COVID-19 in Parkinson’s disease: what holds the key?
et al., Journal of Neurology, doi:10.1007/s00415-020-10272-0, Oct 2020
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
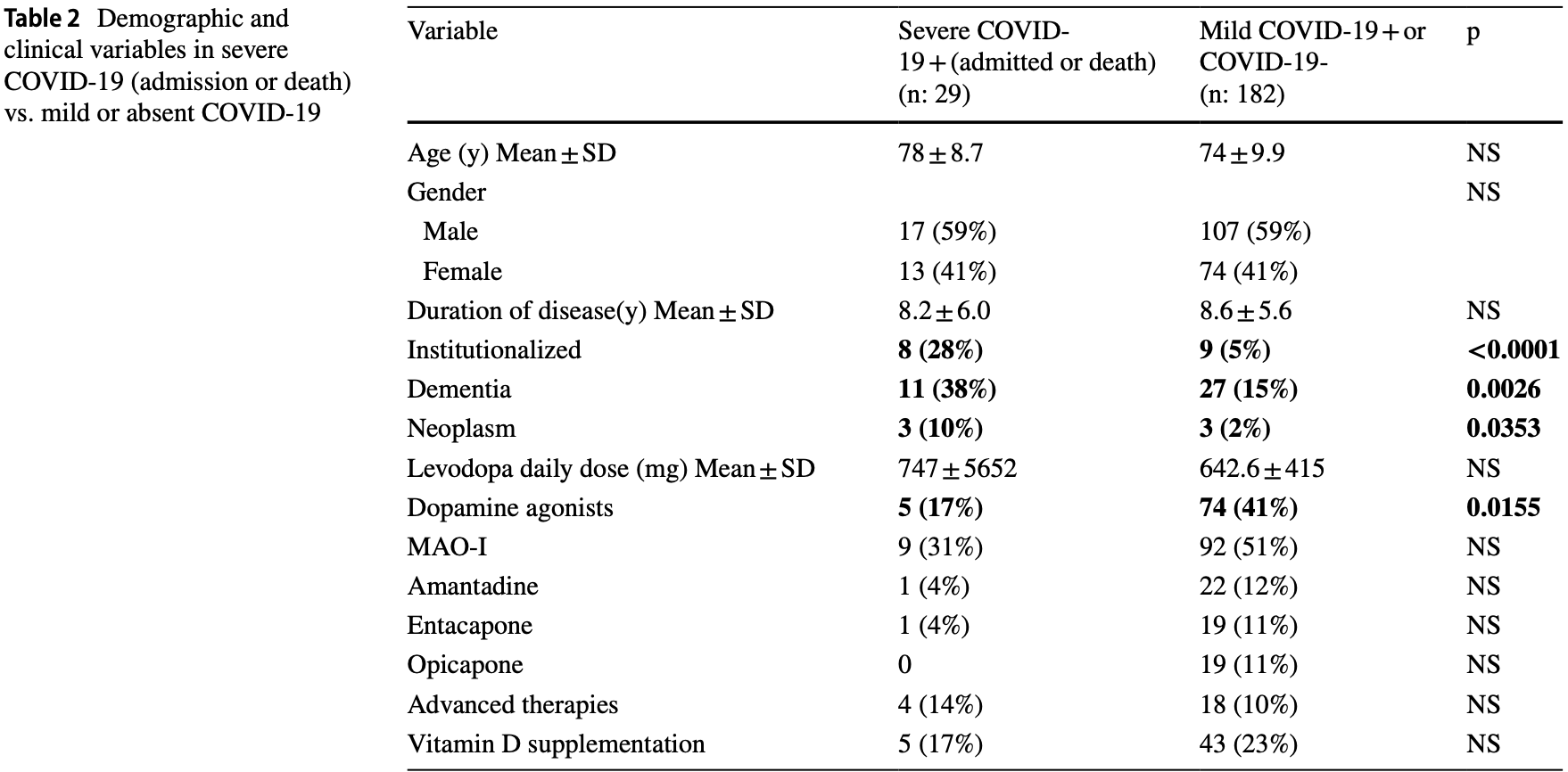
Case control study with 39 COVID+ and 172 COVID- Parkinson's disease patients in Spain, showing positive and severe cases being less likely to use vitamin D supplementation compared to negative or mild/negative cases respectively. These differences were not statistically significant.
