A Pilot Study of Short-Course Oral Vitamin A and Aerosolised Diffuser Olfactory Training for the Treatment of Smell Loss in Long COVID
et al., Brain Sciences, doi:10.3390/brainsci13071014, NCT04900415, Jun 2023
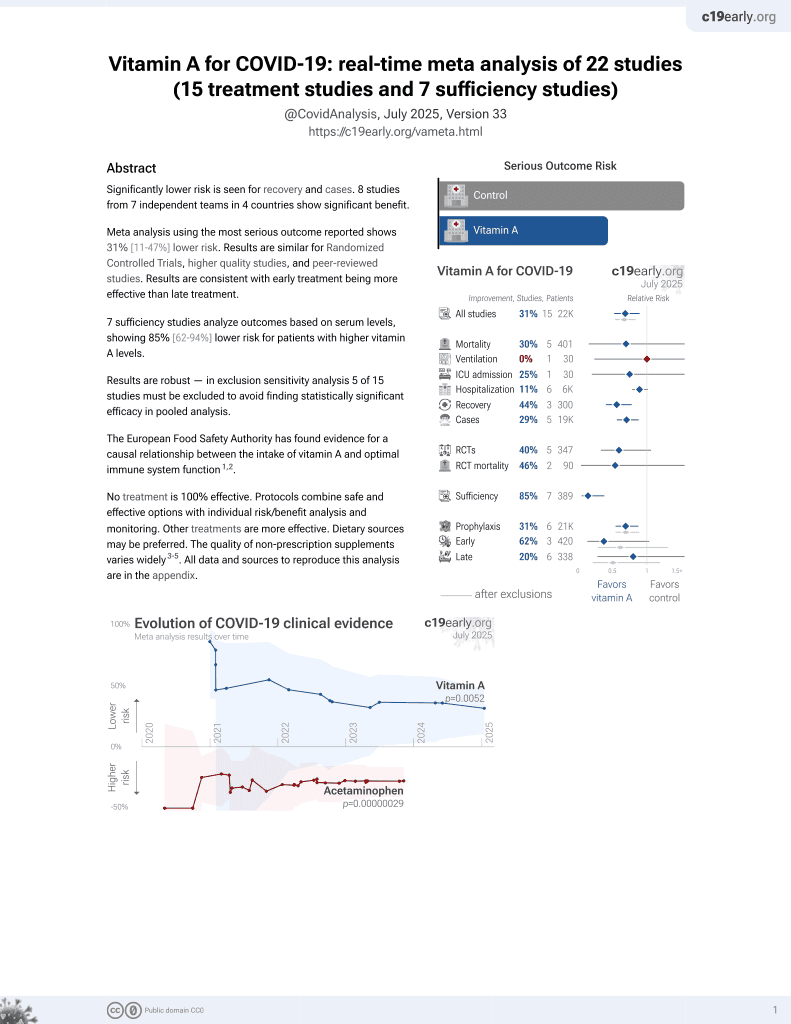
Vitamin A for COVID-19
49th treatment shown to reduce risk in
May 2023, now with p = 0.004 from 14 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
RCT 24 patients with olfactory dysfunction post-COVID-19 in Hong Kong, showing significantly improved recovery with the addition of vitamin A to aerosolised diffuser olfactory training. 25,000IU vitamin A for 14 days.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
|
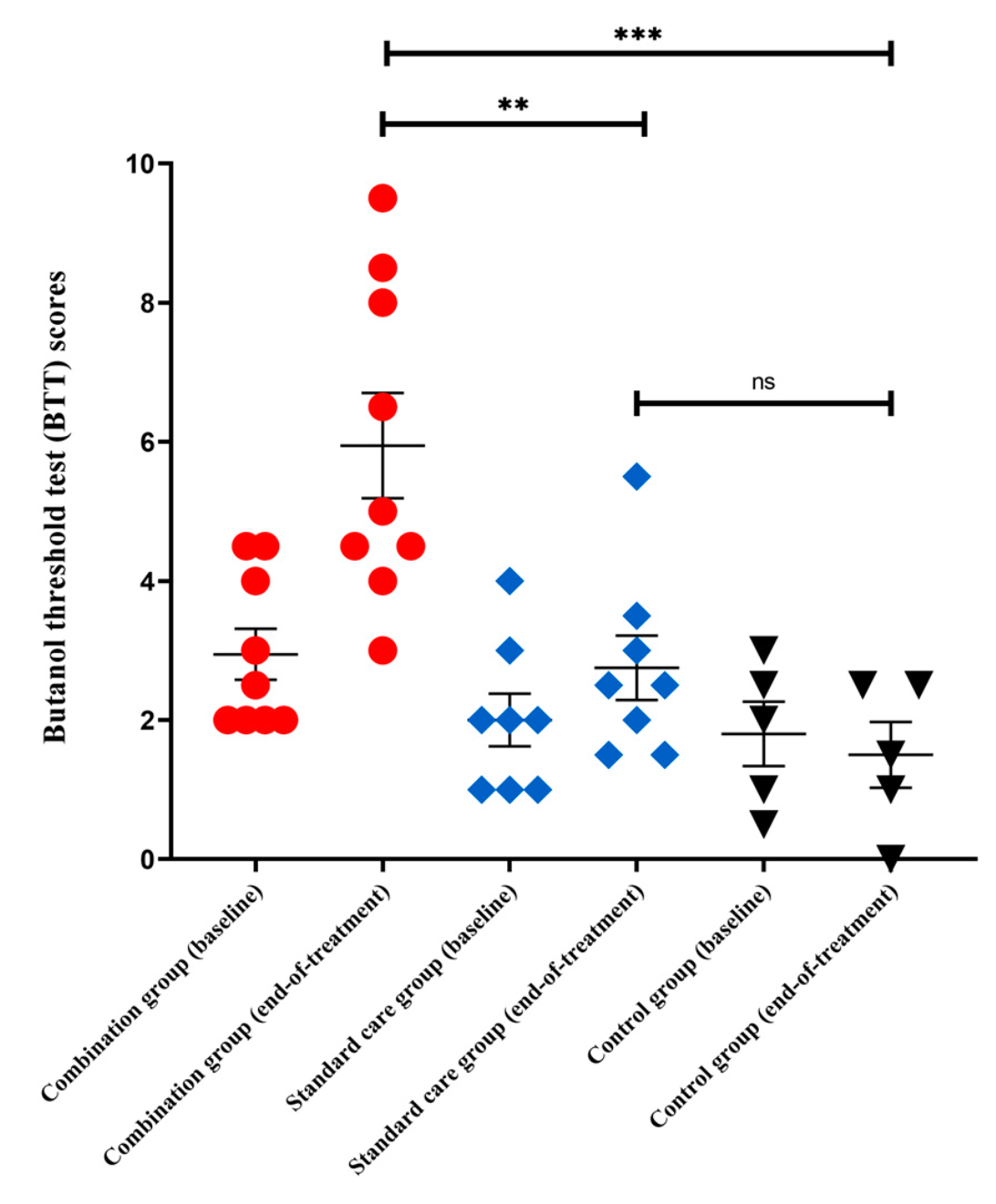
relative BTT improvement, 75.1% better, RR 0.25, p = 0.048, treatment mean 3.01 (±2.52) n=9, control mean 0.75 (±1.67) n=8, vitamin A + OT vs. OT.
