Dysbiosis of gut microbiota in patients with severe COVID‐19
et al., Acute Medicine & Surgery, doi:10.1002/ams2.923, Jan 2024
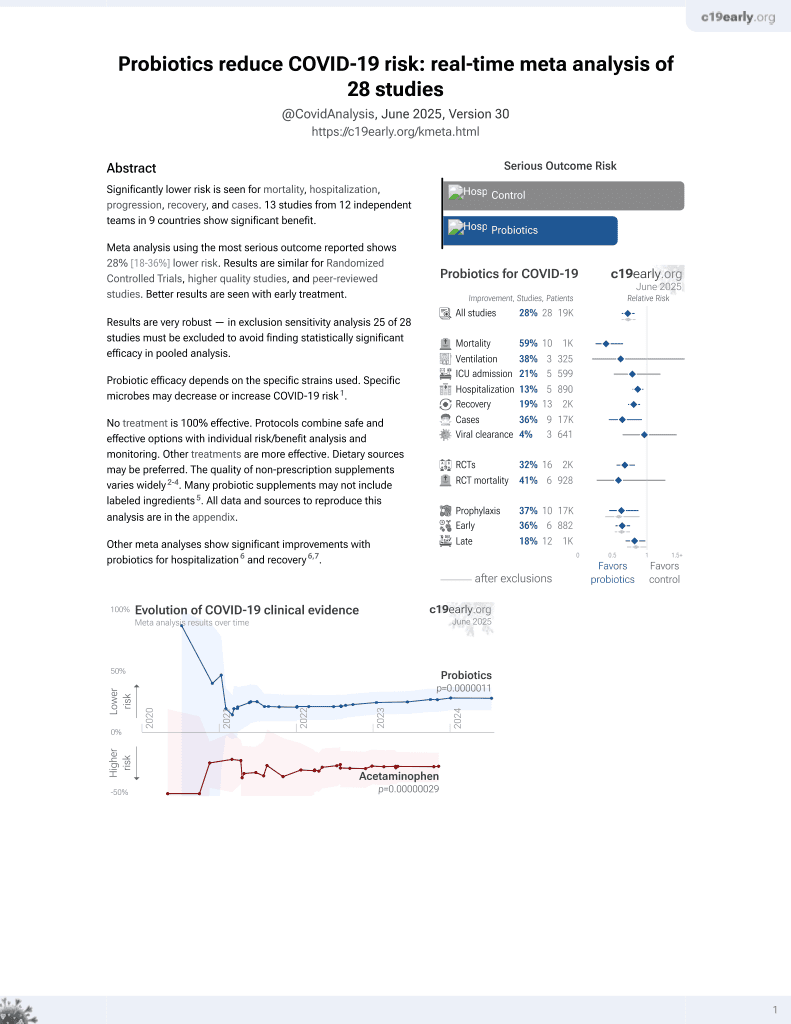
Probiotics for COVID-19
20th treatment shown to reduce risk in
March 2021, now with p = 0.00000044 from 29 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
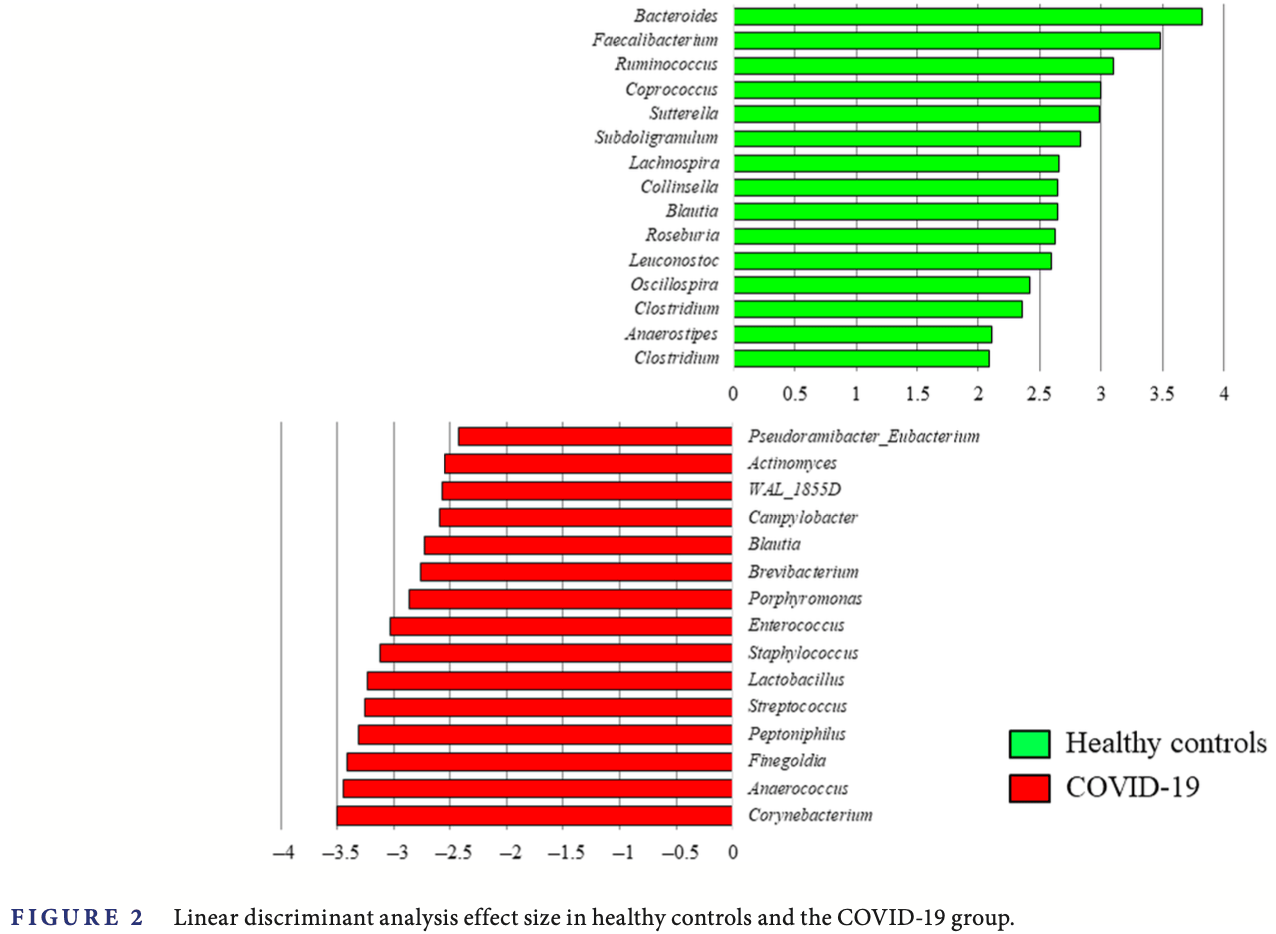
Retrospective 30 mechanically ventilated COVID-19 patients without prior antibiotic use showing dysbiosis of gut microbiota with decreases in commensals like Bacteroides, Faecalibacterium, and Blautia and increases in opportunists like Corynebacterium and Anaerococcus compared to healthy controls. Authors suggest SARS-CoV-2 infection can disrupt gut microbiota, and this dysbiosis could worsen outcomes through gut-lung axis effects. Authors suggest probiotics, prebiotics, and synbiotics as a treatment for COVID-19 to restore gut microbiota and strengthen immune response.
Probiotic efficacy depends on the specific strains used. Specific microbes may decrease or increase COVID-19 risk1.
Shimizu et al., 10 Jan 2024, retrospective, Japan, peer-reviewed, 11 authors, study period November 2020 - May 2021.
Contact: shimiken@hp-emerg.med.osaka-u.ac.jp.
