Genetic and immunological evaluation of children with inborn errors of immunity and severe or critical COVID-19
et al., Journal of Allergy and Clinical Immunology, doi:10.1016/j.jaci.2022.09.005, Sep 2022
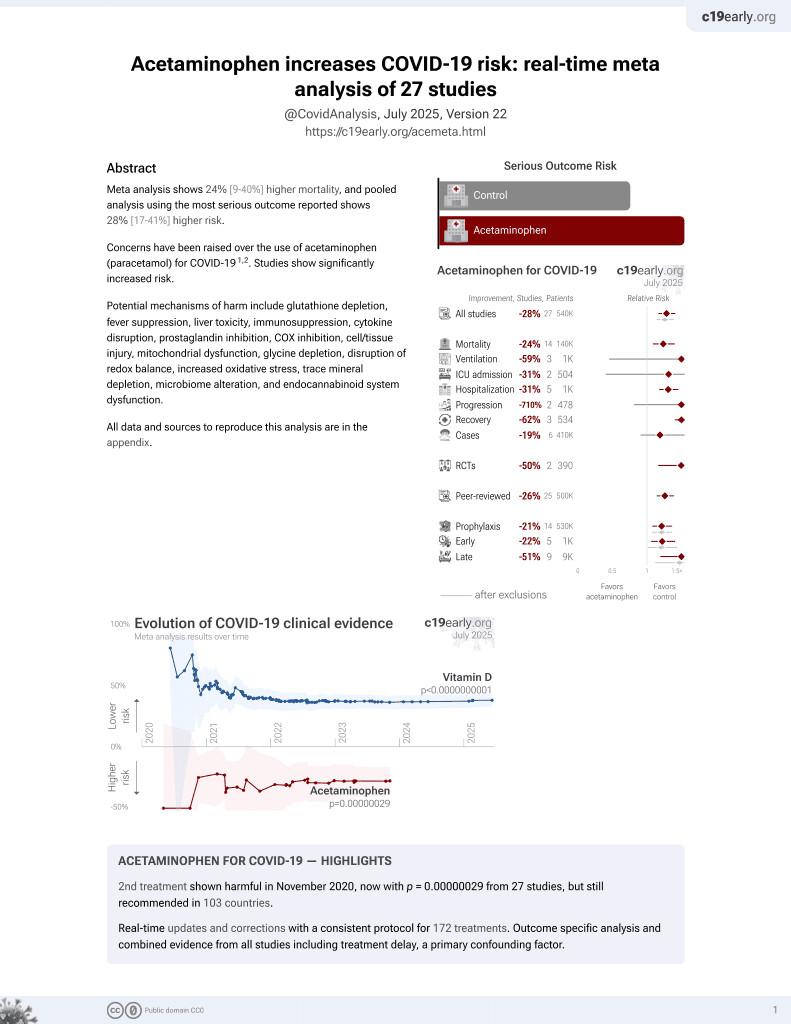
2nd treatment shown to increase risk in
November 2020, now with p = 0.00000029 from 27 studies, but still recommended in 103 countries.
