The Association of Non-Steroidal Anti-Inflammatory Drugs with COVID-19 Severity and Mortality
et al., Archives of Clinical Infectious Diseases, doi:10.5812/archcid.106847, Jul 2020
Retrospective 158 COVID-19 patients in Iran, showing higher risk of mortality with ibuprofen use.
|
risk of death, 100% higher, OR 2.00, p < 0.001, treatment 63, control 95, adjusted per study, multivariable, RR approximated with OR.
|
|
risk of severe case, 427.8% higher, RR 5.28, p < 0.001, treatment 14 of 63 (22.2%), control 4 of 95 (4.2%).
|
|
risk of progression, 13.1% higher, RR 1.13, p = 0.04, treatment 60 of 63 (95.2%), control 80 of 95 (84.2%), moderate or severe.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Samimagham et al., 13 Jul 2020, retrospective, Iran, peer-reviewed, 4 authors.
Contact: mitra.kazemijahromi@gmail.com.
The Association of Non-Steroidal Anti-Inflammatory Drugs with COVID-19 Severity and Mortality
Archives of Clinical Infectious Diseases, doi:10.5812/archcid.106847
Background: No specific study has investigated the effect of non-steroidal anti inflammatory drugs (NSAIDs) and especially the effects of Ibuprofen on COVID-19, so far.
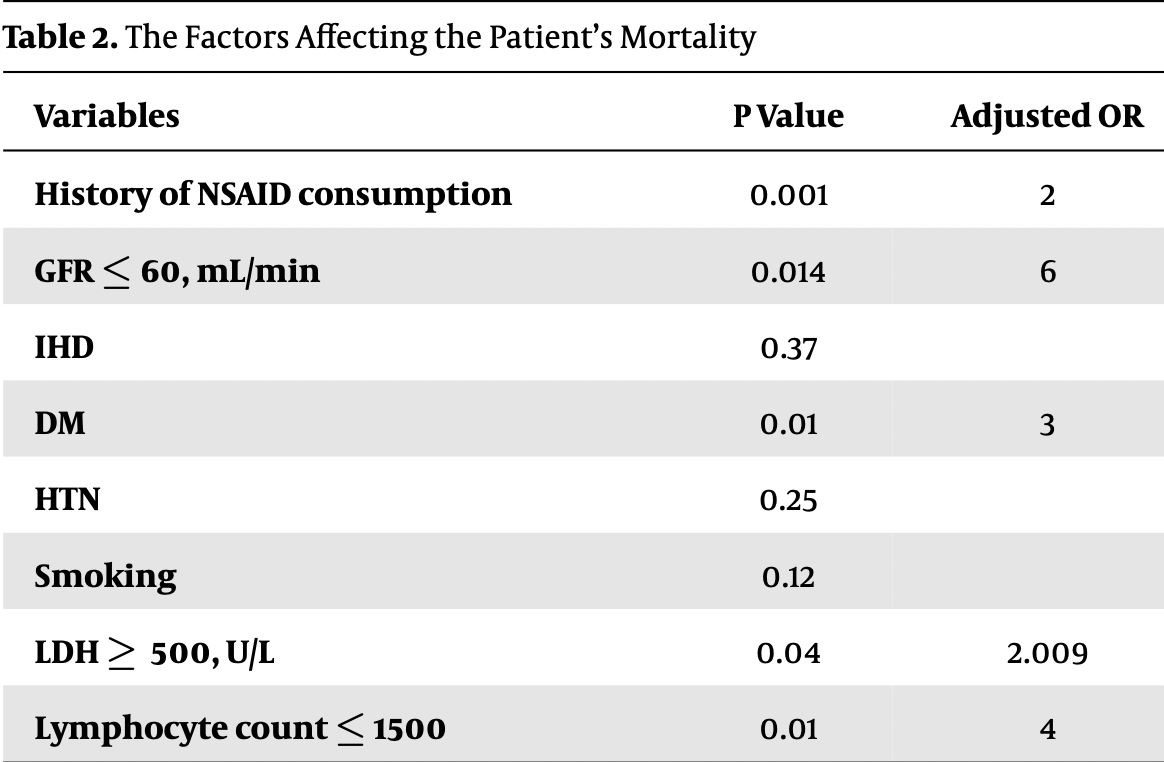
Objectives: The purpose of this study was to investigate the effect of Ibuprofen on the severity of COVID-19 and mortality caused by the disease. Methods: This study was conducted on 158 patients with COVID-19 who had consumed Ibuprofen, Gelofen, and Novafen for at least one week in the last three months. Patients were divided into three groups (mild, moderate and sever). The relationship among the severity of the disease and the history of ibuprofen consumption, diabetes, history of cardiovascular problems, hypertension, and GFR was investigated. Also, the association between the history of ibuprofen consumption, GFR ≤ 60 mL/min, hypertension, LDH ≥ 500 U/L, lymphocyte count ≤ 1500, and mortality was examined. Results: Our findings showed a significant relationship between the history of Ibuprofen before COVID-19 and the severity of COVID-19, as well as the mortality rate (P value < 0.001, adjusted odd ratio: 2, respectively). This study also showed a significant relationship among the severity of the disease and the history of smoking, diabetes, hypertension, history of cardiovascular diseases, and GFR. In addition, a significant relationship was found among GFR ≤ 60 mL/min mortality, diabetes, LDH ≥ 500 U/L, and lymphocyte count ≤ 1500.
