Risk factors for Coronavirus disease-associated mucormycosis
et al., Journal of Infection, doi:10.1016/j.jinf.2021.12.039, Mar 2022
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
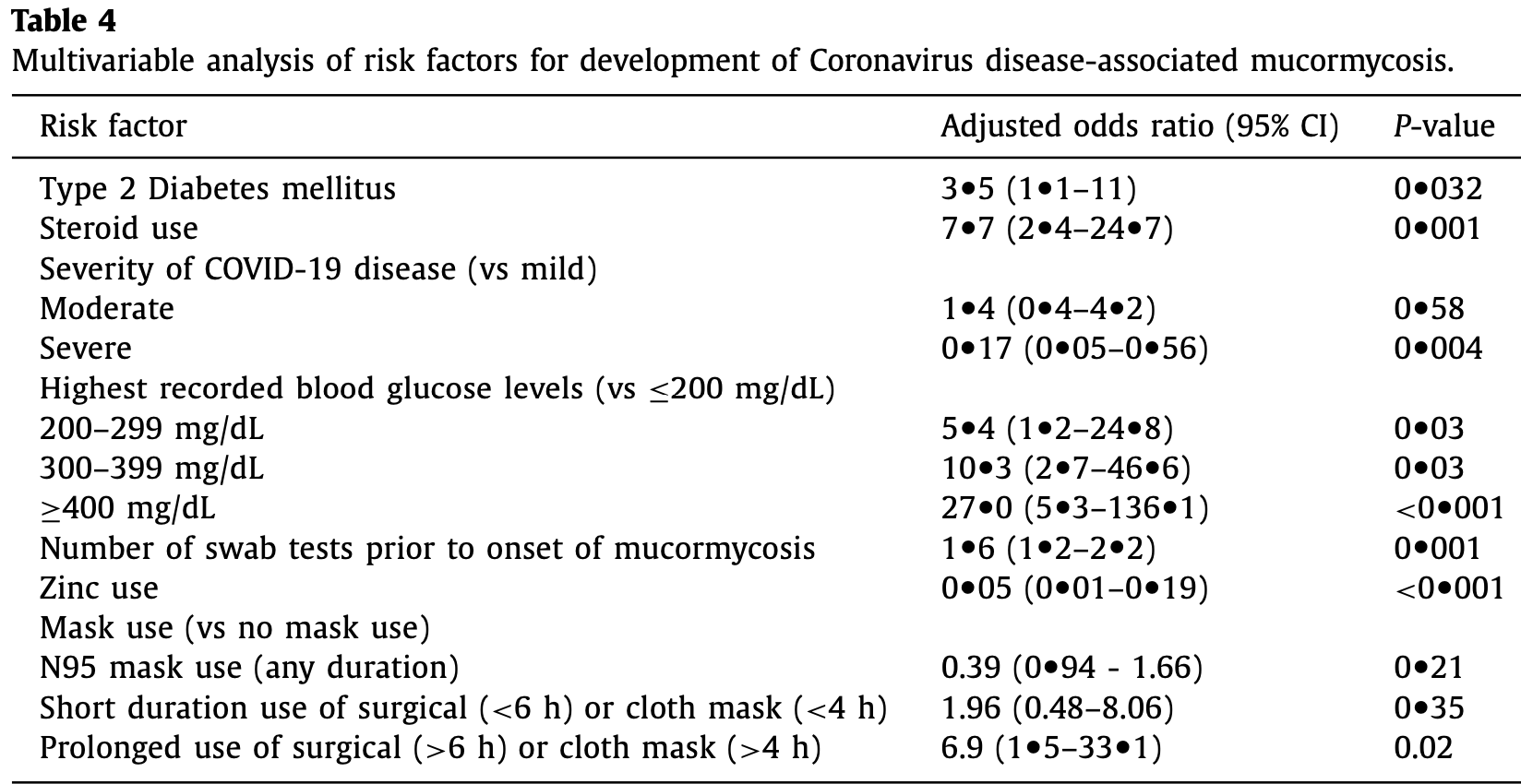
Retrospective 152 COVID-associated mucormycosis cases and 200 controls, showing lower risk of COVID-associated mucormycosis with zinc treatment.
|
risk of progression, 95.0% lower, OR 0.05, p < 0.001, case control OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Arora et al., 31 Mar 2022, retrospective, India, peer-reviewed, 34 authors.
