The predictive power of serum vitamin D for poor outcomes in COVID-19 patients
et al., Food Science & Nutrition, doi:10.1002/fsn3.2591, Sep 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 290 hospitalized patients in Iran, showing higher mortality with vitamin D deficiency.
This is the 96th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
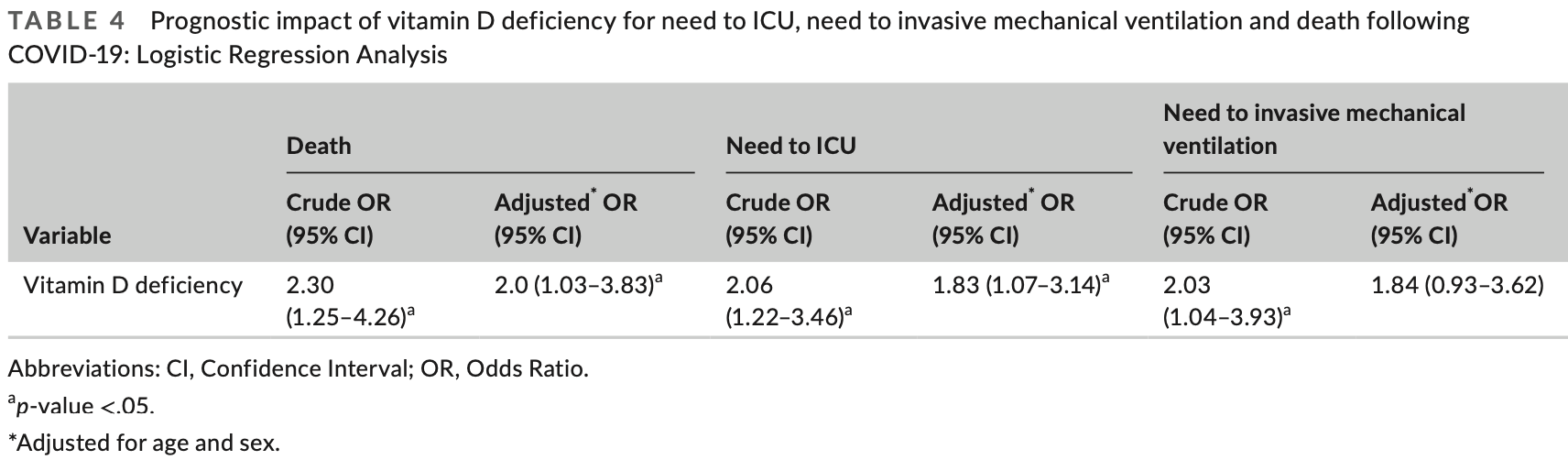
risk of death, 44.8% lower, RR 0.55, p = 0.046, high D levels 148, low D levels 142, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk, control prevalance approximated with overall prevalence.
|
|
risk of mechanical ventilation, 41.7% lower, RR 0.58, p = 0.09, high D levels 148, low D levels 142, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk, control prevalance approximated with overall prevalence.
|
|
risk of ICU admission, 37.3% lower, RR 0.63, p = 0.04, high D levels 148, low D levels 142, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk, control prevalance approximated with overall prevalence.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Derakhshanian et al., 19 Sep 2021, retrospective, Iran, peer-reviewed, 11 authors.
The predictive power of serum vitamin D for poor outcomes in COVID‐19 patients
Food Science & Nutrition, doi:10.1002/fsn3.2591
Considering the high prevalence of vitamin D deficiency worldwide and its relationship with immune response to viral infections, this study attempted to identify the predictive power of serum vitamin D for poor outcomes among the COVID-19 patients. This retrospective cohort study included all patients with confirmed COVID-19 hospitalized between February 20, 2020, and April 20, 2020, at a designated COVID-19 hospital, located in Tehran province, Iran. General characteristics, medical history and clinical symptoms were recorded by trained physicians. Blood parameters including complete blood count, creatinine, lactate dehydrogenase, creatine phosphokinase, erythrocyte sedimentation rate, C-reactive protein and vitamin D were tested. This study included 290 hospitalized patients with COVID-19 (the mean age [SD]: 61.6 [16.9], 56.6% males), of whom 142 had vitamin D concentrations less than 20 ng/ml, defined as vitamin D deficiency. COVID-19 patients with vitamin D deficiency were more likely to die (Crude OR [95% CI]: 2.30 [1.25-4.26]), require ICU (2.06 [1.22-3.46]) and invasive mechanical ventilation (2.03 [1.04-3.93]) based on univariate logistic regression results. Although, after adjusting for potentials confounders such as gender and age, the association between vitamin D and need to invasive mechanical ventilation lost its significance, adjusted values for the risk of death and ICU requirement were still statistically significant. Vitamin D deficiency can be considered as a predictor of poor outcomes and mortality in COVID-19 patients. Therefore, checking serum 25 (OH) D on admission and taking vitamin D supplements according to the prophylactic or treatment protocols is recommended for all COVID-19 patients.
