Assessing the Effect of Selective Serotonin Reuptake Inhibitors in the Prevention of Post-Acute Sequelae of COVID-19
et al., medRxiv, doi:10.1101/2022.11.09.22282142, Nov 2022
30th treatment shown to reduce risk in
November 2021, now with p = 0.00014 from 21 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
N3C retrospective 17,933 COVID-19 patients in the USA, showing lower risk of PASC for SSRIs with or without S1R agonist activity.
|
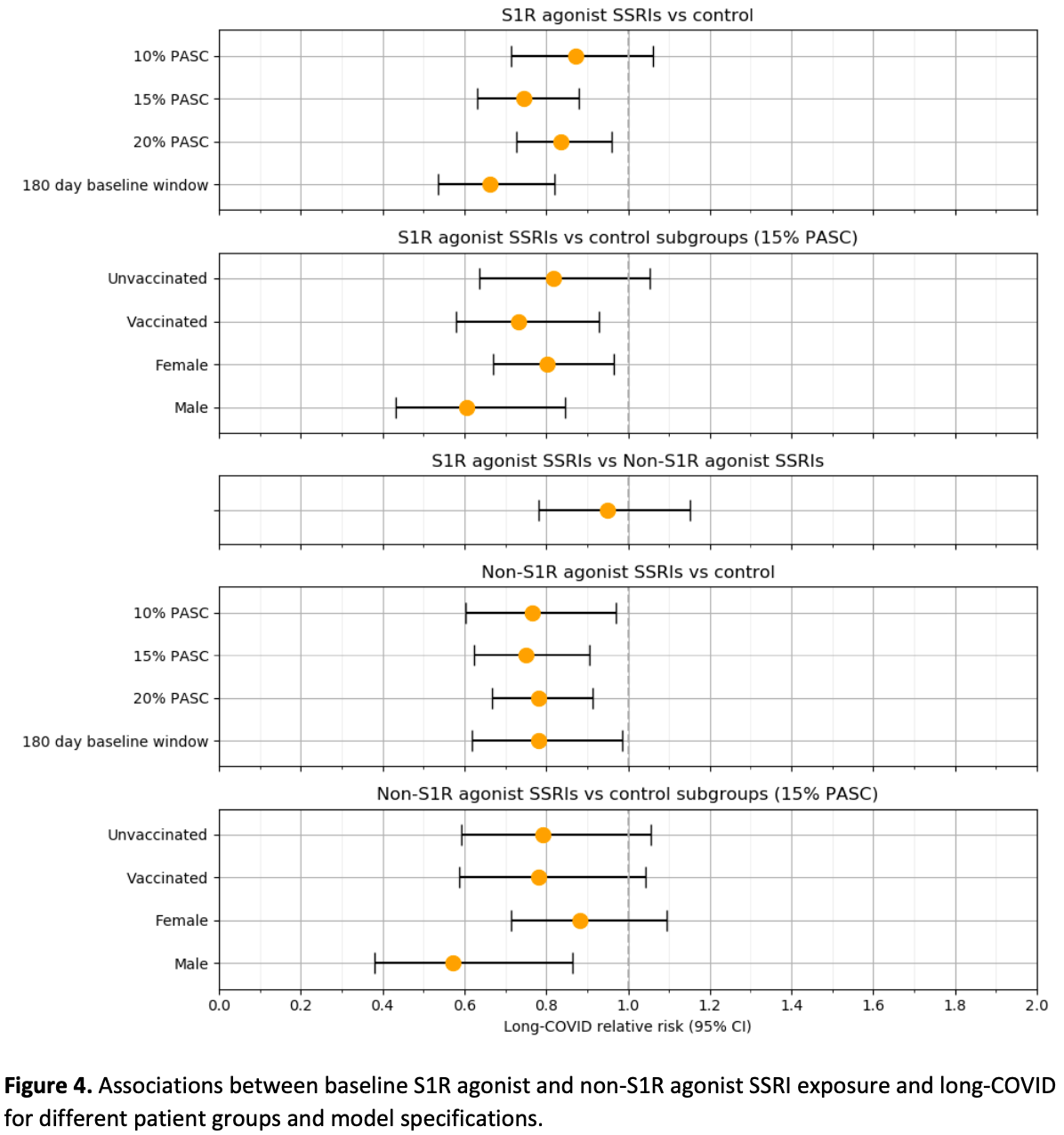
risk of long COVID, 26.0% lower, RR 0.74, p < 0.001, treatment 2,021, control 14,584, S1R agonist SSRI.
