COVID‐19 fatality prediction in people with diabetes and prediabetes using a simple score upon hospital admission
et al., Diabetes, Obesity and Metabolism, doi:10.1111/dom.14256, Dec 2020
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
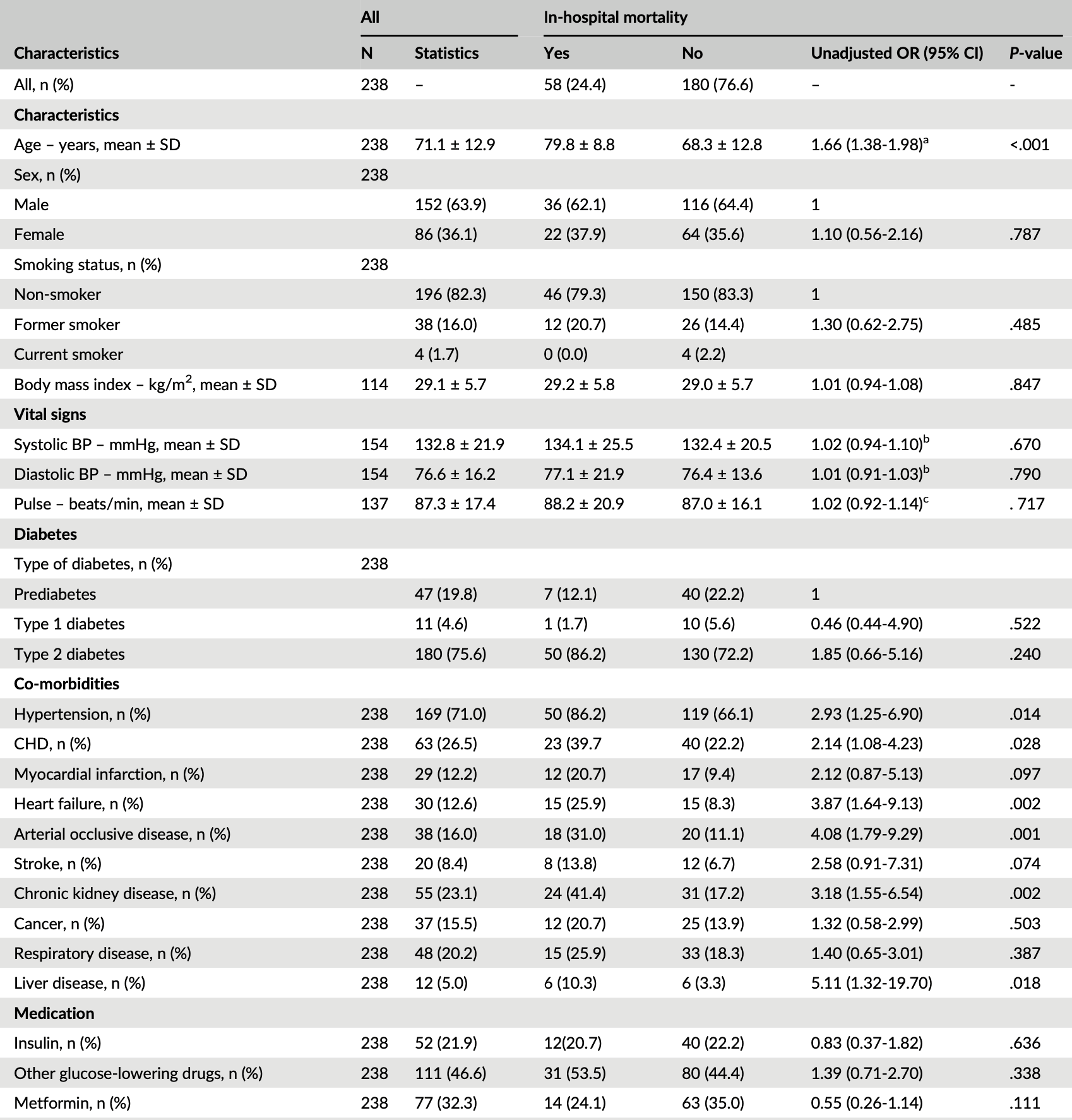
Retrospective 247 hospitalized COVID-19 diabetes patients, showing lower mortality with metformin use in unadjusted results.
Although the 37% lower mortality is not statistically significant, it is consistent with the significant 36% lower mortality [32‑40%] from meta-analysis of the 74 mortality results to date.
|
risk of death, 37.3% lower, RR 0.63, p = 0.13, treatment 14 of 77 (18.2%), control 44 of 161 (27.3%), NNT 11, odds ratio converted to relative risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Sourij et al., 4 Dec 2020, retrospective, Austria, peer-reviewed, mean age 71.1, 24 authors.