Ethics Committee of Alborz University of Medical Sciences (ABZUMS) and Iran University of Medical Sciences (IUMS). All participants signed written informed consent forms.
CO N S E NT FO R PU B LI C ATI O N The authors would like to advise that all authors listed have contributed to the work. All authors have agreed to submit the manuscript to Food Science and Nutrition. No part of the work has been published before.
References
Ai, Yang, Hou, Zhan, Chen et al., Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases, Radiology
Alifano, Alifano, Forgez, Iannelli, Renin-angiotensin system at the heart of COVID-19 pandemic, Biochimie, doi:10.1016/j.biochi.2020.04.008
Alipio, Vitamin D supplementation could possibly improve clinical outcomes of patients infected with coronavirus
Aranow, Vitamin D and the immune system, Journal of Investigative Medicine, doi:10.2310/JIM.0b013e31821b8755
Beard, Bearden, Striker, Vitamin D and the antiviral state, Journal of Clinical Virology, doi:10.1016/j.jcv.2010.12.006
Cannell, Vieth, Umhau, Holick, Grant et al., Epidemic influenza and vitamin D, Epidemiology & Infection, doi:10.1017/S0950268806007175
Cantorna, Snyder, Lin, Yang, Vitamin D and 1, 25 (OH) 2D regulation of T cells, Nutrients, doi:10.3390/nu7043011
Covid C & Team, Severe outcomes among patients with coronavirus disease 2019 (COVID-19)-United States, MMWR. Morbidity and Mortality Weekly Report, doi:10.15585/mmwr.mm6912e2
Derakhshanian, Rastad, Ghosh, Zeinali, Ziaee et al., None
F I G U R E, Receiver operating characteristic curves of vitamin D deficiency and blood parameters for predicting COVID-19 death (a) and need to ICU care (b). CPK, Creatine phosphokinase; PT, prothrombin time survey, Archives of Internal Medicine, doi:10.1001/archinternmed.2008.560
Ginde, Mansbach, Camargo, Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the third national health and nutrition examination
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/nu12040988
Greiller, Martineau, Modulation of the immune response to respiratory viruses by vitamin D, Nutrients, doi:10.3390/nu7064240
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., None
Hewison, An update on vitamin D and human immunity, Clinical Endocrinology, doi:10.1111/j.1365-2265.2011.04261.x
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, The Lancet, doi:10.1016/S0140-6736(20)30183-5
Ji, Zhang, Xu, Chen, Yang et al., Prediction for progression risk in patients with COVID-19 pneumonia: The CALL score, Clinical Infectious Diseases, doi:10.1093/cid/ciaa414
Juzeniene, Ma, Kwitniewski, Polev, Lagunova et al., The seasonality of pandemic and non-pandemic influenzas: The roles of solar radiation and vitamin D, International Journal of Infectious Diseases, doi:10.1016/j.ijid.2010.09.002
Laaksi, Ruohola, Tuohimaa, Auvinen, Haataja et al., An association of serum vitamin D concentrations< 40 nmol/L with acute respiratory tract infection in young Finnish men, The American Journal of Clinical Nutrition
Mahdavi, Khalili, Davarpanah, Faghihi, Mahdavi et al., Radiologic management of COVID-19: Preliminary experience of the Iranian society of radiology COVID-19 consultant group (ISRCC), Iranian Journal of Radiology, doi:10.5812/iranjradiol.102324
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D deficiency and treatment with COVID-19 incidence
Mirzaasgari, The predictive power of serum vitamin D for poor outcomes in COVID-19 patients, Food Science & Nutrition
Rashedi, Poor, Asgharzadeh, Vitamin D3 administration to patients with confirmed COVID-19, Iranian Journal of Public Health, doi:10.18502/ijph.v49iS1.3690
Rhodes, Subramanian, Laird, Kenny, low population mortality from COVID-19 in countries south of latitude 35 degrees North-supports vitamin D as a factor determining severity, Alimentary Pharmacology & therapeutics
Rodriguez, Daniels, Gunawardene, Robbins, High frequency of vitamin D deficiency in ambulatory HIV-positive patients, AIDS Research and Human Retroviruses, doi:10.1089/aid.2008.0183
Schwalfenberg, A review of the critical role of vitamin D in the functioning of the immune system and the clinical implications of vitamin D deficiency, Molecular Nutrition & Food Research, doi:10.1002/mnfr.201000174
Villamor, A potential role for vitamin D on HIV infection?, Nutrition Reviews, doi:10.1111/j.1753-4887.2006.tb00205.x
Wei, Christakos, Mechanisms underlying the regulation of innate and adaptive immunity by vitamin D, Nutrients, doi:10.3390/nu7105392
Wu, Leung, Bushman, Kishore, Niehus et al., Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan. China, Nature Medicine, doi:10.1038/s41591-020-0822-7
