Metformin use in patients hospitalized with COVID-19: lower inflammation, oxidative stress, and thrombotic risk markers and better clinical outcomes
et al., Journal of Thrombosis and Thrombolysis, doi:10.1007/s11239-022-02631-7, Jan 2022
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 75 diabetes patients, 34 on metformin, showing improved clinical outcomes with treatment, without statistical significance.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
This may explain in part the very high mortality seen in this study.
Results may differ in countries with improved SOC.
|
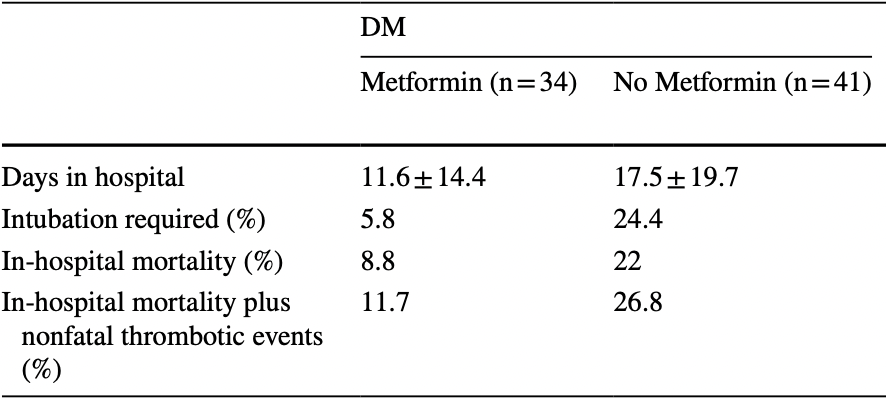
risk of death, 59.8% lower, RR 0.40, p = 0.21, treatment 3 of 34 (8.8%), control 9 of 41 (22.0%), NNT 7.6.
|
|
risk of mechanical ventilation, 75.9% lower, RR 0.24, p = 0.05, treatment 2 of 34 (5.9%), control 10 of 41 (24.4%), NNT 5.4.
|
|
hospitalization time, 33.7% lower, relative time 0.66, p = 0.13, treatment 34, control 41.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Usman et al., 18 Jan 2022, retrospective, USA, peer-reviewed, 10 authors.
Metformin use in patients hospitalized with COVID-19: lower inflammation, oxidative stress, and thrombotic risk markers and better clinical outcomes
Journal of Thrombosis and Thrombolysis, doi:10.1007/s11239-022-02631-7
Diabetes mellitus (DM) is associated with a greater risk of COVID-19 and an increased mortality when the disease is contracted. Metformin use in patients with DM is associated with less COVID-19-related mortality, but the underlying mechanism behind this association remains unclear. Our aim was to explore the effects of metformin on markers of inflammation, oxidative stress, and hypercoagulability, and on clinical outcomes. Patients with DM on metformin (n = 34) and metformin naïve (n = 41), and patients without DM (n = 73) were enrolled within 48 h of hospital admission for COVID-19. Patients on metformin compared to naïve patients had a lower white blood cell count (p = 0.02), d-dimer (p = 0.04), urinary 11-dehydro thromboxane B 2 (p = 0.01) and urinary liver-type fatty acid binding protein (p = 0.03) levels and had lower sequential organ failure assessment score (p = 0.002), and intubation rate (p = 0.03), fewer hospitalized days (p = 0.13), lower in-hospital mortality (p = 0.12) and lower mortality plus nonfatal thrombotic event occurrences (p = 0.10). Patients on metformin had similar clinical outcomes compared to patients without DM. In a multiple regression analysis, metformin use was associated with less days in hospital and lower intubation rate. In conclusion, metformin treatment in COVID-19 patients with DM was associated with lower markers of inflammation, renal ischemia, and thrombosis, and fewer hospitalized days and intubation requirement. Further focused studies are required to support these findings.
