Aspirin Therapy on Prophylactic Anticoagulation for Patients Hospitalized With COVID-19: A Propensity Score-Matched Cohort Analysis of the HOPE-COVID-19 Registry
et al., Journal of the American Heart Association, doi:10.1161/JAHA.121.024530, Jun 2022
HOPE-COVID-19 PSM retrospective 7,824 patients, comparing prophylactic anticoagulation with and without additional treatment with aspirin in hospitalized patients, showing lower mortality with aspirin treatment.
|
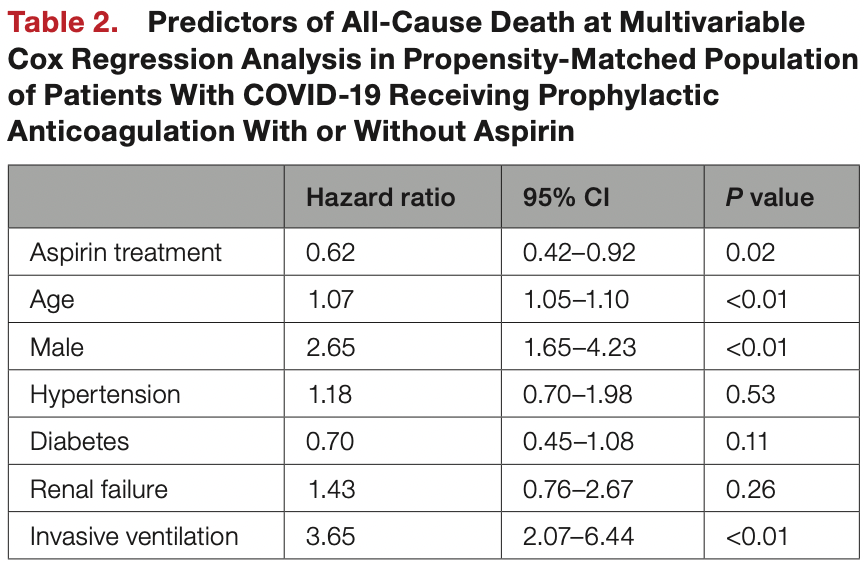
risk of death, 38.0% lower, HR 0.62, p = 0.02, treatment 360, control 2,949.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Santoro et al., 22 Jun 2022, retrospective, propensity score matching, multivariable, multiple countries, peer-reviewed, 31 authors, study period 16 January, 2020 - 30 May, 2020.
Contact: natale.brunetti@unifg.it.
Aspirin Therapy on Prophylactic Anticoagulation for Patients Hospitalized With COVID‐19: A Propensity Score‐Matched Cohort Analysis of the HOPE‐COVID‐19 Registry
Journal of the American Heart Association, doi:10.1161/jaha.121.024530
BACKGROUND: COVID-19 is an infectious illness, featured by an increased risk of thromboembolism. However, no standard antithrombotic therapy is currently recommended for patients hospitalized with COVID-19. The aim of this study was to evaluate safety and efficacy of additional therapy with aspirin over prophylactic anticoagulation (PAC) in patients hospitalized with COVID-19 and its impact on survival.
METHODS AND RESULTS: A total of 8168 patients hospitalized for COVID-19 were enrolled in a multicenter-international prospective registry (HOPE COVID-19). Clinical data and in-hospital complications, including mortality, were recorded. Study population included patients treated with PAC or with PAC and aspirin. A comparison of clinical outcomes between patients treated with PAC versus PAC and aspirin was performed using an adjusted analysis with propensity score matching. Of 7824 patients with complete data, 360 (4.6%) received PAC and aspirin and 2949 (37.6%) PAC. Propensity-score matching yielded 298 patients from each group. In the propensity score-matched population, cumulative incidence of in-hospital mortality was lower in patients treated with PAC and aspirin versus PAC (15% versus 21%, Log Rank P=0.01). At multivariable analysis in propensity matched population of patients with COVID-19, including age, sex, hypertension, diabetes, kidney failure, and invasive ventilation, aspirin treatment was associated with lower risk of in-hospital mortality (hazard ratio [HR], 0.62; [95% CI 0.42-0.92], P=0.018). CONCLUSIONS: Combination PAC and aspirin was associated with lower mortality risk among patients hospitalized with COVID-19 in a propensity score matched population compared to PAC alone.
ARTICLE INFORMATION Received March 9, 2022; accepted April 28, 2022.