Risk factors for Coronavirus disease-associated mucormycosis
Journal of Infection, doi:10.1016/j.jinf.2021.12.039
Background: The epidemiology of the Coronavirus-disease associated mucormycosis (CAM) syndemic is poorly elucidated. We aimed to identify risk factors that may explain the burden of cases and help develop preventive strategies. Methods: We performed a case-control study comparing cases diagnosed with CAM and taking controls as recovered COVID 19 patients who did not develop mucormycosis. Information on comorbidities, glycemic control, and practices related to COVID-19 prevention and treatment was recorded. Multivariate regression analysis was used to identify independent predictors. Results: A total of 352 patients (152 cases and 200 controls) diagnosed with COVID-19 during April-May 2021 were included. In the CAM group, symptoms of mucormycosis began a mean of 18.9 (SD 9.1) days after onset of COVID-19, and predominantly rhino-sinus and orbital involvement was present. All, but one, CAM cases had conventional risk factors of diabetes and steroid use. On multivariable regression, increased odds of CAM were associated with the presence of diabetes (adjusted OR 3.5, 95% CI 1.1-11), use of systemic steroids (aOR 7.7, 95% CI 2.4-24.7), prolonged use of cloth and surgical masks (vs. no mask, aOR 6.9, 95%CI 1.5-33.1), and repeated nasopharyngeal swab testing during the COVID-19 illness (aOR 1.6, 95% CI 1.2-2.2). Zinc therapy was found to be protective (aOR 0.05, 95%CI 0.01-0.19). Notably, the requirement of oxygen supplementation or hospitalization did not affect the risk of CAM. Conclusion: Judicious use of steroids and stringent glycemic control are vital to preventing mucormycosis. Use of clean masks, preference for N95 masks if available, and minimizing swab testing after the diagnosis of COVID-19 may further reduce the incidence of CAM.
IRB approval The study was approved by the Institute Ethics Committee, AI-IMS, Delhi, India. [IECPG-353/28.05.21]
Authors' contributions All listed authors meet the ICMJE criteria. We attest that all authors contributed significantly to the creation of this manuscript, each having fulfilled the criteria as established by the ICMJE.
Declaration of Competing Interest The authors declare that they have no competing interests.
References
Afiat, Nofri, Adi, Rovina, Type 2 diabetes and its impact on the immune system, Curr Diabetes Rev
Banerjee, Pal, Bhadada, Intercepting the deadly trinity of mucormycosis, diabetes and COVID-19 in India, Postgrad Med J
Bhattacharjee, Bahl, Chughtai, Macintyre, Last-resort strategies during mask shortages: optimal design features of cloth masks and decontamination of disposable masks during the COVID-19 pandemic, BMJ Open Respir Res
Binder, Maurer, Lass-Flörl, Mucormycosis-from the pathogens to the disease, Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis
Boelaert, De Locht, Van Cutsem, Kerrels, Cantinieaux et al., Mucormycosis during deferoxamine therapy is a siderophore-mediated infection. In vitro and in vivo animal studies, J Clin Invest
Chakrabarti, Dhaliwal, Epidemiology of mucormycosis in India, Curr Fungal Infect Rep
Chakrabarti, Singh, Mucormycosis in India: unique features, Mycoses
Cornely, Alastruey-Izquierdo, Arenz, Chen, Dannaoui et al., Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium, Lancet Infect Dis
Corrao, Bocchio, Monaco, Natoli, Cavezzi et al., Does evidence exist to blunt inflammatory response by nutraceutical supplementation during COVID-19 pandemic? An overview of systematic reviews of vitamin D, vitamin C, Melatonin, and Zinc, Nutrients
Dadwal, Tegtmeier, Liu, Frankel, Ito et al., Impact of pretransplant serum ferritin level on risk of invasive mold infection after allogeneic hematopoietic stem cell transplantation, Eur J Haematol
Dhatariya, Glaser, Codner, Umpierrez, Diabetic ketoacidosis, Nat Rev Dis Primer
Ghuman, Voelz, Innate and adaptive immunity to mucorales, J Fungi Basel Switz
Ibrahim, Spellberg, Walsh, Kontoyiannis, Pathogenesis of mucormycosis, Clin Infect Dis
Jayawardena, Sooriyaarachchi, Chourdakis, Jeewandara, Ranasinghe, Enhancing immunity in viral infections, with special emphasis on COVID-19: a review, Diabetes Metab Syndr Clin Res Rev
Jeong, Keighley, Wolfe, Lee, Slavin et al., The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports, Clin Microbiol Infect
Jin, Yang, Chen, Zhang, Duan, Endothelial activation and dysfunction in COVID-19: from basic mechanisms to potential therapeutic approaches, Signal Transduct Target Ther