Keywords COVID-19 • Diabetes • Metformin • Thromboelastography • Biomarker • Death • Intubation
Highlights • Fasting blood glucose level in patients with has been shown to be associated with severity of the disease and poor outcomes, including mortality. • Metformin use in patients with DM is associated with less COVID-19-related mortality, but the underlying mechanism behind this association remains unclear. • In this single center study, metformin treatment in COVID-19 patients with DM was associated with lower markers of inflammation, renal ischemia, and thrombosis, and fewer hospitalized days and intubation requirement. • In a multiple regression analysis, metformin use was associated with less days in hospital and lower intubation rate.
Declarations Conflict of interest Dr. Gurbel reports grants and personal fees from Bayer HealthCare LLC, Otitopic Inc, Amgen, Janssen, and US World-Meds LLC; grants from Instrumentation Laboratory, Haemonetics, Medicure Inc, Idorsia Pharmaceuticals, and Hikari Dx; personal fees from UpToDate; Dr Gurbel is a relator and expert witness in litigation involving clopidogrel; in addition, Dr. Gurbel has two patents, Detection of restenosis risk in patients issued and Assessment of cardiac health and thrombotic risk in a patient. Dr. Tantry reports receiving honoraria from UptoDate and Aggredyne. Other authors report no disclosures. Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Alberti, Zimmet, Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation, Diabet Med
Apicella, Campopiano, Mantuano, Mazoni, Coppelli et al., COVID-19 in people with diabetes: understanding the reasons for worse outcomes, Lancet Diabetes Endocrinol
Bai, Chen, Metformin: a novel weapon against inflammation, Front Pharmacol
Bigagli, Lodovici, Circulating oxidative stress biomarkers in clinical studies on type 2 diabetes and its complications, Oxid Med Cell Longev
Chen, Liu, Ye, Effects of metformin on blood and urine pro-inflammatory mediators in patients with type 2 diabetes, J Inflamm (Lond)
Chen, Yang, Cheng, Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care
Crouse, Grimes, Li, Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes, Front Endocrinol
Eikelboom, Hankey, Thom, Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management and Avoidance (CHARISMA) Investigators. Incomplete inhibition of thromboxane biosynthesis by acetylsalicylic acid: determinants and effect on cardiovascular risk, Circulation
Eikelboom, Hirsh, Weitz, Aspirin-resistant thromboxane biosynthesis and the risk of myocardial infarction, stroke, or cardiovascular death in patients at high risk for cardiovascular events, Circulation
Endo, Miyashita, Sasaki, Probucol and atorvastatin decrease urinary 8-hydroxy-2'-deoxyguanosine in patients with diabetes and hypercholesterolemia, J Atheroscler Thromb
Ghany, Palacio, Dawkins, Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA, Diabetes Metab Syndr
Graille, Wild, Sauvain, Urinary 8-OHdG as a biomarker for oxidative stress: a systematic literature review and meta-analysis, Int J Mol Sci
Gurbel, Bliden, Tantry, Defining platelet response to acetylsalicylic acid: the relation between inhibition of serum thromboxane B2 and agonist-induced platelet aggregation, J Thromb Thrombolysis, doi:10.1007/s11239-020-02334-x
Gurbel, Bliden, Tantry, First report of the point-of-care TEG: a technical validation study of the TEG-6S system, Platelets
Han, Ma, Sun, The association between antidiabetic agents and clinical outcomes of COVID-19 in patients with diabetes: a systematic review and meta-analysis, Arch Med Res
Holman, Knighton, Kar, Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes Endocrinol
Kajiwara, Kusaka, Kimura, Metformin mediates protection against legionella pneumonia through activation of AMPK and mitochondrial reactive oxygen species, J Immunol