This is the 6th of 136 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
|
risk of severe case, 32.7% lower, OR 0.67, p = 0.45, treatment 5 of 29 (17.2%) cases,
43 of 182 (23.6%) controls, NNT 23, case control OR.
|
|
risk of case, 43.7% lower, OR 0.56, p = 0.23, treatment 6 of 39 (15.4%) cases,
42 of 172 (24.4%) controls, NNT 13, case control OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Sainz-Amo et al., 24 Oct 2020, retrospective, Spain, peer-reviewed, mean age 74.5, 13 authors, dosage not specified.
COVID-19 in Parkinson’s disease: what holds the key?
Journal of Neurology, doi:10.1007/s00415-020-10272-0
Introduction Parkinson's disease (PD) is more frequent in the elderly and increases the risk of respiratory infections. Previous data on PD and SARS-CoV-2 are scarce, suggesting a poor prognosis in advanced disease and second-line therapies. Methods A retrospective case-control study comparing patients with PD and COVID-19 and patients with PD without COVID-19 was conducted during the pandemic period in Spain (March 1st-July 31st 2020) in a tertiary university hospital. Results Thirty-nine (COVID-19 +) and 172 (COVID-19-) PD patients were included. Fifty-nine percent were males in both groups, with similar age (75.9 ± 9.0 COVID-19 + , 73.9 ± 10.0 COVID-19-), disease duration (8.9 ± 6.2 COVID-19 + , 8.5 ± 5.6 COVID-19-) and PD treatments. COVID-19 was mild in 10 (26%), required admission in 21 (54%) and caused death in 8 (21%) patients. Dementia was the only comorbidity more frequent in COVID-19 + patients (36% vs. 14%, p = 0.0013). However, in a multivariate analysis, institutionalization was the only variable associated with COVID-19 + (OR 17.0, 95% CI 5.0-60.0, p < 0.001). When considering severe COVID-19 (admission or death) vs. mild or absent COVID-19, institutionalization, neoplasm, dementia and a lower frequency of dopamine agonists were associated with severe COVID-19. In multivariate analysis, only institutionalization [OR 5.17, 95% CI 1.57-17, p = 0.004] and neoplasm [OR 8.0, 95%CI 1.27-49.8, p = 0.027] remained significantly associated. Conclusion In our experience, institutionalization and oncologic comorbidity, rather than PD-related variables, increased the risk of developing COVID-19, and impacted on its severity. These findings suggest that epidemiologic factors and frailty are key factors for COVID-19 morbidity/mortality in PD. Appropriate preventive strategies should be implemented in institutionalized patients to prevent infection and improve prognosis.
Compliance with ethical standards Conflicts of interest On behalf of all authors, the corresponding author states that there is no conflict of interest. Data are available upon request to the authors.
Ethical standard The study was approved by the local Ethics Committee.