Contact: ha.sourij@medunigraz.at.
COVID‐19 fatality prediction in people with diabetes and prediabetes using a simple score upon hospital admission
Diabetes, Obesity and Metabolism, doi:10.1111/dom.14256
Aim: To assess predictors of in-hospital mortality in people with prediabetes and diabetes hospitalized for COVID-19 infection and to develop a risk score for identifying those at the greatest risk of a fatal outcome.
Materials and Methods: A combined prospective and retrospective, multicentre, cohort study was conducted at 10 sites in Austria in 247 people with diabetes or newly diagnosed prediabetes who were hospitalized with COVID-19. The primary outcome was in-hospital mortality and the predictor variables upon admission included clinical data, co-morbidities of diabetes or laboratory data. Logistic regression analyses were performed to identify significant predictors and to develop a risk score for in-hospital mortality.
Results: The mean age of people hospitalized (n = 238) for COVID-19 was 71.1 ± 12.9 years, 63.6% were males, 75.6% had type 2 diabetes, 4.6% had type 1 diabetes and 19.8% had prediabetes. The mean duration of hospital stay was 18 ± 16 days, 23.9% required ventilation therapy and 24.4% died in the hospital. The mortality rate in people with diabetes was numerically higher (26.7%) compared with those with prediabetes (14.9%) but without statistical significance (P = .128). A score including age, arterial occlusive disease, C-reactive protein, estimated glomerular filtration rate and aspartate aminotransferase levels at admission predicted in-hospital mortality with a Cstatistic of 0.889 (95% CI: 0.837-0.941) and calibration of 1.000 (P = .909).
Conclusions: The in-hospital mortality for COVID-19 was high in people with diabetes but not significantly different to the risk in people with prediabetes. A risk score
References
Abbasi-Oshaghi, Mirzaei, Farahani, Khodadadi, Tayebinia, Diagnosis and treatment of coronavirus disease 2019 (COVID-19): Laboratory, PCR, and chest CT imaging findings, Int J Surg
Barron, Bakhai, Kar, Associations of type 1 and type 2 diabetes with COVID-19-related mortality
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORO-NADO study, Diabetologia
Chen, Yang, Cheng, Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care
Coppelli, Giannarelli, Aragona, Hyperglycemia at hospital admission is associated with severity of the prognosis in patients hospitalized for COVID-19: The Pisa COVID-19 Study, Diabetes Care
Farah Abbas, Malle, Mader ; Martin Clodi, Klammer, Resl et al., Sourij and FA are the guarantors of the data. COVID-19 IN DIABETES IN AUSTRIA STUDY GROUP Medical University Graz, Rheumatology and Acute Geriatrics
Farahani, Mirzaei, Khodadadi, Abbasi-Oshaghi, Importance of hyperglycemia in preoperative, intraoperative and postoperative periods in COVID-19 patients, Int J Surg
Grasselli, Zangrillo, Zanella, Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy, JAMA
Guan, Ni, Hu, Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med
Harreiter, Roden, Diabetes mellitus -definition, classification, diagnosis, screening and prevention, Wien Klin Wochenschr
Holman, Knighton, Kar, Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes Endocrinol
Joshi, Caputo, Weitekamp, Karchmer, Infections in patients with diabetes mellitus, N Engl J Med
Karolyi, Pawelka, Kautzky-Willer, Wolf, Clinical Division for Endocrinology and Diabetology and Metabolic Diseases
Katulanda, Dissanayake, Ranathunga, Prevention and management of COVID-19 among patients with diabetes: an appraisal of the literature, Diabetologia
Klein, Fries, Kaser, Mathis, Thome et al., Unrecognized diabetes in critically ill COVID-19 patients, Crit Care
Pearson-Stuttard, Blundell, Harris, Cook, Critchley, Diabetes and infection: assessing the association with glycaemic control in population-based studies, Lancet Diabetes Endocrinol
Richardson, Hirsch, Narasimhan, Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area, JAMA
Shi, Zhang, Jiang, Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in Wuhan, China: a two-center, retrospective study, Diabetes Care
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention, JAMA
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.1111/dom.14256",
"ISSN": [
"1462-8902",
"1463-1326"
],
"URL": "http://dx.doi.org/10.1111/dom.14256",