Dysbiosis of gut microbiota in patients with severe COVID‐19
Acute Medicine & Surgery, doi:10.1002/ams2.923
BACKGROU N D The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2/COVID-19) pandemic is an emergency situation throughout the world. COVID-19 has been reported to cause inflammation and cytokine storm and lead to multiple organ dysfunction syndrome. 1 The gut has been a target organ following critical illnesses. 2 Cross talk between the intestinal epithelium, immune system, and commensal bacteria is central to initiating the systemic inflammatory response. The gut-lung axis has been proposed as one of the causes of the exacerbation of disease severity. 3 The human gut microbiota is estimated to contain 10 14 microbes comprising over 1000 different bacterial species that reside in the host's colon. 4 These bacteria have a close connection with human metabolism and homeostasis of the immune system. Dysbiosis, defined as an imbalance in the microbial communities living in or on the body, 5 leads to various diseases such as obesity, metabolic syndrome, cardiovascular diseases, cancer, and autoimmune diseases. In the acute phase of critical care, gut
CONCLUSION In conclusion, the commensal gut microbiota in patients with severe COVID-19 infection was altered, and opportunistic bacteria increased within several days from disease onset.
ACKNOWLEDGMENTS The study was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant Numbers 19H03761 and 22H03174. The authors acknowledge the contributions made by all of the staff in Osaka University Hospital who aided in this research and are involved COVID-19 medical practice.
C ON F L IC T OF I N T E R E S T S TAT E M E N T Dr. Hiroshi Ogura is an Editorial Board member of the AMS Journal and a coauthor of this article. To minimize bias, they were excluded from all editorial decision-making related to the acceptance of this article for publication. Dr. Jun Oda is Editor-in-Chief of the journal and coauthor of this article. They were excluded from the peer-review process and all editorial decisions related to the acceptance and publication of this article. Peer-review was handled independently by Acute Medicine and Surgery editorial office with Dr. Yasuyuki Kuwagata as the Editor to minimize bias.
DATA AVA I L A BI L I T Y S TAT E M E N T The data that support the findings of this study are available from the corresponding author upon reasonable request.
A PPROVA L OF T H E R E SE A RC H PRO T O C OL Approval of the research protocol: This study was approved by the institutional review board of Osaka University Hospital (approval number: 12035).
I N..
References
Batra, Soni, Mathur, Efficacy of probiotics in the prevention of VAP in critically ill ICU patients: an updated systematic review and meta-analysis of randomized control trials, J Intensive Care
Bolyen, Rideout, Dillon, Bokulich, Abnet et al., Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2, Nat Biotechnol
Chowdhury, Adiamah, Kushairi, Varadhan, Krznaric et al., Perioperative probiotics or synbiotics in adults undergoing elective abdominal surgery: a systematic review and meta-analysis of randomized controlled trials, Ann Surg
Clark, Coopersmith, Intestinal crosstalk: a new paradigm for understanding the gut as the "motor" of critical illness, Shock
De Oliveira, Oliveira, Pinzan, De Salis, Cardoso, Microbiota modulation of the gut-lung Axis in COVID-19, Front Immunol
Fajgenbaum, June, Cytokine storm, N Engl J Med
Farsi, Tahvildari, Arbabi, Vazife, Sechi et al., Diagnostic, prognostic, and therapeutic roles of gut microbiota in COVID-19: a comprehensive systematic review, Front Cell Infect Microbiol
Gaibani, ' Amico, Bartoletti, The gut microbiota of critically ill patients with COVID-19, Front Cell Infect Microbiol
Hashimoto, Perlot, Rehman, Trichereau, Ishiguro et al., ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation, Nature
Huang, Inoue, Leone, Dalal, Touw et al., Using corticosteroids to reshape the gut microbiome: implications for inflammatory bowel diseases, Inflamm Bowel Dis
Jenq, Taur, Devlin, Ponce, Goldberg et al., Intestinal Blautia is associated with reduced death from graft-versushost disease, Biol Blood Marrow Transplant
Lankelma, Cranendonk, Belzer, De Vos, De Vos et al., Antibiotic-induced gut microbiota disruption during human endotoxemia: a randomised controlled study, Gut
Leylabadlo, Ghotaslou, Feizabadi, Farajnia, Moaddab et al., The critical role of Faecalibacterium prausnitzii in human health: an overview, Microb Pathog
