Premorbid aspirin use is not associated with lower mortality in older inpatients with SARS-CoV-2 pneumonia
et al., GeroScience, doi:10.1007/s11357-021-00499-8, Jan 2022
Retrospective 1,047 pneumonia patients in 5 COVID-19 geriatric units in France and Switzerland, significantly higher ICU admission and longer hospital stays with existing aspirin treatment. Numbers in this study appear to be inconsistent, for example the abstract says 147 of 301 aspirin patients died, shown as 34.3%, while Table 1 shows 104 of 301 (34.6%).
|
risk of death, 10.0% higher, RR 1.10, p = 0.52, treatment 101 of 301 (33.6%), control 224 of 746 (30.0%).
|
|
risk of ICU admission, 109.7% higher, RR 2.10, p = 0.007, treatment 22 of 301 (7.3%), control 26 of 746 (3.5%).
|
|
hospitalization time, 10.0% higher, relative time 1.10, p = 0.02, treatment 301, control 746.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Sullerot et al., 7 Jan 2022, retrospective, propensity score weighting, multiple countries, peer-reviewed, 15 authors, study period 1 March, 2020 - 31 December, 2020.
Premorbid aspirin use is not associated with lower mortality in older inpatients with SARS-CoV-2 pneumonia
GeroScience, doi:10.1007/s11357-021-00499-8
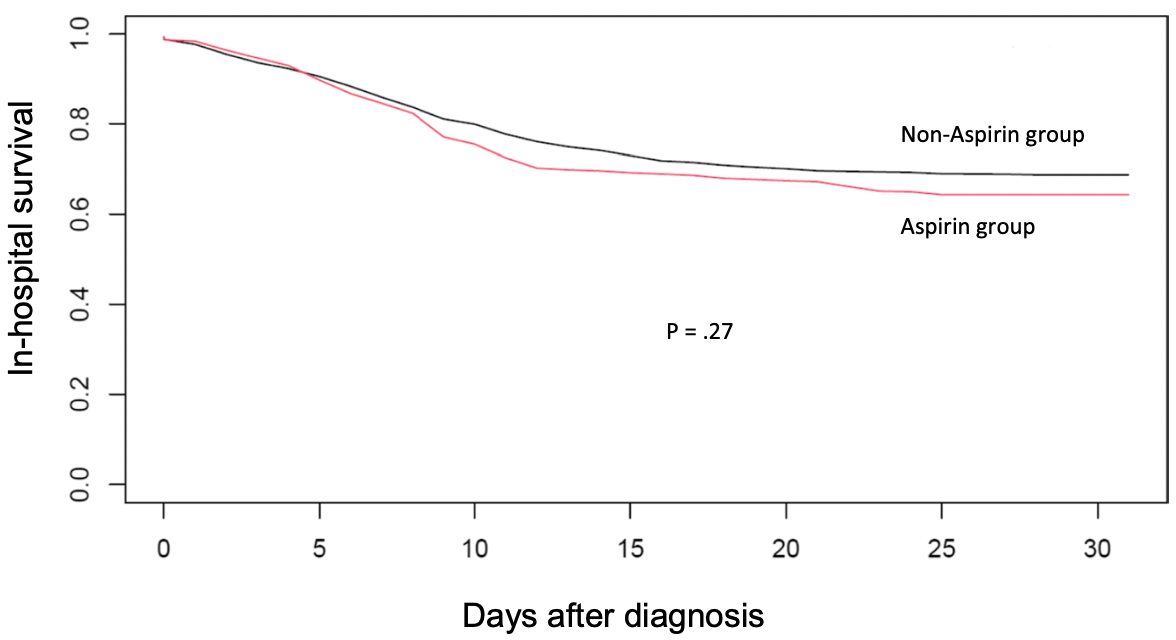
SIPTW) was applied. To assess the association between aspirin use and in-hospital 30-day mortality, SIPTW-adjusted Kaplan-Meier and Cox proportional hazards regression analyses were performed. Of the 1047 patients with SARS-CoV-2 pneumonia and median age 86 years, 301 (28.7%) were taking aspirin treatment before admission. One hundred forty-seven (34.3%) patients who had taken aspirin died in hospital within 1 month vs 118 patients (30.7%) without aspirin. After SIPTW, aspirin treatment was not significantly associated with lower mortality (adjusted hazard ratio: 1.10 [0.81-1.49], P = .52). Moreover, patients on aspirin had a longer hospital stay and were Abstract Platelet aggregation has been associated with COVID-19 pathogenesis. In older patients hospitalized for SARS-CoV-2 pneumonia, we aimed to investigate the association between aspirin use before admission and the risk of in-hospital all-cause mortality. We performed a retrospective international cohort study in five COVID-19 geriatric units in France and Switzerland. Among 1,357 consecutive hospitalized patients aged 75 or older and testing positive for SARS-CoV-2, we included 1,072 with radiologically confirmed pneumonia. To adjust for confounders, a propensity score for treatment was created, and stabilized inverse probability of treatment weighting
Conflict of interest The authors declare no competing interests. Publisher's note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Aghajani, Moradi, Amini, Tehrani, Pourheidar et al., Decreased in-hospital mortality associated with aspirin administration in hospitalized patients due to severe COVID-19, J Med Virol
Alves, Fernandes, Bahat, Benetos, Clemente et al., Protecting older patients with cardiovascular diseases from COVID-19 complications using current medications, Eur Geriatr Med
Bianconi, Violi, Fallarino, Pignatelli, Sahebkar et al., Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19 ?, Drugs
Cangemi, Casciaro, Rossi, Calvieri, Bucci et al., Platelet activation is associated with myocardial infarction in patients with pneumonia, J Am Coll Cardiol
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis
Chow, Khanna, Kethireddy, Yamane, Levine et al., Aspirin use is associated with decreased mechanical ventilation, ICU admission, and inhospital mortality in hospitalized patients with COVID-19
Eisen, Leder, Woods, Lockery, Mcguinness et al., Effect of aspirin on deaths associated with sepsis in healthy older people (ANTISEPSIS): a randomised, double-blind, placebo-controlled primary prevention trial, Lancet Respir Med
