Predictors of Mortality in Hemodialyzed Patients after SARS-CoV-2 Infection
et al., Journal of Clinical Medicine, doi:10.3390/jcm11020285, Jan 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 133 COVID+ hemodialysis patients in Poland, showing lower mortality with existing vitamin D use, without statistical significance.
This is the 65th of 135 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
|
risk of death, 14.4% lower, RR 0.86, p = 0.61, treatment 28 of 85 (32.9%), control 25 of 48 (52.1%), NNT 5.2, adjusted per study, odds ratio converted to relative risk, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Tylicki et al., 6 Jan 2022, retrospective, Poland, peer-reviewed, 10 authors, study period 6 October, 2020 - 28 February, 2021, dosage not specified.
Predictors of Mortality in Hemodialyzed Patients after SARS-CoV-2 Infection
Journal of Clinical Medicine, doi:10.3390/jcm11020285
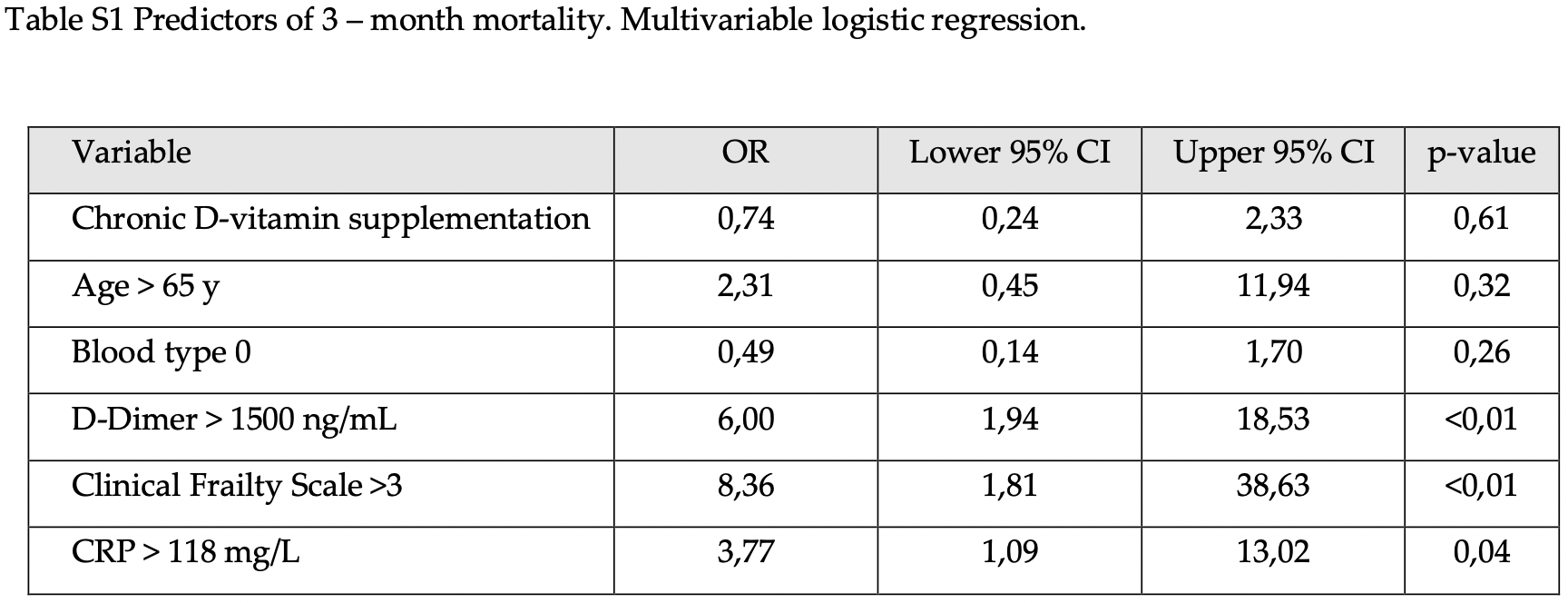
Introduction: The determinants of COVID-19 mortality are well-characterized in the general population. Less numerous and inconsistent data are among the maintenance hemodialysis (HD) patients, who are the population most at risk of an unfavorable prognosis. Methods: In this retrospective cohort study we included all adult HD patients from the Pomeranian Voivodeship, Poland, with laboratory-confirmed SARS-CoV-2 infection hospitalized between 6 October 2020 and 28 February 2021, both those who survived, and also those who died. Demographic, clinical, treatment, and laboratory data on admission, were extracted from the electronic medical records of the dedicated hospital and patients' dialysis unit, and compared between survivors and nonsurvivors. We used univariable and multivariable logistic regression methods to explore the risk factors associated with 3-month all-cause mortality. Results: The 133 patients (53.38% males) aged 73.0 (67-79) years, with a median duration of hemodialysis of 42.0 (17-86) months, were included in this study. At diagnosis, the majority were considered to have a mild course (34 of 133 patients were asymptomatic, another 63 subjects presented mild symptoms), while 36 (27.07%) patients had low blood oxygen saturation and required oxygen supplementation. Three-month mortality was 39.08% including an in-hospital case fatality rate of 33.08%. Multivariable logistic regression showed that the frailty clinical index of 4 or greater (OR 8.36,; p < 0.01), D-Dimer of 1500 ng/mL or greater (6.00, 1.94-18.53; p < 0.01), and CRP of >118 mg/L at admission (3.77 1.09-13.01; p = 0.04) were found to be predictive of mortality. Conclusion: Very high 3-month all-cause mortality in hospitalized HD patients was determined mainly by frailty. High CRP and D-dimer levels upon admission further confer mortality risk.
Author Contributions: Conceptualization, L.T.; methodology, A.O., P.T., K.P., E.P.-R., A.P., K.S., J.W. and L.T.; collecting data, A.O., P.T., K.P., E.P.-R., A.P., K.S. and B.B.; data analysis, A.O., P.T., K.P., E.P.-R., J.W. and L.T.; writing-original draft preparation, L.T.; writing-review and editing, B.B., E.P.-R., A.D.-Ś., J.W. and L.T.; visualization, P.T., J.W. and L.T.; supervision, A.D.-Ś. and L.T. All authors have read and agreed to the published version of the manuscript.
References
Alberici, Delbarba, Manenti, Econimo, Valerio et al., Management of Patients on Dialysis and With Kidney Transplantation During the SARS-CoV-2 (COVID-19) Pandemic in Brescia, Italy, Kidney Int. Rep, doi:10.1016/j.ekir.2020.04.001