|
|
anosmia, 68.0% lower, RR 0.32, p = 0.47, treatment 0 of 9 (0.0%), control 1 of 8 (12.5%), NNT 8.0, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), vitamin A + OT vs. OT.
|
|
severe microsmia, 70.4% lower, RR 0.30, p = 0.29, treatment 1 of 9 (11.1%), control 3 of 8 (37.5%), NNT 3.8, vitamin A + OT vs. OT.
|
|
moderate microsmia, 74.6% lower, RR 0.25, p = 0.02, treatment 2 of 9 (22.2%), control 7 of 8 (87.5%), NNT 1.5, vitamin A + OT vs. OT.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Chung et al., 30 Jun 2023, Randomized Controlled Trial, China, peer-reviewed, 14 authors, study period 14 August, 2020 - 11 June, 2021, trial NCT04900415 (history).
Contact: tomwhc@hku.hk (corresponding author), ivanhung@hku.hk, makkf@hku.hk.
A Pilot Study of Short-Course Oral Vitamin A and Aerosolised Diffuser Olfactory Training for the Treatment of Smell Loss in Long COVID
Brain Sciences, doi:10.3390/brainsci13071014
Background: Olfactory dysfunction (OD) is a common neurosensory manifestation in long COVID. An effective and safe treatment against COVID-19-related OD is needed. Methods: This pilot trial recruited long COVID patients with persistent OD. Participants were randomly assigned to receive short-course (14 days) oral vitamin A (VitA; 25,000 IU per day) and aerosolised diffuser olfactory training (OT) thrice daily (combination), OT alone (standard care), or observation (control) for 4 weeks. The primary outcome was differences in olfactory function by butanol threshold tests (BTT) between baseline and end-of-treatment. Secondary outcomes included smell identification tests (SIT), structural MRI brain, and serial seed-based functional connectivity (FC) analyses in the olfactory cortical network by resting-state functional MRI (rs-fMRI). Results: A total of 24 participants were randomly assigned to receive either combination treatment (n = 10), standard care (n = 9), or control (n = 5). Median OD duration was 157 days (IQR 127-175). Mean baseline BTT score was 2.3 (SD 1.1). At end-of-treatment, mean BTT scores were significantly higher for the combination group than control (p < 0.001, MD = 4.4, 95% CI 1.7 to 7.2) and standard care (p = 0.009) groups. Interval SIT scores increased significantly (p = 0.009) in the combination group. rs-fMRI showed significantly higher FC in the combination group when compared to other groups. At end-of-treatment, positive correlations were found in the increased FC at left inferior frontal gyrus and clinically significant improvements in measured BTT (r = 0.858, p < 0.001) and SIT (r = 0.548, p = 0.042) scores for the combination group. Conclusions: Short-course oral VitA and aerosolised diffuser OT was effective as a combination treatment for persistent OD in long COVID.
References
Abdelalim, Mohamady, Elsayed, Elawady, Ghallab, Corticosteroid nasal spray for recovery of smell sensation in COVID-19 patients: A randomized controlled trial, Am. J. Otolaryngol. 2021, doi:10.1016/j.amjoto.2020.102884
Addison, Wong, Ahmed, Macchi, Konstantinidis et al., Clinical Olfactory Working Group consensus statement on the treatment of postinfectious olfactory dysfunction, J. Allergy Clin. Immunol, doi:10.1016/j.jaci.2020.12.641
Al Aïn, Poupon, Hétu, Mercier, Steffener et al., Smell training improves olfactory function and alters brain structure, Neuroimage, doi:10.1016/j.neuroimage.2019.01.008
Ashburner, A fast diffeomorphic image registration algorithm, Neuroimage, doi:10.1016/j.neuroimage.2007.07.007
Brann, Tsukahara, Weinreb, Lipovsek, Van Den Berge et al., Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia, doi:10.1126/sciadv.abc5801
Bryche, St Albin, Murri, Lacôte, Pulido et al., Massive transient damage of the olfactory epithelium associated with infection of sustentacular cells by SARS-CoV-2 in golden Syrian hamsters, Brain Behav. Immun, doi:10.1016/j.bbi.2020.06.032
Cain, Gent, Goodspeed, Leonard, Evaluation of olfactory dysfunction in the Connecticut Chemosensory Clinical Research Center, Laryngoscope, doi:10.1288/00005537-198801000-00017
Chan, -W.; Yuan, Kok, To, Chu et al., A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster, Lancet, doi:10.1016/S0140-6736(20)30154-9
Chu, Chan, Yuen, Shuai, Yuan et al., Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: An observational study, Lancet Microbe, doi:10.1016/S2666-5247(20)30004-5
Chung, Sridhar, Zhang, Chan, Li et al., Olfactory Dysfunction in Coronavirus Disease 2019 Patients: Observational Cohort Study and Systematic Review, Open. Forum Infect. Dis, doi:10.1093/ofid/ofaa199
Chung, Zhang, Wong, Sridhar, Chan et al., Neurosensory Rehabilitation and Olfactory Network Recovery in Covid-19-related Olfactory Dysfunction, Brain Sci
Damm, Pikart, Reimann, Burkert, Göktas et al., Olfactory training is helpful in postinfectious olfactory loss: A randomized, controlled, multicenter study, Laryngoscope, doi:10.1002/lary.24340
Davis, Assaf, Mccorkell, Wei, Low et al., Characterizing long COVID in an international cohort: 7 months of symptoms and their impact, EClinicalMedicine, doi:10.1016/j.eclinm.2021.101019
Doty, Shaman, Dann, Development of the University of Pennsylvania Smell Identification Test: A standardized microencapsulated test of olfactory function, Physiol. Behav, doi:10.1016/0031-9384(84)90269-5
Duncan, Briggs, Treatment of Uncomplicated Anosmia by Vitamin A, Arch. Otolaryngol, doi:10.1001/archotol.1962.00740040122008
Ercoli, Masala, Pinna, Orofino, Solla et al., Qualitative smell/taste disorders as sequelae of acute COVID-19, Neurol. Sci. 2021, doi:10.1007/s10072-021-05611-6
Everett, Lean, Byrne, Van Diemen, Rhodes et al., Intranasal Infection of Ferrets with SARS-CoV-2 as a Model for Asymptomatic Human Infection
Fjaeldstad, Fernandes, Van Hartevelt, Gleesborg, Møller et al., Brain fingerprints of olfaction: A novel structural method for assessing olfactory cortical networks in health and disease, Sci. Rep
Guan, Ni, Hu, Liang, Ou et al., Clinical Characteristics of coronavirus disease 2019 in China, N. Engl. J. Med, doi:10.1056/NEJMoa2002032