Liu, Ward, Krishnamoorthy, Mandelcorn, Leigh, A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy, Allergy Asthma Clin Immunol
Lucas, Wong, Klein, Castro, Silva et al., Longitudinal analyses reveal immunological misfiring in severe COVID-19, Nature
Macintyre, Seale, Dung, Hien, Nga et al., A cluster randomised trial of cloth masks compared with medical masks in healthcare workers, BMJ Open
Patel, Agarwal, Rudramurthy, Shevkani, Xess et al., Multicenter epidemiologic study of coronavirus disease-associated mucormycosis, India, Emerg Infect Dis
Patel, Kaur, Xess, Michael, Savio et al., A multicentre observational study on the epidemiology, risk factors, management and outcomes of mucormycosis in India, Clin Microbiol Infect
Reusch, Domenico, Bonaguro, Schulte-Schrepping, Baßler et al., Neutrophils in COVID-19, Front Immunol
Ribes, Vanover-Sams, Baker, Zygomycetes in human disease, Clin Microbiol Rev
Scarano, Inchingolo, Lorusso, Facial skin temperature and discomfort when wearing protective face masks: thermal infrared imaging evaluation and hands moving the mask, Int J Environ Res Public Health
Sen, Honavar, Bansal, Sengupta, Rao et al., Epidemiology, clinical profile, management, and outcome of COVID-19-associated rhino-orbital-cerebral mucormycosis in 2826 patients in India -Collaborative OPAI-IJO Study on Mucormycosis in COVID-19 (COSMIC), Report 1, Indian J Ophthalmol
Thomas, Patel, Bittel, Wolski, Wang et al., Effect of high-dose zinc and ascorbic acid supplementation vs usual care on symptom length and reduction among ambulatory patients with SARS-CoV-2 infection: the COVID A to Z randomized clinical trial, JAMA Netw Open
Times, Black fungus: here is a list of states with highest number of mucormycosis cases
Unsworth, Wallace, Oliver, Yeung, Kshirsagar et al., New-onset type 1 diabetes in children during COVID-19: multicenter regional findings in the U, K. Diabetes Care
Vidler, Rogers, Yallop, Devereux, Wellving et al., Outpatient management of steroid-induced hyperglycaemia and steroid-induced diabetes in people with lymphoproliferative disorders treated with intermittent high dose steroids, J Clin Transl Endocrinol
DOI record:
{
"DOI": "10.1016/j.jinf.2021.12.039",
"ISSN": [
"0163-4453"
],
"URL": "http://dx.doi.org/10.1016/j.jinf.2021.12.039",
"alternative-id": [
"S016344532100654X"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Risk factors for Coronavirus disease-associated mucormycosis"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Journal of Infection"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jinf.2021.12.039"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 The British Infection Association. Published by Elsevier Ltd. All rights reserved."
}
],
"author": [
{
"affiliation": [],
"family": "Arora",
"given": "Umang",
"sequence": "first"
},
{
"affiliation": [],
"family": "Priyadarshi",
"given": "Megha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Katiyar",
"given": "Varidh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Soneja",
"given": "Manish",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garg",
"given": "Prerna",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1107-9378",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gupta",
"given": "Ishan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bharadiya",
"given": "Vishwesh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Berry",
"given": "Parul",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6310-1111",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ghosh",
"given": "Tamoghna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Patel",
"given": "Lajjaben",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sarda",
"given": "Radhika",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garg",
"given": "Shreya",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Agarwal",
"given": "Shubham",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Arora",
"given": "Veronica",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ramprasad",
"given": "Aishwarya",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kumar",
"given": "Amit",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garg",
"given": "Rohit Kumar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kodan",
"given": "Parul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nischal",
"given": "Neeraj",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3169-8419",
"affiliation": [],
"authenticated-orcid": false,
"family": "Singh",