Conclusions: Our study showed a significant relationship between the history of the consumption of ibuprofen and its compounds before COVID-19 and the severity of COVID-19, as well as the mortality rate of the patients with this disease, and accordingly, this result can suggest health policies during the epidemic of COVID-19.
References
Basille, Plouvier, Trouve, Duhaut, Andrejak et al., Non-steroidal anti-inflammatory drugs may worsen the course of community-acquired pneumonia: A cohort study, Lung, doi:10.1007/s00408-016-9973-1
Bourgeois, Ferroni, Leruez-Ville, Varon, Thumerelle et al., Nonsteroidal anti-inflammatory drug without antibiotics for acute viral infection increases the empyema risk in children: A matched case-control study, J Pediatr, doi:10.1016/j.jpeds.2016.05.025
Cheng, Luo, Wang, Zhang, Wang et al., Kidney disease is associated with in-hospital death of patients with COVID-19, Kidney Int, doi:10.1016/j.kint.2020.03.005
Crosby, Heimann, Burleson, Anzalone, Swanson et al., COVID-19: A review of therapeutics under investigation, J Am Coll Emerg Physicians Open
Cucinotta, Vanelli, WHO declares COVID-19 a pandemic, Acta Bio-Medica: Atenei Parmensis
De Girolamo, Peretti, Maffulli, Brini, Covid-19-the real role of NSAIDs in Italy, J Orthop Surg Res, doi:10.1186/s13018-020-01682-x
Fang, Karakiulakis, Roth, Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?, Lancet Respir Med, doi:10.1016/S2213-2600(20)30116-8
Fitzgerald, Misguided drug advice for COVID-19, Science, doi:10.1126/science.abb8034
Gandhi, Lynch, Rio, Mild or moderate Covid-19, N Engl J Med, doi:10.1056/NEJMcp2009249
Henry, De Oliveira, Benoit, Plebani, Lippi, Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis, Clin Chem Lab Med, doi:10.1515/cclm-2020-0369
Huang, Lim, Pranata, Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia -A systematic review, meta-analysis, and meta-regression, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.018
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/s0140-6736(20)30183-5
Kumar, Arora, Sharma, Anikhindi, Bansal et al., Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.044
Little, Non-steroidal anti-inflammatory drugs and covid-19, BMJ, doi:10.1136/bmj.m1185
Mehra, Desai, Kuy, Henry, Patel, Cardiovascular disease, drug therapy, and mortality in Covid-19, N Engl J Med, doi:10.1056/NEJMoa2007621
Mo, Xing, Xiao, Deng, Zhao et al., Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China, Clin Infect Dis, doi:10.1093/cid/ciaa270
No, Regulatory agencies issue advice on use of NSAIDs for COVID-19, React Wkly, doi:10.1007/s40278-020-76740-2
Qin, Zhou, Hu, Zhang, Yang et al., Dysregulation of immune response in patients with COVID-19 in Wuhan, China, Clin Infect Dis, doi:10.1093/cid/ciaa248
Russell, Moss, George, Santaolalla, Cope et al., Associations between immune-suppressive and stimulating drugs and novel COVID-19-a systematic review of current evidence, Ecancermedicalscience, doi:10.3332/ecancer.2020.1022
Sohrabi, Alsafi, Neill, Khan, Kerwan et al., World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19), Int J Surg, doi:10.1016/j.ijsu.2020.02.034
Wang, Du, Zhu, Cao, An et al., Comorbidities and multi-organ injuries in the treatment of COVID-19, Lancet, doi:10.1016/S0140-6736(20)30558-4
Wang, Nie, Wang, Zhao, Xiong et al., Characteristics of peripheral lymphocyte subset alteration in COVID-19 pneumonia, J Infect Dis, doi:10.1093/infdis/jiaa150
Wang, Zuo, Liu, Zhang, Zhao et al., Clinical and laboratory predictors of in-hospital mortality in patients with COVID-19: A cohort study in Wuhan, China, Clin Infect Dis, doi:10.1093/cid/ciaa538
Yan, Yang, Wang, Ren, Zhang et al., Clinical characteristics and outcomes of patients with severe covid-19 with diabetes, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2020-001343
Zhao, Yao, Wang, Zheng, Gao et al., A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias, Clin Infect Dis, doi:10.1093/cid/ciaa247