Herrick, Lin, Peterson, Schnittke, Schwob, Notch1 maintains dormancy of olfactory horizontal basal cells, a reserve neural stem cell, Proc. Natl. Acad. Sci, doi:10.1073/pnas.1701333114
Hopkins, Alanin, Philpott, Harries, Whitcroft et al., Management of new onset loss of sense of smell during the COVID-19 pandemic-BRS Consensus Guidelines, Clin. Otolaryngol, doi:10.1111/coa.13636
Huang, Huang, Wang, Li, Ren et al., 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study, Lancet, doi:10.1016/S0140-6736(20)32656-8
Huiming, Chaomin, Meng, Vitamin A for treating measles in children, Cochrane Database Syst Rev
Hummel, Whitcroft, Rueter, Haehner, Intranasal vitamin A is beneficial in post-infectious olfactory loss, Eur. Arch. Otorhinolaryngol, doi:10.1007/s00405-017-4576-x
Hussey, Klein, Randomized, Controlled Trial of Vitamin A in Children with Severe Measles, N. Engl. J. Med, doi:10.1056/NEJM199007193230304
Jiao, Yang, Yu, Zhao, Long et al., The olfactory route is a potential way for SARS-CoV-2 to invade the central nervous system of rhesus monkeys, Signal. Transduct. Target, doi:10.1038/s41392-021-00591-7
Karnath, New insights into the functions of the superior temporal cortex, Nat. Rev. Neurosci, doi:10.1038/35086057
Kartal, Yaşar, Kartal, Özcan, Borlu, Effects of isotretinoin on the olfactory function in patients with acne, Bras. Derm, doi:10.1590/abd1806-4841.20175483
Karunanayaka, Wilson, Tobia, Martinez, Meadowcroft et al., Default mode network deactivation during odor-visual association, Brain Mapp, doi:10.1002/hbm.23440
Kasiri, Rouhani, Salehifar, Ghazaeian, Fallah, Mometasone furoate nasal spray in the treatment of patients with COVID-19 olfactory dysfunction: A randomized, double blind clinical trial, Int. Immunopharmacol, doi:10.1016/j.intimp.2021.107871
Kirschenbaum, Imbach, Ulrich, Rushing, Keller et al., Inflammatory olfactory neuropathy in two patients with COVID-19, Lancet, doi:10.1016/S0140-6736(20)31525-7
Kollndorfer, Fischmeister, Kowalczyk, Hoche, Mueller et al., Olfactory training induces changes in regional functional connectivity in patients with long-term smell loss, NeuroImage Clin, doi:10.1016/j.nicl.2015.09.004
Kollndorfer, Kowalczyk, Hoche, Mueller, Pollak et al., Recovery of Olfactory Function Induces Neuroplasticity Effects in Patients with Smell Loss, Neural Plast, doi:10.1155/2014/140419
Langdon, Lehrer, Berenguer, Laxe, Alobid et al., Olfactory Training in Post-Traumatic Smell Impairment: Mild Improvement in Threshold Performances: Results from a Randomized Controlled Trial, J. Neurotrauma, doi:10.1089/neu.2017.5230
Leung, Coulombe, Reed, Contribution of olfactory neural stem cells to tissue maintenance and regeneration, Nat. Neurosci, doi:10.1038/nn1882
Lu, Yang, Zhang, Eslinger, Zhang et al., Disruptions of the olfactory and default mode networks in Alzheimer's disease, Brain Behav, doi:10.1002/brb3.1296
Margulies, Kelly, Uddin, Biswal, Castellanos et al., Mapping the functional connectivity of anterior cingulate cortex, Neuroimage, doi:10.1016/j.neuroimage.2007.05.019
Matschke, Lütgehetmann, Hagel, Sperhake, Schröder et al., Neuropathology of patients with COVID-19 in Germany: A post-mortem case series, Lancet Neurol, doi:10.1016/S1474-4422(20)30308-2
Meinhardt, Radke, Dittmayer, Franz, Thomas et al., Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19, Nat. Neurosci, doi:10.1038/s41593-020-00758-5
Menni, Valdes, Polidori, Antonelli, Penamakuri et al., Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: A prospective observational study from the ZOE COVID Study, Lancet, doi:10.1016/S0140-6736(22)00327-0
Moffett, Ross, Arun, Madhavarao, Namboodiri, N-Acetylaspartate in the CNS: From neurodiagnostics to neurobiology, Prog. Neurobiol, doi:10.1016/j.pneurobio.2006.12.003
Oz, Alger, Barker, Bartha, Bizzi et al., Clinical proton MR spectroscopy in central nervous system disorders, Radiology, doi:10.1148/radiol.13130531
Paschaki, Cammas, Muta, Matsuoka, Mak et al., Retinoic acid regulates olfactory progenitor cell fate and differentiation, Neural Dev, doi:10.1186/1749-8104-8-13
Peterson, Lin, Barrios-Camacho, Herrick, Holbrook et al., Activating a Reserve Neural Stem Cell Population In Vitro Enables Engraftment and Multipotency after Transplantation, Stem Cell. Rep, doi:10.1016/j.stemcr.2019.02.014
Psaltis, Li, Vaezeafshar, Cho, Hwang, Modification of the lund-kennedy endoscopic scoring system improves its reliability and correlation with patient-reported outcome measures, Laryngoscope, doi:10.1002/lary.24654
Rashid, Zgair, Al-Ani, Effect of nasal corticosteroid in the treatment of anosmia due to COVID-19: A randomised double-blind placebo-controlled study, Am. J. Otolaryngol. 2021, doi:10.1016/j.amjoto.2021.103033
Reden, Lill, Zahnert, Haehner, Hummel, Olfactory function in patients with postinfectious and posttraumatic smell disorders before and after treatment with vitamin A: A double-blind, placebo-controlled, randomized clinical trial, Laryngoscope, doi:10.1002/lary.23405
Reichert, Schöpf, Olfactory Loss and Regain: Lessons for Neuroplasticity, doi:10.1177/1073858417703910
Royet, Koenig, Gregoire, Cinotti, Lavenne et al., Functional anatomy of perceptual and semantic processing for odors, J. Cogn. Neurosci, doi:10.1162/089892999563166
Savic, Berglund, Passive perception of odors and semantic circuits, Hum. Brain Mapp, doi:10.1002/hbm.20009
Schurink, Roos, Radonic, Barbe, Bouman et al., Viral presence and immunopathology in patients with lethal COVID-19: A prospective autopsy cohort study, Lancet Microbe, doi:10.1016/S2666-5247(20)30144-0
Shearer, Stoney, Morgan, Mccaffery, A vitamin for the brain, Trends Neurosci, doi:10.1016/j.tins.2012.08.005
Sudre, Murray, Varsavsky, Graham, Penfold et al., Attributes and predictors of long COVID, Nat. Med, doi:10.1038/s41591-021-01292-y
To, Sridhar, Chiu, Hung, Li et al., Lessons learned 1 year after SARS-CoV-2 emergence leading to COVID-19 pandemic, Emerg. Microbes Infect, doi:10.1080/22221751.2021.1898291
Tyler, Marslen-Wilson, Randall, Wright, Devereux et al., Left inferior frontal cortex and syntax: Function, structure and behaviour in patients with left hemisphere damage, Brain, doi:10.1093/brain/awq369