"abstract": "<jats:title>Abstract</jats:title><jats:sec><jats:title>Aim</jats:title><jats:p>To assess predictors of in‐hospital mortality in people with prediabetes and diabetes hospitalized for COVID‐19 infection and to develop a risk score for identifying those at the greatest risk of a fatal outcome.</jats:p></jats:sec><jats:sec><jats:title>Materials and Methods</jats:title><jats:p>A combined prospective and retrospective, multicentre, cohort study was conducted at 10 sites in Austria in 247 people with diabetes or newly diagnosed prediabetes who were hospitalized with COVID‐19. The primary outcome was in‐hospital mortality and the predictor variables upon admission included clinical data, co‐morbidities of diabetes or laboratory data. Logistic regression analyses were performed to identify significant predictors and to develop a risk score for in‐hospital mortality.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>The mean age of people hospitalized (n = 238) for COVID‐19 was 71.1 ± 12.9 years, 63.6% were males, 75.6% had type 2 diabetes, 4.6% had type 1 diabetes and 19.8% had prediabetes. The mean duration of hospital stay was 18 ± 16 days, 23.9% required ventilation therapy and 24.4% died in the hospital. The mortality rate in people with diabetes was numerically higher (26.7%) compared with those with prediabetes (14.9%) but without statistical significance (<jats:italic>P</jats:italic> = .128). A score including age, arterial occlusive disease, C‐reactive protein, estimated glomerular filtration rate and aspartate aminotransferase levels at admission predicted in‐hospital mortality with a C‐statistic of 0.889 (95% CI: 0.837‐0.941) and calibration of 1.000 (<jats:italic>P</jats:italic> = .909).</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>The in‐hospital mortality for COVID‐19 was high in people with diabetes but not significantly different to the risk in people with prediabetes. A risk score using five routinely available patient variables showed excellent predictive performance for assessing in‐hospital mortality.</jats:p></jats:sec>",
"alternative-id": [
"10.1111/dom.14256"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2020-10-05"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2020-11-11"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2020-12-04"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3510-9594",
"affiliation": [
{
"name": "Clinical Division for Endocrinology and Diabetology Medical University Graz Graz Austria"
},
{
"name": "Center for Biomarker Research in Medicine (CBMed) Graz Austria"
}
],
"authenticated-orcid": false,
"family": "Sourij",
"given": "Harald",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Clinical Division for Endocrinology and Diabetology Medical University Graz Graz Austria"
},
{
"name": "Center for Biomarker Research in Medicine (CBMed) Graz Austria"
}
],
"family": "Aziz",
"given": "Faisal",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Medical Division for Endocrinology, Rheumatology and Acute Geriatrics Wilhelminen Hospital Vienna Vienna Austria"
}
],
"family": "Bräuer",
"given": "Alexander",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Division for Internal Medicine, Endocrinology, Diabetology and Metabolic Diseases, St. Vinzenz Hospital Zams Zams Austria"
}
],
"family": "Ciardi",
"given": "Christian",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Division for Internal Medicine Konventhospital Barmherzige Brüder Linz Linz Austria"
}
],
"family": "Clodi",
"given": "Martin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Medical Division for Endocrinology, Rheumatology and Acute Geriatrics Wilhelminen Hospital Vienna Vienna Austria"
}
],
"family": "Fasching",
"given": "Peter",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "4<sup>th</sup> Medical Division with Infectiology SMZ Süd – KFJ‐Hospital Vienna Vienna Austria"
}
],
"family": "Karolyi",
"given": "Mario",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3520-4105",
"affiliation": [
{
"name": "Clinical Division for Endocrinology and Diabetology and Metabolic Diseases AKH Vienna Vienna Austria"
}
],
"authenticated-orcid": false,
"family": "Kautzky‐Willer",
"given": "Alexandra",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Division for Internal Medicine Konventhospital Barmherzige Brüder Linz Linz Austria"
}
],
"family": "Klammer",
"given": "Carmen",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Division for Endocrinology and Diabetology Medical University Graz Graz Austria"
}
],
"family": "Malle",
"given": "Oliver",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute of Public Health, College of Medicine and Health Sciences United Arab Emirates University Al Ain United Arab Emirates"
}
],
"family": "Oulhaj",
"given": "Abderrahim",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "4<sup>th</sup> Medical Division with Infectiology SMZ Süd – KFJ‐Hospital Vienna Vienna Austria"
}
],
"family": "Pawelka",
"given": "Erich",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "3rd Department and Karl Landsteiner Institute for Metabolic Diseases and Nephrology, Clinic Hietzing Vienna Health Care Group Vienna Austria"
}
],
"family": "Peric",
"given": "Slobodan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department for Internal Medicine I Medical University Innsbruck Innsbruck Austria"
}
],
"family": "Ress",
"given": "Claudia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Division for Cardiology Medical University Graz Graz Austria"
}
],
"family": "Sourij",
"given": "Caren",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department for Internal Medicine I Paracelsus Medical University Salzburg Austria"
}
],
"family": "Stechemesser",