Falcone, Russo, Cangemi, Farcomeni, Calvieri et al., Lower mortality rate in elderly patients with community-onset pneumonia on treatment with aspirin, J Am Heart Assoc
Fine, Auble, Yealy, Hanusa, Weissfeld et al., A prediction rule to identify lowrisk patients with community-acquired pneumonia, N Engl J Med
Gallay, Tran, Perrodeau, Vignier, Mahevas et al., Fourteen-day survival among older adults with severe infection with severe acute respiratory syndrome coronavirus 2 treated with corticosteroid: a cohort study, Clin Microbiol Infect
Granger, Sergeant, Lunt, Avoiding pitfalls when combining multiple imputation and propensity scores, Stat Med
Gurbel, Bliden, Schrör, Can an old ally defeat a new enemy?, Circulation
Hamilton, Arnold, Henley, Payne, Aspirin reduces cardiovascular events in patients with pneumonia: a prior event rate ratio analysis in a large primary care database, Eur Respir J
Kalil, Metersky, Klompas, Muscedere, Sweeney et al., Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society, Clin Infect Dis
Katz, Ford, Moskowitz, Jackson, Jaffe, Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function, JAMA
Keane, Tilley, Cunningham, Smolenski, Kadioglu et al., Invasive Streptococcus pneumoniae trigger platelet activation via Toll-like receptor 2, J Thromb Haemost
Lala, Johnson, Januzzi, Russak, Paranjpe et al., Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection, J Am Coll Cardiol
Lim, Van Der Eerden, Laing, Boersma, Karalus et al., Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study, Thorax
Linden, Samuels, Using balance statistics to determine the optimal number of controls in matching studies, J Eval Clin Pract
Liu, Huang, Li, Zhou, Liang et al., Effect of low-dose aspirin on mortality and viral duration of the hospitalized adults with COVID-19, Medicine
Meizlish, Goshua, Liu, Fine, Amin et al., Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: a propensity scorematched analysis, Am J Hematol
Mendes, Serratrice, Herrmann, Genton, Périvier et al., Predictors of in-hospital mortality in older patients with COVID-19: the COVID age study, J Am Med Dir Assoc
Metlay, Waterer, Long, Anzueto, Brozek et al., Diagnosis and treatment of adults with community-acquired pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America, Am J Respir Crit Care Med
Odille, Girard, Sanchez, Lelarge, Mignot et al., Should we prescribe antibiotics in older patients presenting COVID-19 pneumonia?, J Am Med Dir Assoc
Osborne, Veigulis, Arreola, Mahajan, Röösli et al., Association of mortality and aspirin prescription for COVID-19 patients at the Veterans health administration, PLOS ONE
Oz, Gul, Kaya, Yazici, Bulut et al., Does aspirin use prevent acute coronary syndrome in patients with pneumonia: multicenter prospective randomized trial, Coron Artery Dis
Panka, De Grooth, Spoelstra-De Man, Looney, Tuinman, Prevention or treatment of ARDS with aspirin: a review of preclinical models and meta-analysis of clinical studies, Shock
Putot, Chague, Manckoundia, Cottin, Zeller, Post-infectious myocardial infarction: new insights for improved screening, JCM
Recovery Collaborative Group, Horby, Pessoa-Amorim, Staplin, Emberson et al., Aspirin in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial
Rizk, Lavie, Gupta, Low-dose aspirin for early COVID-19: does the early bird catch the worm?, Expert Opin Investig Drugs
Salah, Mehta, Meta-analysis of the effect of aspirin on mortality COVID-19, Am J Cardiol
Savarapu, Baral, Adhikari, Akanbi, Abdelazeem et al., Aspirin use is associated with decreased mortality in patients with COVID-19: a systematic review and meta-analysis
Son, Noh, Lee, Seo, Park et al., Effect of aspirin on coronavirus disease 2019: a nationwide case-control study in South Korea, Med
Srivastava, Kumar, Use of aspirin in reduction of mortality of COVID-19 patients: a metanalysis, Int J Clin Pract