Zheng, Peng, Xu, Zhao, Liu et al., Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis, J Infect, doi:10.1016/j.jinf.2020.04.021
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study, Lancet, doi:10.1016/s0140-6736(20)30566-3
DOI record:
{
"DOI": "10.5812/archcid.106847",
"ISSN": [
"2345-2641"
],
"URL": "http://dx.doi.org/10.5812/archcid.106847",
"abstract": "<jats:p>Background: No specific study has investigated the effect of non-steroidal anti inflammatory drugs (NSAIDs) and especially the effects of Ibuprofen on COVID-19, so far. Objectives: The purpose of this study was to investigate the effect of Ibuprofen on the severity of COVID-19 and mortality caused by the disease. Methods: This study was conducted on 158 patients with COVID-19 who had consumed Ibuprofen, Gelofen, and Novafen for at least one week in the last three months. Patients were divided into three groups (mild, moderate and sever). The relationship among the severity of the disease and the history of ibuprofen consumption, diabetes, history of cardiovascular problems, hypertension, and GFR was investigated. Also, the association between the history of ibuprofen consumption, GFR ≤ 60 mL/min, hypertension, LDH ≥ 500 U/L, lymphocyte count ≤ 1500, and mortality was examined. Results: Our findings showed a significant relationship between the history of Ibuprofen before COVID-19 and the severity of COVID-19, as well as the mortality rate (P value < 0.001, adjusted odd ratio: 2, respectively). This study also showed a significant relationship among the severity of the disease and the history of smoking, diabetes, hypertension, history of cardiovascular diseases, and GFR. In addition, a significant relationship was found among GFR ≤ 60 mL/min mortality, diabetes, LDH ≥ 500 U/L, and lymphocyte count ≤ 1500. Conclusions: Our study showed a significant relationship between the history of the consumption of ibuprofen and its compounds before COVID-19 and the severity of COVID-19, as well as the mortality rate of the patients with this disease, and accordingly, this result can suggest health policies during the epidemic of COVID-19.</jats:p>",
"alternative-id": [
"5e764ef28031739fda1c07f3f56e47d0d60ff74d"
],
"assertion": [
{
"group": {
"label": "Import History",
"name": "import_history"
},
"label": "Import",
"name": "import",
"value": "Article is imported on 2020-07-13 07:24:20 by user ID: 106060."
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"value": "2020-6-25"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "2020-6-28"
},
{
"group": {
"label": "Import History",
"name": "import_history"
},
"label": "Import",
"name": "import",
"value": "Article is imported on 2020-11-30 16:12:28 by user ID: 274."
}
],
"author": [
{
"affiliation": [],
"family": "Samimagham",
"given": "Hamid Reza",
"sequence": "first"
},
{
"affiliation": [],
"family": "Arabi",
"given": "Mohsen",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0283-5680",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hooshyar",
"given": "Dariush",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9127-3594",
"affiliation": [],
"authenticated-orcid": false,
"family": "KazemiJahromi",
"given": "Mitra",
"sequence": "additional"
}
],
"container-title": "Archives of Clinical Infectious Diseases",
"container-title-short": "Arch Clin Infect Dis",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"sites.kowsarpub.com"
]
},
"created": {
"date-parts": [
[
2020,
7,
13
]
],
"date-time": "2020-07-13T07:24:47Z",
"timestamp": 1594625087000
},
"deposited": {
"date-parts": [
[
2022,
1,
10
]
],
"date-time": "2022-01-10T08:49:43Z",
"timestamp": 1641804583000
},
"indexed": {
"date-parts": [
[
2022,
4,
25
]
],
"date-time": "2022-04-25T19:07:32Z",
"timestamp": 1650913652782
},
"is-referenced-by-count": 6,
"issue": "4",
"issued": {
"date-parts": [
[
2020,
7,
13
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2020,
7,
13
]
]
}
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "am",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2013,