References
Antonini, Leta, Teo, Outcome of Parkinson's disease patients affected by COVID-19, Mov Disord
Cilia, Bonvegna, Straccia, Effects of COVID-19 on Parkinson's disease clinical features: a community-based case-control study, Mov Disord
Fasano, Cereda, Barichella, COVID-19 in Parkinson's disease patients living in Lombardy, Italy, Mov Disord
Fasano, Elia, Dallocchio, Predictors of COVID-19 outcome in Parkinson's disease, Parkinsonism Relat Disord
Gosain, Abdou, Singh, COVID-19 and cancer: a comprehensive review, Curr Oncol Rep
Helmich, Bloem, The Impact of the COVID-19 pandemic on parkinson disease: hidden sorrows and emerging opportunities, J Parkinsons Dis
Hribar, Cobbold, Church, Potential role of vitamin D in the elderly to resist COVID-19 and to slow progression of Parkinson's disease, Brain Sci
Monteiro, Souza-Machado, Valderramas, The effect of levodopa on pulmonary function in Parkinson's disease: a systematic review and meta-analysis, Clin Ther
Nataf, An alteration of the dopamine synthetic pathway is possibly involved in the pathophysiology of COVID-19, J Med Virol, doi:10.1002/jmv.25826
Postuma, Berg, Stern, MDS clinical diagnostic criteria for Parkinson's disease, Mov Disord
Prasad, Holla, Neeraja, Parkinson disease and COVID-19: perceptions and implications in patients and caregivers, Mov Disord
Rada, Covid-19: the precarious position of Spain's nursing homes, BMJ
Rejdak, Grieb, Adamantanes might be protective from COVID-19 in patients with neurological diseases: multiple sclerosis, parkinsonism and cognitive impairment, Mult Scler Relat Disord
Rockwood, Song, Macknight, A global clinical measure of fitness and frailty in elderly people, CMAJ
Wu, Xiaoyan, Yanping, Risk factors associated with acute respiratory distress syndrome and death in patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China, JAMA Intern Med
Zipprich, Teschner, Witte, Knowledge, attitudes, practices and burden during the COVID-19 pandemic in people with Parkinson's disease in Germany, J Clin Med
DOI record:
{
"DOI": "10.1007/s00415-020-10272-0",
"ISSN": [
"0340-5354",
"1432-1459"
],
"URL": "http://dx.doi.org/10.1007/s00415-020-10272-0",
"alternative-id": [
"10272"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "10 September 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Revised",
"name": "revised",
"order": 2,
"value": "4 October 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 3,
"value": "10 October 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 4,
"value": "24 October 2020"
},
{
"group": {
"label": "Compliance with ethical standards",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflicts of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "On behalf of all authors, the corresponding author states that there is no conflict of interest. Data are available upon request to the authors."
},
{
"group": {
"label": "Ethical standard",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "The study was approved by the local Ethics Committee."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-2432-0039",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sainz-Amo",
"given": "R.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Baena-Álvarez",
"given": "B.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pareés",
"given": "I.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sánchez-Díez",
"given": "G.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pérez-Torre",
"given": "P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "López-Sendón",
"given": "J. L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fanjul-Arbos",
"given": "S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Monreal",
"given": "E.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Corral-Corral",
"given": "I.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "García-Barragán",
"given": "N.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Martínez-Castrillo",
"given": "J. C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fasano",
"given": "A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alonso-Cánovas",
"given": "A.",
"sequence": "additional"
}