Affiliations Sources of Funding This work was supported by an unconditioned grant (Fundacion Interhospitalaria para la Investigacion Cardiovascular [FIC] Madrid, Spain). This nonprofit institution had no role in the study design; in the collection, analysis, interpretation of data; in the writing of the report; nor in the decision to submit the paper for publication. This paper has been published with the financial support of the Dept. of Medical and Surgical Sciences of the University of Foggia, Foggia, Italy.
Disclosures None.
Supplemental Material Tables S1-S3 SUPPLEMENTAL MATERIAL
References
Alhazzani, Møller, Arabi, Loeb, Gong et al., Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19), Crit Care Med, doi:10.1097/CCM.0000000000004363
Buijsers, Yanginlar, Maciej-Hulme, De Mast, Der Vlag, Beneficial non-anticoagulant mechanisms underlying heparin treatment of COVID-19 patients, EBioMedicine, doi:10.1016/j.ebiom.2020.102969
Carlo, None
Clinico, Carlos, None
Florêncio, Tenório, Júnior, Lima, Aspirin with or without statin in the treatment of endotheliitis, thrombosis, and ischemia in coronavirus disease, Rev Soc Bras Med Trop, doi:10.1590/0037-8682-0472-2020
Goligher, Bradbury, Mcverry, Lawler, Berger et al., REMAP-CAP Investigators; ACTIV-4a Investigators; ATTACC Investigators. Therapeutic anticoagulation in critically ill patients with Covid-19, N Engl J Med, doi:10.1056/NEJMoa2103417
Henn, Slupsky, Gräfe, Anagnostopoulos, Förster et al., CD40 ligand on activated platelets triggers an inflammatory reaction of endothelial cells, Nature, doi:10.1038/35393
Imib-Arrixaca, Cibercv ; (f, Cardiology and Arrhythmology Clinic, Ospedali Riuniti "Umberto I -Lancisi -Salesi
Infermi Hospital, None
Kopp, Ghosh, Inhibition of NF-kappa B by sodium salicylate and aspirin, Science, doi:10.1126/science.8052854
Lawler, Goligher, Berger, Neal, Mcverry et al., The ATTACC, ACTIV-4a, and REMAP-CAP Investigators* Therapeutic anticoagulation in non-critically ill patients with Covid-19, N Engl J Med, doi:10.1056/NEJMoa2105911
Lopes, De Barros E Silva, Furtado, Macedo, Bronhara et al., Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated Ddimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial, Lancet, doi:10.1016/S0140-6736(21)01203-4
Malas, Naazie, Elsayed, Mathlouthi, Marmor et al., Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: a systematic review and metaanalysis, EClinicalMedicine, doi:10.1016/j.eclinm.2020.100639
Mazloomzadeh, Khaleghparast, Ghadrdoost, Mousavizadeh, Baay et al., Effect of intermediate-dose vs standard-dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID-19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial, JAMA, doi:10.1001/jama.2021.4152
Mazzeffi, Chow, Tanaka, COVID-19 associated hypercoagulability: manifestations, mechanisms, and management, Shock, doi:10.1097/SHK.0000000000001660
Mei, Luo, Hu, Thrombocytopenia and thrombosis in hospitalized patients with COVID-19, J Hematol Oncol, doi:10.1186/s13045-020-01003-z
Núñez-Gil, Estrada, Fernández-Pérez, Feltes, Vedia et al., Health Outcome Predictive Evaluation for COVID 19 international registry (HOPE COVID-19), rationale and design, Contemp Clin Trials Commun, doi:10.1016/j.conctc.2020.100654
Pavoni, Gianesello, Pazzi, Stera, Meconi et al., Venous thromboembolism and bleeding in critically ill COVID-19 patients treated with higher than standard low molecular weight heparin doses and aspirin: a call to action, Thromb Res, doi:10.1016/j.thromres.2020.09.013
Pellegrini, Kawakami, Guagliumi, Sakamoto, Kawai et al., Microthrombi as a major cause of cardiac injury in COVID-19: a pathologic study, Circulation, doi:10.1161/CIRCULATIONAHA.120.051828
Rapkiewicz, Mai, Carsons, Pittaluga, Kleiner et al., Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series, EClinicalMedicine, doi:10.1016/j.eclinm.2020.100434
Santoro, Nuñez-Gil, Vitale, Viana-Llamas, Martinez et al., Antiplatelet therapy and outcome in COVID-19: the Health Outcome Predictive Evaluation Registry, Heart, doi:10.1136/heartjnl-2021-319552
Santoro, Núñez-Gil, Viana-Llamas, Eid, Romero et al., Anticoagulation therapy in patients with coronavirus disease 2019: results from a multicenter international prospective registry (Health Outcome Predictive Evaluation for Corona Virus Disease 2019 [HOPE-COVID19]), Crit Care Med, doi:10.1161/CIRCULATIONAHA.110.009449
Xie, Xu, Bowe, Al-Aly, Long-term cardiovascular outcomes of COVID-19, Nat Med, doi:10.1038/s41591-022-01689-3