Biedunkiewicz, Tylicki, Puchalska-Regli Ńska, Ąbrowska, Ślizie Ń et al., SARS-CoV-2 infection in vaccinated maintenance hemodialysis patients despite anti-spike seroconversion: A report of 3 breakthrough cases, Eur. J. Transl. Clin. Med, doi:10.31373/ejtcm/143208
Boakye, Rillmann, Walter, Jansen, Hoffmeister et al., Impact of comorbidity and frailty on prognosis in colorectal cancer patients: A systematic review and meta-analysis, Cancer Treat. Rev, doi:10.1016/j.ctrv.2018.02.003
Campi, Gennari, Merlotti, Mingiano, Frosali et al., Vitamin D and COVID-19 severity and related mortality: A prospective study in Italy, BMC Infect. Dis
Castilla, Guevara, Miqueleiz, Baigorria, Ibero-Esparza et al., Risk Factors of Infection, Hospitalization and Death from SARS-CoV-2: A Population-Based Cohort Study, J. Clin. Med, doi:10.3390/jcm10122608
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation, J. Chronic Dis, doi:10.1016/0021-9681(87)90171-8
Charlson, Szatrowski, Peterson, Gold, Validation of a combined comorbidity index, J. Clin. Epidemiol, doi:10.1016/0895-4356(94)90129-5
Church, Rogers, Rockwood, Theou, A scoping review of the Clinical Frailty Scale, BMC Geriatr, doi:10.1186/s12877-020-01801-7
Connors, Levy, COVID-19 and its implications for thrombosis and anticoagulation, Blood
Dentali, Sironi, Ageno, Turato, Bonfanti et al., Non-O blood type is the commonest genetic risk factor for VTE: Results from a meta-analysis of the literature, Semin. Thromb. Hemost
Guven, Gultekin, The effect of high-dose parenteral vitamin D3 on COVID-19-related inhospital mortality in critical COVID-19 patients during intensive care unit admission: An observational cohort study, Eur. J. Clin. Nutr
Haarhaus, Santos, Haase, Mota Veiga, Lucas et al., Risk prediction of COVID-19 incidence and mortality in a large multi-national hemodialysis cohort: Implications for management of the pandemic in outpatient hemodialysis settings, Clin. Kidney J, doi:10.1093/ckj/sfab037
Hilbrands, Duivenvoorden, Vart, Franssen, Hemmelder et al., COVID-19-related mortality in kidney transplant and dialysis patients: Results of the ERACODA collaboration, Nephrol. Dial. Transpl, doi:10.1093/ndt/gfaa261
Huang, Yao, Gu, Wang, Ren et al., 1-year outcomes in hospital survivors with COVID-19: A longitudinal cohort study, Lancet, doi:10.1016/S0140-6736(21)01755-4
Inciardi, Lupi, Zaccone, Italia, Raffo et al., Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19), JAMA Cardiol, doi:10.1001/jamacardio.2020.1096
Kakkanattu, Sankarasubbaiyan, Yadav, Kundu, Gowda Bg et al., Outcome and Determinants of Outcome of COVID-19 Infection Among Hemodialysis Patients: Findings From a National Dialysis Network Program in India, Kidney Int. Rep, doi:10.1016/j.ekir.2021.03.003
Kibler, Dietrich, Kanso, Carmona, Marchandot et al., Risk and Severity of COVID-19 and ABO Blood Group in Transcatheter Aortic Valve Patients, J. Clin. Med, doi:10.3390/jcm9113769
Kowalska, Baranski, Brozek, Kaleta-Pilarska, Zejda, COVID-19-related risk of in-hospital death in Silesia, Poland, Pol. Arch. Intern. Med, doi:10.20452/pamw.15893
Lakkireddy, Gadiga, Malathi, Karra, Raju et al., Impact of daily high dose oral vitamin D therapy on the inflammatory markers in patients with COVID 19 disease, Sci. Rep
Muscedere, Waters, Varambally, Bagshaw, Boyd et al., The impact of frailty on intensive care unit outcomes: A systematic review and meta-analysis, Intensive Care Med, doi:10.1007/s00134-017-4867-0