"given": "Gagandeep",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3722-4310",
"affiliation": [],
"authenticated-orcid": false,
"family": "Jorwal",
"given": "Pankaj",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kumar",
"given": "Arvind",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Baitha",
"given": "Upendra",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Meena",
"given": "Ved Prakash",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ray",
"given": "Animesh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sethi",
"given": "Prayas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xess",
"given": "Immaculata",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6202-576X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Vikram",
"given": "Naval",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sinha",
"given": "Sanjeev",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Biswas",
"given": "Ashutosh",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5691-8932",
"affiliation": [],
"authenticated-orcid": false,
"family": "Thakar",
"given": "Alok",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bhatnagar",
"given": "Sushma",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Trikha",
"given": "Anjan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wig",
"given": "Naveet",
"sequence": "additional"
}
],
"container-title": [
"Journal of Infection"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"journalofinfection.com",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.fr",
"clinicalkey.com.au",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
12,
30
]
],
"date-time": "2021-12-30T16:31:31Z",
"timestamp": 1640881891000
},
"deposited": {
"date-parts": [
[
2022,
3,
18
]
],
"date-time": "2022-03-18T07:05:42Z",
"timestamp": 1647587142000
},
"indexed": {
"date-parts": [
[
2022,
4,
5
]
],
"date-time": "2022-04-05T22:23:28Z",
"timestamp": 1649197408834
},
"is-referenced-by-count": 3,
"issn-type": [
{
"type": "print",
"value": "0163-4453"
}
],
"issue": "3",
"issued": {
"date-parts": [
[
2022,
3
]
]
},
"journal-issue": {
"issue": "3",
"published-print": {
"date-parts": [
[
2022,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
3,
1
]
],
"date-time": "2022-03-01T00:00:00Z",
"timestamp": 1646092800000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S016344532100654X?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S016344532100654X?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "383-390",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
3
]
]
},
"published-print": {
"date-parts": [
[
2022,
3
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.3201/eid2709.210934",
"article-title": "Multicenter epidemiologic study of coronavirus disease–associated mucormycosis, India",
"author": "Patel",
"doi-asserted-by": "crossref",
"journal-title": "Emerg Infect Dis",
"key": "10.1016/j.jinf.2021.12.039_bib0001",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1007/s12281-013-0152-z",
"article-title": "Epidemiology of mucormycosis in India",
"author": "Chakrabarti",
"doi-asserted-by": "crossref",
"first-page": "287",
"issue": "4",
"journal-title": "Curr Fungal Infect Rep",
"key": "10.1016/j.jinf.2021.12.039_bib0002",
"volume": "7",
"year": "2013"
},
{
"key": "10.1016/j.jinf.2021.12.039_bib0003",
"series-title": "Black fungus: here is a list of states with highest number of mucormycosis cases [Internet]",
"year": "2021"
},
{
"DOI": "10.1016/S1473-3099(19)30312-3",
"article-title": "Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium",
"author": "Cornely",
"doi-asserted-by": "crossref",
"first-page": "e405",
"issue": "12",
"journal-title": "Lancet Infect Dis",
"key": "10.1016/j.jinf.2021.12.039_bib0004",
"volume": "19",
"year": "2019"
},
{
"key": "10.1016/j.jinf.2021.12.039_bib0005",
"unstructured": "WHO COVID-19 Case definition [Internet]. [cited 2021 Jun 21]. Available from: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-Surveillance_Case_Definition-2020.2"
},
{
"article-title": "Diagnosis and classification of diabetes mellitus",
"first-page": "S62",
"issue": "1",
"journal-title": "Diabetes Care",
"key": "10.1016/j.jinf.2021.12.039_bib0006",
"volume": "33",
"year": "2010"
},
{
"DOI": "10.1186/1710-1492-9-30",
"article-title": "A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "1",
"journal-title": "Allergy Asthma Clin Immunol",
"key": "10.1016/j.jinf.2021.12.039_bib0007",
"volume": "9",
"year": "2013"
},
{
"DOI": "10.1016/j.cmi.2019.11.021",