1,
1
]
],
"date-time": "2013-01-01T00:00:00Z",
"timestamp": 1356998400000
}
}
],
"link": [
{
"URL": "https://archcid.kowsarpub.com/cdn/dl/bf5e488a-3326-11eb-94ab-3b77943e83ed",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://sites.kowsarpub.com/archcid/articles/106847.html",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "3819",
"original-title": [],
"prefix": "10.5812",
"published": {
"date-parts": [
[
2020,
7,
13
]
]
},
"published-online": {
"date-parts": [
[
2020,
7,
13
]
]
},
"publisher": "Briefland",
"reference": [
{
"DOI": "10.1016/j.ijsu.2020.02.034",
"doi-asserted-by": "publisher",
"key": "key-A106847REF1-1"
},
{
"author": "Cucinotta D",
"first-page": "157",
"issue": "1",
"journal-title": "Acta Bio-Medica: Atenei Parmensis.",
"key": "key-A106847REF2-2",
"volume": "91",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30558-4",
"doi-asserted-by": "publisher",
"key": "key-A106847REF3-3"
},
{
"DOI": "10.1016/s0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "key-A106847REF4-4"
},
{
"DOI": "10.1016/S2213-2600(20)30116-8",
"doi-asserted-by": "publisher",
"key": "key-A106847REF5-5"
},
{
"DOI": "10.1007/s40278-020-76740-2",
"doi-asserted-by": "publisher",
"key": "key-A106847REF6-6"
},
{
"DOI": "10.1126/science.abb8034",
"doi-asserted-by": "publisher",
"key": "key-A106847REF7-7"
},
{
"DOI": "10.1016/s0140-6736(20)30183-5",
"doi-asserted-by": "publisher",
"key": "key-A106847REF8-8"
},
{
"author": "Crosby JC",
"journal-title": "J Am Coll Emerg Physicians Open.",
"key": "key-A106847REF9-9",
"year": "2020"
},
{
"DOI": "10.1016/j.jpeds.2016.05.025",
"doi-asserted-by": "publisher",
"key": "key-A106847REF10-10"
},
{
"DOI": "10.1007/s00408-016-9973-1",
"doi-asserted-by": "publisher",
"key": "key-A106847REF11-11"
},
{
"DOI": "10.3332/ecancer.2020.1022",
"doi-asserted-by": "publisher",
"key": "key-A106847REF12-12"
},
{
"DOI": "10.1056/NEJMcp2009249",
"doi-asserted-by": "publisher",
"key": "key-A106847REF13-13"
},
{
"DOI": "10.1136/bmj.m1185",
"doi-asserted-by": "publisher",
"key": "key-A106847REF14-14"
},
{
"DOI": "10.1186/s13018-020-01682-x",
"doi-asserted-by": "publisher",
"key": "key-A106847REF15-15"
},
{
"DOI": "10.1056/NEJMoa2007621",
"doi-asserted-by": "publisher",
"key": "key-A106847REF16-16"
},
{
"DOI": "10.1016/j.dsx.2020.04.044",
"doi-asserted-by": "publisher",
"key": "key-A106847REF17-17"
},
{
"DOI": "10.1016/j.dsx.2020.04.018",
"doi-asserted-by": "publisher",
"key": "key-A106847REF18-18"
},
{
"DOI": "10.1136/bmjdrc-2020-001343",
"doi-asserted-by": "publisher",
"key": "key-A106847REF19-19"
},
{
"DOI": "10.1093/cid/ciaa538",
"doi-asserted-by": "publisher",
"key": "key-A106847REF20-20"
},
{
"DOI": "10.1016/j.kint.2020.03.005",
"doi-asserted-by": "publisher",
"key": "key-A106847REF21-21"
},
{
"DOI": "10.1093/cid/ciaa247",
"doi-asserted-by": "publisher",
"key": "key-A106847REF22-22"
},
{
"DOI": "10.1016/j.jinf.2020.04.021",
"doi-asserted-by": "publisher",
"key": "key-A106847REF23-23"
},
{
"DOI": "10.1093/cid/ciaa270",
"doi-asserted-by": "publisher",
"key": "key-A106847REF24-24"
},
{
"DOI": "10.1515/cclm-2020-0369",
"doi-asserted-by": "publisher",
"key": "key-A106847REF25-25"
},
{
"DOI": "10.1093/infdis/jiaa150",
"doi-asserted-by": "publisher",
"key": "key-A106847REF26-26"
},
{
"DOI": "10.1093/cid/ciaa248",
"doi-asserted-by": "publisher",
"key": "key-A106847REF27-27"
}
],
"reference-count": 27,
"references-count": 27,
"relation": {},
"resource": {
"primary": {
"URL": "https://brief.land/archcid/articles/106847.html"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Toxicology",
"Public Health, Environmental and Occupational Health",
"Critical Care and Intensive Care Medicine",
"Infectious Diseases"
],
"subtitle": [],
"title": "The Association of Non-Steroidal Anti-Inflammatory Drugs with COVID-19 Severity and Mortality",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.5812/crossmark_update_policy",
"volume": "15"
}