Nguyen, Chinn, De Ferrante, Kirby, Hohmann et al., Male gender is a predictor of higher mortality in hospitalized adults with COVID-19, PLoS ONE, doi:10.1371/journal.pone.0254066
Och, Tylicki, Polewska, Puchalska-Regli Ńska, Parczewska et al., Persistent post-COVID-19 syndrome in hemodialyzed patients-A longitudinal cohort study from the North of Poland, J. Clin. Med, doi:10.3390/jcm10194451
Puchalska-Regli Ńska, Debska-Slizien, Biedunkiewicz, Tylicki, Polewska et al., Extremely high mortality in COVID-19 hemodialyzed patients before the anti-SARS-CoV-2 vaccination era. Large database from the North of Poland, Pol. Arch. Intern. Med, doi:10.20452/pamw.16028
Ranganathan, Pramesh, Aggarwal, Common pitfalls in statistical analysis: Logistic regression, Perspect. Clin. Res, doi:10.4103/picr.PICR_87_17
Ray, Schull, Vermeulen, Park, Association Between ABO and Rh Blood Groups and SARS-CoV-2 Infection or Severe COVID-19 Illness: A Population-Based Cohort Study, Ann. Intern. Med, doi:10.7326/M20-4511
Scarpioni, Manini, Valsania, De Amicis, Albertazzi et al., Covid-19 and its impact on nephropathic patients: The experience at Ospedale "Guglielmo da Saliceto, Piacenza. G Ital. Nefrol
Shi, Wang, Ye, Gu, Wang et al., Predictors of mortality in patients with coronavirus disease 2019: A systematic review and meta-analysis, BMC Infect Dis, doi:10.1186/s12879-021-06369-0
Stroehlein, Wallqvist, Iannizzi, Mikolajewska, Metzendorf et al., Vitamin D supplementation for the treatment of COVID-19: A living systematic review, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD015043
Tang, Tu, Xiong, Sun, Tian et al., Risk factors for the mortality of hemodialysis patients with COVID-19: A multicenter study from the overall hemodialysis population in Wuhan, Semin. Dial, doi:10.1111/sdi.12995
Tian, Jiang, Yao, Nicholson, Li et al., Predictors of mortality in hospitalized COVID-19 patients: A systematic review and meta-analysis, J. Med. Virol
Turgutalp, Ozturk, Arici, Eren, Gorgulu et al., Determinants of mortality in a large group of hemodialysis patients hospitalized for COVID-19, BMC Nephrol, doi:10.1186/s12882-021-02233-0
Tylicki, Biedunkiewicz, Ąbrowska, Ślizie Ń, Tylicki et al., Humoral response to SARS-CoV-2 vaccination promises to improve the catastrophic prognosis of hemodialysis patients as a result of COVID-19. The COViNEPH Project, Pol. Arch. Intern. Med, doi:10.20452/pamw.16069
Vergara, Molina-Van Den, Bosch, Toapanta, Villegas et al., The Impact of Age on Mortality in Chronic Haemodialysis Popu-Lation with COVID-19, J. Clin. Med, doi:10.3390/jcm10143022
Wang, Li, Lu, Huang, Does comorbidity increase the risk of patients with COVID-19: Evidence from meta-analysis, Aging, doi:10.18632/aging.103000
Wheeler, Winkelmayer, Kdigo, Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD), Kidney Int. Suppl, doi:10.1016/j.kisu.2017.04.001
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Wynants, Van Calster, Collins, Riley, Heinze et al., Prediction models for diagnosis and prognosis of covid-19: Systematic review and critical appraisal, BMJ, doi:10.1136/bmj.m1328
Zhang, Jiao, Cao, Huo, Zhu et al., Frailty as a predictor of mortality among patients with COVID-19: A systematic review and meta-analysis, BMC Geriatr, doi:10.1186/s12877-021-02138-5
DOI record:
{
"DOI": "10.3390/jcm11020285",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm11020285",