],
"container-title": [
"Journal of Neurology"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2020,
10,
24
]
],
"date-time": "2020-10-24T15:02:24Z",
"timestamp": 1603551744000
},
"deposited": {
"date-parts": [
[
2021,
10,
23
]
],
"date-time": "2021-10-23T23:16:25Z",
"timestamp": 1635030985000
},
"indexed": {
"date-parts": [
[
2021,
11,
30
]
],
"date-time": "2021-11-30T17:50:49Z",
"timestamp": 1638294649696
},
"is-referenced-by-count": 9,
"issn-type": [
{
"type": "print",
"value": "0340-5354"
},
{
"type": "electronic",
"value": "1432-1459"
}
],
"issue": "8",
"issued": {
"date-parts": [
[
2020,
10,
24
]
]
},
"journal-issue": {
"issue": "8",
"published-print": {
"date-parts": [
[
2021,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
10,
24
]
],
"date-time": "2020-10-24T00:00:00Z",
"timestamp": 1603497600000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
10,
24
]
],
"date-time": "2020-10-24T00:00:00Z",
"timestamp": 1603497600000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s00415-020-10272-0.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s00415-020-10272-0/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s00415-020-10272-0.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"page": "2666-2670",
"prefix": "10.1007",
"published": {
"date-parts": [
[
2020,
10,
24
]
]
},
"published-online": {
"date-parts": [
[
2020,
10,
24
]
]
},
"published-print": {
"date-parts": [
[
2021,
8
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"key": "10272_CR1",
"unstructured": "World Health Organization Coronavirus Disease (COVID-19) (2020) https://covid19.who.int. Accessed Aug 31, 2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"author": "Wu Chaomin",
"doi-asserted-by": "publisher",
"first-page": "934",
"journal-title": "JAMA Intern Med",
"key": "10272_CR2",
"unstructured": "Chaomin Wu, Chen Xiaoyan, Cai Yanping et al (2020) Risk factors associated with acute respiratory distress syndrome and death in patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med 180:934–943",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1016/j.clinthera.2012.03.001",
"author": "L Monteiro",
"doi-asserted-by": "publisher",
"first-page": "1049",
"journal-title": "Clin Ther",
"key": "10272_CR3",
"unstructured": "Monteiro L, Souza-Machado A, Valderramas S et al (2012) The effect of levodopa on pulmonary function in Parkinson’s disease: a systematic review and meta-analysis. Clin Ther 2:1049–1055",
"volume": "2",
"year": "2012"
},
{
"DOI": "10.1002/mds.28088",
"author": "S Prasad",
"doi-asserted-by": "publisher",
"first-page": "912",
"journal-title": "Mov Disord",
"key": "10272_CR4",
"unstructured": "Prasad S, Holla VV, Neeraja K et al (2020) Parkinson disease and COVID-19: perceptions and implications in patients and caregivers. Mov Disord 35:912–914",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.3233/JPD-202038",
"author": "RC Helmich",
"doi-asserted-by": "publisher",
"first-page": "351",
"journal-title": "J Parkinsons Dis",
"key": "10272_CR5",
"unstructured": "Helmich RC, Bloem BRC (2020) The Impact of the COVID-19 pandemic on parkinson disease: hidden sorrows and emerging opportunities. J Parkinsons Dis 10:351–354",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.3390/jcm9061643",
"author": "HM Zipprich",
"doi-asserted-by": "publisher",
"first-page": "1643",
"journal-title": "J Clin Med",
"key": "10272_CR6",
"unstructured": "Zipprich HM, Teschner U, Witte OW et al (2020) Knowledge, attitudes, practices and burden during the COVID-19 pandemic in people with Parkinson’s disease in Germany. J Clin Med 9:1643",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.msard.2020.102163",
"author": "K Rejdak",
"doi-asserted-by": "publisher",
"first-page": "102163",
"journal-title": "Mult Scler Relat Disord",
"key": "10272_CR7",
"unstructured": "Rejdak K, Grieb P (2020) Adamantanes might be protective from COVID-19 in patients with neurological diseases: multiple sclerosis, parkinsonism and cognitive impairment. Mult Scler Relat Disord 42:102163",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.1002/jmv.25826",
"author": "S Nataf",
"doi-asserted-by": "publisher",
