Metformin Does Not Reduce Hospitalisation for COVID-19
et al., SSRN Electronic Journal, doi:10.2139/ssrn.4225660, Sep 2022
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 12,331 diabetes patients in Hong Kong, showing no significant difference in outcomes with metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
|
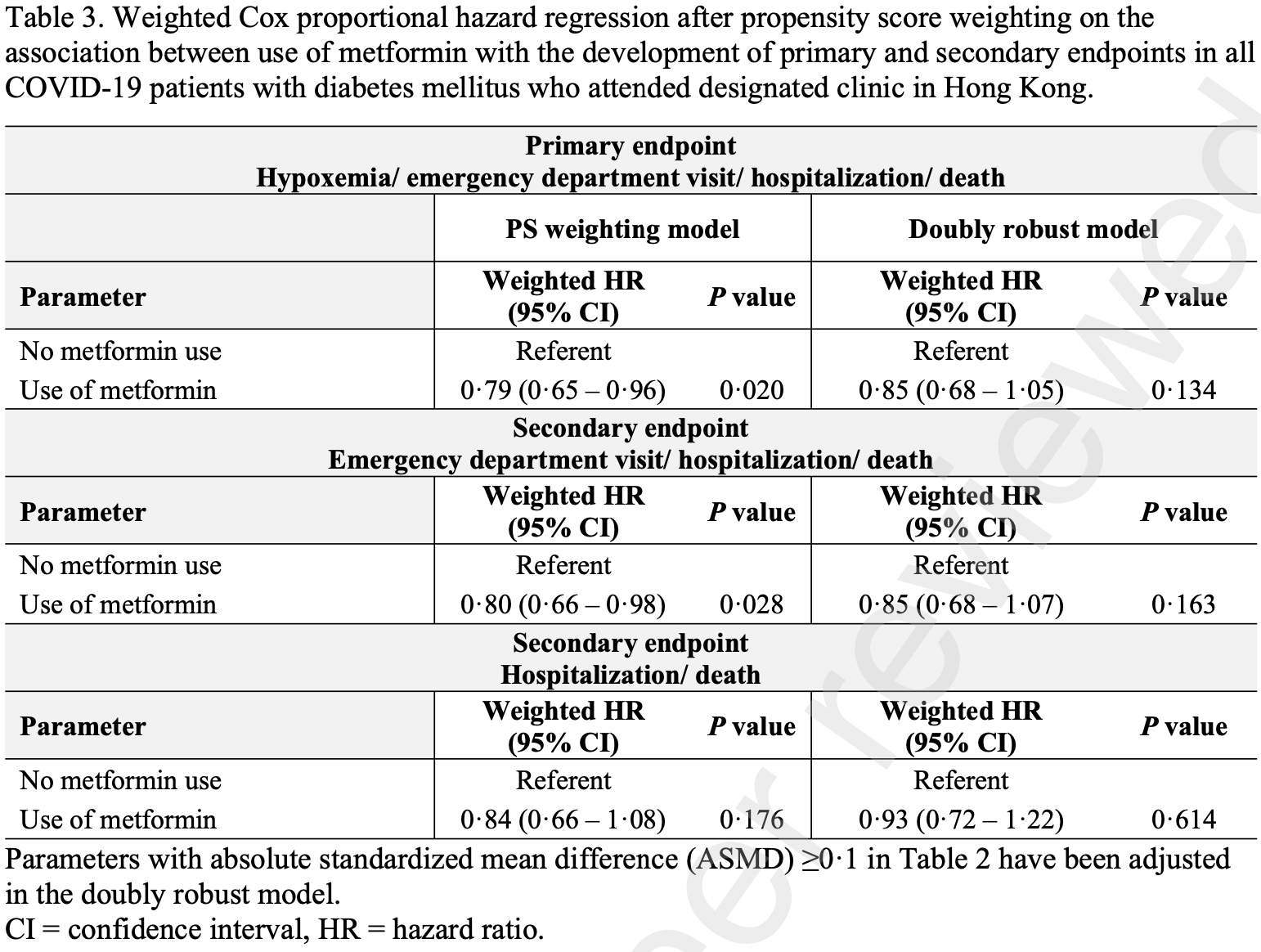
risk of death/hospitalization, 7.0% lower, HR 0.93, p = 0.61, treatment 8,604, control 3,727, propensity score matching, Cox proportional hazards.
|
|
risk of progression, 15.0% lower, HR 0.85, p = 0.16, treatment 8,604, control 3,727, ER/hosp./death, propensity score matching, Cox proportional hazards.
|
|
risk of progression, 15.0% lower, HR 0.85, p = 0.13, treatment 8,604, control 3,727, hypoxemia/ER/hosp./death, propensity score matching, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Yip et al., 21 Sep 2022, retrospective, China, peer-reviewed, mean age 69.0, 10 authors, study period 16 February, 2022 - 31 March, 2022.
