Oropharyngeal Probiotic ENT-K12 Prevents Respiratory Tract Infections Among Frontline Medical Staff Fighting Against COVID-19: A Pilot Study
et al., Front. Bioeng. Biotechnol., doi:10.3389/fbioe.2021.646184, Jun 2021
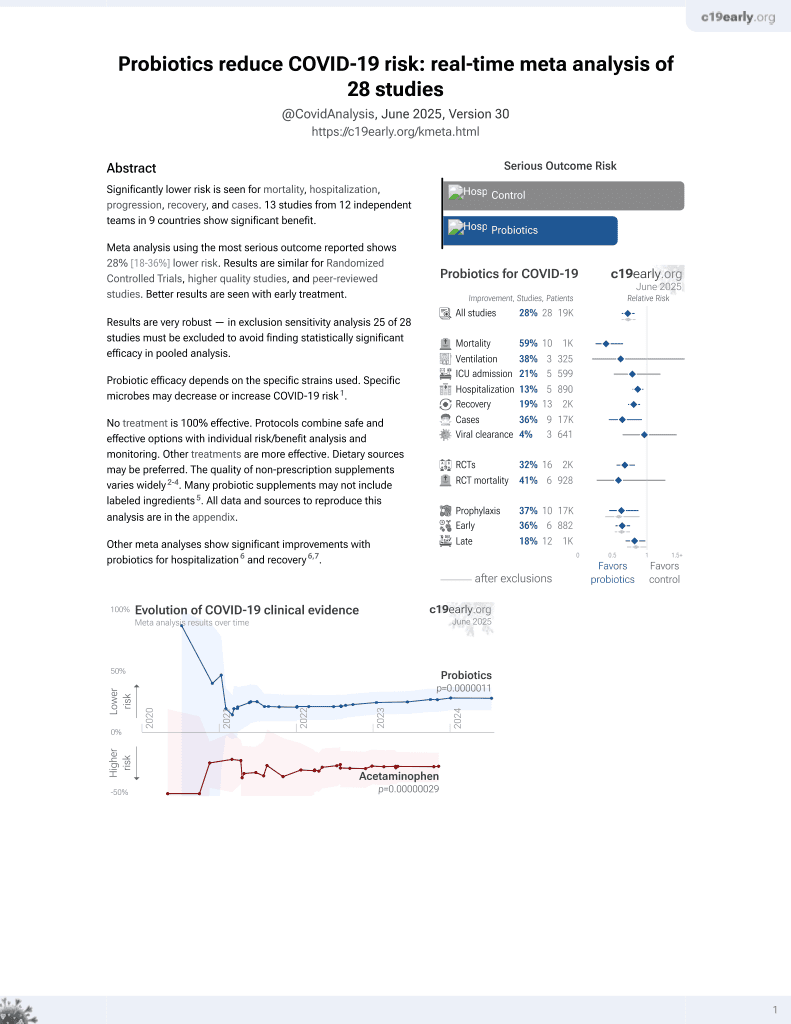
Probiotics for COVID-19
20th treatment shown to reduce risk in
March 2021, now with p = 0.00000044 from 29 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prophylaxis RCT in China with 98 healthcare workers in close contact with COVID-19 patients treated with Bactoblis oropharyngeal probiotic containing S. thermophilus ENT-K12, and 95 control patients, showing lower incidence of respiratory infections with treatment (none were confirmed COVID-19, details of testing are not provided).
Probiotic efficacy depends on the specific strains used. Specific microbes may decrease or increase COVID-19 risk1.
Wang et al., 24 Jun 2021, peer-reviewed, 13 authors.
