SARS-CoV-2 ORF7a activates endothelium to release von Willebrand factor that promotes thrombosis
et al., Research and Practice in Thrombosis and Haemostasis, doi:10.1016/j.rpth.2025.102947, Jun 2025
In vitro and Drosophila study showing that SARS-CoV-2 ORF7a protein activates endothelium to release von Willebrand factor (VWF), promoting thrombosis associated with COVID-19.
Zhang et al., 30 Jun 2025, peer-reviewed, 11 authors.
Contact: zhan@som.umaryland.edu, xzheng2@kumc.edu.
SARS-CoV-2 ORF7a activates endothelium to release von Willebrand factor that promotes thrombosis
Research and Practice in Thrombosis and Haemostasis, doi:10.1016/j.rpth.2025.102947
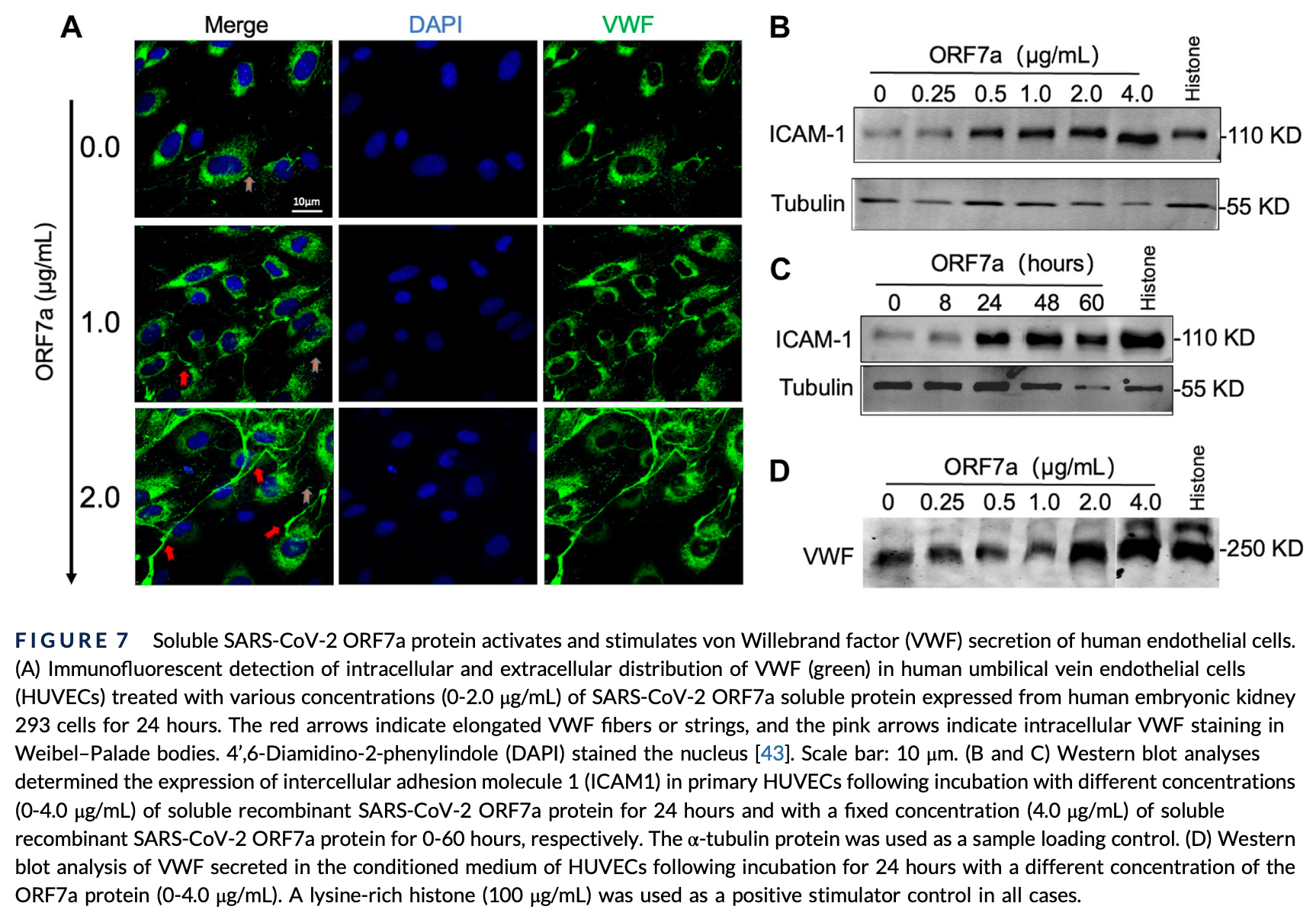
Background: Patients with severe and critical COVID-19 frequently exhibit thromboembolic complications, a significant cause of mortality and morbidity. Increased plasma levels of von Willebrand factor (VWF) following SARS-CoV-2 infection have been extensively reported, which links to thrombosis and increased mortality. However, the mechanism underlying SARS-CoV-2-associated thrombotic complications is not fully understood. Objectives: To determine the mechanism of SARS-CoV-2-associated thrombosis. Methods: Drosophila genetic screening and molecular, cellular, and biochemical approaches were used. Results: Genetic screening identified a SARS-CoV-2 accessory protein, Orf7a, as a crucial factor promoting agglutination of hemolymph, the circulatory fluid of flies, which is functionally comparable to the blood and lymph of vertebrates. Further studies using cultured murine splenic vascular endothelial cells and human umbilical cord endothelial cells demonstrated that overexpression of ORF7a in these cells significantly activated and stimulated the release of VWF, leading to an increased rate and final coverage of Adamts-13 -/-murine platelets on activated endothelial surfaces under arterial shear. Moreover, a soluble recombinant ORF7a could also activate human endothelial cells and trigger the release of VWF from Weibel-Palade bodies.
Conclusion: We demonstrate for the first time that SARS-CoV-2 ORF7a may be one of the pathogenic factors contributing to COVID-19-associated thrombosis by activating the vascular endothelium to release ultralarge VWF, which promotes platelet adhesion and agglutination, and thrombus formation. Thus, a strategy specifically targeting VWFplatelet interaction, such as recombinant a disintegrin and metalloprotease with thrombospondin type 1 repeats, 13 (ADAMTS-13) and/or caplacizumab, may be efficacious in reducing COVID-19-associated thrombosis and mortality.
AUTHOR CONTRIBUTIONS X.H., Q.Z., Z.H., and X.L.Z. conceived and designed the study; X.H., Q.Z., J.-G.L., S. Liu., and F.D. carried out the experiments; X.H., Q.Z., H.L., J.-G.L., S. Liu., S. Limbu, F.D., Z.H., and X.L.Z. analyzed and interpreted the data; X.H., Q.Z., H.L., J.v.d.L., and F.D. prepared the figures; X.H., Q.Z., J.v.d.L., S. Liu., S. Limbu, Z.H., and X.L.Z. drafted the manuscript; S. Limbu and M.K.B. performed the bioinformatic data analysis and drafted the manuscript; X.H., Q.Z., J.v.d.L., Z.H., and X.L.Z. revised and finalized the manuscript. All authors read and approved the final version of this manuscript for publication.
RELATIONSHIP DISCLOSURE X.L.Z. is a consultant for Sanofi and Takeda, as well as a cofounder of Clotsolution. The other authors have nothing to declare.