Vf, Alvarez, Weissfeld, Angus, Chirinos et al., Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease, JAMA
Xu, Hou, Xu, Li, Fu et al., Clinical characteristics and risk factors of cardiac involvement in COVID-19, J Am Heart Assoc
Xu, Ross, Raebel, Shetterly, Blanchette et al., Use of stabilized inverse propensity scores as weights to directly estimate relative risk and its confidence intervals, Value Health
Xu, Samanapally, Nathala, Salunkhe, Furmanek et al., Outcomes and risk factors for cardiovascular events in hospitalized COVID-19 patients, J Cardiothorac Vasc Anesth, doi:10.1053/j.jvca.2021.03.035
Zhang, Liu, Wang, Yang, Li et al., SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19, J Hematol Oncol
DOI record:
{
"DOI": "10.1007/s11357-021-00499-8",
"ISSN": [
"2509-2715",
"2509-2723"
],
"URL": "http://dx.doi.org/10.1007/s11357-021-00499-8",
"alternative-id": [
"499"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "21 September 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "13 December 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "7 January 2022"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The authors declare no competing interests."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"affiliation": [],
"family": "Sullerot",
"given": "Coralie",
"sequence": "first"
},
{
"affiliation": [],
"family": "Bouiller",
"given": "Kevin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Laborde",
"given": "Caroline",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gilis",
"given": "Marine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fèvre",
"given": "Amélie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hacquin",
"given": "Arthur",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Manckoundia",
"given": "Patrick",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hoefler",
"given": "Florence",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bermejo",
"given": "Messaline",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mendes",
"given": "Aline",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Serratrice",
"given": "Christine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prendki",
"given": "Virginie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sanchez",
"given": "Stéphane",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4408-554X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Putot",
"given": "Alain",
"sequence": "additional"
},
{
"affiliation": [],
"name": "On behalf of ESGIE (European Society of Clinical Microbiology, European Society of Clinical Microbiological and Infectious Diseases, Study Group for Infections in the Elderly)",
"sequence": "additional"
}
],
"container-title": [
"GeroScience"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
1,
7
]
],
"date-time": "2022-01-07T01:03:12Z",
"timestamp": 1641517392000
},
"deposited": {
"date-parts": [
[
2022,
1,
7
]
],
"date-time": "2022-01-07T02:27:16Z",
"timestamp": 1641522436000
},
"indexed": {
"date-parts": [
[
2022,
1,
7
]
],
"date-time": "2022-01-07T06:44:52Z",
"timestamp": 1641537892494
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "2509-2715"
},
{
"type": "electronic",
"value": "2509-2723"
}
],
"issued": {
"date-parts": [
[
2022,
1,
7
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
7
]
],
"date-time": "2022-01-07T00:00:00Z",
"timestamp": 1641513600000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
7
]
],
"date-time": "2022-01-07T00:00:00Z",
"timestamp": 1641513600000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11357-021-00499-8.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s11357-021-00499-8/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11357-021-00499-8.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1007",
"published": {
"date-parts": [
[
2022,
1,
7
]
]
},
"published-online": {
"date-parts": [