Contact: wonglaihung@cuhk.edu.hk.
Metformin Does Not Reduce Hospitalisation for COVID-19
Background A recent randomised trial demonstrated the lack of effect of metformin in preventing severe coronavirus disease 2019 (COVID-19) in non-hospitalised adults.
Methods This was a territory-wide retrospective cohort study in Hong Kong. Non-hospitalised adults with COVID-19 and diabetes who attended designated outpatient clinics during the peak of omicron outbreak were identified. Patients were classified into metformin users and non-users. The primary composite end point was hypoxemia, emergency department visit, hospitalisation, or death. Propensity score weighting analysis was adopted to balance the clinical characteristics of metformin users and non-users. Weighted Cox proportional hazard regression after propensity score weighting was performed.
Findings A total of 12,331 patients with diabetes (8,604 metformin users and 3,727 non-users) were included in the primary analysis. The mean age of the patients was 69 years; 50.6% were female, mean glycated hemoglobin was 7.1%, 43% had been vaccinated, and 28.0% had received molnupiravir or nirmatrelvir/ritonavir. The weighted hazard ratio for the primary end point at Day 30 was 0.85 (95% confidence interval [CI], 0.68 to 1.05; P=0.134) with metformin. In secondary analyses, the weighted hazard ratio for emergency department visit, hospitalisation, or death was 0.85 (95% CI, 0.68 to 1.07; P=0.163) with metformin. The weighted hazards ratio for hospitalisation or death was 0.93 (95% CI, 0.72 to 1.22; P=0.614) with metformin.
Interpretation Use of metformin is not associated with a reduced risk of hypoxemia, emergency department visit, hospitalisation, or death in patients who have diabetes and are not hospitalised for COVID-19 in the real world.
would be adjusted in the doubly robust model. The effective sample size after propensity score weighting was 8,604 and 1,264 in metformin users and nonusers respectively. † The definition of comorbidities was stated in Supplementary Table 2 . ‡ The number of patients with complete vaccination was estimated by the product of the number of patients and the complete vaccination rate in the general population matched with the age, sex, and baseline date. Abbreviations: ASMD = absolute standardized mean difference, DPP-4 inhibitors = dipeptidyl peptidase-4; GLP-1 = glucagon-like peptide-1; SGLT2= Sodium-glucose co-transporter 2; TZD = thiazolidinediones. This preprint research paper has not been peer reviewed. Electronic copy available at: https://ssrn.com/abstract=4225660 P r e p r i n t n o t p e e r r e v i e w e d This preprint research paper has not been peer reviewed. Electronic copy available at: https://ssrn.com/abstract=4225660 P r e p r i n t n o t p e e r r e v i e w e d This preprint research paper has not been peer reviewed. Electronic copy available at: https://ssrn.com/abstract=4225660 P r e p r i n t n o t p e e r r e v i e w e d
References
Bernal, Da Silva, Musungaie, Molnupiravir for Oral Treatment of COVID-19 in Nonhospitalised Patients, N Engl J Med
Bramante, Huling, Tignanelli, Randomised Trial of Metformin, Ivermectin, and Fluvoxamine for COVID-19, N Engl J Med
Cameron, Morrison, Levin, Anti-Inflammatory Effects of Metformin Irrespective of Diabetes Status, Circ Res
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia
Chen, Lv, Lin, Arshad, Dai, The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis, Front Endocrinol
Cheng, Tong, Kwok, Development Journey of Clinical Data Analysis and Reporting System (CDARS) in Hospital Authority of
Crouse, Grimes, Li, Might, Ovalle et al., Metformin Use Is Associated With Reduced Mortality in a Diverse Population With COVID-19 and Diabetes, Front Endocrinol
Ghany, Palacio, Dawkins, Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA, Diabetes Metab Syndr
Gordon, Jang, Bouhaddou, A SARS-CoV-2 protein interaction map reveals targets for drug repurposing, Nature
Hammond, Leister-Tebbe, Gardner, Oral Nirmatrelvir for High-Risk, Nonhospitalised Adults with COVID-19, N Engl J Med