6,400+ studies for
210+ treatments. c19early.org
|
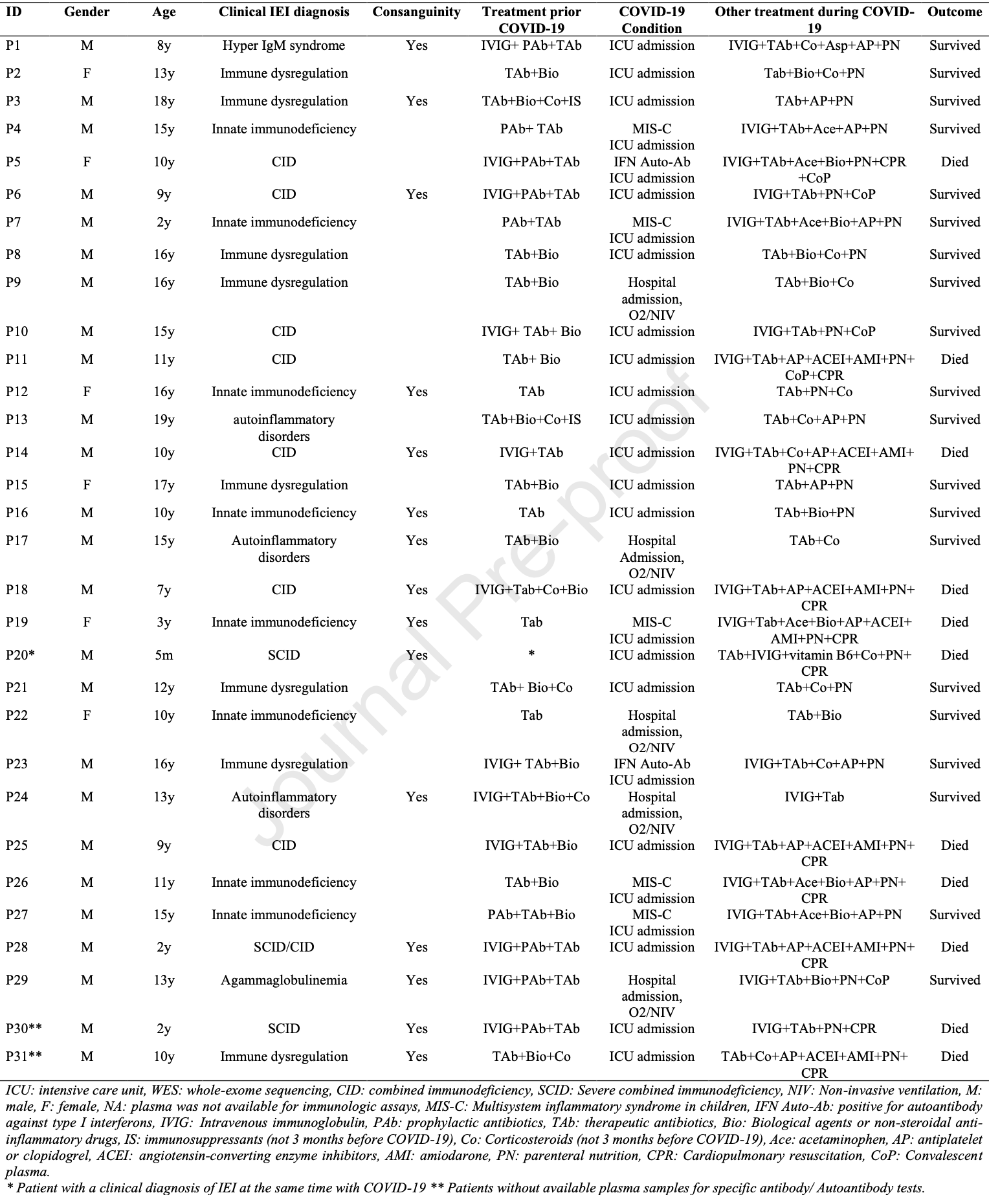
Retrospective 31 hospitalized patients ≤19 with pre-existing inborn errors of immunity, showing no significant difference in mortality with acetaminophen. Only 6 patients were treated with acetaminophen.
Acetaminophen is also known as paracetamol, Tylenol, Panadol, Calpol, Tempra, Calprofen, Doliprane, Efferalgan, Grippostad C, Dolo, Acamol, Fevadol, Crocin, and Perfalgan.
|
risk of death, 56.2% higher, RR 1.56, p = 0.64, treatment 3 of 6 (50.0%), control 8 of 25 (32.0%).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Abolhassani et al., 13 Sep 2022, retrospective, Iran, peer-reviewed, 23 authors.
Contact: qiang.pan-hammarstrom@ki.se (corresponding author), lennart.hammarstrom@ki.se.