DOI record:
{
"DOI": "10.1002/fsn3.2591",
"ISSN": [
"2048-7177",
"2048-7177"
],
"URL": "http://dx.doi.org/10.1002/fsn3.2591",
"abstract": "<jats:title>Abstract</jats:title><jats:p>Considering the high prevalence of vitamin D deficiency worldwide and its relationship with immune response to viral infections, this study attempted to identify the predictive power of serum vitamin D for poor outcomes among the COVID‐19 patients. This retrospective cohort study included all patients with confirmed COVID‐19 hospitalized between February 20, 2020, and April 20, 2020, at a designated COVID‐19 hospital, located in Tehran province, Iran. General characteristics, medical history and clinical symptoms were recorded by trained physicians. Blood parameters including complete blood count, creatinine, lactate dehydrogenase, creatine phosphokinase, erythrocyte sedimentation rate, C‐reactive protein and vitamin D were tested. This study included 290 hospitalized patients with COVID‐19 (the mean age [<jats:italic>SD</jats:italic>]: 61.6 [16.9], 56.6% males), of whom 142 had vitamin D concentrations less than 20 ng/ml, defined as vitamin D deficiency. COVID‐19 patients with vitamin D deficiency were more likely to die (Crude OR [95% CI]: 2.30 [1.25–4.26]), require ICU (2.06 [1.22–3.46]) and invasive mechanical ventilation (2.03 [1.04–3.93]) based on univariate logistic regression results. Although, after adjusting for potentials confounders such as gender and age, the association between vitamin D and need to invasive mechanical ventilation lost its significance, adjusted values for the risk of death and ICU requirement were still statistically significant. Vitamin D deficiency can be considered as a predictor of poor outcomes and mortality in COVID‐19 patients. Therefore, checking serum 25 (OH) D on admission and taking vitamin D supplements according to the prophylactic or treatment protocols is recommended for all COVID‐19 patients.</jats:p>",
"alternative-id": [
"10.1002/fsn3.2591"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2021-01-29"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2021-08-27"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2021-09-19"
}
],
"author": [
{
"affiliation": [
{
"name": "Department of Biochemistry Genetics and Nutrition School of Medicine Alborz University of Medical Sciences Karaj Iran"
},
{
"name": "Dietary Supplements and Probiotic Research Center Alborz University of Medical Sciences Karaj Iran"
}
],
"family": "Derakhshanian",
"given": "Hoda",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Non‐communicable Diseases Research Center Alborz University of Medical Sciences Karaj Iran"
}
],
"family": "Rastad",
"given": "Hadith",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Biology Okanagan Campus University of British Columbia Kelowna BC Canada"
}
],
"family": "Ghosh",
"given": "Sanjoy",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Neurology Firoozgar Hospital Iran University of Medical Sciences Tehran Iran"
}
],
"family": "Zeinali",
"given": "Marjan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Neurology Firoozgar Hospital Iran University of Medical Sciences Tehran Iran"
}
],
"family": "Ziaee",
"given": "Mahsa",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Neurology Firoozgar Hospital Iran University of Medical Sciences Tehran Iran"
}
],
"family": "Khoeini",
"given": "Tara",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine Firoozgar Hospital Iran University of Medical Sciences Tehran Iran"
}
],
"family": "Farrokhpour",
"given": "Mohsen",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9465-7588",
"affiliation": [
{
"name": "Non‐communicable Diseases Research Center Alborz University of Medical Sciences Karaj Iran"
}
],
"authenticated-orcid": false,
"family": "Qorbani",
"given": "Mostafa",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Research Development Unit Shahid Rajaei Educational and Medical Center Alborz University of Medical Sciences Karaj Iran"
}
],
"family": "Ramezani Ghamsari",
"given": "Mona",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Community Nutrition School of Nutritional Sciences and Dietetics Tehran University of Medical Sciences Tehran Iran"
}
],
"family": "Hasani",
"given": "Hossein",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4046-8471",
"affiliation": [
{
"name": "Department of Neurology Firoozgar Hospital Iran University of Medical Sciences Tehran Iran"
},
{
"name": "Shefa Neuroscience Research Center Tehran Iran"
}
],
"authenticated-orcid": false,
"family": "Mirzaasgari",
"given": "Zahra",