Oropharyngeal Probiotic ENT-K12 Prevents Respiratory Tract Infections Among Frontline Medical Staff Fighting Against COVID-19: A Pilot Study
Frontiers in Bioengineering and Biotechnology, doi:10.3389/fbioe.2021.646184
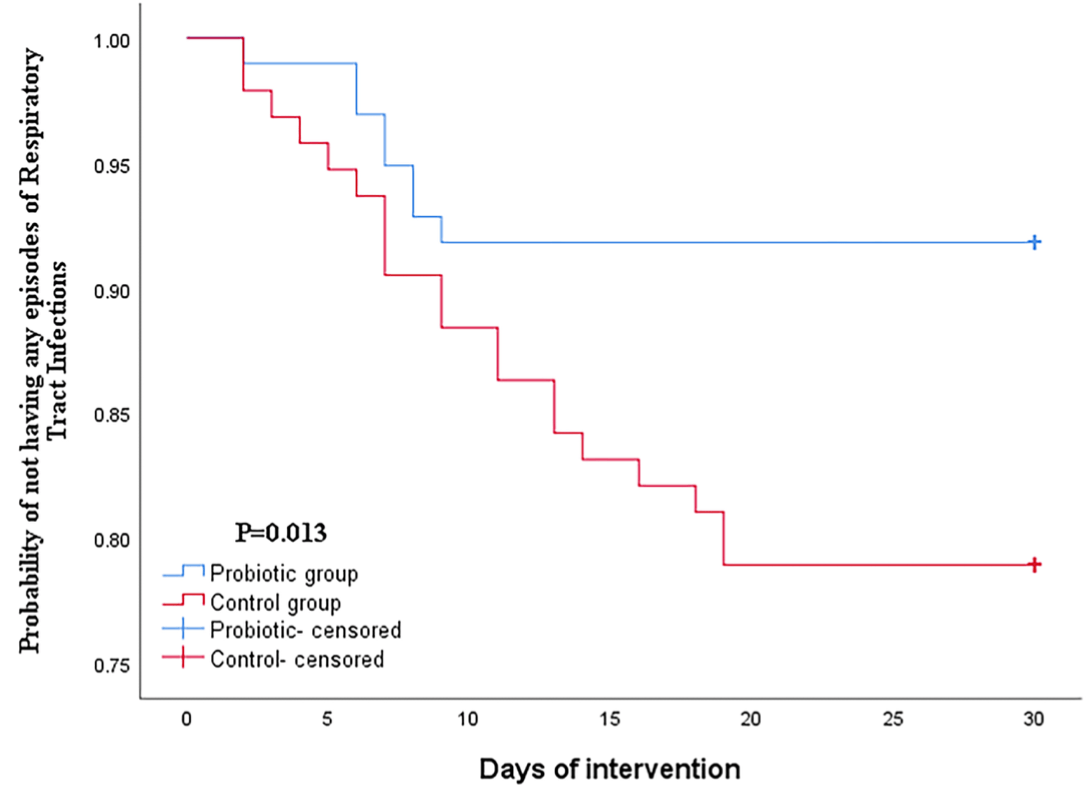
Healthcare workers at the frontline are facing a substantial risk of respiratory tract infection during the COVID-19 outbreak due to an extremely stressful work schedule and public health event. A well-established first-line defense on oropharyngeal microbiome could be a promising strategy to protect individuals from respiratory tract infections including COVID-19. The most thoroughly studied oropharyngeal probiotic product which creates a stable upper respiratory tract microbiota capable of preventing upper respiratory tract infections was chosen to evaluate the safety and efficacy on reducing episodes of upper respiratory tract infections for COVID-19 healthcare workers. To our knowledge to date, this is the very first study describing the beneficial effects of oropharyngeal probiotic been administered by healthcare workers during the COVID-19 pandemic. In this randomized controlled trial, we provided the probiotics to frontline medical staff who work in the hospitals in Wuhan and had been in close contact with hospitalized COVID-19 patients for prophylactic use on a daily basis. Our finding suggests that oropharyngeal probiotic administration significantly reduced the incidence of respiratory tract infections by 64.8%, reduced the time experiencing respiratory tract infections and oral ulcer symptoms by 78%, shortened the days absent from work by 95.5%, and reduced the time under medication where there is no record of antibiotic and anti-viral drug intake in the probiotic group. Furthermore, medical staff treated with Bactoblis experienced sustained protection from respiratory tract infections since the 10th day of oropharyngeal probiotic administration resulting in an extremely low incidence rate of respiratory tract infections.