Genetic and immunologic evaluation of children with inborn errors of immunity and severe or critical COVID-19
Journal of Allergy and Clinical Immunology, doi:10.1016/j.jaci.2022.09.005
This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Abbreviations
J o u r n a l P r e -p r o o f Author contributions HA, SD, NL, SS, PB, LD, FZ, AH, FA, SI, MM, AV, FS, MAG, were involved in subject recruitment and sample acquisition. HA, NL, AC, HM, SYZ, QZ, NR, JLC, OK, LH, QPH were involved in the interpretation of results HA, LH, QPH wrote the manuscript. All authors reviewed and approved the manuscript. LH, and QPH designed the laboratory protocols and supervised the entirety of the project.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Abolhassani, Aghamohammadi, Fang, Rezaei, Jiang et al., Clinical implications of systematic phenotyping and exome sequencing in patients with primary antibody deficiency, Genet Med, doi:10.1038/s41436-018-0012-x
Abolhassani, Azizi, Sharifi, Yazdani, Mohsenzadegan et al., Global systematic review of primary immunodeficiency registries, Expert Rev Clin Immunol, doi:10.1080/1744666X.2020.1801422
Abolhassani, Hammarstrom, Cunningham-Rundles, Current genetic landscape in common variable immune deficiency, Blood, doi:10.1182/blood.2019000929
Abolhassani, Kiaee, Tavakol, Chavoshzadeh, Mahdaviani et al., Fourth update on the Iranian national registry of primary immunodeficiencies: Integration of molecular diagnosis, J Clin Immunol, doi:10.1007/s10875-018-0556-1
Abolhassani, Landegren, Bastard, Materna, Modaresi et al., Inherited IFNAR1 deficiency in a child with both critical COVID-19 pneumonia and multisystem inflammatory syndrome, J Clin Immunol, doi:10.1007/s10875-022-01215-7
Abolhassani, Tavakol, Chavoshzadeh, Mahdaviani, Momen et al., National consensus on diagnosis and management guidelines for primary immunodeficiency, Immunology and Genetics Journal, doi:10.22034/igj.2019.85743
Abolhassani, Vosughimotlagh, Asano, Landegren, Boisson et al., X-Linked TLR7 Deficiency Underlies Critical COVID-19 Pneumonia in a Male Patient with Ataxia-Telangiectasia, J Clin Immunol, doi:10.1007/s10875-021-01151-y
Aghamohammadi, Rezaei, Yazdani, Delavari, Kutukculer et al., Consensus Middle East and North Africa Registry on Inborn Errors of Immunity, J Clin Immunol, doi:10.1007/s10875-021-01053-z
Asano, Boisson, Onodi, Matuozzo, Moncada-Velez et al., Xlinked recessive TLR7 deficiency in ~1% of men under 60 years old with life-threatening COVID-19
Azizi, Ahmadi, Abolhassani, Yazdani, Mohammadi et al., Autoimmunity in Primary Antibody Deficiencies, Int Arch Allergy Immunol, doi:10.1159/000453263
Azizi, Tavakol, Rafiemanesh, Kiaee, Yazdani et al., Autoimmunity in a cohort of 471 patients with primary antibody deficiencies, Expert Rev Clin Immunol, doi:10.1080/1744666X.2017.1384312
Bastard, Gervais, Voyer, Rosain, Philippot et al., Autoantibodies neutralizing type I IFNs are present in ~4% of uninfected individuals over 70 years old and account for ~20% of COVID-19 deaths, Sci Immunol, doi:10.1126/sciimmunol.abl4340
Bastard, Manry, Chen, Rosain, Seeleuthner et al., Herpes simplex encephalitis in a patient with a distinctive form of inherited IFNAR1 deficiency, J Clin Invest, doi:10.1172/JCI139980
Bastard, Orlova, Sozaeva, Levy, James et al., Preexisting autoantibodies to type I IFNs underlie critical COVID-19 pneumonia in patients with APS-1, J Exp Med, doi:10.1084/jem.20210554
Bastard, Rosen, Zhang, Michailidis, Hoffmann et al., Autoantibodies against type I IFNs in patients with life-threatening COVID-19, Science, doi:10.1126/science.abd4585
Benetti, Giliberti, Emiliozzi, Valentino, Bergantini et al., Clinical and molecular characterization of COVID-19 hospitalized patients, PLoS One, doi:10.1371/journal.pone.0242534