Kaneto, Kimura, Obata, Multifaceted mechanisms of action of metformin which have been unraveled one after another in the long history, Int J Mol Sci
Katagiri, Doi, Honda, Negishi, Combination of two urinary biomarkers predicts acute kidney injury after adult cardiac surgery, Ann Thorac Surg
Katagiri, Ishikane, Asai, Evaluation of coronavirus disease 2019 severity using urine biomarkers, Crit Care Explor
Kelly, Tannahill, Murphy, Neill, Metformin inhibits the production of reactive oxygen species from NADH: ubiquinone oxidoreductase to limit induction of Interleukin-1b (IL-1b) and boosts Interleukin-10 (IL-10) in Lipopolysaccharide (LPS)-activated macrophages, J Biol Chem
Khunti, Knighton, Zaccardi, Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol
Kumar, Arora, Sharma, Anikhindi, Bansal et al., Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis, Diabetes Metab Syndr
Lalau, Al-Salameh, Hadjadj, Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19, Diabetes Metab
Lazarus, Audrey, Wangsaputra, High admission blood glucose independently predicts poor prognosis in COVID-19 patients: a systematic review and dose-response metaanalysis, Diabetes Res Clin Pract
Lukito, Pranata, Henrina, The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes Metab Syndr
Luo, Qiu, Liu, Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis, Am J Trop Med Hyg
Minno, Turnu, Porro, 8-Hydroxy-2-deoxyguanosine levels and cardiovascular disease: a systematic review and meta-analysis of the literature, Antioxid Redox Signal
Negishi, Noiri, Doi, Monitoring of urinary L-type fatty acid-binding protein predicts histological severity of acute kidney injury, Am J Pathol
Petrilli, Jones, Yang, Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City, BMJ
Rocca, Buck, Petrucci, Thromboxane metabolite excretion is associated with serious vascular events in diabetes mellitus: a sub-study of the ASCEND trial, Eur Heart J
Roncon, Zuin, Rigatelli, Zuliani, Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome, J Clin Virol
Saha, Al-Rifai, Saha, Diabetes prevalence and mortality in COVID-19 patients: a systematic review, meta-analysis, and meta-regression, J Diabetes Metab Disord
Samuel, Varghese, Büsselberg, Therapeutic potential of metformin in COVID-19: reasoning for its protective role, Trends Microbiol
Scheen, Metformin and COVID-19: from cellular mechanisms to reduced mortality, Diabetes Metab
Tantry, Mahla, Gurbel, Aspirin resistance, Prog Cardiovasc Dis
Torigoe, Muta, Tsuji, Urinary liver-type fatty acid-binding protein predicts residual renal function decline in patients on peritoneal dialysis, Med Sci Monit
Tousoulis, Papageorgiou, Androulakis, Diabetes mellitus-associated vascular impairment: novel circulating biomarkers and therapeutic approaches, J Am Coll Cardiol
Valavanidis, Vlachogianni, Fiotakis, 8-Hydroxy2'-deoxyguanosine (8-OHdG): a critical biomarker of oxidative stress and carcinogenesis, J Environ Sci Health C
Viswanathan, Puvvula, Jamthikar, Bidirectional link between diabetes mellitus and coronavirus disease 2019 leading to cardiovascular disease: a narrative review, World J Diabetes
White-Dzuro, Gibson, Zazzeron, Multisystem effects of COVID-19: a concise review for practitioners, Postgrad Med
Yang, Lin, Ji, Guo, Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes, Acta Diabetol
Zhu, She, Cheng, Association of blood glucose control and outcomes in patients with COVID-19 and preexisting type 2 diabetes, Cell Metab
DOI record:
{
"DOI": "10.1007/s11239-022-02631-7",
"ISSN": [
"0929-5305",
"1573-742X"
],
"URL": "http://dx.doi.org/10.1007/s11239-022-02631-7",
"alternative-id": [
"2631"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "30 December 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 2,