|
|
risk of long COVID, 25.0% lower, RR 0.75, p = 0.003, treatment 1,328, control 14,584, non-S1R agonist SSRI.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Sidky et al., 10 Nov 2022, retrospective, multiple countries, preprint, 8 authors, study period 1 October, 2021 - 7 April, 2022.
Contact: hythem.sidky@nih.gov, david.sahner@nih.gov.
Assessing the Effect of Selective Serotonin Reuptake Inhibitors in the Prevention of Post-Acute Sequelae of COVID-19
doi:10.1101/2022.11.09.22282142
Findings: In this retrospective study leveraging real-world clinical data that included 17 933 patients, a 28% reduction in risk of PASC was observed for S1R agonist SSRIs and a 25% reduction in risk of PASC was observed for non-S1R agonist SSRIs, both versus controls, using a computable phenotype to define PASC. Meaning: SSRIs may play a role in managing the long term disease burden of COVID-19. Future prospective studies are warranted to confirm these findings and evaluate potential mechanisms of action.
Authors' contributions Authorship was determined using ICMJE recommendations. The authors hereby declare no conflicting interests pertaining to the material in this manuscript.
References
Bramante, Randomized Trial of Metformin, Ivermectin, and Fluvoxamine for Covid-19, N. Engl. J. Med
Brunoni, Cytokines plasma levels during antidepressant treatment with sertraline and transcranial direct current stimulation (tDCS): results from a factorial, randomized, controlled trial, Psychopharmacology (Berl.)
Canas, Profiling post-COVID syndrome across different variants of SARS-CoV-2, doi:10.1101/2022.07.28.22278159
Chaplin, Summary of joint guideline on the management of long COVID, Prescriber
Chertow, SARS-CoV-2 infection and persistence throughout the human body and brain, doi:10.21203/rs.3.rs-1139035/v1
Dahl, The plasma levels of various cytokines are increased during ongoing depression and are reduced to normal levels after recovery, Psychoneuroendocrinology
Di Rosso, Palumbo, Genaro, Immunomodulatory effects of fluoxetine: A new potential pharmacological action for a classic antidepressant drug?, Pharmacol. Res
Gobin, Van Steendam, Denys, Deforce, Selective serotonin reuptake inhibitors as a novel class of immunosuppressants, Int. Immunopharmacol
Hannestad, Dellagioia, Bloch, The effect of antidepressant medication treatment on serum levels of inflammatory cytokines: a meta-analysis, Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol
Hashimoto, Repurposing of CNS drugs to treat COVID-19 infection: targeting the sigma-1 receptor, Eur. Arch. Psychiatry Clin. Neurosci
Hoertel, Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study, Mol. Psychiatry
Huang, COVID Symptoms, Symptom Clusters, and Predictors for Becoming a Long-Hauler: Looking for Clarity in the Haze of the Pandemic, doi:10.1101/2021.03.03.21252086
Jacobs, Persistent SARS-2 infections contribute to long COVID-19, Med. Hypotheses
Kell, Laubscher, Pretorius, A central role for amyloid fibrin microclots in long COVID/PASC: origins and therapeutic implications, Biochem. J
Komaroff, Lipkin, Insights from myalgic encephalomyelitis/chronic fatigue syndrome may help unravel the pathogenesis of postacute COVID-19 syndrome, Trends Mol. Med
Kostadinov, Study on anti-inflammatory and immunomodulatory effects of fluoxetine in rat models of inflammation, Eur. J. Inflamm
Kuodi, Association between vaccination status and reported incidence of post-acute COVID-19 symptoms in Israel: a cross-sectional study of patients tested between March, doi:10.1101/2022.01.05.22268800
Lenze, Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients With Symptomatic COVID-19: A Randomized Clinical Trial, JAMA
Leung, COVID-19 in an immunocompromised host: persistent shedding of viable SARS-CoV-2 and emergence of multiple mutations: a case report, Int. J. Infect. Dis
Mahase, Covid-19: One in eight adults develops long covid symptoms, study suggests, BMJ
Michelen, Characterising long COVID: a living systematic review, BMJ Glob. Health
Montazersaheb, COVID-19 infection: an overview on cytokine storm and related interventions, Virol. J