[
2022,
1,
7
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1097/SHK.0000000000000745",
"author": "BA Panka",
"doi-asserted-by": "publisher",
"first-page": "13",
"journal-title": "Shock",
"key": "499_CR1",
"unstructured": "Panka BA, de Grooth H-J, Spoelstra–de Man A, Looney M, Tuinman P-R. Prevention or treatment of ARDS with aspirin: a review of preclinical models and meta- analysis of clinical studies. Shock. 2017;47:13–21.",
"volume": "47",
"year": "2017"
},
{
"DOI": "10.1016/j.cmi.2021.03.021",
"author": "L Gallay",
"doi-asserted-by": "publisher",
"first-page": "1145",
"journal-title": "Clin Microbiol Infect",
"key": "499_CR2",
"unstructured": "Gallay L, Tran V-T, Perrodeau E, Vignier N, Mahevas M, Bisio F, et al. Fourteen-day survival among older adults with severe infection with severe acute respiratory syndrome coronavirus 2 treated with corticosteroid: a cohort study. Clin Microbiol Infect. 2021;27:1145–50.",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1007/s40265-020-01365-1",
"author": "V Bianconi",
"doi-asserted-by": "publisher",
"first-page": "1383",
"journal-title": "Drugs",
"key": "499_CR3",
"unstructured": "Bianconi V, Violi F, Fallarino F, Pignatelli P, Sahebkar A, Pirro M. Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19 ? Drugs. 2020;80:1383–96.",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047830",
"author": "PA Gurbel",
"doi-asserted-by": "publisher",
"first-page": "315",
"journal-title": "Circulation",
"key": "499_CR4",
"unstructured": "Gurbel PA, Bliden KP, Schrör K. Can an old ally defeat a new enemy? Circulation. 2020;142:315–7.",
"volume": "142",
"year": "2020"
},
{
"DOI": "10.1161/JAHA.114.001595",
"doi-asserted-by": "crossref",
"key": "499_CR5",
"unstructured": "Falcone M, Russo A, Cangemi R, Farcomeni A, Calvieri C, Barillà F, et al. Lower mortality rate in elderly patients with community‐onset pneumonia on treatment with aspirin. J Am Heart Assoc. 2015;4."
},
{
"DOI": "10.1183/13993003.02795-2020",
"doi-asserted-by": "crossref",
"key": "499_CR6",
"unstructured": "Hamilton F, Arnold D, Henley W, Payne RA. Aspirin reduces cardiovascular events in patients with pneumonia: a prior event rate ratio analysis in a large primary care database. Eur Respir J. 2020;57:2002795."
},
{
"DOI": "10.1111/ijcp.14515",
"doi-asserted-by": "crossref",
"key": "499_CR7",
"unstructured": "Srivastava R, Kumar A. Use of aspirin in reduction of mortality of COVID-19 patients: a metanalysis. Int J Clin Pract. 2021;75:e14515."
},
{
"DOI": "10.1016/j.amjcard.2020.12.073",
"author": "HM Salah",
"doi-asserted-by": "publisher",
"first-page": "158",
"journal-title": "Am J Cardiol",
"key": "499_CR8",
"unstructured": "Salah HM, Mehta JL. Meta-analysis of the effect of aspirin on mortality in COVID-19. Am J Cardiol. 2021;142:158–9.",
"volume": "142",
"year": "2021"
},
{
"DOI": "10.1002/ajh.26102",
"author": "ML Meizlish",
"doi-asserted-by": "publisher",
"first-page": "471",
"journal-title": "Am J Hematol",
"key": "499_CR9",
"unstructured": "Meizlish ML, Goshua G, Liu Y, Fine R, Amin K, Chang E, et al. Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: a propensity score-matched analysis. Am J Hematol. 2021;96:471–9.",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1097/MD.0000000000024544",
"author": "Q Liu",
"doi-asserted-by": "publisher",
"first-page": "e24544",
"journal-title": "Medicine",
"key": "499_CR10",
"unstructured": "Liu Q, Huang N, Li A, Zhou Y, Liang L, Song X, et al. Effect of low-dose aspirin on mortality and viral duration of the hospitalized adults with COVID-19. Medicine. 2021;100:e24544.",
"volume": "100",
"year": "2021"
},
{
"key": "499_CR11",
"unstructured": "Chow JH, Khanna AK, Kethireddy S, Yamane D, Levine A, Jackson AM, et al. Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19. Anesthesia & Analgesia. 2020;Publish Ahead of Print."