SUPPLEMENTARY MATERIAL The online version contains supplementary material available at https://doi.org/10.1016/j.rpth.2025.102947 ZHANG ET AL.
References
Bernardo, Ball, Nolasco, Moake, Dong, Effects of inflammatory cytokines on the release and cleavage of the endothelial cell-derived ultralarge von Willebrand factor multimers under flow, Blood
Cao, Niiya, Zheng, Shang, Zheng, Inflammatory cytokines inhibit ADAMTS13 synthesis in hepatic stellate cells and endothelial cells, J Thromb Haemost
Chen, Chen, Lun, Baldoni, Smyth, edgeR v4: powerful differential analysis of sequencing data with expanded functionality and improved support for small counts and larger datasets, Nucleic Acids Res, doi:10.1093/nar/gkaf018
Chung, Zidar, Bristow, Cameron, Chan et al., COVID-19 and cardiovascular disease: from bench to bedside, Circ Res
Delrue, Siguret, Neuwirth, Joly, Beranger, von Willebrand factor/ADAMTS13 axis and venous thromboembolism in moderate-to-severe COVID-19 patients, Br J Haematol
Dlott, Danielson, Blue-Hnidy, Mccarthy, Drug-induced thrombotic thrombocytopenic purpura/hemolytic uremic syndrome: a concise review, Ther Apher Dial
Dobin, Davis, Schlesinger, Drenkow, Zaleski et al., STAR: ultrafast universal RNA-seq aligner, Bioinformatics
Escher, Breakey, Lammle, ADAMTS13 activity, von Willebrand factor, factor VIII and D-dimers in COVID-19 inpatients, Thromb Res
García-García, Ández-Rodríguez, Redondo, De Lucas-Rius, Ópez et al., Impairment of antiviral immune response and disruption of cellular functions by SARS-CoV-2 ORF7a and ORF7b, iScience, doi:10.1016/j.isci.2022.105444
Goto, Kumagai, Kumagai, Hirose, Narita et al., A Drosophila haemocyte-specific protein, hemolectin, similar to human von Willebrand factor, Biochem J
Hafez, Ziade, Arya, Saleh, Ali et al., Reduced ADAMTS13 activity in correlation with pathophysiology, severity, and outcome of COVID-19: a retrospective observational study, Int J Infect Dis
Halkidis, Lammle, Zheng, The history of thrombotic thrombocytopenic purpura research: a narrative review, Ann Blood, doi:10.21037/aob-23-46
Henry, Benoit, De Oliveira, Lippi, Favaloro et al., ADAMTS13 activity to von Willebrand factor antigen ratio predicts acute kidney injury in patients with COVID-19: evidence of SARS-CoV-2 induced secondary thrombotic microangiopathy, Int J Lab Hematol
Hirano, Murakami, COVID-19: a new virus, but a familiar receptor and cytokine release syndrome, Immunity
Hou, Wang, Wang, Wang, Yu et al., The ORF7a protein of SARS-CoV-2 initiates autophagy and limits autophagosome-lysosome fusion via degradation of SNAP29 to promote virus replication, Autophagy
Iqbal, Absar, Akhtar, Aleem, Jameel et al., Integrated genomic analysis identifies ANKRD36 gene as a novel and common biomarker of disease progression in chronic myeloid leukemia, Biology, doi:10.3390/biology10111182
Joly, Darmon, Dekimpe, Dupont, Dumas et al., Imbalance of von Willebrand factor and ADAMTS13 axis is rather a biomarker of strong inflammation and endothelial damage than a cause of thrombotic process in critically ill COVID-19 patients, J Thromb Haemost
Jose, Manuel, COVID-19 cytokine storm: the interplay between inflammation and coagulation, Lancet Respir Med, doi:10.1016/S2213-2600(20)30216-2
Kucerova, Broz, Arefin, Maaroufi, Hurychova et al., The Drosophila chitinase-like protein IDGF3 is involved in protection against nematodes and in wound healing, J Innate Immun
Ladikou, Sivaloganathan, Milne, Arter, Ramasamy et al., Von Willebrand factor (vWF): marker of endothelial damage and thrombotic risk in COVID-19?, Clin Med (Lond), doi:10.7861/clinmed.2020-0346