Breda, Nozzi, Sanctis, Chiarelli, Laboratory tests in the diagnosis and follow-up of pediatric rheumatic diseases: an update, Semin Arthritis Rheum, doi:10.1016/j.semarthrit.2008.12.001
Bucciol, Tangye, Meyts, Coronavirus disease 2019 in patients with inborn errors of immunity: lessons learned, Curr Opin Pediatr, doi:10.1097/MOP.0000000000001062
Burgner, Crawford, Goeman, Gray, Hsu, COVID-19 in children. II: Pathogenesis, disease spectrum and management, J Paediatr Child Health, doi:10.1111/jpc.15811
Consiglio, Cotugno, Sardh, Pou, Amodio et al., The Immunology of Multisystem Inflammatory Syndrome in Children with COVID-19, Cell, doi:10.1016/j.cell.2020.09.016
Delavari, Abolhassani, Abolnezhadian, Babaha, Iranparast et al., Impact of SARS-CoV-2 pandemic on patients with primary immunodeficiency, J Clin Immunol, doi:10.1007/s10875-020-00928-x
Dong, Mo, Hu, Qi, Jiang et al., Epidemiology of COVID-19 Among Children in China, Pediatrics, doi:10.1542/peds.2020-0702
Duncan, Randall, Hambleton, Genetic lesions of type I Interferon signalling in human antiviral immunity, Trends Genet, doi:10.1016/j.tig.2020.08.017
Fallerini, Daga, Mantovani, Benetti, Picchiotti et al., Association of Toll-like receptor 7 variants with life-threatening COVID-19 disease in males: findings from a nested casecontrol study, Elife, doi:10.7554/eLife.67569
Funk, Florin, Kuppermann, Tancredi, Xie et al., Outcomes of SARS-CoV-2-Positive Youths Tested in Emergency Departments: The Global PERN-COVID-19 Study, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.42322
Garcia-Morato, Apalategi, Bravo-Gallego, Moreno, Simon-Fuentes et al., Impaired control of multiple viral infections in a family with complete IRF9 deficiency, J Allergy Clin Immunol, doi:10.1016/j.jaci.2019.02.019
Gavriilaki, Asteris, Touloumenidou, Koravou, Koutra et al., Genetic justification of severe COVID-19 using a rigorous algorithm, Clin Immunol, doi:10.1016/j.clim.2021.108726
Giardino, Romano, Coppola, Cillo, Borzachiello et al., SARS-CoV-2 Infection in the Immunodeficient Host: Necessary and Dispensable Immune Pathways, J Allergy Clin Immunol Pract, doi:10.1016/j.jaip.2021.06.045
Gotzinger, Santiago-Garcia, Noguera-Julian, Lanaspa, Lancella et al., COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study, Lancet Child Adolesc Health, doi:10.1016/S2352-4642(20)30177-2
Gotzinger, Santiago-Garcia, Noguera-Julian, Lanaspa, Lancella et al., COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study, Lancet Child Adolesc Health, doi:10.1016/S2352-4642(20)30177-2
Haidar, Mellors, Improving the outcomes of immunocompromised patients with COVID-19, Clin Infect Dis, doi:10.1093/cid/ciab397
Hambleton, Goodbourn, Young, Dickinson, Mohamad et al., STAT2 deficiency and susceptibility to viral illness in humans, Proc Natl Acad Sci U S A, doi:10.1073/pnas.1220098110
Hammarstrom, Abolhassani, Baldanti, Marcotte, Pan-Hammarstrom, Development of passive immunity against SARS-CoV-2 for management of immunodeficient patients-a perspective, J Allergy Clin Immunol, doi:10.1016/j.jaci.2020.04.043
Hammarstrom, Marcotte, Piralla, Baldanti, Pan-Hammarstrom, Antibody therapy for COVID-19, Curr Opin Allergy Clin Immunol, doi:10.1097/ACI.0000000000000787
Hernandez, Bucciol, Moens, Pen, Shahrooei et al., Inherited IFNAR1 deficiency in otherwise healthy patients with adverse reaction to measles and yellow fever live vaccines, J Exp Med, doi:10.1084/jem.20182295
Hernandez, Melki, Jing, Habib, Huang et al., Life-threatening influenza pneumonitis in a child with inherited IRF9 deficiency, J Exp Med, doi:10.1084/jem.20180628
Initiative, Mapping the human genetic architecture of COVID-19, Nature, doi:10.1038/s41586-021-03767-x