Conflict of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Copyright © 2021 Wang, Lin, Xiang, Liu, Fang, Chen, Tang, Guo, Chen, Hu, Wu, Zhu and Xia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
References
Barbour, Tagg, Abou-Zied, New insights into the mode of action of the lantibiotic salivaricin, B. Sci. Rep, doi:10.1038/srep31749
Barbour, Wescombe, Smith, Evolution of lantibiotic salivaricins: new weapons to fight infectious diseases, Trends Microbiol, doi:10.1016/j.tim.2020.03.001
Beata, Antibiotic resistance of Streptococcus pneumoniae in children with acute otitis media treatment failure, Int. J. Pediatric Otorhinolaryngol, doi:10.1016/j.ijporl.2015.09.030
Burton, Chilcott, Wescombe, Tagg, Extended safety data for the oral cavity probiotic Streptococcus salivarius K12, Probiotics Antimicro. Prot, doi:10.1007/s12602-010-9045-4
Clark, Nabeetha, Ali, Gregory, James et al., Nasopharyngeal microbiota composition of children is related to the frequency of upper respiratory infection and acute sinusitis, Microbiome, doi:10.1186/s40168-016-0179-9
Cotter, Ross, Hill, Bacteriocins -a viable alternative to antibiotics?, Nat. Rev. Microbiol, doi:10.1038/nrmicro2937
De Francesco, Giorgio, Hassan, Manes, Vannella et al., Worldwide H. pylori antibiotic resistance: a systematic review, J. Gastrointestin Liver Dis
Di Pierro, A possible probiotic (S. salivarius K12) approach to improve oral and lung microbiotas and raise defenses against SAR S-CoV-2, Minerva Med, doi:10.23736/S0026-4806.20.06570-2
Harald, Per, Mathias, The impact of perinatal immune development on mucosal homeostasis and chronic inflammation, Nat. Rev. Immunol, doi:10.1038/nri3112
Hongcheng, Shuaiyin, Alternation of nasopharyngeal microbiota in healthy youth is associated with environmental factors: implication for respiratory diseases, Int. J. Environ. Health Res, doi:10.1080/09603123.2020.1810209
Horz, Meinelt, Houben, Conrads, Ilchenko et al., The effectiveness application of the respiratory probiotic Streptococcus salivarius K12 for the correction of dysbiotic oral cavity disorders in children with juvenile rheumatoid arthritis, Oral. Microbiol. Immunol, doi:10.1111/j.1399-302X.2007.00334.x
Ilchenko, Fialkovska, Ivanus, The effectiveness of using respiratory probiotic Streptococcus salivarius K12 in children with recurrent tonsillitis, Actual Infectol, doi:10.22141/2312-413x.8.2.2020.199732
Ilchenko, Fialkovska, Mozheiko, Modern possibilities of correcting dysbiotic disorders of the mucous membranes of the upper respiratory tract in infants, Clin. Pediatr
Jakobsson, Jernberg, Andersson, Short-term antibiotic treatment has differing long-term impacts on the human throat and gut microbiome, PLoS One, doi:10.1371/journal.pone.0009836
Jincun, Jingxian, Ashutosh, Rudragouda, Craig et al., Airway memory CD4+ T cells mediate protective immunity against emerging respiratory coronaviruses, Immunity, doi:10.1016/j.immuni.2016.05.006
Khan, Petersen, Shekhar, Commensal bacteria: an emerging player in defense against respiratory pathogens, Front. Immunol, doi:10.3389/fimmu.2019.01203
Kramarev, Yevtushenko, Seryakova, Kaminskaya, Application of Streptococcus salivarius K12 probiotic strain in the treatment of acute tonsillopharyngitis in children, Actual Infectol, doi:10.22141/2312-413x.8.3-4.2020.212657
Lichun, Xiang, Chongchong, Qin, Shuang et al., Analysis of the infection status of the medical staff in Wuhan during the COVID-19 outbreak: a cross-sectional study, Clin. Infect. Dis, doi:10.1093/cid/ciaa588
Lirong, Cheng, Jiajia, Lei, Yan et al., Oral Microbiome and SARS-CoV-2: beware of lung co-infection, Front. Microbiol, doi:10.3389/fmicb.2020.01840
Martens, Pugin, De Boeck, Spacova, Steelant et al., Probiotics for the airways: potential to improve epithelial and immune homeostasis, Allergy, doi:10.1111/all.13495
Mikari, Toru, Tongue microbiota and oral health status in community-dwelling elderly adults, Clin. Sci. Epidemiol, doi:10.1128/mSphere.00332-18
