Associations between the Dietary Inflammatory Index and COVID-19 Outcomes in the UK Biobank Cohort
et al., SSRN Electronic Journal, doi:10.2139/ssrn.4300209, Dec 2022
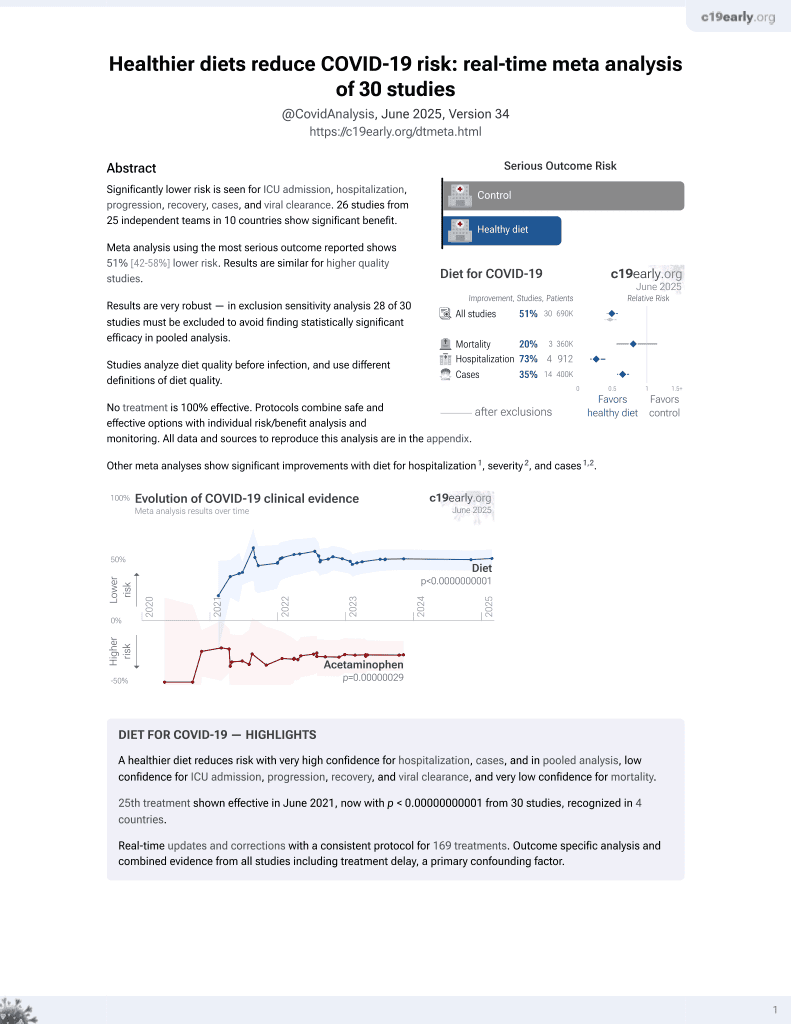
Diet for COVID-19
26th treatment shown to reduce risk in
June 2021, now with p < 0.00000000001 from 30 studies, recognized in 4 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
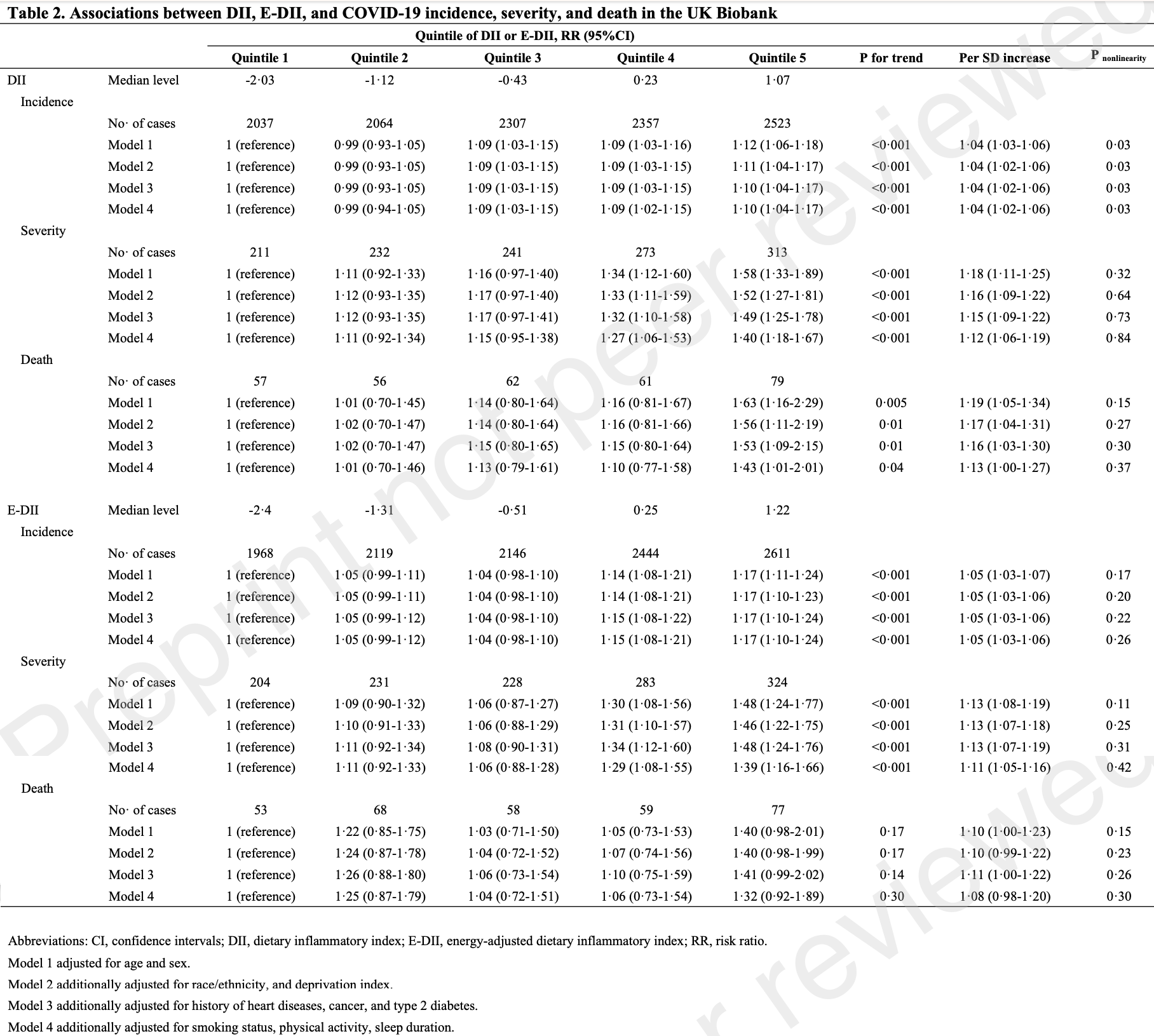
UK Biobank retrospective 196,154 participants with 11,288 COVID-19 cases, showing lower COVID-19 mortality, severity, and incidence for lower dietary inflammatory scores.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 24.2% lower, RR 0.76, p = 0.13, higher quality diet 39,230, lower quality diet 39,231, adjusted per study, inverted to make RR<1 favor higher quality diet, E-DII, quintile 1 vs. quintile 5, multivariable, model 4.
|
|
risk of death, 30.1% lower, RR 0.70, p = 0.04, higher quality diet 39,230, lower quality diet 39,231, adjusted per study, inverted to make RR<1 favor higher quality diet, DII, quintile 1 vs. quintile 5, multivariable, model 4.
|
|
risk of severe case, 28.1% lower, RR 0.72, p < 0.001, higher quality diet 39,230, lower quality diet 39,231, adjusted per study, inverted to make RR<1 favor higher quality diet, E-DII, quintile 1 vs. quintile 5, multivariable, model 4.