Itan, Shang, Boisson, Ciancanelli, Markle et al., The mutation significance cutoff: gene-level thresholds for variant predictions, Nat Methods, doi:10.1038/nmeth.3739
J O U R N A L P R E, -p r o o f
J O U R N A L P R E, -p r o o f
Kapustova, Petrovicova, Banovcin, Antosova, Bobcakova et al., COVID-19 and the differences in physiological background between children and adults and their clinical consequences, Physiol Res, doi:10.33549/physiolres.934759
Kousathanas, Pairo-Castineira, Rawlik, Stuckey, Odhams et al., Whole genome sequencing reveals host factors underlying critical Covid-19, Nature, doi:10.1038/s41586-022-04576-6
Kreins, Ciancanelli, Okada, Kong, Ramirez-Alejo et al., Human TYK2 deficiency: Mycobacterial and viral infections without hyper-IgE syndrome, J Exp Med, doi:10.1084/jem.20140280
Ladhani, Amin-Chowdhury, Davies, Aiano, Hayden et al., COVID-19 in children: analysis of the first pandemic peak in England, Arch Dis Child, doi:10.1136/archdischild-2020-320042
Lang-Meli, Fuchs, Mathe, Ho, Kern et al., Case Series: Convalescent Plasma Therapy for Patients with COVID-19 and Primary Antibody Deficiency, J Clin Immunol, doi:10.1007/s10875-021-01193-2
Ledford, Deaths from COVID 'incredibly rare'among children, Nature, doi:10.1038/d41586-021-01897-w
Li, Lei, Zhang, Rapaport, Seeleuthner et al., Biochemically deleterious human NFKB1 variants underlie an autosomal dominant form of common variable immunodeficiency, J Exp Med, doi:10.1084/jem.20210566
Li, Wang, InterVar: Clinical interpretation of genetic variants by the 2015 ACMG-AMP guidelines, Am J Hum Genet, doi:10.1016/j.ajhg.2017.01.004
Lorenzini, Fliegauf, Klammer, Frede, Proietti et al., Characterization of the clinical and immunologic phenotype and management of 157 individuals with 56 distinct heterozygous NFKB1 mutations, J Allergy Clin Immunol, doi:10.1016/j.jaci.2019.11.051
Lundberg, Eriksson, Tran, Assarsson, Fredriksson, Homogeneous antibody-based proximity extension assays provide sensitive and specific detection of low-abundant proteins in human blood, Nucleic Acids Res, doi:10.1093/nar/gkr424
Marcotte, Piralla, Zuo, Du, Cassaniti et al., Immunity to SARS-CoV-2 up to 15 months after infection, iScience, doi:10.1016/j.isci.2022.103743
Mccrindle, Bw, Rowley, Newburger, Burns et al., Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association, Circulation, doi:10.1161/CIR.0000000000000484
Meyts, Bucciol, Quinti, Neven, Fischer et al., Coronavirus disease 2019 in patients with inborn errors of immunity: an international study, J Allergy Clin Immunol, doi:10.1016/j.jaci.2020.09.010
Milito, Soccodato, Pulvirenti, Quinti, COVID-19 in complex common variable immunodeficiency patients affected by lung diseases, Curr Opin Allergy Clin Immunol, doi:10.1097/ACI.0000000000000789
Modell, Orange, Quinn, Modell, Global report on primary immunodeficiencies: 2018 update from the Jeffrey Modell Centers Network on disease classification, regional trends, treatment modalities, and physician reported outcomes, Immunol Res, doi:10.1007/s12026-018-8996-5
Nikolopoulou, Maltezou, COVID-19 in children: where do we stand?, Arch Med Res, doi:10.1016/j.arcmed.2021.07.002
Parri, Lenge, Buonsenso, Coronavirus infection in pediatric emergency departments research group. Children with Covid-19 in pediatric emergency departments in Italy, N Engl J Med, doi:10.1056/NEJMc2007617
Pierce, Sy, Galen, Goldstein, Orner et al., Natural mucosal barriers and COVID-19 in children, JCI Insight, doi:10.1172/jci.insight.148694
Quinti, Lougaris, Milito, Cinetto, Pecoraro et al., A possible role for B cells in COVID-19? Lesson from patients with agammaglobulinemia, J Allergy Clin Immunol, doi:10.1016/j.jaci.2020.04.013