"article-title": "A multicentre observational study on the epidemiology, risk factors, management and outcomes of mucormycosis in India",
"author": "Patel",
"doi-asserted-by": "crossref",
"first-page": "944",
"issue": "7",
"journal-title": "Clin Microbiol Infect",
"key": "10.1016/j.jinf.2021.12.039_bib0008",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1111/myc.12243",
"article-title": "Mucormycosis in India: unique features",
"author": "Chakrabarti",
"doi-asserted-by": "crossref",
"first-page": "85",
"journal-title": "Mycoses",
"key": "10.1016/j.jinf.2021.12.039_bib0009",
"volume": "57",
"year": "2014"
},
{
"DOI": "10.4103/ijo.IJO_1565_21",
"article-title": "Epidemiology, clinical profile, management, and outcome of COVID-19-associated rhino-orbital-cerebral mucormycosis in 2826 patients in India – Collaborative OPAI-IJO Study on Mucormycosis in COVID-19 (COSMIC), Report 1",
"author": "Sen",
"doi-asserted-by": "crossref",
"first-page": "1670",
"issue": "7",
"journal-title": "Indian J Ophthalmol",
"key": "10.1016/j.jinf.2021.12.039_bib0010",
"volume": "69",
"year": "2021"
},
{
"DOI": "10.3390/jof3030048",
"article-title": "Innate and adaptive immunity to mucorales",
"author": "Ghuman",
"doi-asserted-by": "crossref",
"first-page": "E48",
"issue": "3",
"journal-title": "J Fungi Basel Switz",
"key": "10.1016/j.jinf.2021.12.039_bib0011",
"volume": "3",
"year": "2017"
},
{
"DOI": "10.3389/fimmu.2021.652470",
"article-title": "Neutrophils in COVID-19",
"author": "Reusch",
"doi-asserted-by": "crossref",
"journal-title": "Front Immunol",
"key": "10.1016/j.jinf.2021.12.039_bib0012",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2588-y",
"article-title": "Longitudinal analyses reveal immunological misfiring in severe COVID-19",
"author": "Lucas",
"doi-asserted-by": "crossref",
"first-page": "463",
"issue": "7821",
"journal-title": "Nature",
"key": "10.1016/j.jinf.2021.12.039_bib0013",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1038/s41392-020-00454-7",
"article-title": "Endothelial activation and dysfunction in COVID-19: from basic mechanisms to potential therapeutic approaches",
"author": "Jin",
"doi-asserted-by": "crossref",
"first-page": "293",
"issue": "1",
"journal-title": "Signal Transduct Target Ther",
"key": "10.1016/j.jinf.2021.12.039_bib0014",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.2174/1573399815666191024085838",
"article-title": "Type 2 diabetes and its impact on the immune system",
"author": "Afiat",
"doi-asserted-by": "crossref",
"first-page": "442",
"issue": "5",
"journal-title": "Curr Diabetes Rev",
"key": "10.1016/j.jinf.2021.12.039_bib0015",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1093/cid/cir865",
"article-title": "Pathogenesis of mucormycosis",
"author": "Ibrahim",
"doi-asserted-by": "crossref",
"first-page": "S16",
"issue": "suppl_1",
"journal-title": "Clin Infect Dis",
"key": "10.1016/j.jinf.2021.12.039_bib0016",
"volume": "54",
"year": "2012"
},
{
"article-title": "Mucormycosis–from the pathogens to the disease",
"author": "Binder",
"first-page": "60",
"issue": "6",
"journal-title": "Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis",
"key": "10.1016/j.jinf.2021.12.039_bib0017",
"year": "2014"
},
{
"DOI": "10.2337/dc20-1551",
"article-title": "New-onset type 1 diabetes in children during COVID-19: multicenter regional findings in the U.K",
"author": "Unsworth",
"doi-asserted-by": "crossref",
"first-page": "e170",
"issue": "11",
"journal-title": "Diabetes Care",
"key": "10.1016/j.jinf.2021.12.039_bib0018",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1038/s41572-020-0165-1",
"article-title": "Diabetic ketoacidosis",
"author": "Dhatariya",
"doi-asserted-by": "crossref",
"first-page": "40",
"issue": "1",
"journal-title": "Nat Rev Dis Primer",
"key": "10.1016/j.jinf.2021.12.039_bib0019",
"volume": "6",
"year": "2020"
},
{
"article-title": "Outpatient management of steroid-induced hyperglycaemia and steroid-induced diabetes in people with lymphoproliferative disorders treated with intermittent high dose steroids",
"author": "Vidler",
"first-page": "18",
"journal-title": "J Clin Transl Endocrinol",
"key": "10.1016/j.jinf.2021.12.039_bib0020",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.1056/NEJMoa2021436",
"article-title": "Dexamethasone in hospitalized patients with Covid-19",
"doi-asserted-by": "crossref",
"first-page": "693",
"issue": "8",
"journal-title": "N Engl J Med",
"key": "10.1016/j.jinf.2021.12.039_bib0021",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.0369",