Tzourio-Mazoyer, Landeau, Papathanassiou, Crivello, Etard et al., Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain, Neuroimage, doi:10.1006/nimg.2001.0978
Vaira, Hopkins, Petrocelli, Lechien, Cutrupi et al., Efficacy of corticosteroid therapy in the treatment of long-lasting olfactory disorders in COVID-19 patients, Rhinology, doi:10.4193/Rhin20.515
Vihta, Pouwels, Peto, Pritchard, House et al., Omicron-associated changes in SARS-CoV-2 symptoms in the United Kingdom, Clin. Infect. Dis
Yildiz, Koca Yildiz, Kuzu, Günebakan, Bucak et al., Comparison of the Healing Effect of Nasal Saline Irrigation with Triamcinolone Acetonide Versus Nasal Saline Irrigation alone in COVID-19 Related Olfactory Dysfunction: A Randomized Controlled Study, Indian J. Otolaryngol. Head Neck Surg, doi:10.1007/s12070-021-02749-9
Yousem, Geckle, Bilker, Mckeown, Doty, Posttraumatic olfactory dysfunction: MR and clinical evaluation, AJNR Am. J. Neuroradiol
Zahn, Moll, Krueger, Huey, Garrido et al., Social concepts are represented in the superior anterior temporal cortex, Proc. Natl. Acad. Sci, doi:10.1073/pnas.0607061104
Zhang, Chu, Han, Shuai, Deng et al., SARS-CoV-2 infects human neural progenitor cells and brain organoids, Cell. Res, doi:10.1038/s41422-020-0390-x
Zhang, Chung, Wong, Hung, Mak et al., Changes in the Intranetwork and Internetwork Connectivity of the Default Mode Network and Olfactory Network in Patients with COVID-19 and Olfactory Dysfunction, Brain Sci, doi:10.3390/brainsci12040511
Zhang, Hao, Manor, Novak, Milberg et al., Intranasal insulin enhanced resting-state functional connectivity of hippocampal regions in type 2 diabetes, Diabetes, doi:10.2337/db14-1000
Zhang, Lee, Chu, Chan, Fan et al., Severe Acute Respiratory Syndrome Coronavirus 2 Infects and Damages the Mature and Immature Olfactory Sensory Neurons of Hamsters, Clin. Infect. Dis, doi:10.1093/cid/ciaa995
Zheng, Wong, Li, Verma, Ortiz et al., COVID-19 treatments and pathogenesis including anosmia in K18-hACE2 mice, Nature
DOI record:
{
"DOI": "10.3390/brainsci13071014",
"ISSN": [
"2076-3425"
],
"URL": "http://dx.doi.org/10.3390/brainsci13071014",
"abstract": "<jats:p>Background: Olfactory dysfunction (OD) is a common neurosensory manifestation in long COVID. An effective and safe treatment against COVID-19-related OD is needed. Methods: This pilot trial recruited long COVID patients with persistent OD. Participants were randomly assigned to receive short-course (14 days) oral vitamin A (VitA; 25,000 IU per day) and aerosolised diffuser olfactory training (OT) thrice daily (combination), OT alone (standard care), or observation (control) for 4 weeks. The primary outcome was differences in olfactory function by butanol threshold tests (BTT) between baseline and end-of-treatment. Secondary outcomes included smell identification tests (SIT), structural MRI brain, and serial seed-based functional connectivity (FC) analyses in the olfactory cortical network by resting-state functional MRI (rs–fMRI). Results: A total of 24 participants were randomly assigned to receive either combination treatment (n = 10), standard care (n = 9), or control (n = 5). Median OD duration was 157 days (IQR 127–175). Mean baseline BTT score was 2.3 (SD 1.1). At end-of-treatment, mean BTT scores were significantly higher for the combination group than control (p < 0.001, MD = 4.4, 95% CI 1.7 to 7.2) and standard care (p = 0.009) groups. Interval SIT scores increased significantly (p = 0.009) in the combination group. rs–fMRI showed significantly higher FC in the combination group when compared to other groups. At end-of-treatment, positive correlations were found in the increased FC at left inferior frontal gyrus and clinically significant improvements in measured BTT (r = 0.858, p < 0.001) and SIT (r = 0.548, p = 0.042) scores for the combination group. Conclusions: Short-course oral VitA and aerosolised diffuser OT was effective as a combination treatment for persistent OD in long COVID.</jats:p>",
"alternative-id": [
"brainsci13071014"
],
"author": [
{
"affiliation": [
{
"name": "Department of Microbiology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China"
}
],
"family": "Chung",
"given": "Tom Wai-Hin",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-8313-0756",
"affiliation": [
{
"name": "Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong, China"
},
{
"name": "Research Institute for Intelligent Wearable Systems, The Hong Kong Polytechnic University, Hong Kong, China"
}
],
"authenticated-orcid": false,
"family": "Zhang",
"given": "Hui",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6620-2479",
"affiliation": [
{
"name": "Department of Ear, Nose and Throat, Pamela Youde Nethersole Eastern Hospital, Hong Kong, China"
}
],
"authenticated-orcid": false,
"family": "Wong",
"given": "Fergus Kai-Chuen",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2022-8307",
"affiliation": [
{
"name": "Department of Microbiology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China"
},
{
"name": "State Key Laboratory of Emerging Infectious Diseases, The University of Hong Kong, Hong Kong, China"
},
{
"name": "Carol Yu Centre for Infection, The University of Hong Kong, Hong Kong, China"
}
],
"authenticated-orcid": false,
"family": "Sridhar",
"given": "Siddharth",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Psychology, The University of Hong Kong, Hong Kong, China"
},
{
"name": "State Key Laboratory of Brain and Cognitive Sciences, The University of Hong Kong, Hong Kong, China"
}
],
"family": "Lee",
"given": "Tatia Mei-Chun",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Surgery, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China"
}
],
"family": "Leung",
"given": "Gilberto Ka-Kit",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China"
}
],
"family": "Chan",
"given": "Koon-Ho",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "State Key Laboratory of Brain and Cognitive Sciences, The University of Hong Kong, Hong Kong, China"
},
{
"name": "Department of Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China"
}
],
"family": "Lau",
"given": "Kui-Kai",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China"