Zhang, Penninger, Li, Zhong, Slutsky, Angiotensinconverting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target, Intensive Care Med, doi:10.1007/s00134-020-05985-9
Zhu, Zhang, Li, Yang, Song et al., A novel coronavirus from patients with pneumonia in China, 2019, N Engl J Med, doi:10.1056/NEJMoa2001017
DOI record:
{
"DOI": "10.1161/jaha.121.024530",
"ISSN": [
"2047-9980"
],
"URL": "http://dx.doi.org/10.1161/JAHA.121.024530",
"abstract": "<jats:sec xml:lang=\"en\">\n <jats:title>Background</jats:title>\n <jats:p xml:lang=\"en\">COVID‐19 is an infectious illness, featured by an increased risk of thromboembolism. However, no standard antithrombotic therapy is currently recommended for patients hospitalized with COVID‐19. The aim of this study was to evaluate safety and efficacy of additional therapy with aspirin over prophylactic anticoagulation (PAC) in patients hospitalized with COVID‐19 and its impact on survival.</jats:p>\n </jats:sec>\n <jats:sec xml:lang=\"en\">\n <jats:title>Methods and Results</jats:title>\n <jats:p xml:lang=\"en\">\n A total of 8168 patients hospitalized for COVID‐19 were enrolled in a multicenter‐international prospective registry (HOPE COVID‐19). Clinical data and in‐hospital complications, including mortality, were recorded. Study population included patients treated with PAC or with PAC and aspirin. A comparison of clinical outcomes between patients treated with PAC versus PAC and aspirin was performed using an adjusted analysis with propensity score matching. Of 7824 patients with complete data, 360 (4.6%) received PAC and aspirin and 2949 (37.6%) PAC. Propensity‐score matching yielded 298 patients from each group. In the propensity score‐matched population, cumulative incidence of in‐hospital mortality was lower in patients treated with PAC and aspirin versus PAC (15% versus 21%, Log Rank\n <jats:italic>P</jats:italic>\n =0.01). At multivariable analysis in propensity matched population of patients with COVID‐19, including age, sex, hypertension, diabetes, kidney failure, and invasive ventilation, aspirin treatment was associated with lower risk of in‐hospital mortality (hazard ratio [HR], 0.62; [95% CI 0.42–0.92],\n <jats:italic>P</jats:italic>\n =0.018).\n </jats:p>\n </jats:sec>\n <jats:sec xml:lang=\"en\">\n <jats:title>Conclusions</jats:title>\n <jats:p xml:lang=\"en\">Combination PAC and aspirin was associated with lower mortality risk among patients hospitalized with COVID‐19 in a propensity score matched population compared to PAC alone.</jats:p>\n </jats:sec>",
"alternative-id": [
"10.1161/JAHA.121.024530"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-9909-6513",
"affiliation": [
{
"name": "Department of Medical and Surgical Sciences University of Foggia Italy"
}
],
"authenticated-orcid": false,
"family": "Santoro",
"given": "Francesco",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Hospital Clinico San Carlos Madrid Spain"
}
],
"family": "Núñez‐Gil",
"given": "Ivan J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medical and Surgical Sciences University of Foggia Italy"
}
],
"family": "Vitale",
"given": "Enrica",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9523-1631",
"affiliation": [
{
"name": "Hospital Universitario Guadalajara Guadalajara Spain"
}
],
"authenticated-orcid": false,
"family": "Viana‐Llamas",
"given": "María C.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3777-2050",
"affiliation": [
{
"name": "Universidad Europea Madrid Spain"
}
],
"authenticated-orcid": false,
"family": "Romero",
"given": "Rodolfo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7684-868X",
"affiliation": [
{
"name": "Hospital Universitario de la Paz Madrid Spain"
}
],
"authenticated-orcid": false,
"family": "Maroun Eid",
"given": "Charbel",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Cardiology Hospital Nuestra Señora de America Madrid Spain"
}
],
"family": "Feltes Guzman",
"given": "Gisela",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6454-7644",
"affiliation": [
{
"name": "Servicio de Cardiología Hospital Universitario Virgen de la VictoriaIBIMA Málaga Spain"
}
],
"authenticated-orcid": false,
"family": "Becerra‐Muñoz",
"given": "Victor Manuel",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Universitario Severo Ochoa Leganés Spain"
}
],
"family": "Fernández Rozas",
"given": "Inmaculada",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6911-7480",
"affiliation": [
{