},
{
"DOI": "10.1101/2021.07.08.21260236",
"doi-asserted-by": "crossref",
"key": "499_CR12",
"unstructured": "Savarapu P, Baral N, Adhikari G, Akanbi M, Abdelazeem B, Isa SO, et al. Aspirin use is associated with decreased mortality in patients with COVID-19: a systematic review and meta-analysis. preprint. Infectious Diseases (except HIV/AIDS); 2021."
},
{
"DOI": "10.1002/jmv.27053",
"author": "M Haji Aghajani",
"doi-asserted-by": "publisher",
"first-page": "5390",
"journal-title": "J Med Virol",
"key": "499_CR13",
"unstructured": "Haji Aghajani M, Moradi O, Amini H, Azhdari Tehrani H, Pourheidar E, Rabiei MM, et al. Decreased in-hospital mortality associated with aspirin administration in hospitalized patients due to severe COVID-19. J Med Virol. 2021;93:5390–5.",
"volume": "93",
"year": "2021"
},
{
"key": "499_CR14",
"unstructured": "RECOVERY Collaborative Group, Horby PW, Pessoa-Amorim G, Staplin N, Emberson JR, Campbell M, et al. Aspirin in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. preprint. Infectious Diseases (except HIV/AIDS); 2021."
},
{
"DOI": "10.1053/j.jvca.2021.03.035",
"author": "Q Xu",
"doi-asserted-by": "publisher",
"journal-title": "J Cardiothorac Vasc Anesth",
"key": "499_CR15",
"unstructured": "Xu Q, Samanapally H, Nathala P, Salunkhe V, Furmanek S, Cahill MN, et al. Outcomes and risk factors for cardiovascular events in hospitalized COVID-19 patients. J Cardiothorac Vasc Anesth. 2021. https://doi.org/10.1053/j.jvca.2021.03.035.",
"year": "2021"
},
{
"DOI": "10.1016/j.jacc.2020.06.007",
"author": "A Lala",
"doi-asserted-by": "publisher",
"first-page": "533",
"journal-title": "J Am Coll Cardiol",
"key": "499_CR16",
"unstructured": "Lala A, Johnson KW, Januzzi JL, Russak AJ, Paranjpe I, Richter F, et al. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020;76:533–46.",
"volume": "76",
"year": "2020"
},
{
"author": "H Xu",
"first-page": "e016807",
"journal-title": "J Am Heart Assoc",
"key": "499_CR17",
"unstructured": "Xu H, Hou K, Xu R, Li Z, Fu H, Wen L, et al. Clinical characteristics and risk factors of cardiac involvement in COVID-19. J Am Heart Assoc. 2020;9:e016807.",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0246825",
"author": "TF Osborne",
"doi-asserted-by": "publisher",
"first-page": "e0246825",
"journal-title": "PLOS ONE",
"key": "499_CR18",
"unstructured": "Osborne TF, Veigulis ZP, Arreola DM, Mahajan SM, Röösli E, Curtin CM. Association of mortality and aspirin prescription for COVID-19 patients at the Veterans health administration. PLOS ONE. 2021;16:e0246825.",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1164/rccm.201908-1581ST",
"author": "JP Metlay",
"doi-asserted-by": "publisher",
"first-page": "e45",
"journal-title": "Am J Respir Crit Care Med",
"key": "499_CR19",
"unstructured": "Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200:e45-67.",
"volume": "200",
"year": "2019"
},
{
"DOI": "10.1016/j.jamda.2020.11.034",
"doi-asserted-by": "crossref",
"key": "499_CR20",
"unstructured": "Odille G, Girard N, Sanchez S, Lelarge S, Mignot A, Putot S, et al. Should we prescribe antibiotics in older patients presenting COVID-19 pneumonia? J Am Med Dir Assoc. 2021;22:258–9."