|
|
risk of severe case, 28.6% lower, RR 0.71, p < 0.001, higher quality diet 39,230, lower quality diet 39,231, adjusted per study, inverted to make RR<1 favor higher quality diet, DII, quintile 1 vs. quintile 5, multivariable, model 4.
|
|
risk of case, 14.5% lower, RR 0.85, p < 0.001, higher quality diet 39,230, lower quality diet 39,231, adjusted per study, inverted to make RR<1 favor higher quality diet, E-DII, quintile 1 vs. quintile 5, multivariable, model 4.
|
|
risk of case, 9.1% lower, RR 0.91, p = 0.002, higher quality diet 39,230, lower quality diet 39,231, adjusted per study, inverted to make RR<1 favor higher quality diet, DII, quintile 1 vs. quintile 5, multivariable, model 4.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Zhao et al., 14 Dec 2022, retrospective, United Kingdom, peer-reviewed, survey, 9 authors, study period January 2020 - March 2021.
Contact: jhebert@mailbox.sc.edu.
Associations between the Dietary Inflammatory Index and COVID-19 outcomes in the
Government officers or employees acting as part of their official duties; on a worldwide, perpetual, irrevocable, royalty-free basis to BMJ Publishing Group Ltd ("BMJ") its licensees.
Research in context Evidence before this study We conducted a systematic search of the National Library of Medicine for articles on associations between diet and COVID-19 risk. We found that a limited number of studies have evaluated the role of specific food groups in the onset and progression of SARS-CoV-2 infection and COVID-19 symptoms. However, evidence on associations between dietary patterns or indexes, treating diet as a whole, is rare. Generally small studies have indicated that a healthy anti-inflammatory diet is associated with a lower risk of COVID-19 infection. However, there are no prospective data from sufficiently large cohorts to provide robust evidence on the effect of dietary inflammatory potential on the risk of COVID-19 incidence, disease severity, or mortality.
Competing interests: The authors declare that they have no competing interests.
Ethical approval: Not required. This preprint research paper has not been peer reviewed. Electronic copy available at: https://ssrn.com/abstract=4300209 P r e p r i n t n o t p e e r r e v i e w e d
22/24 This preprint research paper has not been peer reviewed. Electronic copy available at: https://ssrn.com/abstract=4300209 P r e p r i n t n o t p e e r r e v i e w e d This preprint research paper has not been peer reviewed. Electronic copy available at: https://ssrn.com/abstract=4300209 P r e p r i n t n o t p e e r r e v i e w e d
References
Allard, Ouedraogo, Molleville, Malnutrition: Percentage and Association with Prognosis in Patients Hospitalized for Coronavirus Disease 2019, Nutrients
Barazzoni, Bischoff, Breda, ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection, Clin Nutr
Bradbury, Young, Guo, Key, Dietary assessment in UK Biobank: an evaluation of the performance of the touchscreen dietary questionnaire, J Nutr Sci
Cecconello1, Ribas, Norling, Chapter 4. Resolving acute inflammation; what happens when inflammation goes haywire? How can it get back in line?