"name": "Department of Cardiology Hospital Clinico Universitario de Valladolid Spain"
}
],
"authenticated-orcid": false,
"family": "Uribarri",
"given": "Aitor",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1063-9898",
"affiliation": [
{
"name": "Institute of Cardiology and Cardiovascular Surgery Havana Cuba"
}
],
"authenticated-orcid": false,
"family": "Alfonso‐Rodriguez",
"given": "Emilio",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Puerta de Hierro de Majadahonda Majadahonda, Madrid Spain"
}
],
"family": "García Aguado",
"given": "Marcos",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The Second Affiliated Hospital of Southern University of Science and Technology Shenzhen China"
}
],
"family": "Huang",
"given": "Jia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4208-1681",
"affiliation": [
{
"name": "Hospital General del Norte de Guayaquil IESS, Los Ceibos Guayaquil Ecuador"
}
],
"authenticated-orcid": false,
"family": "Castro Mejía",
"given": "Alex Fernando",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Emergency Medicine Hospital de Manises Valencia Spain"
}
],
"family": "Garcia Prieto",
"given": "Juan Fortunato",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4473-5864",
"affiliation": [
{
"name": "IMAS Foundation Madrid Spain"
}
],
"authenticated-orcid": false,
"family": "Elola",
"given": "Javier",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Cardiology Sant'Andrea Hospital Vercelli Italy"
}
],
"family": "Ugo",
"given": "Fabrizio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1260-7534",
"affiliation": [
{
"name": "San Luigi Gonzaga University Hospital Orbassano Italy"
},
{
"name": "Rivoli Infermi Hospital Rivoli Italy"
}
],
"authenticated-orcid": false,
"family": "Cerrato",
"given": "Enrico",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Lung Disease Hospital Clinico Valencia Spain"
}
],
"family": "Signes‐Costa",
"given": "Jaime",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6462-4715",
"affiliation": [
{
"name": "University Hospital Alvaro Cunqueiro Vigo Spain"
}
],
"authenticated-orcid": false,
"family": "Raposeiras Roubin",
"given": "Sergio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3338-607X",
"affiliation": [
{
"name": "Department of Cardiology Hospital De Especialidades De Las Fuerzas Armadas Quito Ecuador"
}
],
"authenticated-orcid": false,
"family": "Jativa Mendez",
"given": "Jorge Luis",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Cardiology Hospital Universitario Principe de Asturias Madrid Spain"
}
],
"family": "Espejo Paeres",
"given": "Carolina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Cardiology Hospital Universitario Juan Ramon Jimenez Huelva Spain"
}
],
"family": "López Masjuan",
"given": "Alvaro",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "IMIB‐Arrixaca CIBERCV Hospital Clínico Universitario Virgen de la ArrixacaUniversidad de Murcia Spain"
}
],
"family": "Marin",
"given": "Francisco",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5394-1312",
"affiliation": [
{
"name": "Cardiology and Arrhythmology Clinic Ospedali Riuniti \"Umberto I ‐ Lancisi ‐ Salesi\" Università Politecnica delle Marche Ancona Italy"
}
],
"authenticated-orcid": false,
"family": "Guerra",
"given": "Federico",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0139-1045",
"affiliation": [
{
"name": "First Department of Medicine Faculty of Medicine University of Mannheim Mannheim Germany"
}
],
"authenticated-orcid": false,
"family": "El‐Battrawy",
"given": "Ibrahim",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5808-7810",
"affiliation": [
{
"name": "San Carlo Clinic Milano Italy"
}
],
"authenticated-orcid": false,
"family": "Cortese",
"given": "Bernardo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8785-5092",
"affiliation": [
{
"name": "Department of Anesthesiology Mayo Clinic Rochester MN"
}
],
"authenticated-orcid": false,
"family": "Ramakrishna",
"given": "Harish",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4867-3912",
"affiliation": [
{
"name": "Hospital Clinico San Carlos Madrid Spain"
}
],
"authenticated-orcid": false,
"family": "Perez‐Villacastín",
"given": "Julian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3239-1910",
"affiliation": [
{
"name": "Hospital Clinico San Carlos Madrid Spain"
}
],
"authenticated-orcid": false,
"family": "Fernandez‐Ortiz",
"given": "Antonio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9610-7408",
"affiliation": [
{
"name": "Department of Medical and Surgical Sciences University of Foggia Italy"