"value": "18 January 2022"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "Dr. Gurbel reports grants and personal fees from Bayer HealthCare LLC, Otitopic Inc, Amgen, Janssen, and US WorldMeds LLC; grants from Instrumentation Laboratory, Haemonetics, Medicure Inc, Idorsia Pharmaceuticals, and Hikari Dx; personal fees from UpToDate; Dr Gurbel is a relator and expert witness in litigation involving clopidogrel; in addition, Dr. Gurbel has two patents, Detection of restenosis risk in patients issued and Assessment of cardiac health and thrombotic risk in a patient. Dr. Tantry reports receiving honoraria from UptoDate and Aggredyne. Other authors report no disclosures."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"affiliation": [],
"family": "Usman",
"given": "Abira",
"sequence": "first"
},
{
"affiliation": [],
"family": "Bliden",
"given": "Kevin P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cho",
"given": "Alastair",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Walia",
"given": "Naval",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jerjian",
"given": "Christophe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Singh",
"given": "Arvind",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kundan",
"given": "Parshotam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Duhan",
"given": "Sanchit",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tantry",
"given": "Udaya S.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5461-568X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gurbel",
"given": "Paul A.",
"sequence": "additional"
}
],
"container-title": [
"Journal of Thrombosis and Thrombolysis"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
1,
18
]
],
"date-time": "2022-01-18T09:22:57Z",
"timestamp": 1642497777000
},
"deposited": {
"date-parts": [
[
2022,
1,
18
]
],
"date-time": "2022-01-18T10:11:27Z",
"timestamp": 1642500687000
},
"funder": [
{
"name": "Platelet and Thrombosis Research"
}
],
"indexed": {
"date-parts": [
[
2022,
1,
19
]
],
"date-time": "2022-01-19T17:23:07Z",
"timestamp": 1642612987928
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "0929-5305"
},
{
"type": "electronic",
"value": "1573-742X"
}
],
"issued": {
"date-parts": [
[
2022,
1,
18
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
18
]
],
"date-time": "2022-01-18T00:00:00Z",
"timestamp": 1642464000000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
18
]
],
"date-time": "2022-01-18T00:00:00Z",
"timestamp": 1642464000000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11239-022-02631-7.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s11239-022-02631-7/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11239-022-02631-7.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1007",
"published": {
"date-parts": [
[
2022,
1,
18
]
]
},
"published-online": {
"date-parts": [
[
2022,
1,
18
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/S2213-8587(20)30238-2",
"author": "M Apicella",
"doi-asserted-by": "crossref",
"first-page": "782",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2631_CR1",
"unstructured": "Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, Del Prato S (2020) COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol 8:782–792",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.4239/wjd.v12.i3.215",
"author": "V Viswanathan",
"doi-asserted-by": "crossref",
"first-page": "215",
"journal-title": "World J Diabetes",
"key": "2631_CR2",
"unstructured": "Viswanathan V, Puvvula A, Jamthikar AD et al (2021) Bidirectional link between diabetes mellitus and coronavirus disease 2019 leading to cardiovascular disease: a narrative review. World J Diabetes 12:215–237",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1136/bmj.m1966",
"author": "CM Petrilli",
"doi-asserted-by": "crossref",
"first-page": "1966",
"journal-title": "BMJ",
"key": "2631_CR3",
"unstructured": "Petrilli CM, Jones SA, Yang J (2020) Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City. BMJ 369:1966",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1016/j.jcv.2020.104354",
"author": "L Roncon",
"doi-asserted-by": "crossref",