Karam, Morris, Bramante, mTOR inhibition in COVID-19: A commentary and review of efficacy in RNA viruses, J Med Virol
Karim, Devnarain, Time to Stop Using Ineffective COVID-19 Drugs, N Engl J Med
Keehner, Horton, Binkin, Resurgence of SARS-CoV-2 Infection in a Highly Vaccinated Health System Workforce, N Engl J Med
Lui, Yip, Wong, Significantly Lower Case-fatality Ratio of Coronavirus Disease 2019 (COVID-19) than Severe Acute Respiratory Syndrome (SARS) in Hong Kong-A Territory-Wide Cohort Study, Clin Infect Dis
Luk, Yip, Zhang, Glucose-lowering drugs and outcome from COVID-19 among patients with type 2 diabetes mellitus: a population-wide analysis in Hong Kong, BMJ Open
Mauvais-Jarvis, Aging, Male Sex, Obesity, and Metabolic Inflammation Create the Perfect Storm for COVID-19, Diabetes
Postler, Peng, Bhatt, Ghosh, Metformin selectively dampens the acute inflammatory response through an AMPK-dependent mechanism, Sci Rep
Ps, or death) E. before PS weighting, and F. after PS weighting
Teoh, Yip, Lui, Risks of AKI and Major Adverse Clinical Outcomes in Patients with Severe Acute Respiratory Syndrome or Coronavirus Disease 2019, J Am Soc Nephrol
Timmins, Donahue, Meeker, Marathe, Steady-state pharmacokinetics of a novel extended-release metformin formulation, Clin Pharmacokinet
Wong, Yip, Wong, SARS-CoV-2 Viral Persistence Based on Cycle Threshold Value and Liver Injury in Patients With COVID-19, Open Forum Infect Dis
Xin, Wei, Ji, Metformin Uniquely Prevents Thrombosis by Inhibiting Platelet Activation and mtDNA Release, Sci Rep
Yip, Lui, Lai, Impact of the use of oral antiviral agents on the risk of hospitalization in community COVID-19 patients, Clin Infect Dis
Yip, Wong, Lui, Current and Past Infections of HBV Do Not Increase Mortality in Patients With COVID-19, Hepatology
Zhang, Dong, Martin, AMP-activated Protein Kinase Phosphorylation of Angiotensin-Converting Enzyme 2 in Endothelium Mitigates Pulmonary Hypertension, Am J Respir Crit Care Med
Zhang, He, Impacts of metformin on tuberculosis incidence and clinical outcomes in patients with diabetes: a systematic review and meta-analysis, Eur J Clin Pharmacol
DOI record:
{
"DOI": "10.2139/ssrn.4225660",
"ISSN": [
"1556-5068"
],
"URL": "http://dx.doi.org/10.2139/ssrn.4225660",
"author": [
{
"affiliation": [],
"family": "Yip",
"given": "Cheuk Fung",
"sequence": "first"
},
{
"affiliation": [],
"family": "Luk",
"given": "Andrea O. Y.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lui",
"given": "Grace C.Y.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Man Lai",
"given": "Mandy Sze",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wong",
"given": "Vincent Wai-Sun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tse",
"given": "Yee-Kit",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chan",
"given": "Henry Lik-Yuen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hui",
"given": "David S. C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kong",
"given": "Alice P. S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hui",
"given": "David Shu-Cheong",
"sequence": "additional"
}
],
"container-title": "SSRN Electronic Journal",
"container-title-short": "SSRN Journal",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
9,
27
]
],
"date-time": "2022-09-27T22:28:48Z",
"timestamp": 1664317728000
},
"deposited": {
"date-parts": [
[
2022,
9,
27
]
],
"date-time": "2022-09-27T22:29:11Z",
"timestamp": 1664317751000
},
"indexed": {
"date-parts": [
[
2022,
9,
28
]
],
"date-time": "2022-09-28T05:37:40Z",
"timestamp": 1664343460404
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022
]
]
},
"language": "en",
"member": "78",
"original-title": [],
"prefix": "10.2139",
"published": {
"date-parts": [
[
2022
]
]
},
"published-other": {
"date-parts": [
[
2022
]
]
},
"publisher": "Elsevier BV",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.ssrn.com/abstract=4225660"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Earth and Planetary Sciences",
"General Environmental Science"
],
"subtitle": [],
"title": "Metformin Does Not Reduce Hospitalisation for COVID-19",
"type": "journal-article"
}