"sequence": "additional"
}
],
"container-title": "Food Science & Nutrition",
"container-title-short": "Food Science & Nutrition",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2021,
9,
20
]
],
"date-time": "2021-09-20T05:20:44Z",
"timestamp": 1632115244000
},
"deposited": {
"date-parts": [
[
2023,
8,
28
]
],
"date-time": "2023-08-28T09:17:47Z",
"timestamp": 1693214267000
},
"funder": [
{
"DOI": "10.13039/501100012411",
"doi-asserted-by": "publisher",
"name": "Alborz University of Medical Sciences"
},
{
"DOI": "10.13039/501100006766",
"doi-asserted-by": "publisher",
"name": "Iran University of Science and Technology"
}
],
"indexed": {
"date-parts": [
[
2023,
9,
14
]
],
"date-time": "2023-09-14T16:55:46Z",
"timestamp": 1694710546093
},
"is-referenced-by-count": 6,
"issue": "11",
"issued": {
"date-parts": [
[
2021,
9,
19
]
]
},
"journal-issue": {
"issue": "11",
"published-print": {
"date-parts": [
[
2021,
11
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
19
]
],
"date-time": "2021-09-19T00:00:00Z",
"timestamp": 1632009600000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/fsn3.2591",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/full-xml/10.1002/fsn3.2591",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/fsn3.2591",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"page": "6307-6313",
"prefix": "10.1002",
"published": {
"date-parts": [
[
2021,
9,
19
]
]
},
"published-online": {
"date-parts": [
[
2021,
9,
19
]
]
},
"published-print": {
"date-parts": [
[
2021,
11
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.1148/radiol.2020200642",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_2_1"
},
{
"DOI": "10.1016/j.biochi.2020.04.008",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_3_1"
},
{
"author": "Alipio M.",
"key": "e_1_2_10_4_1",
"volume-title": "Vitamin D supplementation could possibly improve clinical outcomes of patients infected with coronavirus‐2019 (COVID‐19)",
"year": "2020"
},
{
"DOI": "10.2310/JIM.0b013e31821b8755",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_5_1"
},
{
"DOI": "10.1016/j.jcv.2010.12.006",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_6_1"
},
{
"DOI": "10.1017/S0950268806007175",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_7_1"
},
{
"DOI": "10.3390/nu7043011",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_8_1"
},
{
"DOI": "10.15585/mmwr.mm6912e2",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_9_1"
},
{
"DOI": "10.1001/archinternmed.2008.560",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_10_1"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_11_1"
},
{
"DOI": "10.3390/nu7064240",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_12_1"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_13_1"
},
{
"DOI": "10.1111/j.1365‐2265.2011.04261.x",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_14_1"
},
{
"DOI": "10.1016/S0140‐6736(20)30183‐5",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_15_1"
},
{
"DOI": "10.1093/cid/ciaa414",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_16_1"
},
{
"DOI": "10.1016/j.ijid.2010.09.002",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_17_1"
},
{
"DOI": "10.1093/ajcn/86.3.714",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_18_1"
},
{
"DOI": "10.5812/iranjradiol.102324",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_19_1"
},
{
"article-title": "Association of vitamin D deficiency and treatment with COVID‐19 incidence",
"author": "Meltzer D. O.",
"journal-title": "medRxiv",
"key": "e_1_2_10_20_1",
"year": "2020"
},
{
"DOI": "10.18502/ijph.v49iS1.3690",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_21_1"
},
{
"DOI": "10.1111/apt.15777",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_22_1"
},
{
"DOI": "10.1089/aid.2008.0183",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_23_1"
},
{
"DOI": "10.1002/mnfr.201000174",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_24_1"
},
{
"DOI": "10.1111/j.1753‐4887.2006.tb00205.x",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_25_1"
},
{
"DOI": "10.3390/nu7105392",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_26_1"
},
{
"DOI": "10.1038/s41591‐020‐0822‐7",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_27_1"
}
],
"reference-count": 26,
"references-count": 26,
"relation": {},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1002/fsn3.2591"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science"
],
"subtitle": [],
"title": "The predictive power of serum vitamin D for poor outcomes in COVID‐19 patients",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy",
"volume": "9"
}