"abstract": "<jats:p>Introduction: The determinants of COVID-19 mortality are well-characterized in the general population. Less numerous and inconsistent data are among the maintenance hemodialysis (HD) patients, who are the population most at risk of an unfavorable prognosis. Methods: In this retrospective cohort study we included all adult HD patients from the Pomeranian Voivodeship, Poland, with laboratory-confirmed SARS-CoV-2 infection hospitalized between 6 October 2020 and 28 February 2021, both those who survived, and also those who died. Demographic, clinical, treatment, and laboratory data on admission, were extracted from the electronic medical records of the dedicated hospital and patients’ dialysis unit, and compared between survivors and non-survivors. We used univariable and multivariable logistic regression methods to explore the risk factors associated with 3-month all-cause mortality. Results: The 133 patients (53.38% males) aged 73.0 (67–79) years, with a median duration of hemodialysis of 42.0 (17–86) months, were included in this study. At diagnosis, the majority were considered to have a mild course (34 of 133 patients were asymptomatic, another 63 subjects presented mild symptoms), while 36 (27.07%) patients had low blood oxygen saturation and required oxygen supplementation. Three-month mortality was 39.08% including an in-hospital case fatality rate of 33.08%. Multivariable logistic regression showed that the frailty clinical index of 4 or greater (OR 8.36, 95%CI 1.81–38.6; p < 0.01), D-Dimer of 1500 ng/mL or greater (6.00, 1.94–18.53; p < 0.01), and CRP of >118 mg/L at admission (3.77 1.09–13.01; p = 0.04) were found to be predictive of mortality. Conclusion: Very high 3-month all-cause mortality in hospitalized HD patients was determined mainly by frailty. High CRP and D-dimer levels upon admission further confer mortality risk.</jats:p>",
"alternative-id": [
"jcm11020285"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-5515-5072",
"affiliation": [],
"authenticated-orcid": false,
"family": "Tylicki",
"given": "Leszek",
"sequence": "first"
},
{
"affiliation": [],
"family": "Puchalska-Reglińska",
"given": "Ewelina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tylicki",
"given": "Piotr",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Och",
"given": "Aleksander",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Polewska",
"given": "Karolina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Biedunkiewicz",
"given": "Bogdan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Parczewska",
"given": "Aleksandra",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Szabat",
"given": "Krzysztof",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wolf",
"given": "Jacek",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8210-8063",
"affiliation": [],
"authenticated-orcid": false,
"family": "Dębska-Ślizień",
"given": "Alicja",
"sequence": "additional"
}
],
"container-title": [
"Journal of Clinical Medicine"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
1,
7
]
],
"date-time": "2022-01-07T06:14:02Z",
"timestamp": 1641536042000
},
"deposited": {
"date-parts": [
[
2022,
1,
7
]
],
"date-time": "2022-01-07T06:19:17Z",
"timestamp": 1641536357000
},
"indexed": {
"date-parts": [
[
2022,
1,
8
]
],
"date-time": "2022-01-08T06:04:06Z",
"timestamp": 1641621846386
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "2077-0383"
}
],
"issue": "2",
"issued": {
"date-parts": [
[
2022,
1,
6
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2022,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
6
]
],
"date-time": "2022-01-06T00:00:00Z",