}
],
"family": "Tam",
"given": "Anthony Raymond",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China"
}
],
"family": "Ho",
"given": "Deborah Tip-Yin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1765-7706",
"affiliation": [
{
"name": "Department of Microbiology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China"
}
],
"authenticated-orcid": false,
"family": "Cheng",
"given": "Vincent Chi-Chung",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Microbiology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China"
},
{
"name": "State Key Laboratory of Emerging Infectious Diseases, The University of Hong Kong, Hong Kong, China"
},
{
"name": "Carol Yu Centre for Infection, The University of Hong Kong, Hong Kong, China"
},
{
"name": "The Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, The University of Hong Kong, Hong Kong, China"
}
],
"family": "Yuen",
"given": "Kwok-Yung",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1556-2538",
"affiliation": [
{
"name": "Carol Yu Centre for Infection, The University of Hong Kong, Hong Kong, China"
},
{
"name": "Department of Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China"
},
{
"name": "The Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, The University of Hong Kong, Hong Kong, China"
}
],
"authenticated-orcid": false,
"family": "Hung",
"given": "Ivan Fan-Ngai",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2007-0650",
"affiliation": [
{
"name": "State Key Laboratory of Brain and Cognitive Sciences, The University of Hong Kong, Hong Kong, China"
},
{
"name": "Department of Diagnostic Radiology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China"
},
{
"name": "Alzheimer’s Disease Research Network, The University of Hong Kong, Hong Kong, China"
}
],
"authenticated-orcid": false,
"family": "Mak",
"given": "Henry Ka-Fung",
"sequence": "additional"
}
],
"container-title": "Brain Sciences",
"container-title-short": "Brain Sciences",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
6,
30
]
],
"date-time": "2023-06-30T20:06:37Z",
"timestamp": 1688155597000
},
"deposited": {
"date-parts": [
[
2023,
6,
30
]
],
"date-time": "2023-06-30T22:01:50Z",
"timestamp": 1688162510000
},
"indexed": {
"date-parts": [
[
2024,
2,
7
]
],
"date-time": "2024-02-07T10:21:43Z",
"timestamp": 1707301303859
},
"is-referenced-by-count": 1,
"issue": "7",
"issued": {
"date-parts": [
[
2023,
6,
30
]
]
},
"journal-issue": {
"issue": "7",
"published-online": {
"date-parts": [
[
2023,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
30
]
],
"date-time": "2023-06-30T00:00:00Z",
"timestamp": 1688083200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2076-3425/13/7/1014/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1014",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
6,
30
]
]
},
"published-online": {
"date-parts": [
[
2023,
6,
30
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30154-9",
"article-title": "A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster",
"author": "Chan",
"doi-asserted-by": "crossref",
"first-page": "514",
"journal-title": "Lancet",
"key": "ref_1",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1080/22221751.2021.1898291",
"article-title": "Lessons learned 1 year after SARS-CoV-2 emergence leading to COVID-19 pandemic",
"author": "To",
"doi-asserted-by": "crossref",
"first-page": "507",
"journal-title": "Emerg. Microbes Infect.",
"key": "ref_2",
"volume": "10",
"year": "2021"
},
{
"key": "ref_3",
"unstructured": "National Institute for Health and Care Excellence (2020). COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19, National Institute for Health and Care Excellence. NICE Guideline."
},
{
"DOI": "10.1093/ofid/ofaa199",
"article-title": "Olfactory Dysfunction in Coronavirus Disease 2019 Patients: Observational Cohort Study and Systematic Review",
"author": "Chung",
"doi-asserted-by": "crossref",
"first-page": "ofaa199",
"journal-title": "Open. Forum Infect. Dis.",
"key": "ref_4",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1038/s41591-021-01292-y",
"article-title": "Attributes and predictors of long COVID",
"author": "Sudre",
"doi-asserted-by": "crossref",
"first-page": "626",
"journal-title": "Nat. Med.",
"key": "ref_5",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(20)32656-8",
"article-title": "6-month consequences of COVID-19 in patients discharged from hospital: A cohort study",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "220",
"journal-title": "Lancet",
"key": "ref_6",
"volume": "397",
"year": "2021"
},
{
"DOI": "10.1016/j.eclinm.2021.101019",
"article-title": "Characterizing long COVID in an international cohort: 7 months of symptoms and their impact",
"author": "Davis",
"doi-asserted-by": "crossref",
"first-page": "101019",
"journal-title": "EClinicalMedicine",
"key": "ref_7",
"volume": "38",
"year": "2021"
},
{
"DOI": "10.1007/s10072-021-05611-6",
"article-title": "Qualitative smell/taste disorders as sequelae of acute COVID-19",
"author": "Ercoli",
"doi-asserted-by": "crossref",
"first-page": "4921",
"journal-title": "Neurol. Sci.",
"key": "ref_8",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1016/j.stemcr.2019.02.014",
"article-title": "Activating a Reserve Neural Stem Cell Population In Vitro Enables Engraftment and Multipotency after Transplantation",
"author": "Peterson",
"doi-asserted-by": "crossref",
"first-page": "680",
"journal-title": "Stem Cell. Rep.",
"key": "ref_9",
"volume": "12",
"year": "2019"
},
{
"DOI": "10.1186/1749-8104-8-13",
"article-title": "Retinoic acid regulates olfactory progenitor cell fate and differentiation",
"author": "Paschaki",
"doi-asserted-by": "crossref",
"first-page": "13",
"journal-title": "Neural Dev.",
"key": "ref_10",
"volume": "8",
"year": "2013"
},
{
"DOI": "10.21203/rs.3.rs-304849/v1",
"doi-asserted-by": "crossref",
"key": "ref_11",
"unstructured": "Chung, T.W.-H., Zhang, H., Wong, F.K.-C., Sridhar, S., Chan, K.H., Cheng, V.C.-C., Yuen, K.Y., Hung, I.F.-N., and Mak, H.K.-F. (2021). Neurosensory Rehabilitation and Olfactory Network Recovery in Covid-19-related Olfactory Dysfunction. Brain Sci., 11."
