Effect of Aspirin Use on clinical Outcome among Critically Ill Patients with COVID-19
et al., Egyptian Journal of Anaesthesia, doi:10.1080/11101849.2022.2139104, Oct 2022
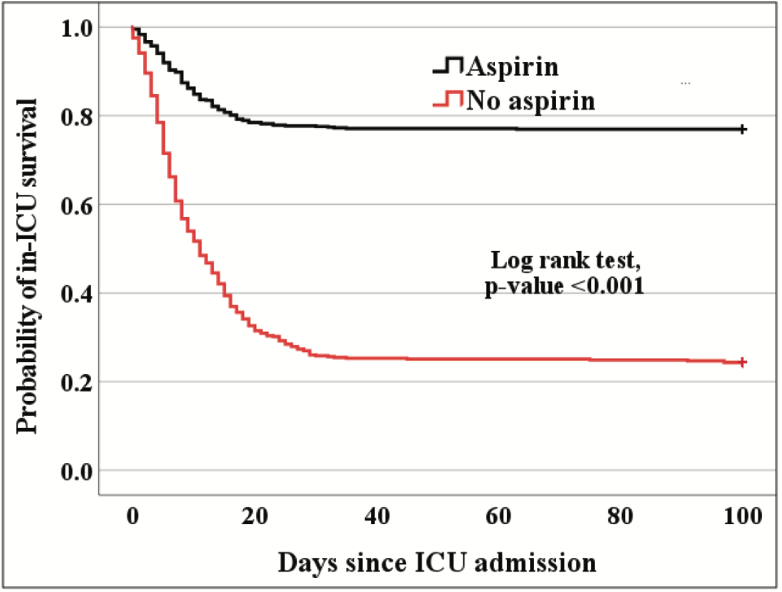
Retrospective 1,190 ICU patients in Egypt, showing lower mortality with aspirin treatment. 150mg daily.
|
risk of death, 39.6% lower, RR 0.60, p < 0.001, treatment 152 of 660 (23.0%), control 202 of 530 (38.1%), NNT 6.6.
|
|
risk of ARDS, 37.4% lower, RR 0.63, p = 0.001, treatment 74 of 660 (11.2%), control 95 of 530 (17.9%), NNT 15.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ali et al., 31 Oct 2022, retrospective, Egypt, peer-reviewed, 3 authors.
Contact: rania_m_ismail@yahoo.com.
Effect of Aspirin Use on clinical Outcome among Critically Ill Patients with COVID- 19
Egyptian Journal of Anaesthesia, doi:10.1080/11101849.2022.2139104
Background: Critically ill COVID-19 patients are at risk of developing major complications with high mortality rate. Aspirin might have favorable effects in severe COVID-19 via various mechanisms besides inhibition of platelet aggregation. The role of aspirin as adjuvant therapy in critically ill patients with COVID-19 has not been studied. In this study, we investigated the correlation between aspirin use and the clinical outcome in critically ill COVID-19 patients. Methods: This is a retrospective cohort observational study of critically ill COVID-19 Egyptian patients. Participants were divided into two groups: patients who received aspirin, 150 mg per day orally, upon admission to the intensive care unit, and those who did not. The primary outcome in this study was the shift to invasive ventilatory support. Results: A total of 1190 patients were involved in the study, 660 patients received aspirin, while 530 patients did not. Among aspirin group compared to non-aspirin group, invasive ventilatory support, DVT, PE, stroke, ACS, ARDS, AKI, septic shock, and mortality were less frequent, and the differences were significant except for ACS, AKI, and septic shock. Major bleeding was non-significantly more frequent. The length of ICU stay was significantly longer among non-survivors, and shorter among survivors. The variations between the two groups were significant among subgroups ≥40 or 60. Conclusions: In critically ill patients with COVID-19, aspirin has the potential role as an adjuvant therapeutic, lowering the risk of mechanical ventilation, thromboembolic events, ARDS, and ICU mortality. Patients older than 40 years were a significant category that might benefit from aspirin.
Disclosure statement No potential conflict of interest was reported by the author(s).
