European Diabetes Data Dictionary for Clinical Audit and Healthcare Delivery. Methods Inf Med",
"key": "pone.0301056.ref056",
"volume": "55",
"year": "2016"
},
{
"DOI": "10.3389/fcdhc.2021.704807",
"article-title": "COVID-19 Pandemic Influence on Diabetes Management in Croatia.",
"author": "I Cerovečki",
"doi-asserted-by": "crossref",
"first-page": "704807",
"journal-title": "Front Clin Diabetes Healthc",
"key": "pone.0301056.ref057",
"volume": "2",
"year": "2021"
}
],
"reference-count": 57,
"references-count": 57,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0301056"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Association of anti-diabetic drugs and covid-19 outcomes in patients with diabetes mellitus type 2 and chronic kidney disease: Nationwide registry analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "19"
}