},
{
"DOI": "10.1016/j.jamda.2020.09.014",
"author": "A Mendes",
"doi-asserted-by": "publisher",
"first-page": "1546",
"journal-title": "J Am Med Dir Assoc",
"key": "499_CR21",
"unstructured": "Mendes A, Serratrice C, Herrmann FR, Genton L, Périvier S, Scheffler M, et al. Predictors of in-hospital mortality in older patients with COVID-19: the COVID age study. J Am Med Dir Assoc. 2020;21:1546-1554.e3.",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1001/jama.1963.03060120024016",
"author": "S Katz",
"doi-asserted-by": "publisher",
"first-page": "914",
"journal-title": "JAMA",
"key": "499_CR22",
"unstructured": "Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9.",
"volume": "185",
"year": "1963"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"author": "ME Charlson",
"doi-asserted-by": "publisher",
"first-page": "373",
"journal-title": "J Chronic Dis",
"key": "499_CR23",
"unstructured": "Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.",
"volume": "40",
"year": "1987"
},
{
"DOI": "10.1136/thorax.58.5.377",
"author": "WS Lim",
"doi-asserted-by": "publisher",
"first-page": "377",
"journal-title": "Thorax",
"key": "499_CR24",
"unstructured": "Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–82.",
"volume": "58",
"year": "2003"
},
{
"DOI": "10.1056/NEJM199701233360402",
"author": "MJ Fine",
"doi-asserted-by": "publisher",
"first-page": "243",
"journal-title": "N Engl J Med",
"key": "499_CR25",
"unstructured": "Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–50.",
"volume": "336",
"year": "1997"
},
{
"DOI": "10.1093/cid/ciw353",
"author": "AC Kalil",
"doi-asserted-by": "publisher",
"first-page": "e61",
"journal-title": "Clin Infect Dis",
"key": "499_CR26",
"unstructured": "Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63:e61-111.",
"volume": "63",
"year": "2016"
},
{
"DOI": "10.1002/sim.8355",
"author": "E Granger",
"doi-asserted-by": "publisher",
"first-page": "5120",
"journal-title": "Stat Med",
"key": "499_CR27",
"unstructured": "Granger E, Sergeant JC, Lunt M. Avoiding pitfalls when combining multiple imputation and propensity scores. Stat Med. 2019;38:5120–32.",
"volume": "38",
"year": "2019"
},
{
"DOI": "10.1111/j.1524-4733.2009.00671.x",
"author": "S Xu",
"doi-asserted-by": "publisher",
"first-page": "273",
"journal-title": "Value Health",
"key": "499_CR28",
"unstructured": "Xu S, Ross C, Raebel MA, Shetterly S, Blanchette C, Smith D. Use of stabilized inverse propensity scores as weights to directly estimate relative risk and its confidence intervals. Value Health. 2010;13:273–7.",
"volume": "13",
"year": "2010"
},
{
"DOI": "10.1111/jep.12072",
"author": "A Linden",
"doi-asserted-by": "publisher",
"first-page": "968",
"journal-title": "J Eval Clin Pract",
"key": "499_CR29",
"unstructured": "Linden A, Samuels SJ. Using balance statistics to determine the optimal number of controls in matching studies. J Eval Clin Pract. 2013;19:968–75.",
"volume": "19",
"year": "2013"
},
{
"DOI": "10.1007/s41999-021-00504-5",
"author": "M Alves",
"doi-asserted-by": "publisher",
"first-page": "725",
"journal-title": "Eur Geriatr Med",
"key": "499_CR30",
"unstructured": "Alves M, Fernandes MA, Bahat G, Benetos A, Clemente H, Grodzicki T, et al. Protecting older patients with cardiovascular diseases from COVID-19 complications using current medications. Eur Geriatr Med. 2021;12:725–39.",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1080/13543784.2021.1950687",
"doi-asserted-by": "crossref",
"key": "499_CR31",
"unstructured": "Rizk JG, Lavie CJ, Gupta A. Low-dose aspirin for early COVID-19: does the early bird catch the worm? Expert Opin Investig Drugs. 2021;30:785–8."