},
{
"DOI": "10.1007/s00405-017-4576-x",
"article-title": "Intranasal vitamin A is beneficial in post-infectious olfactory loss",
"author": "Hummel",
"doi-asserted-by": "crossref",
"first-page": "2819",
"journal-title": "Eur. Arch. Otorhinolaryngol.",
"key": "ref_12",
"volume": "274",
"year": "2017"
},
{
"DOI": "10.1590/abd1806-4841.20175483",
"article-title": "Effects of isotretinoin on the olfactory function in patients with acne",
"author": "Kartal",
"doi-asserted-by": "crossref",
"first-page": "191",
"journal-title": "Bras. Derm.",
"key": "ref_13",
"volume": "92",
"year": "2017"
},
{
"DOI": "10.1002/lary.23405",
"article-title": "Olfactory function in patients with postinfectious and posttraumatic smell disorders before and after treatment with vitamin A: A double-blind, placebo-controlled, randomized clinical trial",
"author": "Reden",
"doi-asserted-by": "crossref",
"first-page": "1906",
"journal-title": "Laryngoscope",
"key": "ref_14",
"volume": "122",
"year": "2012"
},
{
"DOI": "10.1001/archotol.1962.00740040122008",
"article-title": "Treatment of Uncomplicated Anosmia by Vitamin A",
"author": "Duncan",
"doi-asserted-by": "crossref",
"first-page": "116",
"journal-title": "Arch. Otolaryngol.",
"key": "ref_15",
"volume": "75",
"year": "1962"
},
{
"DOI": "10.1111/coa.13636",
"article-title": "Management of new onset loss of sense of smell during the COVID-19 pandemic—BRS Consensus Guidelines",
"author": "Hopkins",
"doi-asserted-by": "crossref",
"first-page": "16",
"journal-title": "Clin. Otolaryngol.",
"key": "ref_16",
"volume": "46",
"year": "2021"
},
{
"DOI": "10.1016/j.jaci.2020.12.641",
"article-title": "Clinical Olfactory Working Group consensus statement on the treatment of postinfectious olfactory dysfunction",
"author": "Addison",
"doi-asserted-by": "crossref",
"first-page": "1704",
"journal-title": "J. Allergy Clin. Immunol.",
"key": "ref_17",
"volume": "147",
"year": "2021"
},
{
"article-title": "Efficacy of corticosteroid therapy in the treatment of long- lasting olfactory disorders in COVID-19 patients",
"author": "Vaira",
"first-page": "21",
"journal-title": "Rhinology",
"key": "ref_18",
"volume": "59",
"year": "2021"
},
{
"DOI": "10.1016/j.amjoto.2020.102884",
"article-title": "Corticosteroid nasal spray for recovery of smell sensation in COVID-19 patients: A randomized controlled trial",
"author": "Abdelalim",
"doi-asserted-by": "crossref",
"first-page": "102884",
"journal-title": "Am. J. Otolaryngol.",
"key": "ref_19",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1016/j.intimp.2021.107871",
"article-title": "Mometasone furoate nasal spray in the treatment of patients with COVID-19 olfactory dysfunction: A randomized, double blind clinical trial",
"author": "Kasiri",
"doi-asserted-by": "crossref",
"first-page": "107871",
"journal-title": "Int. Immunopharmacol.",
"key": "ref_20",
"volume": "98",
"year": "2021"
},
{
"DOI": "10.1016/j.amjoto.2021.103033",
"article-title": "Effect of nasal corticosteroid in the treatment of anosmia due to COVID-19: A randomised double-blind placebo-controlled study",
"author": "Rashid",
"doi-asserted-by": "crossref",
"first-page": "103033",
"journal-title": "Am. J. Otolaryngol.",
"key": "ref_21",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1007/s12070-021-02749-9",
"article-title": "Comparison of the Healing Effect of Nasal Saline Irrigation with Triamcinolone Acetonide Versus Nasal Saline Irrigation alone in COVID-19 Related Olfactory Dysfunction: A Randomized Controlled Study",
"author": "Yildiz",
"doi-asserted-by": "crossref",
"first-page": "3022",
"journal-title": "Indian J. Otolaryngol. Head Neck Surg.",
"key": "ref_22",
"volume": "74",
"year": "2021"
},
{
"DOI": "10.1288/00005537-198801000-00017",
"article-title": "Evaluation of olfactory dysfunction in the Connecticut Chemosensory Clinical Research Center",
"author": "Cain",
"doi-asserted-by": "crossref",
"first-page": "83",
"journal-title": "Laryngoscope",
"key": "ref_23",
"volume": "98",
"year": "1988"
},
{
"DOI": "10.1016/0031-9384(84)90269-5",
"article-title": "Development of the University of Pennsylvania Smell Identification Test: A standardized microencapsulated test of olfactory function",
"author": "Doty",
"doi-asserted-by": "crossref",
"first-page": "489",
"journal-title": "Physiol. Behav.",
"key": "ref_24",
"volume": "32",
"year": "1984"
},
{
"article-title": "Posttraumatic olfactory dysfunction: MR and clinical evaluation",
"author": "Yousem",
"first-page": "1171",
"journal-title": "AJNR Am. J. Neuroradiol.",
"key": "ref_25",
"volume": "17",
"year": "1996"
},
{
"DOI": "10.1148/radiol.13130531",
"article-title": "Clinical proton MR spectroscopy in central nervous system disorders",
"author": "Oz",
"doi-asserted-by": "crossref",
"first-page": "658",
"journal-title": "Radiology",
"key": "ref_26",
"volume": "270",
"year": "2014"
},
{
"DOI": "10.1016/j.pneurobio.2006.12.003",
"article-title": "N-Acetylaspartate in the CNS: From neurodiagnostics to neurobiology",
"author": "Moffett",
"doi-asserted-by": "crossref",
"first-page": "89",
"journal-title": "Prog. Neurobiol.",
"key": "ref_27",
"volume": "81",
"year": "2007"
},
{
"DOI": "10.1016/j.neuroimage.2007.07.007",
"article-title": "A fast diffeomorphic image registration algorithm",
"author": "Ashburner",
"doi-asserted-by": "crossref",
"first-page": "95",
"journal-title": "Neuroimage",
"key": "ref_28",
"volume": "38",
"year": "2007"
},
{
"DOI": "10.1006/nimg.2001.0978",
"article-title": "Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain",
"author": "Landeau",
"doi-asserted-by": "crossref",
"first-page": "273",
"journal-title": "Neuroimage",
"key": "ref_29",
"volume": "15",
"year": "2002"
},
{
"DOI": "10.1038/srep42534",
"article-title": "Brain fingerprints of olfaction: A novel structural method for assessing olfactory cortical networks in health and disease",
"author": "Fjaeldstad",
"doi-asserted-by": "crossref",
"first-page": "42534",
"journal-title": "Sci. Rep.",
"key": "ref_30",
"volume": "7",
"year": "2017"
},
{
"DOI": "10.1016/S2666-5247(20)30004-5",
"article-title": "Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: An observational study",
"author": "Chu",
"doi-asserted-by": "crossref",