"given": "Lars",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Division for Internal Medicine Hospital Melk Melk Austria"
}
],
"family": "Stingl",
"given": "Harald",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "3rd Department and Karl Landsteiner Institute for Metabolic Diseases and Nephrology, Clinic Hietzing Vienna Health Care Group Vienna Austria"
}
],
"family": "Stulnig",
"given": "Thomas",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7566-2047",
"affiliation": [
{
"name": "Clinical Division for Endocrinology and Diabetology Medical University Graz Graz Austria"
}
],
"authenticated-orcid": false,
"family": "Tripolt",
"given": "Norbert",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Division for Internal Medicine Hospital Melk Melk Austria"
}
],
"family": "Wagner",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Division for Endocrinology and Diabetology and Metabolic Diseases AKH Vienna Vienna Austria"
}
],
"family": "Wolf",
"given": "Peter",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "3rd Department and Karl Landsteiner Institute for Metabolic Diseases and Nephrology, Clinic Hietzing Vienna Health Care Group Vienna Austria"
}
],
"family": "Zitterl",
"given": "Andreas",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department for Internal Medicine I Medical University Innsbruck Innsbruck Austria"
}
],
"family": "Kaser",
"given": "Susanne",
"sequence": "additional"
},
{
"affiliation": [],
"name": "for the COVID‐19 in diabetes in Austria study group",
"sequence": "additional"
}
],
"container-title": "Diabetes, Obesity and Metabolism",
"container-title-short": "Diabetes Obesity Metabolism",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"dom-pubs.onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2020,
11,
17
]
],
"date-time": "2020-11-17T07:42:11Z",
"timestamp": 1605598931000
},
"deposited": {
"date-parts": [
[
2023,
9,
2
]
],
"date-time": "2023-09-02T05:31:15Z",
"timestamp": 1693632675000
},
"indexed": {
"date-parts": [
[
2023,
9,
3
]
],
"date-time": "2023-09-03T11:16:26Z",
"timestamp": 1693739786808
},
"is-referenced-by-count": 39,
"issue": "2",
"issued": {
"date-parts": [
[
2020,
12,
4
]
]
},
"journal-issue": {
"issue": "2",
"published-print": {
"date-parts": [
[
2021,
2
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
12,
4
]
],
"date-time": "2020-12-04T00:00:00Z",
"timestamp": 1607040000000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1111/dom.14256",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/full-xml/10.1111/dom.14256",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1111/dom.14256",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"page": "589-598",
"prefix": "10.1111",
"published": {
"date-parts": [
[
2020,
12,
4
]
]
},
"published-online": {
"date-parts": [
[
2020,
12,
4
]
]
},
"published-print": {
"date-parts": [
[
2021,
2
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.1016/j.ijsu.2020.05.018",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_2_1"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_3_1"
},
{
"DOI": "10.1056/NEJMoa2002032",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_4_1"
},
{
"DOI": "10.1001/jama.2020.6775",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_5_1"
},
{
"DOI": "10.1001/jama.2020.5394",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_6_1"
},
{
"DOI": "10.1001/jama.2020.2648",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_7_1"
},
{
"DOI": "10.2337/dc20-0598",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_8_1"
},
{
"DOI": "10.1186/s13054-020-03139-3",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_9_1"
},
{
"DOI": "10.1016/S2213-8587(15)00379-4",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_10_1"
},
{
"DOI": "10.1056/NEJM199912163412507",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_11_1"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_12_1"
},
{
"DOI": "10.1007/s00508-019-1450-4",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_13_1"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_14_1"
},
{
"DOI": "10.2337/dc20-1380",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_15_1"
},
{
"DOI": "10.1016/j.ijsu.2020.08.048",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_16_1"
},
{
"DOI": "10.1007/s00125-020-05164-x",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_17_1"
},
{
"DOI": "10.2337/dc20-0660",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_18_1"
},
{
"DOI": "10.1016/S2213-8587(20)30272-2",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_19_1"
}
],
"reference-count": 18,
"references-count": 18,
"relation": {},
"resource": {
"primary": {
"URL": "https://dom-pubs.pericles-prod.literatumonline.com/doi/10.1111/dom.14256"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology",
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": "COVID‐19 fatality prediction in people with diabetes and prediabetes using a simple score upon hospital admission",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy",
"volume": "23"
}