Chandra, Nutrition, immunity, and infection: present knowledge and future directions, Lancet
Deschasaux-Tanguy, Srour, Bourhis, Nutritional risk factors for SARS-CoV-2 infection: a prospective study within the NutriNet-Sante cohort, BMC Med
Fernandez-Ayala, Navas, Lopez-Lluch, Age-related mitochondrial dysfunction as a key factor in COVID-19 disease, Exp Gerontol
Fisman, Tuite, Evaluation of the relative virulence of novel SARS-CoV-2 variants: a retrospective cohort study in Ontario, Canada, CMAJ
Fu, Pei, Shivappa, Association between Dietary Inflammatory Index and Type 2 diabetes mellitus in Xinjiang Uyghur autonomous region, China, PeerJ
Furuyashiki, Akiyama, Kitaoka, Roles of multiple lipid mediators in stress and depression, Int Immunol
Hariharan, Odjidja, Scott, The dietary inflammatory index, obesity, type 2 diabetes, and cardiovascular risk factors and diseases, Obes Rev
Hebert, Chapter 2. History of nutrition and inflammation
Hebert, Shivappa, Wirth, Hussey, Hurley, Perspective: The Dietary Inflammatory Index (DII)-Lessons Learned, Improvements Made, and Future Directions, Advances in Nutrition
Hofseth, Hebert, Chapter 3. Diet and acute and chronic, systemic, low-grade inflammation
Holmes, Dick, Nelson, A comparison of four dietary assessment methods in materially deprived households in England, Public Health Nutr
Holt, Talaei, Greenig, Risk factors for developing COVID-19: a populationbased longitudinal study (COVIDENCE UK), Thorax
Hu, Dietary pattern analysis: a new direction in nutritional epidemiology, Curr Opin Lipidol
Keusch, The history of nutrition: malnutrition, infection and immunity, J Nutr
Khan, Heart failure and COVID-19: synergism of two inflammatory conditions?, Br J Community Nurs
Khoury, Julien, Inverse Association Between the Mediterranean Diet and COVID-19 Risk in Lebanon: A Case-Control Study, Front Nutr
Lee, Olefsky, Chronic tissue inflammation and metabolic disease, Genes Dev
Li, Hodge, Macinnis, Inflammation-Related Marker Profiling of Dietary Patterns and All-cause Mortality in the Melbourne Collaborative Cohort Study, J Nutr (Genomics, Proteomics, and Metabolomics
Liao, Gao, Cao, Associations of Metabolic/Obesity Phenotypes with Insulin Resistance and C-Reactive Protein: Results from the CNTR Study, Diabetes Metab Syndr Obes
Liu, Young, Crowe, Development and evaluation of the Oxford WebQ, a low-cost, web-based method for assessment of previous 24 h dietary intakes in large-scale prospective studies, Public Health Nutr
Liu, Zhou, Wang, Malnutrition is associated with hyperinflammation and immunosuppression in COVID-19 patients: A prospective observational study, Nutr Clin Pract
Malcomson, Willis, Mccallum, Diet-associated inflammation modulates inflammation and WNT signaling in the rectal mucosa, and the response to supplementation with dietary fibre, Cancer prevention research
Marx, Veronese, Kelly, The Dietary Inflammatory Index and Human Health: An Umbrella Review of Meta-Analyses of Observational Studies, Adv Nutr
Mccance, Widdowson, McCance and Widdowson's the Composition of Foods, Royal Society of Chemistry
Mcdiarmid, Wood, Upham, The Impact of Meal Dietary Inflammatory Index on Exercise-Induced Changes in Airway Inflammation in Adults with Asthma, Nutrients
Menzel, Samouda, Dohet, Loap, Ellulu et al., Common and Novel Markers for Measuring Inflammation and Oxidative Stress Ex Vivo in Research and Clinical Practice-Which to Use Regarding Disease Outcomes?, Antioxidants
Merino, Joshi, Nguyen, Diet quality and risk and severity of COVID-19: a prospective cohort study, Gut
Mittal, Ghosh, Bhatt, Anoop, Ansari et al., High prevalence of post COVID-19 fatigue in patients with type 2 diabetes: A case-control study, Diabetes Metab Syndr
Moludi, Qaisar, Alizadeh, The relationship between Dietary Inflammatory Index and disease severity and inflammatory status: a case-control study of COVID-19 patients, Br J Nutr
Morais, Aquino, Da Silva-Maia, Vale, Maciel et al., Nutritional status, diet and viral respiratory infections: perspectives for severe acute respiratory syndrome coronavirus 2, Br J Nutr
Morais, Aquino, Da Silva-Maia, Vale, Maciel et al., Nutritional status, diet and viral respiratory infections: perspectives for severe acute respiratory syndrome coronavirus 2, Br J Nutr