References
Azboy, Barrack, Thomas, Aspirin and the prevention of venous thromboembolism following total joint arthroplasty: commonly asked questions, Bone Joint J
Becattini, Agnelli, Schenone, Aspirin for preventing the recurrence of venous thromboembolism, N Engl J Med
Bradbury, Lawler, Stanworth, Investigators, Effect of antiplatelet therapy on survival and organ support-free days in critically ill patients with COVID-19: a randomized clinical trial, JAMA
Brighton, Eikelboom, Mann, Low-dose aspirin for preventing recurrent venous thromboembolism, N Engl J Med
Chow, Khanna, Kethireddy, Aspirin use is associated with decreased mechanical ventilation, intensive care unit admission, and in-hospital mortality in hospitalized patients with coronavirus disease, Anesth Analg, doi:10.1213/ANE.0000000000005292
Chow, Rahnavard, Gomberg-Maitland, Association of early aspirin use with in-hospital mortality in patients with moderate COVID-19, JAMA Netw open
Guan, Ni, Hu, Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med
Ikonomidis, Andreotti, Economou, Increased proinflammatory cytokines in patients with chronic stable angina and their reduction by aspirin, Circulation
Ismail, Bensasi, Taha, Characteristics and outcome of critically ill patients with coronavirus disease-2019 (COVID-19) pneumonia admitted to a tertiary care center in the United Arab Emirates during the first wave of the SARS-CoV-2 pandemic. A retrospective analysis, PLoS One
Kor, Carter, Park, Effect of aspirin on development of ARDS in at-risk patients presenting to the emergency department: the LIPS-a randomized clinical trial, JAMA
Liang, Liang, Ou, Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19, JAMA Intern Med
Middeldorp, Coppens, Van Haaps, Incidence of venous thromboembolism in hospitalized patients with COVID-19, J Thromb Haemost
Osborne, Veigulis, Arreola, Association of mortality and aspirin prescription for COVID-19 patients at the veterans health administration, PLoS One
Panka, De Grooth, Spoelstra-De Man, Prevention or treatment of ards with aspirin: a review of preclinical models and meta-analysis of clinical studies, Shock
Rapkiewicz, Mai, Carsons, Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series, EClinicalMedicine
Shaw, Bradbury, Abrams, COVID-19 and immunothrombosis: emerging understanding and clinical management, Br J Haematol
Varga, Flammer, Steiger, Endothelial cell infection and endotheliitis in COVID-19, Lancet
Voruganti, Bassareo, Calcaterra, Does aspirin save lives in patients with COVID-19?, Heart
Wijaya, Andhika, Huang, The effects of aspirin on the outcome of COVID-19: a systematic review and meta-analysis, Clin Epidemiol Glob Heal
DOI record:
{
"DOI": "10.1080/11101849.2022.2139104",
"ISSN": [
"1110-1849"
],
"URL": "http://dx.doi.org/10.1080/11101849.2022.2139104",
"alternative-id": [
"10.1080/11101849.2022.2139104"
],
"assertion": [
{
"label": "Peer Review Statement",
"name": "peerreview_statement",
"order": 1,
"value": "The publishing and review policy for this title is described in its Aims & Scope."