"first-page": "104354",
"journal-title": "J Clin Virol",
"key": "2631_CR4",
"unstructured": "Roncon L, Zuin M, Rigatelli G, Zuliani G (2020) Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J Clin Virol 127:104354",
"volume": "127",
"year": "2020"
},
{
"DOI": "10.1007/s40200-021-00779-2",
"doi-asserted-by": "crossref",
"key": "2631_CR5",
"unstructured": "Saha S, Al-Rifai RH, Saha S (2021) Diabetes prevalence and mortality in COVID-19 patients: a systematic review, meta-analysis, and meta-regression. J Diabetes Metab Disord 1–12"
},
{
"DOI": "10.1016/j.diabres.2020.108561",
"author": "G Lazarus",
"doi-asserted-by": "crossref",
"first-page": "108561",
"journal-title": "Diabetes Res Clin Pract",
"key": "2631_CR6",
"unstructured": "Lazarus G, Audrey J, Wangsaputra VK et al (2021) High admission blood glucose independently predicts poor prognosis in COVID-19 patients: a systematic review and dose-response meta-analysis. Diabetes Res Clin Pract 171:108561",
"volume": "171",
"year": "2021"
},
{
"DOI": "10.4269/ajtmh.20-0375",
"author": "P Luo",
"doi-asserted-by": "crossref",
"first-page": "69",
"journal-title": "Am J Trop Med Hyg",
"key": "2631_CR7",
"unstructured": "Luo P, Qiu L, Liu Y et al (2020) Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis. Am J Trop Med Hyg 103:69–72",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.11.006",
"author": "AA Lukito",
"doi-asserted-by": "crossref",
"first-page": "2177",
"journal-title": "Diabetes Metab Syndr",
"key": "2631_CR8",
"unstructured": "Lukito AA, Pranata R, Henrina J et al (2020) The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis. Diabetes Metab Syndr 14:2177–2183",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"author": "K Khunti",
"doi-asserted-by": "crossref",
"first-page": "293",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2631_CR9",
"unstructured": "Khunti K, Knighton P, Zaccardi F et al (2021) Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England. Lancet Diabetes Endocrinol 9:293–303",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2021.02.022",
"author": "R Ghany",
"doi-asserted-by": "crossref",
"first-page": "513",
"journal-title": "Diabetes Metab Syndr",
"key": "2631_CR10",
"unstructured": "Ghany R, Palacio A, Dawkins E et al (2021) Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA. Diabetes Metab Syndr 15:513–518",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.4049/jimmunol.1700474",
"author": "C Kajiwara",
"doi-asserted-by": "crossref",
"first-page": "623",
"journal-title": "J Immunol",
"key": "2631_CR11",
"unstructured": "Kajiwara C, Kusaka Y, Kimura S et al (2018) Metformin mediates protection against legionella pneumonia through activation of AMPK and mitochondrial reactive oxygen species. J Immunol 200:623–631",
"volume": "200",
"year": "2018"
},
{
"DOI": "10.1074/jbc.M115.662114",
"author": "B Kelly",
"doi-asserted-by": "crossref",
"first-page": "20348",
"journal-title": "J Biol Chem",
"key": "2631_CR12",
"unstructured": "Kelly B, Tannahill GM, Murphy MP, O’Neill LAJ (2015) Metformin inhibits the production of reactive oxygen species from NADH: ubiquinone oxidoreductase to limit induction of Interleukin-1b (IL-1b) and boosts Interleukin-10 (IL-10) in Lipopolysaccharide (LPS)-activated macrophages. J Biol Chem 290:20348–20359",
"volume": "290",
"year": "2015"
},
{
"DOI": "10.3390/ijms22052596",
"author": "H Kaneto",
"doi-asserted-by": "crossref",
"first-page": "2596",
"journal-title": "Int J Mol Sci",
"key": "2631_CR13",
"unstructured": "Kaneto H, Kimura T, Obata A et al (2021) Multifaceted mechanisms of action of metformin which have been unraveled one after another in the long history. Int J Mol Sci 22:2596",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S",
"author": "KG Alberti",
"doi-asserted-by": "crossref",
"first-page": "539",
"journal-title": "Diabet Med",
"key": "2631_CR14",