"first-page": "e14",
"journal-title": "Lancet Microbe",
"key": "ref_31",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1038/s41422-020-0390-x",
"article-title": "SARS-CoV-2 infects human neural progenitor cells and brain organoids",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "928",
"journal-title": "Cell. Res.",
"key": "ref_32",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa995",
"article-title": "Severe Acute Respiratory Syndrome Coronavirus 2 Infects and Damages the Mature and Immature Olfactory Sensory Neurons of Hamsters",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "e503",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_33",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(20)31525-7",
"article-title": "Inflammatory olfactory neuropathy in two patients with COVID-19",
"author": "Kirschenbaum",
"doi-asserted-by": "crossref",
"first-page": "166",
"journal-title": "Lancet",
"key": "ref_34",
"volume": "396",
"year": "2020"
},
{
"DOI": "10.1016/S1474-4422(20)30308-2",
"article-title": "Neuropathology of patients with COVID-19 in Germany: A post-mortem case series",
"author": "Matschke",
"doi-asserted-by": "crossref",
"first-page": "919",
"journal-title": "Lancet Neurol.",
"key": "ref_35",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1038/s41593-020-00758-5",
"article-title": "Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19",
"author": "Meinhardt",
"doi-asserted-by": "crossref",
"first-page": "168",
"journal-title": "Nat. Neurosci.",
"key": "ref_36",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1016/S2666-5247(20)30144-0",
"article-title": "Viral presence and immunopathology in patients with lethal COVID-19: A prospective autopsy cohort study",
"author": "Schurink",
"doi-asserted-by": "crossref",
"first-page": "e290",
"journal-title": "Lancet Microbe",
"key": "ref_37",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2020.06.032",
"article-title": "Massive transient damage of the olfactory epithelium associated with infection of sustentacular cells by SARS-CoV-2 in golden Syrian hamsters",
"author": "Bryche",
"doi-asserted-by": "crossref",
"first-page": "579",
"journal-title": "Brain Behav. Immun.",
"key": "ref_38",
"volume": "89",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2943-z",
"article-title": "COVID-19 treatments and pathogenesis including anosmia in K18-hACE2 mice",
"author": "Zheng",
"doi-asserted-by": "crossref",
"first-page": "603",
"journal-title": "Nature",
"key": "ref_39",
"volume": "589",
"year": "2021"
},
{
"DOI": "10.3390/v13010113",
"doi-asserted-by": "crossref",
"key": "ref_40",
"unstructured": "Everett, H.E., Lean, F.Z.X., Byrne, A.M.P., van Diemen, P.M., Rhodes, S., James, J., Mollett, B., Coward, V.J., Skinner, P., and Warren, C.J. (2021). Intranasal Infection of Ferrets with SARS-CoV-2 as a Model for Asymptomatic Human Infection. Viruses, 13."
},
{
"DOI": "10.1038/s41392-021-00591-7",
"article-title": "The olfactory route is a potential way for SARS-CoV-2 to invade the central nervous system of rhesus monkeys",
"author": "Jiao",
"doi-asserted-by": "crossref",
"first-page": "169",
"journal-title": "Signal. Transduct. Target. Ther.",
"key": "ref_41",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1126/sciadv.abc5801",
"article-title": "Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia",
"author": "Brann",
"doi-asserted-by": "crossref",
"first-page": "eabc5801",
"journal-title": "Sci. Adv.",
"key": "ref_42",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1038/nn1882",
"article-title": "Contribution of olfactory neural stem cells to tissue maintenance and regeneration",
"author": "Leung",
"doi-asserted-by": "crossref",
"first-page": "720",
"journal-title": "Nat. Neurosci.",
"key": "ref_43",
"volume": "10",
"year": "2007"
},
{
"DOI": "10.1073/pnas.1701333114",
"article-title": "Notch1 maintains dormancy of olfactory horizontal basal cells, a reserve neural stem cell",
"author": "Herrick",
"doi-asserted-by": "crossref",
"first-page": "E5589",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_44",
"volume": "114",
"year": "2017"
},
{
"DOI": "10.1016/j.neuroimage.2007.05.019",
"article-title": "Mapping the functional connectivity of anterior cingulate cortex",
"author": "Margulies",
"doi-asserted-by": "crossref",
"first-page": "579",
"journal-title": "Neuroimage",
"key": "ref_45",
"volume": "37",
"year": "2007"
},
{
"DOI": "10.1073/pnas.0607061104",
"article-title": "Social concepts are represented in the superior anterior temporal cortex",
"author": "Zahn",
"doi-asserted-by": "crossref",
"first-page": "6430",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_46",
"volume": "104",
"year": "2007"
},
{
"DOI": "10.1038/35086057",
"article-title": "New insights into the functions of the superior temporal cortex",
"author": "Karnath",
"doi-asserted-by": "crossref",
"first-page": "568",
"journal-title": "Nat. Rev. Neurosci.",
"key": "ref_47",
"volume": "2",
"year": "2001"
},
{
"DOI": "10.1093/brain/awq369",
"article-title": "Left inferior frontal cortex and syntax: Function, structure and behaviour in patients with left hemisphere damage",
"author": "Tyler",
"doi-asserted-by": "crossref",
"first-page": "415",
"journal-title": "Brain",
"key": "ref_48",
"volume": "134",
"year": "2011"
},
{
"DOI": "10.1162/089892999563166",
"article-title": "Functional anatomy of perceptual and semantic processing for odors",
"author": "Royet",
"doi-asserted-by": "crossref",
"first-page": "94",
"journal-title": "J. Cogn. Neurosci.",
"key": "ref_49",
"volume": "11",
"year": "1999"
},
{
"DOI": "10.1002/hbm.20009",
"article-title": "Passive perception of odors and semantic circuits",
"author": "Savic",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Hum. Brain Mapp.",
"key": "ref_50",
"volume": "21",
"year": "2004"
},
{
"DOI": "10.3390/brainsci12040511",
"doi-asserted-by": "crossref",
"key": "ref_51",
"unstructured": "Zhang, H., Chung, T.W.-H., Wong, F.K.-C., Hung, I.F.-N., and Mak, H.K.-F. (2022). Changes in the Intranetwork and Internetwork Connectivity of the Default Mode Network and Olfactory Network in Patients with COVID-19 and Olfactory Dysfunction. Brain Sci., 12."