},
{
"URL": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=teja20",
"label": "Aim & Scope",
"name": "aims_and_scope_url",
"order": 2,
"value": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=teja20"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2022-09-03"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Revised",
"name": "revised",
"order": 1,
"value": "2022-10-08"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "2022-10-17"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 3,
"value": "2022-10-31"
}
],
"author": [
{
"affiliation": [
{
"name": "Department of Anesthesia, Intensive Care and Pain Management, Faculty of Medicine, Ain Shams University, Cairo, Egypt"
}
],
"family": "Ali",
"given": "Rania M.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Anesthesia, Intensive Care and Pain Management, Faculty of Medicine, Ain Shams University, Cairo, Egypt"
}
],
"family": "Tharwat",
"given": "Ayman I.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Anesthesia, Intensive Care and Pain Management, Faculty of Medicine, Ain Shams University, Cairo, Egypt"
}
],
"family": "Labib",
"given": "Heba A.",
"sequence": "additional"
}
],
"container-title": "Egyptian Journal of Anaesthesia",
"container-title-short": "Egyptian Journal of Anaesthesia",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"www.tandfonline.com"
]
},
"created": {
"date-parts": [
[
2022,
11,
1
]
],
"date-time": "2022-11-01T06:30:42Z",
"timestamp": 1667284242000
},
"deposited": {
"date-parts": [
[
2022,
11,
1
]
],
"date-time": "2022-11-01T06:30:43Z",
"timestamp": 1667284243000
},
"indexed": {
"date-parts": [
[
2022,
11,
2
]
],
"date-time": "2022-11-02T05:01:48Z",
"timestamp": 1667365308444
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2022,
10,
31
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2022,
12,
31
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
10,
31
]
],
"date-time": "2022-10-31T00:00:00Z",
"timestamp": 1667174400000
}
}
],
"link": [
{
"URL": "https://www.tandfonline.com/doi/pdf/10.1080/11101849.2022.2139104",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "629-635",
"prefix": "10.1080",
"published": {
"date-parts": [
[
2022,
10,
31
]
]
},
"published-online": {
"date-parts": [
[
2022,
10,
31
]
]
},
"published-print": {
"date-parts": [
[
2022,
12,
31
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1111/bjh.17664",
"doi-asserted-by": "publisher",
"key": "cit0001"
},
{
"DOI": "10.1371/journal.pone.0251687",
"doi-asserted-by": "publisher",
"key": "cit0002"
},
{
"DOI": "10.1111/jth.14888",
"doi-asserted-by": "publisher",
"key": "cit0003"
},
{
"DOI": "10.1136/heartjnl-2021-320255",
"doi-asserted-by": "publisher",
"key": "cit0004"
},
{
"DOI": "10.1213/ANE.0000000000005292",
"doi-asserted-by": "publisher",
"key": "cit0005"
},
{
"DOI": "10.1001/jamanetworkopen.2022.3890",
"doi-asserted-by": "publisher",
"key": "cit0006"
},
{
"DOI": "10.1016/j.eclinm.2020.100434",
"doi-asserted-by": "publisher",
"key": "cit0007"
},
{
"DOI": "10.1016/S0140-6736(20)30937-5",
"doi-asserted-by": "publisher",
"key": "cit0008"
},
{
"DOI": "10.1016/j.cegh.2021.100883",
"doi-asserted-by": "publisher",
"key": "cit0009"
},
{
"DOI": "10.1161/01.CIR.100.8.793",
"doi-asserted-by": "publisher",
"key": "cit0010"
},
{
"DOI": "10.1016/S0140-6736(21)01825-0",
"doi-asserted-by": "publisher",
"key": "cit0011"
},
{
"DOI": "10.1001/jama.2016.6330",
"doi-asserted-by": "publisher",
"key": "cit0012"
},
{
"DOI": "10.1097/SHK.0000000000000745",
"doi-asserted-by": "publisher",
"key": "cit0013"
},
{
"DOI": "10.1371/journal.pone.0246825",
"doi-asserted-by": "publisher",
"key": "cit0014"
},
{
"DOI": "10.1001/jama.2022.2910",
"doi-asserted-by": "publisher",
"key": "cit0015"
},
{
"DOI": "10.1056/NEJMoa1114238",
"doi-asserted-by": "publisher",
"key": "cit0016"
},
{
"DOI": "10.1056/NEJMoa1210384",
"doi-asserted-by": "publisher",
"key": "cit0017"
},
{
"DOI": "10.1302/0301-620X.99B11.BJJ-2017-0337.R2",
"doi-asserted-by": "publisher",
"key": "cit0018"
},
{
"DOI": "10.1056/NEJMoa2002032",
"doi-asserted-by": "publisher",
"key": "cit0019"
},
{
"DOI": "10.1001/jamainternmed.2020.2033",
"doi-asserted-by": "publisher",
"key": "cit0020"
}
],
"reference-count": 20,
"references-count": 20,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.tandfonline.com/doi/full/10.1080/11101849.2022.2139104"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Anesthesiology and Pain Medicine"
],
"subtitle": [],
"title": "Effect of Aspirin Use on clinical Outcome among Critically Ill Patients with COVID- 19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1080/tandf_crossmark_01",
"volume": "38"
}