"unstructured": "Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553",
"volume": "15",
"year": "1998"
},
{
"DOI": "10.3109/09537104.2016.1153617",
"author": "PA Gurbel",
"doi-asserted-by": "crossref",
"first-page": "642",
"journal-title": "Platelets",
"key": "2631_CR15",
"unstructured": "Gurbel PA, Bliden KP, Tantry US et al (2016) First report of the point-of-care TEG: a technical validation study of the TEG-6S system. Platelets 27:642–649",
"volume": "27",
"year": "2016"
},
{
"DOI": "10.1007/s11239-020-02334-x",
"author": "PA Gurbel",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Thrombolysis",
"key": "2631_CR16",
"unstructured": "Gurbel PA, Bliden KP, Tantry US (2020) Defining platelet response to acetylsalicylic acid: the relation between inhibition of serum thromboxane B2 and agonist-induced platelet aggregation. J Thromb Thrombolysis. https://doi.org/10.1007/s11239-020-02334-x",
"year": "2020"
},
{
"DOI": "10.5551/jat.13.68",
"author": "K Endo",
"doi-asserted-by": "crossref",
"first-page": "68",
"journal-title": "J Atheroscler Thromb",
"key": "2631_CR17",
"unstructured": "Endo K, Miyashita Y, Sasaki H et al (2006) Probucol and atorvastatin decrease urinary 8-hydroxy-2’-deoxyguanosine in patients with diabetes and hypercholesterolemia. J Atheroscler Thromb 13:68–75",
"volume": "13",
"year": "2006"
},
{
"DOI": "10.1016/j.athoracsur.2011.10.048",
"author": "D Katagiri",
"doi-asserted-by": "crossref",
"first-page": "577",
"journal-title": "Ann Thorac Surg",
"key": "2631_CR18",
"unstructured": "Katagiri D, Doi K, Honda K, Negishi K et al (2012) Combination of two urinary biomarkers predicts acute kidney injury after adult cardiac surgery. Ann Thorac Surg 93:577–583",
"volume": "93",
"year": "2012"
},
{
"DOI": "10.1080/00325481.2020.1823094",
"author": "G White-Dzuro",
"doi-asserted-by": "crossref",
"first-page": "20",
"journal-title": "Postgrad Med",
"key": "2631_CR19",
"unstructured": "White-Dzuro G, Gibson LE, Zazzeron L et al (2021) Multisystem effects of COVID-19: a concise review for practitioners. Postgrad Med 133:20–27",
"volume": "133",
"year": "2021"
},
{
"DOI": "10.1007/s00592-009-0109-4",
"author": "JK Yang",
"doi-asserted-by": "crossref",
"first-page": "193",
"journal-title": "Acta Diabetol",
"key": "2631_CR20",
"unstructured": "Yang JK, Lin SS, Ji XJ, Guo LM (2010) Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol 47:193–199",
"volume": "47",
"year": "2010"
},
{
"DOI": "10.1016/j.dsx.2020.04.044",
"author": "A Kumar",
"doi-asserted-by": "crossref",
"first-page": "535",
"journal-title": "Diabetes Metab Syndr",
"key": "2631_CR21",
"unstructured": "Kumar A, Arora A, Sharma P, Anikhindi SA, Bansal N, Singla V, Khare S, Srivastava A (2020) Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes Metab Syndr 14:535–545",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.04.021",
"author": "L Zhu",
"doi-asserted-by": "crossref",
"first-page": "1068",
"journal-title": "Cell Metab",
"key": "2631_CR22",
"unstructured": "Zhu L, She Z-G, Cheng X et al (2020) Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab 31:1068–1077",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"author": "N Holman",
"doi-asserted-by": "crossref",
"first-page": "823",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2631_CR23",
"unstructured": "Holman N, Knighton P, Kar P et al (2020) Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol 8:823–833",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.3389/fendo.2020.600439",
"author": "AB Crouse",
"doi-asserted-by": "crossref",
"first-page": "600439",
"journal-title": "Front Endocrinol",
"key": "2631_CR24",
"unstructured": "Crouse AB, Grimes T, Li P et al (2021) Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes. Front Endocrinol 11:600439",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.tim.2021.03.004",
"doi-asserted-by": "crossref",
"key": "2631_CR25",
