Up to 40% of COVID-19 Critically Ill Patients Have Vitamin D Deficiency
et al., Preprints, doi:10.20944/preprints202009.0555.v1, Sep 2020
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
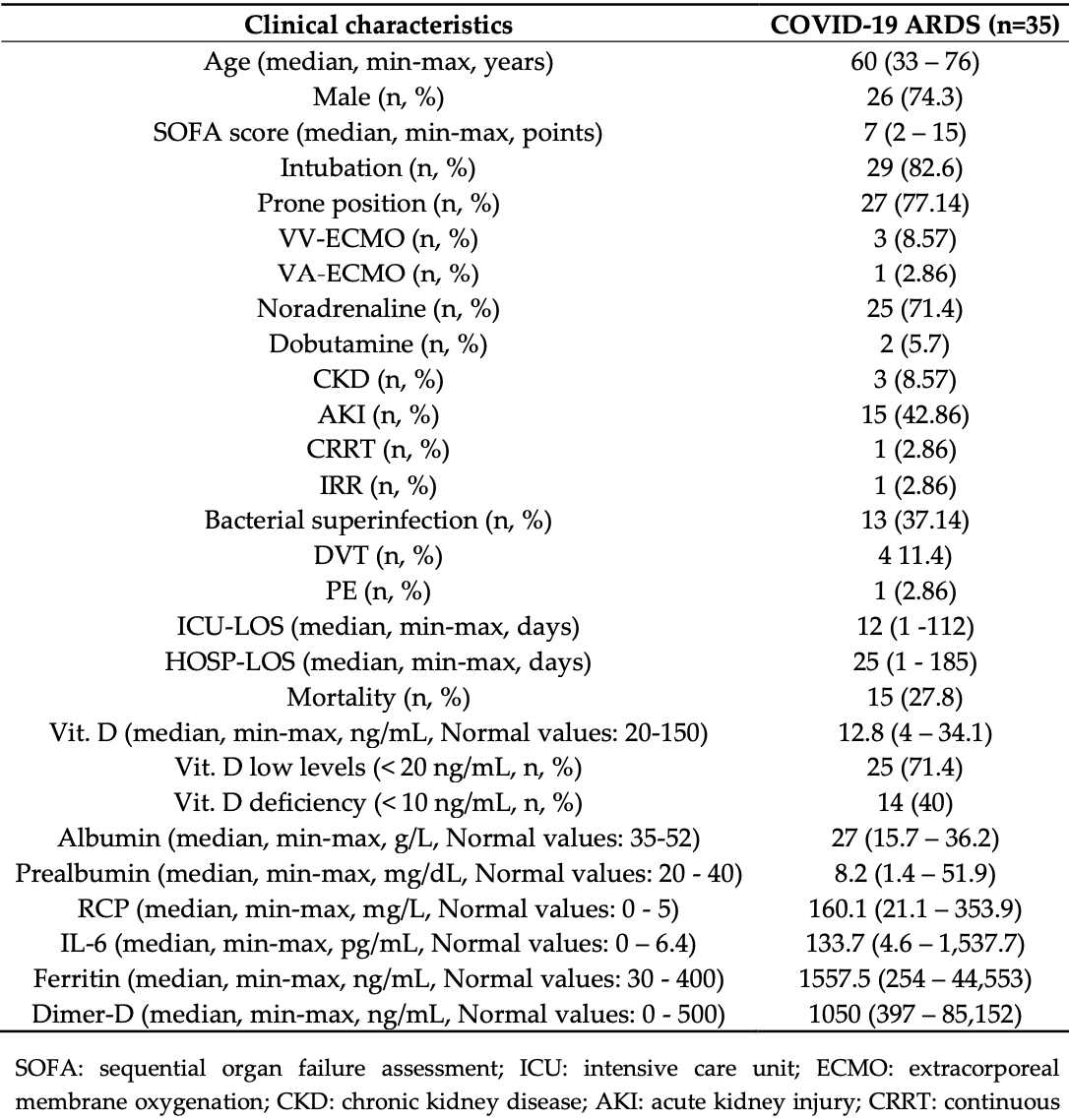
Retrospective 35 ICU patients in Spain showing 71% of patients had vitamin D levels <20 ng/mL, and 40% <10 ng/mL.
Tomasa-Irriguible et al., 23 Sep 2020, retrospective, preprint, 2 authors.
Contact: teresatomasa@gmail.com (corresponding author), larabielsa@gmail.com, luisabordeje@gmail.com.
Up to 40% of COVID-19 Critically Ill Patients Have Vitamin D Deficiency
doi:10.20944/preprints202009.0555.v1
Background: Coronavirus disease (COVID-19) has caused more than 745,000 deaths worldwide. Vitamin D has been identified as a potential strategy to prevent or treat this disease. The purpose of the study was to measure vitamin D at hospital admission of COVID-19; Methods: We included critically ill patients with the polymerase chain reaction positive test for COVID-19, from March to April, 2020. Statistical significance was defined as P < .05. All tests were 2-tailed; Results: A total of 35 patients (median age, 60 years; 26 [74.3%] male) were included. Vitamin D levels were categorized as deficient for 14 participants (40%). Vitamin D deficiency was associated with vitamin A (P= 0.003) and Zinc (P= 0.019) deficiency and lower levels of albumin (P= 0.026) and prealbumin (P= 0.009). Overall, none of the studied variables were associated with vitamin D status: mortality, intensive care unit (ICU) or hospital stay, necessity of vasoactive agents, intubation, prone position, C reactive protein (CRP), Dimer-D, Interleukin 6 levels (IL-6), ferritin levels, or bacterial superinfection; Conclusions: In this single-center, retrospective cohort study, deficient vitamin D status was found in 40% in COVID-19 critically ill patients. However, deficient vitamin D status was not associated with inflammation or outcome.