},
{
"DOI": "10.1016/S0140-6736(22)00327-0",
"article-title": "Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: A prospective observational study from the ZOE COVID Study",
"author": "Menni",
"doi-asserted-by": "crossref",
"first-page": "1618",
"journal-title": "Lancet",
"key": "ref_52",
"volume": "399",
"year": "2022"
},
{
"article-title": "Omicron-associated changes in SARS-CoV-2 symptoms in the United Kingdom",
"author": "Vihta",
"first-page": "e133",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_53",
"volume": "76",
"year": "2022"
},
{
"key": "ref_54",
"unstructured": "World Health Organization (2020, September 14). Coronavirus Disease 2019 (COVID-19) Weekly Operational Update on COVID-19 9 September 2020, Available online: https://www.who.int/docs/default-source/coronaviruse/weekly-updates/wou-9-september-2020-cleared.pdf?sfvrsn=d39784f7_2."
},
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical Characteristics of coronavirus disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "1708",
"journal-title": "N. Engl. J. Med.",
"key": "ref_55",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1002/lary.24340",
"article-title": "Olfactory training is helpful in postinfectious olfactory loss: A randomized, controlled, multicenter study",
"author": "Damm",
"doi-asserted-by": "crossref",
"first-page": "826",
"journal-title": "Laryngoscope",
"key": "ref_56",
"volume": "124",
"year": "2013"
},
{
"DOI": "10.1089/neu.2017.5230",
"article-title": "Olfactory Training in Post-Traumatic Smell Impairment: Mild Improvement in Threshold Performances: Results from a Randomized Controlled Trial",
"author": "Langdon",
"doi-asserted-by": "crossref",
"first-page": "2641",
"journal-title": "J. Neurotrauma",
"key": "ref_57",
"volume": "35",
"year": "2018"
},
{
"DOI": "10.1016/j.nicl.2015.09.004",
"article-title": "Olfactory training induces changes in regional functional connectivity in patients with long-term smell loss",
"author": "Kollndorfer",
"doi-asserted-by": "crossref",
"first-page": "401",
"journal-title": "NeuroImage Clin.",
"key": "ref_58",
"volume": "9",
"year": "2015"
},
{
"DOI": "10.1016/j.neuroimage.2019.01.008",
"article-title": "Smell training improves olfactory function and alters brain structure",
"author": "Poupon",
"doi-asserted-by": "crossref",
"first-page": "45",
"journal-title": "Neuroimage",
"key": "ref_59",
"volume": "189",
"year": "2019"
},
{
"DOI": "10.1016/j.tins.2012.08.005",
"article-title": "A vitamin for the brain",
"author": "Shearer",
"doi-asserted-by": "crossref",
"first-page": "733",
"journal-title": "Trends Neurosci.",
"key": "ref_60",
"volume": "35",
"year": "2012"
},
{
"key": "ref_61",
"unstructured": "World Health Organization (2020, July 22). Measles, Available online: https://www.who.int/news-room/fact-sheets/detail/measles."
},
{
"article-title": "Vitamin A for treating measles in children",
"author": "Huiming",
"first-page": "CD001479",
"journal-title": "Cochrane Database Syst Rev.",
"key": "ref_62",
"volume": "2005",
"year": "2005"
},
{
"DOI": "10.1056/NEJM199007193230304",
"article-title": "A Randomized, Controlled Trial of Vitamin A in Children with Severe Measles",
"author": "Hussey",
"doi-asserted-by": "crossref",
"first-page": "160",
"journal-title": "N. Engl. J. Med.",
"key": "ref_63",
"volume": "323",
"year": "1990"
},
{
"DOI": "10.1002/lary.24654",
"article-title": "Modification of the lund-kennedy endoscopic scoring system improves its reliability and correlation with patient-reported outcome measures",
"author": "Psaltis",
"doi-asserted-by": "crossref",
"first-page": "2216",
"journal-title": "Laryngoscope",
"key": "ref_64",
"volume": "124",
"year": "2014"
},
{
"key": "ref_65",
"unstructured": "(2020, July 22). Guidance for Industry: Converting Units of Measure for Folate, Niacin, and Vitamins A, D, and E on the Nutrition and Supplement Facts Labels. Docket Number: FDA-2016-D-4484. Center for Food Safety and Applied Nutrition, Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-converting-units-measure-folate-niacin-and-vitamins-d-and-e-nutrition-and."
},
{
"key": "ref_66",
"unstructured": "(2020, June 15). Vitamin A Fact Sheet for Health Professionals, Available online: https://ods.od.nih.gov/factsheets/Vitamin%20A-HealthProfessional/#en5."
},
{
"article-title": "Olfactory Loss and Regain: Lessons for Neuroplasticity",
"author": "Reichert",
"first-page": "22",
"journal-title": "Neurosci.",
"key": "ref_67",
"volume": "24",
"year": "2017"
},
{
"DOI": "10.1155/2014/140419",
"article-title": "Recovery of Olfactory Function Induces Neuroplasticity Effects in Patients with Smell Loss",
"author": "Kollndorfer",
"doi-asserted-by": "crossref",
"first-page": "140419",
"journal-title": "Neural Plast.",
"key": "ref_68",
"volume": "2014",
"year": "2014"
},
{
"DOI": "10.1002/hbm.23440",
"article-title": "Default mode network deactivation during odor-visual association",
"author": "Karunanayaka",
"doi-asserted-by": "crossref",
"first-page": "1125",
"journal-title": "Hum. Brain Mapp.",
"key": "ref_69",
"volume": "38",
"year": "2016"
},
{
"DOI": "10.1002/brb3.1296",
"article-title": "Karunanayaka. Disruptions of the olfactory and default mode networks in Alzheimer’s disease",
"author": "Lu",
"doi-asserted-by": "crossref",
"first-page": "e01296",
"journal-title": "Brain Behav.",
"key": "ref_70",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.2337/db14-1000",
"article-title": "Intranasal insulin enhanced resting-state functional connectivity of hippocampal regions in type 2 diabetes",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "1025",
"journal-title": "Diabetes",
"key": "ref_71",
"volume": "64",
"year": "2015"
}
],
"reference-count": 71,
"references-count": 71,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2076-3425/13/7/1014"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Neuroscience"
],
"subtitle": [],
"title": "A Pilot Study of Short-Course Oral Vitamin A and Aerosolised Diffuser Olfactory Training for the Treatment of Smell Loss in Long COVID",
"type": "journal-article",
"volume": "13"
}