"unstructured": "Samuel SM, Varghese E, Büsselberg D (2021) Therapeutic potential of metformin in COVID-19: reasoning for its protective role. Trends Microbiol. S0966–842X(21)00063–9"
},
{
"DOI": "10.1016/S0140-6736(98)07037-8",
"author": "UK Prospective Diabetes Study (UKPDS) Group",
"doi-asserted-by": "crossref",
"first-page": "854",
"journal-title": "Lancet",
"key": "2631_CR26",
"unstructured": "UK Prospective Diabetes Study (UKPDS) Group (1998) Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 352:854–865",
"volume": "352",
"year": "1998"
},
{
"DOI": "10.3389/fphar.2021.622262",
"author": "B Bai",
"doi-asserted-by": "crossref",
"first-page": "622262",
"journal-title": "Front Pharmacol",
"key": "2631_CR27",
"unstructured": "Bai B, Chen H (2021) Metformin: a novel weapon against inflammation. Front Pharmacol 12:622262",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1186/s12950-016-0142-3",
"author": "W Chen",
"doi-asserted-by": "crossref",
"first-page": "34",
"journal-title": "J Inflamm (Lond)",
"key": "2631_CR28",
"unstructured": "Chen W, Liu X, Ye S (2016) Effects of metformin on blood and urine pro-inflammatory mediators in patients with type 2 diabetes. J Inflamm (Lond) 13:34",
"volume": "13",
"year": "2016"
},
{
"DOI": "10.2337/dc20-0660",
"author": "Y Chen",
"doi-asserted-by": "crossref",
"first-page": "1399",
"journal-title": "Diabetes Care",
"key": "2631_CR29",
"unstructured": "Chen Y, Yang D, Cheng B et al (2020) Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care 43:1399–1407",
"volume": "43",
"year": "2020"
},
{
"author": "K Torigoe",
"first-page": "e928236",
"journal-title": "Med Sci Monit",
"key": "2631_CR30",
"unstructured": "Torigoe K, Muta K, Tsuji K et al (2020) Urinary liver-type fatty acid-binding protein predicts residual renal function decline in patients on peritoneal dialysis. Med Sci Monit 26:e928236",
"volume": "26",
"year": "2020"
},
{
"author": "K Negishi",
"first-page": "25",
"issue": "1154–59",
"journal-title": "Am J Pathol",
"key": "2631_CR31",
"unstructured": "Negishi K, Noiri E, Doi K et al (2009) Monitoring of urinary L-type fatty acid-binding protein predicts histological severity of acute kidney injury. Am J Pathol 174(1154–59):25",
"volume": "174",
"year": "2009"
},
{
"DOI": "10.1097/CCE.0000000000000170",
"author": "D Katagiri",
"doi-asserted-by": "crossref",
"first-page": "e0170",
"journal-title": "Crit Care Explor",
"key": "2631_CR32",
"unstructured": "Katagiri D, Ishikane M, Asai Y et al (2020) Evaluation of coronavirus disease 2019 severity using urine biomarkers. Crit Care Explor 2:e0170",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1016/j.pcad.2009.05.001",
"author": "US Tantry",
"doi-asserted-by": "crossref",
"first-page": "141",
"journal-title": "Prog Cardiovasc Dis",
"key": "2631_CR33",
"unstructured": "Tantry US, Mahla E, Gurbel PA (2009) Aspirin resistance. Prog Cardiovasc Dis 52:141–152",
"volume": "52",
"year": "2009"
},
{
"DOI": "10.1161/01.CIR.0000013777.21160.07",
"author": "JW Eikelboom",
"doi-asserted-by": "crossref",
"first-page": "1650",
"journal-title": "Circulation",
"key": "2631_CR34",
"unstructured": "Eikelboom JW, Hirsh J, Weitz JI et al (2002) Aspirin-resistant thromboxane biosynthesis and the risk of myocardial infarction, stroke, or cardiovascular death in patients at high risk for cardiovascular events. Circulation 105:1650–1655",
"volume": "105",
"year": "2002"
},
{
"DOI": "10.1161/CIRCULATIONAHA.108.768283",
"author": "JW Eikelboom",
"doi-asserted-by": "crossref",
"first-page": "1705",
"journal-title": "Circulation",
"key": "2631_CR35",
"unstructured": "Eikelboom JW, Hankey GJ, Thom J et al (2008) Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management and Avoidance (CHARISMA) Investigators. Incomplete inhibition of thromboxane biosynthesis by acetylsalicylic acid: determinants and effect on cardiovascular risk. Circulation 118:1705–1712",
"volume": "118",
"year": "2008"
},
{
"author": "B Rocca",