Richards, Aziz, Bale, Bick, Das et al., Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology, Genet Med, doi:10.1038/gim.2015.30
Rodriguez, Pekkarinen, Lakshmikanth, Tan, Consiglio et al., Systems-Level Immunomonitoring from Acute to Recovery Phase of Severe COVID-19, Cell Rep Med, doi:10.1016/j.xcrm.2020.100078
Sancho-Shimizu, Brodin, Cobat, Biggs, Toubiana et al., SARS-CoV-2-related MIS-C: A key to the viral and genetic causes of Kawasaki disease?, J Exp Med, doi:10.1084/jem.20210446
Satyam, Tsokos, Brook, Hecht, Moulton et al., Activation of classical and alternative complement pathways in the pathogenesis of lung injury in COVID-19, Clin Immunol, doi:10.1016/j.clim.2021.108716
Seidel, Kindle, Gathmann, Quinti, Buckland et al., The European Society for Immunodeficiencies (ESID) Registry Working Definitions for the Clinical Diagnosis of Inborn Errors of Immunity, J Allergy Clin Immunol Pract, doi:10.1016/j.jaip.2019.02.004
Sherina, Piralla, Du, Wan, Kumagai-Braesch et al., Persistence of SARS-CoV-2-specific B and T cell responses in convalescent COVID-19 patients 6-8 months after the infection, Med, doi:10.1016/j.medj.2021.02.001
Sowers, Galantino, Living with primary immunodeficiency disease during the Covid-19 pandemic, Z Gesundh Wiss, doi:10.1007/s10389-021-01545-7
Tangye, Al-Herz, Bousfiha, Chatila, Cunningham-Rundles et al., Human Inborn Errors of Immunity: 2019 Update on the Classification from the International Union of Immunological Societies Expert Committee, J Clin Immunol, doi:10.1007/s10875-019-00737-x
Tangye, Al-Herz, Bousfiha, Cunningham-Rundles, Franco et al., The Ever-Increasing Array of Novel Inborn Errors of Immunity: an Interim Update by the IUIS Committee, J Clin Immunol, doi:10.1007/s10875-021-00980-1
Trelle, Ramsey, Lee, Zheng, Lamboy et al., Binding of NFkappaB Appears to Twist the Ankyrin Repeat Domain of IkappaBalpha, Biophys J, doi:10.1016/j.bpj.2016.01.001
Van Der Made, Simons, Schuurs-Hoeijmakers, Van Den Heuvel, Mantere et al., Presence of Genetic Variants Among Young Men With Severe COVID-19, JAMA, doi:10.1001/jama.2020.13719
Wang, Abolhassani, Hammarstrom, Pan-Hammarstrom, SARS-CoV-2 infection in patients with inborn errors of immunity due to DNA repair defects, Acta Biochim Biophys Sin, doi:10.3724/abbs.2022071
Wang, Berger, Kaelber, Davis, Volkow et al., COVID infection severity in children under 5 years old before and after Omicron emergence in the US, medRxiv, doi:10.1101/2022.01.12.22269179
Wang, Huang, Gao, Zhou, Lai et al., Initial whole-genome sequencing and analysis of the host genetic contribution to COVID-19 severity and susceptibility, Cell Discov, doi:10.1038/s41421-020-00231-4
Yu, Gerber, Chen, Yuan, Chaturvedi et al., Complement dysregulation is associated with severe COVID-19 illness, Haematologica, doi:10.3324/haematol.2021.279155
Zhang, Bastard, Effort, Cobat, Casanova, Human genetic and immunological determinants of critical COVID-19 pneumonia, Nature, doi:10.1038/s41586-022-04447-0
Zhang, Boisson-Dupuis, Chapgier, Yang, Bustamante et al., Inborn errors of interferon (IFN)-mediated immunity in humans: insights into the respective roles of IFN-alpha/beta, J o u r n a l P r e -p r o o f IFN-gamma, and IFN-lambda in host defense, Immunol Rev, doi:10.1111/j.1600-065X.2008.00698
Zhang, Matuozzo, Pen, Lee, Moens et al., Recessive inborn errors of type I IFN immunity in children with COVID-19 pneumonia, J Exp Med, doi:10.1084/jem.20220131
DOI record:
{
"DOI": "10.1016/j.jaci.2022.09.005",
"ISSN": [
"0091-6749"
],
"URL": "http://dx.doi.org/10.1016/j.jaci.2022.09.005",
"alternative-id": [