Olga, Viktoria, Bernard, Anne, Kristina et al., Nasopharyngeal microbiota in healthy children and Pneumonia patients, J. Clin. Microbiol, doi:10.1128/JCM.03280-13
Pascal, Laura, Philippe, Mignolet, Mobilization of Microbiota commensals and their bacteriocins for therapeutics, Trends Microbiol, doi:10.1016/j.tim.2019.03.007
Piewngam, Zheng, Nguyen, Dickey, Joo et al., Does probiotic consumption reduce antibiotic utilization for common acute infections? A systematic review and meta-analysis, Eur. J. Public Health, doi:10.1093/eurpub/cky185
Trueba, Ritz, Stress, asthma, and respiratory infections: pathways involving airway immunology and microbial endocrinology, Brain Behav. Immun, doi:10.1016/j.bbi.2012.09.012
Upton, Tagg, Wescombe, Jenkinson, Intra-and Interspecies signaling between streptococcus salivarius and streptococcus pyogenes mediated by SalA and SalA1 lantibiotic peptides, J. Bacteriol, doi:10.1128/jb.183.13.3931-3938.2001
Wilcox, Stuart, Leaver, Lown, Willcox et al., Effectiveness of the probiotic Streptococcus salivarius K12 for the treatment and/or prevention of sore throat: a systematic review, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2018.12.031
Wing, Melanie, Wouter, Loss of microbial topography between oral and nasopharyngeal microbiota and development of respiratory infections early in life, Eur. Respiratory J, doi:10.1183/13993003
Yaowen, Jing, Dong, Zhirong, Yanyan et al., Annual surveys for point-prevalence of healthcare-associated infection in a tertiary hospital in Beijing, China, 2012-2014, BMC Infect. Dis, doi:10.1186/s12879-016-1504-4
Zijie, Yan, Lu, Wentai, Leisheng et al., Genomic diversity of SARS-CoV-2 in Coronavirus Disease 2019 patients, Clin. Infect. Dis, doi:10.1093/cid/ciaa203
DOI record:
{
"DOI": "10.3389/fbioe.2021.646184",
"ISSN": [
"2296-4185"
],
"URL": "http://dx.doi.org/10.3389/fbioe.2021.646184",
"abstract": "<jats:p>Healthcare workers at the frontline are facing a substantial risk of respiratory tract infection during the COVID-19 outbreak due to an extremely stressful work schedule and public health event. A well-established first-line defense on oropharyngeal microbiome could be a promising strategy to protect individuals from respiratory tract infections including COVID-19. The most thoroughly studied oropharyngeal probiotic product which creates a stable upper respiratory tract microbiota capable of preventing upper respiratory tract infections was chosen to evaluate the safety and efficacy on reducing episodes of upper respiratory tract infections for COVID-19 healthcare workers. To our knowledge to date, this is the very first study describing the beneficial effects of oropharyngeal probiotic been administered by healthcare workers during the COVID-19 pandemic. In this randomized controlled trial, we provided the probiotics to frontline medical staff who work in the hospitals in Wuhan and had been in close contact with hospitalized COVID-19 patients for prophylactic use on a daily basis. Our finding suggests that oropharyngeal probiotic administration significantly reduced the incidence of respiratory tract infections by 64.8%, reduced the time experiencing respiratory tract infections and oral ulcer symptoms by 78%, shortened the days absent from work by 95.5%, and reduced the time under medication where there is no record of antibiotic and anti-viral drug intake in the probiotic group. Furthermore, medical staff treated with Bactoblis experienced sustained protection from respiratory tract infections since the 10th day of oropharyngeal probiotic administration resulting in an extremely low incidence rate of respiratory tract infections.</jats:p>",
"alternative-id": [
"10.3389/fbioe.2021.646184"
],
"author": [
{
"affiliation": [],
"family": "Wang",
"given": "Qiang",
"sequence": "first"
},
{
"affiliation": [],
"family": "Lin",
"given": "Xuan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xiang",
"given": "Xiaochen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Wanxin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fang",