Lee, Huang, Lee, Van De Leemput, Kane et al., Characterization of SARS-CoV-2 proteins reveals Orf6 pathogenicity, subcellular localization, host interactions and attenuation by Selinexor, Cell Biosci, doi:10.1186/s13578-021-00568-7
Li, Dewey, RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome, BMC Bioinformatics, doi:10.1186/1471-2105-12-323
Li, Li, Liang, Yu, Zhai et al., SARS-CoV-2 ORF7a blocked autophagy flux by intervening in the fusion between autophagosome and lysosome to promote viral infection and pathogenesis, J Med Virol, doi:10.1002/jmv.29200
Malas, Naazie, Elsayed, Mathlouthi, Marmor et al., Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: a systematic review and meta-analysis, EClinicalMedicine, doi:10.1016/j.eclinm.2020.100639
Mancini, Baronciani, Artoni, Colpani, Biganzoli et al., The ADAMTS13-von Willebrand factor axis in COVID-19 patients, J Thromb Haemost
Martinelli, Montagnana, Pizzolo, Friso, Salvagno et al., A relative ADAMTS13 deficiency supports the presence of a secondary microangiopathy in COVID 19, Thromb Res
Mcdaniel, Abdelgawwad, Hargett, Renfrow, Bdeir et al., Human neutrophil peptide-1 inhibits thrombus formation under arterial flow via its terminal free cysteine thiols, J Thromb Haemost
Middeldorp, Coppens, Van Haaps, Foppen, Vlaar et al., Incidence of venous thromboembolism in hospitalized patients with COVID-19, J Thromb Haemost
Milacic, Beavers, Conley, Gong, Gillespie et al., The Reactome Pathway Knowledgebase 2024, Nucleic Acids Res
Moore, June, Cytokine release syndrome in severe COVID-19, Science
Moradian, Gouravani, Salehi, Heidari, Shafeghat et al., Cytokine release syndrome: inhibition of proinflammatory cytokines as a solution for reducing COVID-19 mortality, Eur Cytokine Netw
Nachman, Jaffe, Subcellular platelet factor VIII antigen and von Willebrand factor, J Exp Med
Nelson, Pekosz, Lee, Dimond, Fremont, Structure and intracellular targeting of the SARS-coronoviraus Orf7a accessory protein, Structure
Panigada, Bottino, Tagliabue, Grasselli, Novembrino et al., Hypercoagulability of COVID-19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis, J Thromb Haemost
Peyvandi, Scully, Hovinga, Cataland, Knöbl et al., Caplacizumab for acquired thrombotic thrombocytopenic purpura, N Engl J Med
Philippe, Gendron, Bory, Beauvais, Mirault et al., Von Willebrand factor collagen-binding capacity predicts inhospital mortality in COVID-19 patients: insight from VWF/ ADAMTS13 ratio imbalance, Angiogenesis
Pluta, Cieniewicz, Trzebicki, COVID-19: coagulation disorders and anticoagulant treatment in patients hospitalised in ICU, Anaesthesiol Intensive Ther
Porfidia, Pola, Venous thromboembolism and heparin use in COVID-19 patients: juggling between pragmatic choices, suggestions of medical societies and the lack of guidelines, J Thromb Thrombolysis
Porfidia, Pola, Venous thromboembolism in COVID-19 patients, J Thromb Haemost
Ramacciotti, Agati, Calderaro, Aguiar, Spyropoulos et al., Rivaroxaban versus no anticoagulation for post-discharge thromboprophylaxis after hospitalisation for COVID-19 (MICHELLE): an open-label, multicentre, randomised, controlled trial, Lancet
Rostami, Mansouritorghabeh, Parsa-Kondelaji, High levels of Von Willebrand factor markers in COVID-19: a systematic review and meta-analysis, Clin Exp Med
Sadler, The evolving landscape of von Willebrand disease diagnosis, J Thromb Haemost