Lozupone, Hamady, Kelley, Knight, Quantitative and qualitative beta diversity measures lead to different insights into factors that structure microbial communities, Appl Environ Microbiol
Mazzarelli, Giancola, Farina, Marchioni, Rueca et al., 16S rRNA gene sequencing of rectal swab in patients affected by COVID-19, PLoS One
Mitsuyama, Yamakawa, Kayano, Maruyama, Umemura et al., Residual persistence of cytotoxicity lymphocytes and regulatory T cells in patients with severe coronavirus disease 2019 over a 1-year recovery process, Acute Med Surg
Moreira-Rosario, Marques, Pinheiro, Gut microbiota diversity and C-reactive protein are predictors of disease severity in COVID-19 patients, Front Microbiol
Niitsu, Shiroyama, Hirata, Noda, Adachi et al., Cytomegalovirus infection in critically ill patients with COVID-19, J Infect
Ojima, Shimizu, Motooka, Ishihara, Nakamura et al., Gut dysbiosis associated with antibiotics and disease severity and its relation to mortality in critically ill patients, Dig Dis Sci
Petersen, Round, Defining dysbiosis and its influence on host immunity and disease, Cell Microbiol
Qin, Li, Raes, A human gut microbial gene catalogue established by metagenomic sequencing, Nature
Segata, Izard, Waldron, Gevers, Miropolsky et al., Metagenomic biomarker discovery and explanation, Genome Biol
Shimizu, Hibino, Biros, Irisawa, Shimazu, Emergency medicine in Japan: past, present, and future, Int J Emerg Med
Shimizu, Hirata, Kabata, Tokuhira, Koide et al., Ivermectin administration is associated with lower gastrointestinal complications and greater ventilator-free days in ventilated patients with COVID-19: a propensity score analysis, J Infect Chemother
Shimizu, Hirata, Tokuhira, Ueda, Motooka et al., A case of massive refractory diarrhea in a patient with COVID-19, Acute Med Surg
Shimizu, Hirose, Ogura, Efficacy of probiotics in the prevention of diarrhea in ventilated critically ill ICU patients: meta-analysis of randomized control trials, J Intensive Care
Shimizu, Ogura, Goto, Asahara, Nomoto et al., Altered gut flora and environment in patients with severe SIRS, J Trauma
Shimizu, Ogura, Hamasaki, Goto, Tasaki et al., Altered gut flora are associated with septic complications and death in critically ill patients with systemic inflammatory response syndrome, Dig Dis Sci
Thaiss, Zmora, Levy, Elinav, The microbiome and innate immunity, Nature
Whowgotc, Management of C-i: a minimal common outcome measure set for COVID-19 clinical research, Lancet Infect Dis
Wu, Cheng, Jiang, Tang, Ming et al., Altered oral and gut microbiota and its association with SARS-CoV-2 viral load in COVID-19 patients during hospitalization, NPJ Biofilms Microbiomes
Xiao, Tang, Zheng, Liu, Li et al., Evidence for gastrointestinal infection of SARS-CoV-2, Gastroenterology
Yamada, Shimizu, Ogura, Asahara, Nomoto et al., Rapid and sustained long-term decrease of fecal short-chain fatty acids in critically ill patients with systemic inflammatory response syndrome, JPEN J Parenter Enteral Nutr
Zafar, Saier, Jr, Gut bacteroides species in health and disease, Gut Microbes
Zuo, Zhang, Lui, Yeoh, Li et al., Alterations in gut microbiota of patients with COVID-19 during time of hospitalization, Gastroenterology
DOI record:
{
"DOI": "10.1002/ams2.923",
"ISSN": [
"2052-8817",
"2052-8817"
],
"URL": "http://dx.doi.org/10.1002/ams2.923",
"abstract": "<jats:title>Abstract</jats:title><jats:sec><jats:title>Aim</jats:title><jats:p>Altered gut microbiota has been proposed as one of the causes of exacerbation of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2/COVID‐19) from the perspective of the gut–lung axis. We aimed to evaluate gut microbiota in mechanically ventilated patients with COVID‐19 prior to using antibiotics.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>We retrospectively selected for enrollment COVID‐19 patients who required mechanical ventilation on admission but who had not used antibiotics before admission to observe the influence of SARS‐Cov‐2 on gut microbiota. Fecal samples were collected serially on admission and were evaluated by 16S rRNA gene deep sequencing.