Conflicts of Interest: The authors declare no conflict of interest.
References
Ali, Role of vitamin D in preventing of COVID-19 infection, progression and severity, J Infect Public Health, doi:10.1016/j.jiph.2020.06.021
Ards Definition, Force, Ranieri, Rubenfeld, Thompson et al., Acute respiratory distress syndrome: the Berlin definition, JAMA
Castillo, Costa, Barrios, Díaz, Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, Journal of Steroid Biochemistry and Molecular Biology
Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet, doi:10.1016/S0140-6736(20)30211-7
Fan, Brodie, Slutsky, Acute respiratory distress syndrome, JAMA, doi:10.1001/jama.2017.21907
Grant, Lahore, Mcdonnell, Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/nu12040988
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Laird, Rhodes, Kenny, Vitamin, And inflammation: potential implications for severity of Covid-19, Ir. Med. J
Martineau, Jolliffe, Hooper, Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity, Clin. Endocrinol, doi:10.1111/cen.14276
Ranieri, Rubenfeld, Thompson, Ferguson, Caldwell et al., Acute respiratory distress syndrome: the Berlin definition, JAMA -J. Am. Med. Assoc, doi:10.1001/jama.2012.5669
Russo, Carlucci, Cipriani, Ragno, Piemonte et al., Metabolic changes following 500 μg monthly administration of calcidiol: a study in normal females, Calcif. Tissue Int, doi:10.1007/s00223-011-9513-1
Viechtbauer, Smits, Kotz, Bud´e, Spigt et al., A simple formula for the calculation of sample size in pilot studies, J. Clin. Epidemiol, doi:10.1016/j.jclinepi.2015.04.014
Wu, Chen, Cai, Xia, Zhou et al., Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 Pneumonia in Wuhan, China, JAMA Intern. Med, doi:10.1001/jamainternmed.2020.0994
Yin, Agrawal, Vitamin D and inflammatory diseases, J Inflamm Res, doi:10.2147/JIR.S63898
DOI record:
{
"DOI": "10.20944/preprints202009.0555.v1",
"URL": "http://dx.doi.org/10.20944/preprints202009.0555.v1",
"abstract": "<jats:p>Background: Coronavirus disease (COVID-19) has caused more than 745,000 deaths worldwide. Vitamin D has been identified as a potential strategy to prevent or treat this disease. The purpose of the study was to measure vitamin D at hospital admission of COVID-19; Methods: We included critically ill patients with the polymerase chain reaction positive test for COVID-19, from March to April, 2020. Statistical significance was defined as P &amp;lt; .05. All tests were 2-tailed; Results: A total of 35 patients (median age, 60 years; 26 [74.3%] male) were included. Vitamin D levels were categorized as deficient for 14 participants (40%). Vitamin D deficiency was associated with vitamin A (P= 0.003) and Zinc (P= 0.019) deficiency and lower levels of albumin (P= 0.026) and prealbumin (P= 0.009). Overall, none of the studied variables were associated with vitamin D status: mortality, intensive care unit (ICU) or hospital stay, necessity of vasoactive agents, intubation, prone position, C reactive protein (CRP), Dimer-D, Interleukin 6 levels (IL-6), ferritin levels, or bacterial superinfection; Conclusions: In this single-center, retrospective cohort study, deficient vitamin D status was found in 40% in COVID-19 critically ill patients. However, deficient vitamin D status was not associated with inflammation or outcome.</jats:p>",
"accepted": {
"date-parts": [
[
2020,
9,
22
]
]
},
"author": [
{
"affiliation": [],
"family": "Tomasa-Irriguible",
"given": "Teresa-Maria",
"sequence": "first"
},
{
"affiliation": [],
"family": "Bielsa-Berrocal",
"given": "Lara",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
9,
24
]
],
"date-time": "2020-09-24T10:02:37Z",
"timestamp": 1600941757000
},
"deposited": {
"date-parts": [
[
2020,
9,
24
]
],
"date-time": "2020-09-24T12:33:42Z",
"timestamp": 1600950822000
},
"group-title": "MEDICINE & PHARMACOLOGY",
"indexed": {
"date-parts": [
[
2022,
3,
29
]
],
"date-time": "2022-03-29T04:32:51Z",
"timestamp": 1648528371860
},
"is-referenced-by-count": 1,
"issued": {
"date-parts": [
[
2020,
9,
23
]
]
},
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
9,
23
]
],
"date-time": "2020-09-23T00:00:00Z",
"timestamp": 1600819200000
}
}
],
"member": "1968",
"original-title": [],
"posted": {
"date-parts": [
[
2020,
9,
23
]
]
},
"prefix": "10.20944",
"published": {
"date-parts": [
[
2020,
9,
23
]
]
},
"publisher": "MDPI AG",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.preprints.org/manuscript/202009.0555/v1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Up to 40% of COVID-19 Critically Ill Patients Have Vitamin D Deficiency",
"type": "posted-content"
}