}
],
"authenticated-orcid": false,
"family": "Brunetti",
"given": "Natale Daniele",
"sequence": "additional"
}
],
"container-title": "Journal of the American Heart Association",
"container-title-short": "JAHA",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
6,
22
]
],
"date-time": "2022-06-22T10:32:46Z",
"timestamp": 1655893966000
},
"deposited": {
"date-parts": [
[
2022,
6,
22
]
],
"date-time": "2022-06-22T10:32:49Z",
"timestamp": 1655893969000
},
"indexed": {
"date-parts": [
[
2022,
6,
22
]
],
"date-time": "2022-06-22T11:17:00Z",
"timestamp": 1655896620590
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
6,
22
]
]
},
"language": "en",
"link": [
{
"URL": "https://www.ahajournals.org/doi/full/10.1161/JAHA.121.024530",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "276",
"original-title": [],
"prefix": "10.1161",
"published": {
"date-parts": [
[
2022,
6,
22
]
]
},
"published-online": {
"date-parts": [
[
2022,
6,
22
]
]
},
"publisher": "Ovid Technologies (Wolters Kluwer Health)",
"reference": [
{
"DOI": "10.1056/NEJMoa2001017",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_2_2"
},
{
"DOI": "10.1016/j.eclinm.2020.100639",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_3_2"
},
{
"DOI": "10.1001/jama.2021.4152",
"article-title": "Effect of intermediate‐dose vs standard‐dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID‐19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial",
"author": "Mazloomzadeh S",
"doi-asserted-by": "crossref",
"first-page": "1620",
"journal-title": "JAMA",
"key": "e_1_3_1_4_2",
"unstructured": "Mazloomzadeh S, Khaleghparast S, Ghadrdoost B, Mousavizadeh M, Baay MR, Noohi F, Sharifnia H, Ahmadi A, Tavan S, Malekpour Alamdari N, et al. Effect of intermediate‐dose vs standard‐dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID‐19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial. JAMA. 2021;325:1620–1630. doi: 10.1001/jama.2021.4152",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2103417",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_5_2"
},
{
"DOI": "10.1056/NEJMoa2105911",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_6_2"
},
{
"DOI": "10.1016/S0140-6736(21)01203-4",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_7_2"
},
{
"DOI": "10.1136/heartjnl-2021-319552",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_8_2"
},
{
"DOI": "10.1016/S0140-6736(21)01825-0",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_9_2"
},
{
"DOI": "10.1016/j.conctc.2020.100654",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_10_2"
},
{
"DOI": "10.1097/CCM.0000000000005010",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_11_2"
},
{
"DOI": "10.1161/circulationaha.110.009449",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_12_2"
},
{
"DOI": "10.1097/CCM.0000000000004363",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_13_2"
},
{
"DOI": "10.1097/SHK.0000000000001660",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_14_2"
},
{
"DOI": "10.1007/s00134-020-05985-9",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_15_2"
},
{
"DOI": "10.1016/j.eclinm.2020.100434",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_16_2"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.051828",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_17_2"
},
{
"DOI": "10.1186/s13045-020-01003-z",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_18_2"
},
{
"DOI": "10.1016/j.ebiom.2020.102969",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_19_2"
},
{
"DOI": "10.1126/science.8052854",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_20_2"
},
{
"DOI": "10.1590/0037-8682-0472-2020",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_21_2"
},
{
"DOI": "10.1038/35393",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_22_2"
},
{
"DOI": "10.1016/j.thromres.2020.09.013",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_23_2"
},
{
"DOI": "10.1038/s41591-022-01689-3",
"doi-asserted-by": "publisher",
"key": "e_1_3_1_24_2"
}
],
"reference-count": 23,
"references-count": 23,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.ahajournals.org/doi/10.1161/JAHA.121.024530"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cardiology and Cardiovascular Medicine"
],
"subtitle": [],
"title": "Aspirin Therapy on Prophylactic Anticoagulation for Patients Hospitalized With COVID‐19: A Propensity Score‐Matched Cohort Analysis of the HOPE‐COVID‐19 Registry",
"type": "journal-article"
}