"article-title": "Effect of high-dose zinc and ascorbic acid supplementation vs usual care on symptom length and reduction among ambulatory patients with SARS-CoV-2 infection: the COVID A to Z randomized clinical trial",
"author": "Thomas",
"doi-asserted-by": "crossref",
"issue": "2",
"journal-title": "JAMA Netw Open",
"key": "10.1016/j.jinf.2021.12.039_bib0022",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.3390/nu13041261",
"article-title": "Does evidence exist to blunt inflammatory response by nutraceutical supplementation during COVID-19 pandemic? An overview of systematic reviews of vitamin D, vitamin C, Melatonin, and Zinc",
"author": "Corrao",
"doi-asserted-by": "crossref",
"first-page": "1261",
"issue": "4",
"journal-title": "Nutrients",
"key": "10.1016/j.jinf.2021.12.039_bib0023",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.04.015",
"article-title": "Enhancing immunity in viral infections, with special emphasis on COVID-19: a review",
"author": "Jayawardena",
"doi-asserted-by": "crossref",
"first-page": "367",
"issue": "4",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "10.1016/j.jinf.2021.12.039_bib0024",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1172/JCI116419",
"article-title": "Mucormycosis during deferoxamine therapy is a siderophore-mediated infection. In vitro and in vivo animal studies",
"author": "Boelaert",
"doi-asserted-by": "crossref",
"first-page": "1979",
"issue": "5",
"journal-title": "J Clin Invest",
"key": "10.1016/j.jinf.2021.12.039_bib0025",
"volume": "91",
"year": "1993"
},
{
"DOI": "10.1111/ejh.12421",
"article-title": "Impact of pretransplant serum ferritin level on risk of invasive mold infection after allogeneic hematopoietic stem cell transplantation",
"author": "Dadwal",
"doi-asserted-by": "crossref",
"first-page": "235",
"issue": "3",
"journal-title": "Eur J Haematol",
"key": "10.1016/j.jinf.2021.12.039_bib0026",
"volume": "94",
"year": "2015"
},
{
"DOI": "10.1128/CMR.13.2.236",
"article-title": "Zygomycetes in human disease",
"author": "Ribes",
"doi-asserted-by": "crossref",
"first-page": "236",
"issue": "2",
"journal-title": "Clin Microbiol Rev",
"key": "10.1016/j.jinf.2021.12.039_bib0027",
"volume": "13",
"year": "2000"
},
{
"DOI": "10.3390/ijerph17134624",
"article-title": "Facial skin temperature and discomfort when wearing protective face masks: thermal infrared imaging evaluation and hands moving the mask",
"author": "Scarano",
"doi-asserted-by": "crossref",
"first-page": "E4624",
"issue": "13",
"journal-title": "Int J Environ Res Public Health",
"key": "10.1016/j.jinf.2021.12.039_bib0028",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1136/bmjopen-2014-006577",
"article-title": "A cluster randomised trial of cloth masks compared with medical masks in healthcare workers",
"author": "MacIntyre",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "BMJ Open",
"key": "10.1016/j.jinf.2021.12.039_bib0029",
"volume": "5",
"year": "2015"
},
{
"DOI": "10.1136/bmjresp-2020-000698",
"article-title": "Last-resort strategies during mask shortages: optimal design features of cloth masks and decontamination of disposable masks during the COVID-19 pandemic",
"author": "Bhattacharjee",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "BMJ Open Respir Res",
"key": "10.1016/j.jinf.2021.12.039_bib0030",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.cmi.2018.07.011",
"article-title": "The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports",
"author": "Jeong",
"doi-asserted-by": "crossref",
"first-page": "26",
"issue": "1",
"journal-title": "Clin Microbiol Infect",
"key": "10.1016/j.jinf.2021.12.039_bib0031",
"volume": "25",
"year": "2019"
},
{
"article-title": "Intercepting the deadly trinity of mucormycosis, diabetes and COVID-19 in India",
"author": "Banerjee",
"journal-title": "Postgrad Med J [Internet].",
"key": "10.1016/j.jinf.2021.12.039_bib0032",
"year": "2021"
},
{
"key": "10.1016/j.jinf.2021.12.039_bib0033",
"unstructured": "Covid19india.org. Coronavirus in India [Internet]. [cited 2021 Jun 21]. Available from: https://www.covid19india.org"
}
],
"reference-count": 33,
"references-count": 33,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S016344532100654X"
}
},
"score": 1,
"short-container-title": [
"Journal of Infection"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Microbiology (medical)"
],
"subtitle": [],
"title": [
"Risk factors for Coronavirus disease-associated mucormycosis"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "84"
}