"given": "Ying",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Haiping",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tang",
"given": "Fang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guo",
"given": "Hongyan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Di",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hu",
"given": "Xiafen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wu",
"given": "Qingming",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhu",
"given": "Baoli",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xia",
"given": "Junbo",
"sequence": "additional"
}
],
"container-title": "Frontiers in Bioengineering and Biotechnology",
"container-title-short": "Front. Bioeng. Biotechnol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2021,
6,
24
]
],
"date-time": "2021-06-24T07:06:36Z",
"timestamp": 1624518396000
},
"deposited": {
"date-parts": [
[
2021,
6,
24
]
],
"date-time": "2021-06-24T07:06:39Z",
"timestamp": 1624518399000
},
"indexed": {
"date-parts": [
[
2024,
4,
1
]
],
"date-time": "2024-04-01T15:18:56Z",
"timestamp": 1711984736347
},
"is-referenced-by-count": 14,
"issued": {
"date-parts": [
[
2021,
6,
24
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
24
]
],
"date-time": "2021-06-24T00:00:00Z",
"timestamp": 1624492800000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fbioe.2021.646184/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2021,
6,
24
]
]
},
"published-online": {
"date-parts": [
[
2021,
6,
24
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1038/srep31749",
"article-title": "New insights into the mode of action of the lantibiotic salivaricin B.",
"author": "Barbour",
"doi-asserted-by": "publisher",
"first-page": "31749",
"journal-title": "Sci. Rep.",
"key": "B1",
"volume": "6",
"year": "2016"
},
{
"DOI": "10.1016/j.tim.2020.03.001",
"article-title": "Evolution of lantibiotic salivaricins: new weapons to fight infectious diseases.",
"author": "Barbour",
"doi-asserted-by": "publisher",
"first-page": "578",
"journal-title": "Trends Microbiol.",
"key": "B2",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1016/j.ijporl.2015.09.030",
"article-title": "Antibiotic resistance of Streptococcus pneumoniae in children with acute otitis media treatment failure.",
"author": "Beata",
"doi-asserted-by": "publisher",
"first-page": "2129",
"journal-title": "Int. J. Pediatric Otorhinolaryngol.",
"key": "B3",
"volume": "79",
"year": "2015"
},
{
"DOI": "10.1007/s12602-010-9045-4",
"article-title": "Extended safety data for the oral cavity probiotic Streptococcus salivarius K12.",
"author": "Burton",
"doi-asserted-by": "publisher",
"first-page": "135",
"journal-title": "Probiotics Antimicro. Prot.",
"key": "B4",
"volume": "2",
"year": "2010"
},
{
"DOI": "10.1186/s40168-016-0179-9",
"article-title": "Nasopharyngeal microbiota composition of children is related to the frequency of upper respiratory infection and acute sinusitis.",
"author": "Clark",
"doi-asserted-by": "publisher",
"first-page": "34",
"journal-title": "Microbiome",
"key": "B5",
"volume": "4",
"year": "2016"
},
{
"DOI": "10.1038/nrmicro2937",
"article-title": "Bacteriocins — a viable alternative to antibiotics?",
"author": "Cotter",
"doi-asserted-by": "publisher",
"first-page": "95",
"journal-title": "Nat. Rev. Microbiol.",
"key": "B6",
"volume": "11",
"year": "2013"
},
{
"article-title": "Worldwide H. pylori antibiotic resistance: a systematic review.",
"author": "De Francesco",
"first-page": "409",
"journal-title": "J. Gastrointestin Liver Dis.",
"key": "B7",
"volume": "19",
"year": "2010"
},
{
"DOI": "10.23736/S0026-4806.20.06570-2",
"article-title": "A possible probiotic (S. salivarius K12) approach to improve oral and lung microbiotas and raise defenses against SAR S-CoV-2.",
"author": "Di Pierro",
"doi-asserted-by": "publisher",
"first-page": "281",
"journal-title": "Minerva Med.",
"key": "B8",
"volume": "111",
"year": "2020"
},
{
"DOI": "10.1038/nri3112",