"S009167492201185X"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Genetic and immunological evaluation of children with inborn errors of immunity and severe or critical COVID-19"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Journal of Allergy and Clinical Immunology"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jaci.2022.09.005"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2022 Published by Elsevier Inc. on behalf of the American Academy of Allergy, Asthma & Immunology."
}
],
"author": [
{
"affiliation": [],
"family": "Abolhassani",
"given": "Hassan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Delavari",
"given": "Samaneh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Landegren",
"given": "Nils",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shokri",
"given": "Sima",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bastard",
"given": "Paul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Du",
"given": "Likun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zuo",
"given": "Fanglei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hajebi",
"given": "Reza",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abolnezhadian",
"given": "Farhad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Iranparast",
"given": "Sara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Modaresi",
"given": "Mohammadreza",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vosughimotlagh",
"given": "Ahmad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Salami",
"given": "Fereshte",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aranda-Guillén",
"given": "Maribel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cobat",
"given": "Aurélie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Marcotte",
"given": "Harold",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Shen-Ying",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Qian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rezaei",
"given": "Nima",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Casanova",
"given": "Jean-Laurent",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kämpe",
"given": "Olle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hammarström",
"given": "Lennart",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pan-Hammarström",
"given": "Qiang",
"sequence": "additional"
}
],
"container-title": "Journal of Allergy and Clinical Immunology",
"container-title-short": "Journal of Allergy and Clinical Immunology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.com.au",
"clinicalkey.es",
"clinicalkey.com",
"jacionline.org",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2022,
9,
13
]
],
"date-time": "2022-09-13T16:03:36Z",
"timestamp": 1663085016000
},
"deposited": {
"date-parts": [
[
2022,
9,
13
]
],
"date-time": "2022-09-13T16:03:37Z",
"timestamp": 1663085017000
},
"indexed": {
"date-parts": [
[
2022,
9,
13
]
],
"date-time": "2022-09-13T16:45:37Z",
"timestamp": 1663087537942
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
9
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
9,
1
]
],
"date-time": "2022-09-01T00:00:00Z",
"timestamp": 1661990400000
}
},
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 11,
"start": {
"date-parts": [
[
2022,
9,
12
]
],
"date-time": "2022-09-12T00:00:00Z",
"timestamp": 1662940800000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S009167492201185X?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S009167492201185X?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
9
]
]
},
"published-print": {
"date-parts": [
[
2022,
9
]
]
},
"publisher": "Elsevier BV",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S009167492201185X"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Immunology",
"Immunology and Allergy"
],
"subtitle": [],
"title": "Genetic and immunological evaluation of children with inborn errors of immunity and severe or critical COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}