},
{
"DOI": "10.1016/S2213-2600(20)30411-2",
"doi-asserted-by": "crossref",
"key": "499_CR32",
"unstructured": "Eisen DP, Leder K, Woods RL, Lockery JE, McGuinness SL, Wolfe R, et al. Effect of aspirin on deaths associated with sepsis in healthy older people (ANTISEPSIS): a randomised, double-blind, placebo-controlled primary prevention trial. \nLancet Respir Med. 2021;9:186–5."
},
{
"DOI": "10.1097/MD.0000000000026670",
"author": "M Son",
"doi-asserted-by": "publisher",
"first-page": "e26670",
"journal-title": "Med (Baltimore)",
"key": "499_CR33",
"unstructured": "Son M, Noh M-G, Lee JH, Seo J, Park H, Yang S. Effect of aspirin on coronavirus disease 2019: a nationwide case-control study in South Korea. Med (Baltimore). 2021;100:e26670.",
"volume": "100",
"year": "2021"
},
{
"DOI": "10.1111/j.1538-7836.2010.04093.x",
"author": "C Keane",
"doi-asserted-by": "publisher",
"first-page": "2757",
"journal-title": "J Thromb Haemost",
"key": "499_CR34",
"unstructured": "Keane C, Tilley D, Cunningham A, Smolenski A, Kadioglu A, Cox D, et al. Invasive Streptococcus pneumoniae trigger platelet activation via Toll-like receptor 2. J Thromb Haemost. 2010;8:2757–65.",
"volume": "8",
"year": "2010"
},
{
"DOI": "10.1186/s13045-020-00954-7",
"author": "S Zhang",
"doi-asserted-by": "publisher",
"first-page": "120",
"journal-title": "J Hematol Oncol",
"key": "499_CR35",
"unstructured": "Zhang S, Liu Y, Wang X, Yang L, Li H, Wang Y, et al. SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19. J Hematol Oncol. 2020;13:120.",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1001/jama.2014.18229",
"author": "VF Corrales-Medina",
"doi-asserted-by": "publisher",
"first-page": "264",
"journal-title": "JAMA",
"key": "499_CR36",
"unstructured": "Corrales-Medina VF, Alvarez KN, Weissfeld LA, Angus DC, Chirinos JA, Chang C-CH, et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA. 2015;313:264–74.",
"volume": "313",
"year": "2015"
},
{
"DOI": "10.3390/jcm8060827",
"author": "A Putot",
"doi-asserted-by": "publisher",
"first-page": "827",
"journal-title": "JCM",
"key": "499_CR37",
"unstructured": "Putot A, Chague F, Manckoundia P, Cottin Y, Zeller M. Post-infectious myocardial infarction: new insights for improved screening. JCM. 2019;8:827.",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1097/MCA.0b013e32835d7610",
"author": "F Oz",
"doi-asserted-by": "publisher",
"first-page": "231",
"journal-title": "Coron Artery Dis",
"key": "499_CR38",
"unstructured": "Oz F, Gul S, Kaya MG, Yazici M, Bulut I, Elitok A, et al. Does aspirin use prevent acute coronary syndrome in patients with pneumonia: multicenter prospective randomized trial. Coron Artery Dis. 2013;24:231–7.",
"volume": "24",
"year": "2013"
},
{
"DOI": "10.1016/j.jacc.2014.07.985",
"author": "R Cangemi",
"doi-asserted-by": "publisher",
"first-page": "1917",
"journal-title": "J Am Coll Cardiol",
"key": "499_CR39",
"unstructured": "Cangemi R, Casciaro M, Rossi E, Calvieri C, Bucci T, Calabrese CM, et al. Platelet activation is associated with myocardial infarction in patients with pneumonia. J Am Coll Cardiol. 2014;64:1917–25.",
"volume": "64",
"year": "2014"
}
],
"reference-count": 39,
"references-count": 39,
"relation": {},
"score": 1,
"short-container-title": [
"GeroScience"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Geriatrics and Gerontology",
"Aging"
],
"subtitle": [],
"title": [
"Premorbid aspirin use is not associated with lower mortality in older inpatients with SARS-CoV-2 pneumonia"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy"
}