"article-title": "The impact of perinatal immune development on mucosal homeostasis and chronic inflammation.",
"author": "Harald",
"doi-asserted-by": "publisher",
"first-page": "9",
"journal-title": "Nat. Rev. Immunol.",
"key": "B9",
"volume": "12",
"year": "2012"
},
{
"DOI": "10.1080/09603123.2020.1810209",
"article-title": "Alternation of nasopharyngeal microbiota in healthy youth is associated with environmental factors: implication for respiratory diseases.",
"author": "Hongcheng",
"doi-asserted-by": "publisher",
"first-page": "11",
"journal-title": "Int. J. Environ. Health Res.",
"key": "B10",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1111/j.1399-302X.2007.00334.x",
"article-title": "Distribution and persistence of probiotic Streptococcus salivarius K12 in the human oral cavity as determined by real-time quantitative polymerase chain reaction.",
"author": "Horz",
"doi-asserted-by": "publisher",
"first-page": "126",
"journal-title": "Oral. Microbiol. Immunol.",
"key": "B11",
"volume": "22",
"year": "2007"
},
{
"article-title": "The effectiveness application of the respiratory probiotic Streptococcus salivarius K12 for the correction of dysbiotic oral cavity disorders in children with juvenile rheumatoid arthritis.",
"author": "Ilchenko",
"first-page": "116",
"journal-title": "Clin. Pediatr.",
"key": "B12",
"volume": "3",
"year": ""
},
{
"DOI": "10.22141/2312-413x.8.2.2020.199732",
"article-title": "The effectiveness of using respiratory probiotic Streptococcus salivarius K12 in children with recurrent tonsillitis.",
"author": "Ilchenko",
"doi-asserted-by": "publisher",
"first-page": "25",
"journal-title": "Actual Infectol.",
"key": "B13",
"volume": "8",
"year": "2020"
},
{
"article-title": "Modern possibilities of correcting dysbiotic disorders of the mucous membranes of the upper respiratory tract in infants.",
"author": "Ilchenko",
"first-page": "7",
"journal-title": "Clin. Pediatr.",
"key": "B14",
"volume": "14",
"year": ""
},
{
"DOI": "10.1371/journal.pone.0009836",
"article-title": "Short-term antibiotic treatment has differing long-term impacts on the human throat and gut microbiome.",
"author": "Jakobsson",
"doi-asserted-by": "publisher",
"first-page": "e9836",
"journal-title": "PLoS One",
"key": "B15",
"volume": "24",
"year": "2010"
},
{
"DOI": "10.1016/j.immuni.2016.05.006",
"article-title": "Airway memory CD4+ T cells mediate protective immunity against emerging respiratory coronaviruses.",
"author": "Jincun",
"doi-asserted-by": "publisher",
"first-page": "1379",
"journal-title": "Immunity",
"key": "B16",
"volume": "44",
"year": "2016"
},
{
"DOI": "10.3389/fimmu.2019.01203",
"article-title": "Commensal bacteria: an emerging player in defense against respiratory pathogens.",
"author": "Khan",
"doi-asserted-by": "publisher",
"first-page": "1203",
"journal-title": "Front. Immunol.",
"key": "B17",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.22141/2312-413x.8.3-4.2020.212657",
"article-title": "Application of Streptococcus salivarius K12 probiotic strain in the treatment of acute tonsillopharyngitis in children.",
"author": "Kramarev",
"doi-asserted-by": "publisher",
"first-page": "29",
"journal-title": "Actual Infectol.",
"key": "B18",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa588",
"article-title": "Analysis of the infection status of the medical staff in Wuhan during the COVID-19 outbreak: a cross-sectional study.",
"author": "Lichun",
"doi-asserted-by": "publisher",
"first-page": "2109",
"journal-title": "Clin. Infect. Dis.",
"key": "B19",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.3389/fmicb.2020.01840",
"article-title": "Oral Microbiome and SARS-CoV-2: beware of lung co-infection.",
"author": "Lirong",
"doi-asserted-by": "publisher",
"first-page": "1840",
"journal-title": "Front. Microbiol.",
"key": "B20",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1111/all.13495",
"article-title": "Probiotics for the airways: potential to improve epithelial and immune homeostasis.",