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>The phylum of Bacteroidetes decreased, and those of Firmicutes and Actinobacteria increased in COVID‐19 patients compared with those in healthy controls (<jats:italic>p</jats:italic> < 0.001). The main commensals of <jats:italic>Bacteroides</jats:italic>, <jats:italic>Faecalibacterium</jats:italic>, and <jats:italic>Blautia</jats:italic> at the genus level were significantly decreased in the COVID‐19 patients, and opportunistic bacteria including <jats:italic>Corynebacterium</jats:italic>, <jats:italic>Anaerococcus</jats:italic>, <jats:italic>Finegoldia Peptoniphilus</jats:italic>, <jats:italic>Actinomyces</jats:italic>, and <jats:italic>Enterococcus</jats:italic> were increased (<jats:italic>p</jats:italic> < 0.001). α‐Diversity and β‐diversity in COVID‐19 patients significantly changed compared with those in the healthy controls.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>The commensal gut microbiota were altered, and opportunistic bacteria increased in patients with severe COVID‐19 who required mechanical ventilation on admission.</jats:p></jats:sec>",
"alternative-id": [
"10.1002/ams2.923"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2023-04-04"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2023-12-28"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2024-01-10"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-0631-9365",
"affiliation": [
{
"name": "Department of Traumatology and Acute Critical Medicine Osaka University Graduate School of Medicine Suita Japan"
}
],
"authenticated-orcid": false,
"family": "Shimizu",
"given": "Kentaro",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Respiratory Medicine and Clinical Immunology, Graduate School of Medicine Osaka University Osaka Japan"
}
],
"family": "Hirata",
"given": "Haruhiko",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Intensive Care Unit, Osaka University Hospital Osaka University Suita Japan"
}
],
"family": "Tokuhira",
"given": "Natsuko",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Infection Metagenomics, Research Institute for Microbial Diseases Osaka University Suita Japan"
}
],
"family": "Motooka",
"given": "Daisuke",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Infection Metagenomics, Research Institute for Microbial Diseases Osaka University Suita Japan"
}
],
"family": "Nakamura",
"given": "Shota",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Laboratory for Clinical Investigation, Osaka University Hospital Osaka University Suita Japan"
}
],
"family": "Ueda",
"given": "Akiko",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Traumatology and Acute Critical Medicine Osaka University Graduate School of Medicine Suita Japan"
}
],
"family": "Tachino",
"given": "Jotaro",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Intensive Care Unit, Osaka University Hospital Osaka University Suita Japan"
}
],
"family": "Koide",
"given": "Moe",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Intensive Care Unit, Osaka University Hospital Osaka University Suita Japan"
}
],
"family": "Uchiyama",
"given": "Akinori",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Traumatology and Acute Critical Medicine Osaka University Graduate School of Medicine Suita Japan"
}
],
"family": "Ogura",
"given": "Hiroshi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Traumatology and Acute Critical Medicine Osaka University Graduate School of Medicine Suita Japan"
}
],
"family": "Oda",
"given": "Jun",
"sequence": "additional"
}
],
"container-title": "Acute Medicine & Surgery",
"container-title-short": "Acute Medicine & Surgery",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2024,
1,
11
]
],
"date-time": "2024-01-11T04:46:19Z",
"timestamp": 1704948379000
},
"deposited": {
"date-parts": [
[
2024,
1,
11
]
],
"date-time": "2024-01-11T04:46:25Z",
"timestamp": 1704948385000
},
"funder": [
{
"DOI": "10.13039/501100001691",
"award": [
"19H03761",
"22H03174"
],
"doi-asserted-by": "publisher",
"name": "Japan Society for the Promotion of Science"
}
],
"indexed": {
"date-parts": [
[
2024,
1,
12
]
],
"date-time": "2024-01-12T00:20:22Z",
"timestamp": 1705018822588
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
1
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2024,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "vor",
"delay-in-days": 9,
"start": {
"date-parts": [
[
2024,
1,
10
]
],
"date-time": "2024-01-10T00:00:00Z",
"timestamp": 1704844800000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/ams2.923",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"prefix": "10.1002",
"published": {
"date-parts": [
[
2024,
1
]
]
},
"published-online": {
"date-parts": [
[
2024,
1,
10
]
]
},
"published-print": {
"date-parts": [
[
2024,
1
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.1056/NEJMra2026131",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_2_1"
},
{