Schoettler, Patel, Bryson, Deeb, Watkins et al., Compassionate use narsoplimab for severe refractory transplantation-associated thrombotic microangiopathy in children, Transplant Cell Ther, doi:10.1016/j.jtct.2023.12.017
Scialpi, Scialpi, Piscioli, Scalera, Longo, Pulmonary thromboembolism in criticall ill COVID-19 patients, Int J Infect Dis
Scully, Antun, Cataland, Coppo, Dossier et al., Recombinant ADAMTS13 in congenital thrombotic thrombocytopenic purpura, N Engl J Med
Shi, Zhang, Sang, Qu, Zhong et al., Coagulation dysfunction in ICU patients with coronavirus disease 2019 in Wuhan, China: a retrospective observational study of 75 fatal cases, Aging
Sinkovits, Müller, Iv Ányi Z, G Ál, Gopcsa, Associations between the von Willebrand factor-ADAMTS13 axis, complement activation, and COVID-19 severity and mortality, Thromb Haemost
Sporn, Chavin, Marder, Wagner, Biosynthesis of von Willebrand protein by human megakaryocytes, J Clin Invest
Sweeney, Barouqa, Krause, Gonzalez-Lugo, Rahman et al., Low ADAMTS13 activity correlates with increased mortality in COVID-19 patients, TH Open, doi:10.1055/s-0041-1723784
Wagner, Bonfanti, von Willebrand factor and the endothelium, Mayo Clin Proc
Wagner, The Weibel-Palade body: the storage granule for von Willebrand factor and P-selectin, Thromb Haemost
Wang, Du, Zhu, Cao, An et al., Comorbidities and multi-organ injuries in the treatment of COVID-19, Lancet, doi:10.1016/S0140-6736(20)30558-4
Xiao, Sy, Xue, Sorvillo, Voorberg et al., Essential domains of a disintegrin and metalloprotease with thrombospondin type 1 repeats-13 metalloprotease required for modulation of arterial thrombosis, Arterioscler Thromb Vasc Biol
Yada, Zhang, Bignotti, Ye, Zheng, ADAMTS13 or caplacizumab reduces the accumulation of neutrophil extracellular traps and thrombus in whole blood of COVID-19 patients under flow, Thromb Haemost
Yu, Wang, Han, He, clusterProfiler: an R package for comparing biological themes among gene clusters, OMICS
Zhang, Bignotti, Yada, Ye, Liu et al., Dynamic assessment of plasma von Willebrand factor and ADAMTS13 predicts mortality in hospitalized patients with SARS-CoV-2 infection, J Clin Med, doi:10.3390/jcm12227174
Zhang, Tecson, Mccullough, Endothelial dysfunction contributes to COVID-19-associated vascular inflammation and coagulopathy, Rev Cardiovasc Med
Zhang, Zang, Stevenson, Lei, Copertino et al., Inhibition of major histocompatibility complex-I antigen presentation by sarbecovirus ORF7a proteins, Proc Natl Acad Sci, doi:10.1073/pnas.2209042119
Zheng, ADAMTS13 and von Willebrand factor in thrombotic thrombocytopenic purpura, Annu Rev Med
Zheng, Chung, Takayama, Majerus, Sadler et al., Structure of von Willebrand factor-cleaving protease (ADAMTS13), a metalloprotease involved in thrombotic thrombocytopenic purpura, J Biol Chem
Zhou, Huang, Zhou, Huang, Su et al., Structural insight reveals SARS-CoV-2 ORF7a as an immunomodulating factor for human CD14(+) monocytes, iScience, doi:10.1016/j.isci.2021.102187
Zhu, Lee, Van De Leemput, Lee, Han, Functional analysis of SARS-CoV-2 proteins in Drosophila identifies Orf6-induced pathogenic effects with Selinexor as an effective treatment, Cell Biosci, doi:10.1186/s13578-021-00567-8
Ómez-Seguí, Izquierdo, Castellano, Comos, An update on the pathogenesis and diagnosis of thrombotic thrombocytopenic purpura, Expert Rev Hematol
DOI record:
{
"DOI": "10.1016/j.rpth.2025.102947",
"ISSN": [
"2475-0379"
],
"URL": "http://dx.doi.org/10.1016/j.rpth.2025.102947",