"first-page": "ehaa946",
"issue": "2",
"journal-title": "Eur Heart J",
"key": "2631_CR36",
"unstructured": "Rocca B, Buck G, Petrucci G et al (2020) Thromboxane metabolite excretion is associated with serious vascular events in diabetes mellitus: a sub-study of the ASCEND trial. Eur Heart J 41(2):ehaa946",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.3390/ijms21113743",
"author": "M Graille",
"doi-asserted-by": "crossref",
"first-page": "3743",
"journal-title": "Int J Mol Sci",
"key": "2631_CR37",
"unstructured": "Graille M, Wild P, Sauvain JJ et al (2020) Urinary 8-OHdG as a biomarker for oxidative stress: a systematic literature review and meta-analysis. Int J Mol Sci 21:3743",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2013.03.089",
"author": "D Tousoulis",
"doi-asserted-by": "crossref",
"first-page": "667",
"journal-title": "J Am Coll Cardiol",
"key": "2631_CR38",
"unstructured": "Tousoulis D, Papageorgiou N, Androulakis E, et al (2013) Diabetes mellitus-associated vascular impairment: novel circulating biomarkers and therapeutic approaches. J Am Coll Cardiol 62:667–676",
"volume": "62",
"year": "2013"
},
{
"DOI": "10.1089/ars.2015.6508",
"author": "A Di Minno",
"doi-asserted-by": "crossref",
"first-page": "548",
"journal-title": "Antioxid Redox Signal",
"key": "2631_CR39",
"unstructured": "Di Minno A, Turnu L, Porro B et al (2016) 8-Hydroxy-2-deoxyguanosine levels and cardiovascular disease: a systematic review and meta-analysis of the literature. Antioxid Redox Signal 24:548–555",
"volume": "24",
"year": "2016"
},
{
"DOI": "10.1080/10590500902885684",
"author": "A Valavanidis",
"doi-asserted-by": "crossref",
"first-page": "120",
"journal-title": "J Environ Sci Health C",
"key": "2631_CR40",
"unstructured": "Valavanidis A, Vlachogianni T, Fiotakis C et al (2009) “8-Hydroxy2’-deoxyguanosine (8-OHdG): a critical biomarker of oxidative stress and carcinogenesis. J Environ Sci Health C 27:120–139",
"volume": "27",
"year": "2009"
},
{
"DOI": "10.1155/2019/5953685",
"author": "E Bigagli",
"doi-asserted-by": "crossref",
"first-page": "5953685",
"journal-title": "Oxid Med Cell Longev",
"key": "2631_CR41",
"unstructured": "Bigagli E, Lodovici M (2019) Circulating oxidative stress biomarkers in clinical studies on type 2 diabetes and its complications. Oxid Med Cell Longev 2019:5953685",
"volume": "2019",
"year": "2019"
},
{
"DOI": "10.1016/j.diabet.2020.07.006",
"author": "AJ Scheen",
"doi-asserted-by": "crossref",
"first-page": "423",
"journal-title": "Diabetes Metab",
"key": "2631_CR42",
"unstructured": "Scheen AJ (2020) Metformin and COVID-19: from cellular mechanisms to reduced mortality. Diabetes Metab 46:423–426",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.101216",
"author": "JD Lalau",
"doi-asserted-by": "crossref",
"first-page": "101216",
"journal-title": "Diabetes Metab",
"key": "2631_CR43",
"unstructured": "Lalau JD, Al-Salameh A, Hadjadj S et al (2021) Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19. Diabetes Metab 47:101216",
"volume": "47",
"year": "2021"
},
{
"author": "T Han",
"first-page": "00167",
"issue": "21",
"journal-title": "Arch Med Res",
"key": "2631_CR44",
"unstructured": "Han T, Ma S, Sun C et al (2021) The association between anti-diabetic agents and clinical outcomes of COVID-19 in patients with diabetes: a systematic review and meta-analysis. Arch Med Res S0188–4409(21):00167–00173",
"volume": "S0188–4409",
"year": "2021"
}
],
"reference-count": 44,
"references-count": 44,
"relation": {},
"score": 1,
"short-container-title": [
"J Thromb Thrombolysis"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Cardiology and Cardiovascular Medicine",
"Hematology"
],
"subtitle": [],
"title": [
"Metformin use in patients hospitalized with COVID-19: lower inflammation, oxidative stress, and thrombotic risk markers and better clinical outcomes"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy"
}