Müller, Müller, Psychotropic drugs: Therapeutic perspectives against Covid-19, Psychopharmakotherapie
Nalbandian, Post-acute COVID-19 syndrome, Nat. Med
Oskotsky, Mortality Risk Among Patients With COVID-19 Prescribed Selective Serotonin Reuptake Inhibitor Antidepressants, JAMA Netw. Open
Patterson, Immune-Based Prediction of COVID-19 Severity and Chronicity Decoded Using Machine Learning, Front. Immunol
Paul, Lemle, Komaroff, Snyder, Redox imbalance links COVID-19 and myalgic encephalomyelitis/chronic fatigue syndrome, Proc. Natl. Acad. Sci
Peluso, Markers of Immune Activation and Inflammation in Individuals With Postacute Sequelae of Severe Acute Respiratory Syndrome Coronavirus 2 Infection, J. Infect. Dis
Pfaff, Identifying who has long COVID in the USA: a machine learning approach using N3C data, Lancet Digit. Health
Reis, Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial, Lancet Glob. Health
Rosen, Modulation of the sigma-1 receptor-IRE1 pathway is beneficial in preclinical models of inflammation and sepsis, Sci. Transl. Med
Simon, Luginbuhl, Parker, Reduced Incidence of Long-COVID Symptoms Related to Administration of COVID-19 Vaccines Both Before COVID-19 Diagnosis and Up to 12 Weeks After, doi:10.1101/2021.11.17.21263608
Song, Halbreich, Han, Leonard, Luo, Imbalance between Pro-and Antiinflammatory Cytokines, and between Th1 and Th2 Cytokines in Depressed Patients: The Effect of Electroacupuncture or Fluoxetine Treatment, Pharmacopsychiatry
Strawbridge, Inflammation and clinical response to treatment in depression: A metaanalysis, Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol
Su, Multiple early factors anticipate post-acute COVID-19 sequelae, Cell
Swank, Senussi, Alter, Walt, Persistent circulating SARS-CoV-2 spike is associated with post-acute COVID-19 sequelae, doi:10.1101/2022.06.14.22276401
Szałach, Lisowska, Cubała, The Influence of Antidepressants on the Immune System, Arch. Immunol. Ther. Exp. (Warsz.)
Taler, Gil-Ad, Korob, Weizman, The immunomodulatory effect of the antidepressant sertraline in an experimental autoimmune encephalomyelitis mouse model of multiple sclerosis, Neuroimmunomodulation
Taler, Immunomodulatory effect of selective serotonin reuptake inhibitors (SSRIs) on human T lymphocyte function and gene expression, Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol
Taquet, Incidence, co-occurrence, and evolution of long-COVID features: A 6-month retrospective cohort study of 273,618 survivors of COVID-19, PLOS Med
Vijayakumar, Immuno-proteomic profiling reveals aberrant immune cell regulation in the airways of individuals with ongoing post-COVID-19 respiratory disease, Immunity
We Acknowledge, Pfaff, Fessel, Adam, Wilcox et al., Authorship was determined using ICMJE recommendations
Wood, Hall, Tate, Role of mitochondria, oxidative stress and the response to antioxidants in myalgic encephalomyelitis/chronic fatigue syndrome: A possible approach to SARS-CoV-2 'long-haulers'?, Chronic Dis. Transl. Med
Zhang, Prevalence and Persistent Shedding of Fecal SARS-CoV-2 RNA in Patients With COVID-19 Infection: A Systematic Review and Meta-analysis, Clin. Transl. Gastroenterol
Zhang, Reverse-transcribed SARS-CoV-2 RNA can integrate into the genome of cultured for use under a CC0 license. human cells and can be expressed in patient-derived tissues, Proc. Natl. Acad. Sci. U. S. A
DOI record:
{
"DOI": "10.1101/2022.11.09.22282142",
"URL": "http://dx.doi.org/10.1101/2022.11.09.22282142",
"abstract": "<jats:p>Importance: Post-acute sequelae of COVID-19 (PASC) produce significant morbidity, prompting evaluation of interventions that might lower risk. Selective serotonin reuptake inhibitors (SSRIs) potentially could modulate risk of PASC via their central hypothesized immunomodulatory, and/or antiplatelet properties and therefore have been hypothesized to be of potential benefit in patients with PASC, although clinical data are lacking. Objectives: The main objective was to evaluate whether SSRIs with agonist activity at the sigma-1 receptor lower the risk of PASC, since agonism at this receptor may serve as a