"alternative-id": [
"S2475037925002717"
],
"article-number": "102947",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "SARS-CoV-2 ORF7a activates endothelium to release von Willebrand factor that promotes thrombosis"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Research and Practice in Thrombosis and Haemostasis"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.rpth.2025.102947"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2025 The Authors. Published by Elsevier Inc. on behalf of International Society on Thrombosis and Haemostasis."
}
],
"author": [
{
"affiliation": [],
"family": "Zhang",
"given": "Quan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Huang",
"given": "Xiaohu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Hangnoh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Jin-Gu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Szumam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Limbu",
"given": "Shiwani",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Basu",
"given": "Malay K.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "van de Leemput",
"given": "Joyce",
"sequence": "additional"
},
{
"affiliation": [],
"family": "D’Agnillo",
"given": "Felice",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Han",
"given": "Zhe",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0003-1680-5295",
"affiliation": [],
"authenticated-orcid": false,
"family": "Zheng",
"given": "X. Long",
"sequence": "additional"
}
],
"container-title": "Research and Practice in Thrombosis and Haemostasis",
"container-title-short": "Research and Practice in Thrombosis and Haemostasis",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"rpthjournal.org",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2025,
6,
20
]
],
"date-time": "2025-06-20T23:45:50Z",
"timestamp": 1750463150000
},
"deposited": {
"date-parts": [
[
2025,
6,
24
]
],
"date-time": "2025-06-24T23:31:36Z",
"timestamp": 1750807896000
},
"funder": [
{
"DOI": "10.13039/100000050",
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/100000050",
"id-type": "DOI"
}
],
"name": "National Heart Lung and Blood Institute"
}
],
"indexed": {
"date-parts": [
[
2025,
6,
25
]
],
"date-time": "2025-06-25T00:10:03Z",
"timestamp": 1750810203158,
"version": "3.41.0"
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2025,
6
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
6,
1
]
],
"date-time": "2025-06-01T00:00:00Z",
"timestamp": 1748736000000
}
},
{
"URL": "https://www.elsevier.com/legal/tdmrep-license",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
6,
1
]
],
"date-time": "2025-06-01T00:00:00Z",
"timestamp": 1748736000000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 15,
"start": {
"date-parts": [
[
2025,
6,
16
]
],
"date-time": "2025-06-16T00:00:00Z",
"timestamp": 1750032000000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2475037925002717?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2475037925002717?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "102947",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2025,
6
]
]
},
"published-print": {
"date-parts": [
[
2025,
6
]
]
},
"publisher": "Elsevier BV",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2475037925002717"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "SARS-CoV-2 ORF7a activates endothelium to release von Willebrand factor that promotes thrombosis",
"type": "journal-article",
"update-policy": "https://doi.org/10.1016/elsevier_cm_policy"
}