"journal-title": "J Med Virol",
"key": "10272_CR8",
"unstructured": "Nataf S (2020) An alteration of the dopamine synthetic pathway is possibly involved in the pathophysiology of COVID-19. J Med Virol. https://doi.org/10.1002/jmv.25826",
"year": "2020"
},
{
"DOI": "10.1002/mds.28104",
"author": "A Antonini",
"doi-asserted-by": "publisher",
"first-page": "905",
"journal-title": "Mov Disord",
"key": "10272_CR9",
"unstructured": "Antonini A, Leta V, Teo J et al (2020) Outcome of Parkinson’s disease patients affected by COVID-19. Mov Disord 35:905–908",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1002/mds.28176",
"author": "A Fasano",
"doi-asserted-by": "publisher",
"first-page": "1089",
"journal-title": "Mov Disord",
"key": "10272_CR10",
"unstructured": "Fasano A, Cereda E, Barichella M et al (2020) COVID-19 in Parkinson’s disease patients living in Lombardy, Italy. Mov Disord 35:1089–1093",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.3390/brainsci10050284",
"author": "CA Hribar",
"doi-asserted-by": "publisher",
"first-page": "284",
"journal-title": "Brain Sci",
"key": "10272_CR11",
"unstructured": "Hribar CA, Cobbold PH, Church FC (2020) Potential role of vitamin D in the elderly to resist COVID-19 and to slow progression of Parkinson’s disease. Brain Sci 10:284",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1002/mds.28170",
"author": "R Cilia",
"doi-asserted-by": "publisher",
"first-page": "1287",
"journal-title": "Mov Disord",
"key": "10272_CR12",
"unstructured": "Cilia R, Bonvegna S, Straccia G et al (2020) Effects of COVID-19 on Parkinson’s disease clinical features: a community-based case-control study. Mov Disord 35:1287–1292",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1016/j.parkreldis.2020.08.012",
"author": "A Fasano",
"doi-asserted-by": "publisher",
"first-page": "134",
"journal-title": "Parkinsonism Relat Disord",
"key": "10272_CR13",
"unstructured": "Fasano A, Elia AE, Dallocchio C et al (2020) Predictors of COVID-19 outcome in Parkinson’s disease. Parkinsonism Relat Disord 78:134–137",
"volume": "78",
"year": "2020"
},
{
"key": "10272_CR14",
"unstructured": "Ministerio de Sanidad (2020) Situación de COVID-19 en España. https://cnecovid.isciii.es/covid19. Accessed July 31, 2020"
},
{
"DOI": "10.1002/mds.26424",
"author": "RB Postuma",
"doi-asserted-by": "publisher",
"first-page": "1591",
"journal-title": "Mov Disord",
"key": "10272_CR15",
"unstructured": "Postuma RB, Berg D, Stern M et al (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1601",
"volume": "30",
"year": "2015"
},
{
"key": "10272_CR16",
"unstructured": "Centers for Disease Control and Prevention (2020) Coronavirus disease 2019 (COVID-19). Interim Case Definition, Approved April 5, 2020. https://www.cdc.gov/nndss/conditions/coronavirus-disease-2019-covid-19/casedefinition/2020. Accessed on August 31, 2020"
},
{
"DOI": "10.1136/bmj.m1554",
"author": "AG Rada",
"doi-asserted-by": "publisher",
"first-page": "m1554",
"journal-title": "BMJ",
"key": "10272_CR17",
"unstructured": "Rada AG (2020) Covid-19: the precarious position of Spain’s nursing homes. BMJ 369:m1554",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1503/cmaj.050051",
"author": "K Rockwood",
"doi-asserted-by": "publisher",
"first-page": "489",
"journal-title": "CMAJ",
"key": "10272_CR18",
"unstructured": "Rockwood K, Song X, MacKnight C et al (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173:489–495",
"volume": "173",
"year": "2005"
},
{
"DOI": "10.1007/s11912-020-00934-7",
"author": "R Gosain",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "Curr Oncol Rep",
"key": "10272_CR19",
"unstructured": "Gosain R, Abdou Y, Singh A et al (2020) COVID-19 and cancer: a comprehensive review. Curr Oncol Rep 22:53",
"volume": "22",
"year": "2020"
}
],
"reference-count": 19,
"references-count": 19,
"relation": {},
"score": 1,
"short-container-title": [
"J Neurol"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Clinical Neurology",
"Neurology"
],
"subtitle": [],
"title": [
"COVID-19 in Parkinson’s disease: what holds the key?"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "268"
}