mechanism by which SSRIs attenuate an inflammatory response. A secondary objective was to determine whether potential benefit could be traced to sigma-1 agonism by evaluating the risk of PASC among recipients of SSRIs that are not S1R agonists. Design: Retrospective study leveraging real-world clinical data within the National COVID Cohort Collaborative (N3C), a large centralized multi-institutional de-identified EHR database. Presumed PASC was defined based on a computable PASC phenotype trained on the U09.9 ICD-10 diagnosis code to more comprehensively identify patients likely to have the condition, since the ICD code has come into wide-spread use only recently. Setting: Population-based study at US medical centers. Participants: Adults (≥ 18 years of age) with a confirmed COVID-19 diagnosis date between October 1, 2021 and April 7, 2022 and at least one follow up visit 45 days post-diagnosis. Of the 17 933 patients identified, 2021 were exposed at baseline to a S1R agonist SSRI, 1328 to a non-S1R agonist SSRI, and 14 584 to neither. Exposures: Exposure at baseline (at or prior to COVID-19 diagnosis) to an SSRI with documented or presumed agonist activity at the S1R (fluvoxamine, fluoxetine, escitalopram, or citalopram), an SSRI without agonist activity at S1R (sertraline, an antagonist, or paroxetine, which does not appreciably bind to the S1R), or none of these agents. Main Outcome and Measurement: Development of PASC based on a previously validated XGBoost-trained algorithm. Using inverse probability weighting and Poisson regression, relative risk (RR) of PASC was assessed. Results: A 26% reduction in the RR of PASC (0.74 [95% CI, 0.63-0.88]; P = 5 x 10-4) was seen among patients who received an S1R agonist SSRI compared to SSRI unexposed patients and a 25% reduction in the RR of PASC was seen among those receiving an SSRI without S1R agonist activity (0.75 [95% CI, 0.62 - 0.90]; P = 0.003) compared to SSRI unexposed patients. Conclusions and Relevance: SSRIs with and without reported agonist activity at the S1R were associated with a significant decrease in the risk of PASC. Future prospective studies are warranted.</jats:p>",
"accepted": {
"date-parts": [
[
2022,
11,
10
]
]
},
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3532-4809",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sidky",
"given": "Hythem",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-4616-1171",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sahner",
"given": "David K",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2031-9209",
"affiliation": [],
"authenticated-orcid": false,
"family": "Girvin",
"given": "Andrew T",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8423-6464",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hotaling",
"given": "Nathan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Michael",
"given": "Sam G",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kurilla",
"given": "Michael G",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gersing",
"given": "Ken",
"sequence": "additional"
},
{
"affiliation": [],
"name": "The N3C consortium",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
11,
10
]
],
"date-time": "2022-11-10T23:20:15Z",
"timestamp": 1668122415000
},
"deposited": {
"date-parts": [
[
2022,
11,
10
]
],
"date-time": "2022-11-10T23:20:16Z",
"timestamp": 1668122416000
},
"group-title": "Infectious Diseases (except HIV/AIDS)",
"indexed": {
"date-parts": [
[
2022,
11,
11
]
],
"date-time": "2022-11-11T05:52:47Z",
"timestamp": 1668145967576
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
11,
10
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2022.11.09.22282142",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2022,
11,
10
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2022,
11,
10
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://medrxiv.org/lookup/doi/10.1101/2022.11.09.22282142"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Assessing the Effect of Selective Serotonin Reuptake Inhibitors in the Prevention of Post-Acute Sequelae of COVID-19",
"type": "posted-content"
}