"timestamp": 1641427200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/11/2/285/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "285",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
1,
6
]
]
},
"published-online": {
"date-parts": [
[
2022,
1,
6
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.3390/jcm10143022",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1093/ndt/gfaa261",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.20452/pamw.16028",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.3390/jcm10194451",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1001/jamacardio.2020.1096",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.20452/pamw.16069",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.31373/ejtcm/143208",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1016/0895-4356(94)90129-5",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1186/s12877-020-01801-7",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.4103/picr.PICR_87_17",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.20452/pamw.15893",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1371/journal.pone.0254066",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.18632/aging.103000",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.3390/jcm10122608",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1186/s12882-021-02233-0",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1093/ckj/sfab037",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1111/sdi.12995",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"article-title": "Covid-19 and its impact on nephropathic patients: The experience at Ospedale “Guglielmo da Saliceto” in Piacenza",
"author": "Scarpioni",
"first-page": "1",
"journal-title": "G Ital. Nefrol.",
"key": "ref20",
"volume": "37",
"year": "2020"
},
{
"DOI": "10.1186/s12877-021-02138-5",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1007/s00134-017-4867-0",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1016/j.ctrv.2018.02.003",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1186/s12879-021-06369-0",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1002/jmv.26050",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1016/j.ekir.2021.03.003",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1016/j.ekir.2020.04.001",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1182/blood.2020006000",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.7326/M20-4511",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.3390/jcm9113769",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1055/s-0032-1315758",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1186/s12879-021-06281-7",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1038/s41430-021-00984-5",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1038/s41598-021-90189-4",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1002/14651858.CD015043",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1016/j.kisu.2017.04.001",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1016/S0140-6736(21)01755-4",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1136/bmj.m1328",
"doi-asserted-by": "publisher",
"key": "ref38"
}
],
"reference-count": 38,
"references-count": 38,
"relation": {},
"score": 1,
"short-container-title": [
"JCM"
],
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": [
"Predictors of Mortality in Hemodialyzed Patients after SARS-CoV-2 Infection"
],
"type": "journal-article",
"volume": "11"
}