"author": "Martens",
"doi-asserted-by": "publisher",
"first-page": "1954",
"journal-title": "Allergy",
"key": "B21",
"volume": "73",
"year": "2018"
},
{
"DOI": "10.1128/mSphere.00332-18",
"article-title": "Tongue microbiota and oral health status in community-dwelling elderly adults.",
"author": "Mikari",
"doi-asserted-by": "publisher",
"first-page": "e00332",
"journal-title": "Clin. Sci. Epidemiol.",
"key": "B22",
"volume": "3",
"year": "2018"
},
{
"DOI": "10.1128/JCM.03280-13",
"article-title": "Nasopharyngeal microbiota in healthy children and Pneumonia patients.",
"author": "Olga",
"doi-asserted-by": "publisher",
"first-page": "1590",
"journal-title": "J. Clin. Microbiol.",
"key": "B23",
"volume": "52",
"year": "2014"
},
{
"DOI": "10.1016/j.tim.2019.03.007",
"article-title": "Mobilization of Microbiota commensals and their bacteriocins for therapeutics.",
"author": "Pascal",
"doi-asserted-by": "publisher",
"first-page": "690",
"journal-title": "Trends Microbiol.",
"key": "B24",
"volume": "27",
"year": "2019"
},
{
"DOI": "10.1038/s41586-018-0616-y",
"article-title": "Pathogen elimination by probiotic Bacillus via signalling interference.",
"author": "Piewngam",
"doi-asserted-by": "publisher",
"first-page": "532",
"journal-title": "Nature",
"key": "B25",
"volume": "562",
"year": "2018"
},
{
"DOI": "10.1093/eurpub/cky185",
"article-title": "Does probiotic consumption reduce antibiotic utilization for common acute infections? A systematic review and meta-analysis.",
"author": "Sarah",
"doi-asserted-by": "publisher",
"first-page": "494",
"journal-title": "Eur. J. Public Health",
"key": "B26",
"volume": "29",
"year": "2019"
},
{
"DOI": "10.1016/j.bbi.2012.09.012",
"article-title": "Stress, asthma, and respiratory infections: pathways involving airway immunology and microbial endocrinology.",
"author": "Trueba",
"doi-asserted-by": "publisher",
"first-page": "11",
"journal-title": "Brain Behav. Immun.",
"key": "B27",
"volume": "29",
"year": "2012"
},
{
"DOI": "10.1128/jb.183.13.3931-3938.2001",
"article-title": "Intra- and Interspecies signaling between streptococcus salivarius and streptococcus pyogenes mediated by SalA and SalA1 lantibiotic peptides.",
"author": "Upton",
"doi-asserted-by": "publisher",
"first-page": "3931",
"journal-title": "J. Bacteriol.",
"key": "B28",
"volume": "183",
"year": "2001"
},
{
"DOI": "10.1016/j.cmi.2018.12.031",
"article-title": "Effectiveness of the probiotic Streptococcus salivarius K12 for the treatment and/or prevention of sore throat: a systematic review.",
"author": "Wilcox",
"doi-asserted-by": "publisher",
"first-page": "673",
"journal-title": "Clin. Microbiol. Infect.",
"key": "B29",
"volume": "25",
"year": "2019"
},
{
"DOI": "10.1183/13993003",
"article-title": "Loss of microbial topography between oral and nasopharyngeal microbiota and development of respiratory infections early in life.",
"author": "Wing",
"doi-asserted-by": "publisher",
"first-page": "A4995",
"journal-title": "Eur. Respiratory J.",
"key": "B30",
"year": "2019"
},
{
"DOI": "10.1186/s12879-016-1504-4",
"article-title": "Annual surveys for point-prevalence of healthcare-associated infection in a tertiary hospital in Beijing, China, 2012-2014.",
"author": "Yaowen",
"doi-asserted-by": "publisher",
"first-page": "161",
"journal-title": "BMC Infect. Dis.",
"key": "B31",
"volume": "16",
"year": "2016"
},
{
"DOI": "10.1093/cid/ciaa203",
"article-title": "Genomic diversity of SARS-CoV-2 in Coronavirus Disease 2019 patients.",
"author": "Zijie",
"doi-asserted-by": "publisher",
"first-page": "ciaa203",
"journal-title": "Clin. Infect. Dis.",
"key": "B32",
"volume": "9",
"year": "2020"
}
],
"reference-count": 32,
"references-count": 32,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fbioe.2021.646184/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Oropharyngeal Probiotic ENT-K12 Prevents Respiratory Tract Infections Among Frontline Medical Staff Fighting Against COVID-19: A Pilot Study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "9"
}