Ouchi, Parker, Lugus, Walsh, Adipokines in inflammation and metabolic disease, Nature Rev Immunol
Phillips, Chen, Heude, Dietary Inflammatory Index and Non-Communicable Disease Risk: A Narrative Review, Nutrients
Ponzo, Pellegrini, Eusebio, Mediterranean Diet and SARS-COV-2 Infection: Is There Any Association? A Proof-of-Concept Study, Nutrients
Sawadogo, Tsegaye, Gizaw, Adera, Overweight and obesity as risk factors for COVID-19-associated hospitalisations and death: systematic review and meta-analysis, BMJ Nutr Prev Health
Scrimshaw, INCAP studies of nutrition and infection, Food Nutr Bull
Seclen, Nunez-Robles, Yovera-Aldana, Arias-Chumpitaz, Incidence of COVID-19 infection and prevalence of diabetes, obesity and hypertension according to altitude in Peruvian population, Diabetes Res Clin Pract
Shivappa, Steck, Hurley, Hussey, Hebert, Designing and developing a literature-derived, population-based dietary inflammatory index, Public Health Nutr
Steck, Murphy, Dietary patterns and cancer risk, Nat Rev Cancer
Sudlow, Gallacher, Allen, UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age, PLoS Med
Sukkar, Bassetti, Induction of ketosis as a potential therapeutic option to limit hyperglycemia and prevent cytokine storm in COVID-19, Nutrition
Townsend, Phillimore, Beattie: A Health and deprivation: inequalities and the north
Vahid, Rahmani, Can an anti-inflammatory diet be effective in preventing or treating viral respiratory diseases? A systematic narrative review, Clin Nutr ESPEN
Wirth, Robinson, Murphy, Shivappa, Hebert, The dietary inflammatory index is associated with gastrointestinal infection symptoms in the national health and nutrition examination survey, Int J Food Sci Nutr
Yap, Marino, An Insight Into the Intestinal Web of Mucosal Immunity, Microbiota, and Diet in Inflammation, Front Immunol
Yi, Li, He, Associations of dietary inflammatory index with metabolic syndrome and its components: a systematic review and meta-analysis, Public Health Nutr
Yue, Ma, Accorsi, Long-term diet and risk of SARS -CoV-2 infection and Coronavirus Disease 2019 (COVID-19) severity, Am J Clin Nutr
Zhou, Li, Zhang, Yang, Ma et al., Impact of ultra-processed food intake on the risk of COVID-19: a prospective cohort study, Eur J Nutr
Zinder, Cooley, Vlad, Molnar, Vitamin A and Wound Healing, Nutr Clin Pract
DOI record:
{
"DOI": "10.2139/ssrn.4300209",
"ISSN": [
"1556-5068"
],
"URL": "http://dx.doi.org/10.2139/ssrn.4300209",
"author": [
{
"affiliation": [],
"family": "Zhao",
"given": "Longgang",
"sequence": "first"
},
{
"affiliation": [],
"family": "Wirth",
"given": "Michael D.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Petermann-Rocha",
"given": "Fanny",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Parra-Soto",
"given": "Solange",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mathers",
"given": "John C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pell",
"given": "Jill",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ho",
"given": "Frederick",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Celis-Morales",
"given": "Carlos",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hebert",
"given": "James",
"sequence": "additional"
}
],
"container-title": "SSRN Electronic Journal",
"container-title-short": "SSRN Journal",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
12,
15
]
],
"date-time": "2022-12-15T03:16:56Z",
"timestamp": 1671074216000
},
"deposited": {
"date-parts": [
[
2022,
12,
15
]
],
"date-time": "2022-12-15T03:18:02Z",
"timestamp": 1671074282000
},
"indexed": {
"date-parts": [
[
2022,
12,
16
]
],
"date-time": "2022-12-16T06:10:53Z",
"timestamp": 1671171053314
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022
]
]
},
"language": "en",
"member": "78",
"original-title": [],
"prefix": "10.2139",
"published": {
"date-parts": [
[
2022
]
]
},
"published-other": {
"date-parts": [
[
2022
]
]
},
"publisher": "Elsevier BV",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.ssrn.com/abstract=4300209"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Earth and Planetary Sciences",
"General Environmental Science"
],
"subtitle": [],
"title": "Associations between the Dietary Inflammatory Index and COVID-19 Outcomes in the UK Biobank Cohort",
"type": "journal-article"
}