"DOI": "10.1097/shk.0b013e31805569df",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_3_1"
},
{
"DOI": "10.3389/fimmu.2021.635471",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_4_1"
},
{
"DOI": "10.1038/nature08821",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_5_1"
},
{
"DOI": "10.1111/cmi.12308",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_6_1"
},
{
"DOI": "10.1007/s10620-010-1418-8",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_7_1"
},
{
"DOI": "10.1007/s10620-021-07000-7",
"article-title": "Gut dysbiosis associated with antibiotics and disease severity and its relation to mortality in critically ill patients",
"author": "Ojima M",
"doi-asserted-by": "crossref",
"first-page": "2420",
"journal-title": "Dig Dis Sci",
"key": "e_1_2_13_8_1",
"volume": "67",
"year": "2021"
},
{
"DOI": "10.1186/s12245-020-00316-7",
"article-title": "Emergency medicine in Japan: past, present, and future",
"author": "Shimizu K",
"doi-asserted-by": "crossref",
"first-page": "2",
"journal-title": "Int J Emerg Med",
"key": "e_1_2_13_9_1",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1038/s41587-019-0209-9",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_10_1"
},
{
"DOI": "10.1186/gb-2011-12-6-r60",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_11_1"
},
{
"DOI": "10.1128/AEM.01996-06",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_12_1"
},
{
"DOI": "10.3389/fcimb.2022.804644",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_13_1"
},
{
"DOI": "10.1136/gutjnl-2016-312132",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_14_1"
},
{
"DOI": "10.1177/0148607114529596",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_15_1"
},
{
"DOI": "10.1038/nature18847",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_16_1"
},
{
"DOI": "10.1097/01.ta.0000197374.99755.fe",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_17_1"
},
{
"DOI": "10.1002/ams2.793",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_18_1"
},
{
"DOI": "10.1080/19490976.2020.1848158",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_19_1"
},
{
"DOI": "10.1016/j.micpath.2020.104344",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_20_1"
},
{
"DOI": "10.1016/j.bbmt.2015.04.016",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_21_1"
},
{
"DOI": "10.1053/j.gastro.2020.05.048",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_22_1"
},
{
"DOI": "10.1097/MIB.0000000000000332",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_23_1"
},
{
"DOI": "10.3389/fcimb.2021.670424",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_24_1"
},
{
"DOI": "10.1038/nature11228",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_25_1"
},
{
"DOI": "10.1038/s41522-021-00232-5",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_26_1"
},
{
"DOI": "10.1053/j.gastro.2020.02.055",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_27_1"
},
{
"DOI": "10.3389/fmicb.2021.705020",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_28_1"
},
{
"DOI": "10.1016/S1473-3099(20)30483-7",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_29_1"
},
{
"DOI": "10.1371/journal.pone.0247041",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_30_1"
},
{
"DOI": "10.1002/ams2.803",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_31_1"
},
{
"DOI": "10.1016/j.jinf.2021.07.004",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_32_1"
},
{
"DOI": "10.1016/j.jiac.2021.12.024",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_33_1"
},
{
"DOI": "10.1186/s40560-021-00567-3",
"article-title": "Efficacy of probiotics in the prevention of diarrhea in ventilated critically ill ICU patients: meta‐analysis of randomized control trials",
"author": "Shimizu K",
"doi-asserted-by": "crossref",
"first-page": "62",
"journal-title": "J Intensive Care",
"key": "e_1_2_13_34_1",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1097/SLA.0000000000003581",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_35_1"
},
{
"DOI": "10.1186/s40560-020-00487-8",
"doi-asserted-by": "publisher",
"key": "e_1_2_13_36_1"
}
],
"reference-count": 35,
"references-count": 35,
"relation": {},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1002/ams2.923"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Industrial and Manufacturing Engineering",
"Materials Science (miscellaneous)",
"Business and International Management"
],
"subtitle": [],
"title": "Dysbiosis of gut microbiota in patients with severe <scp>COVID</scp>‐19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy",
"volume": "11"
}