History of heart failure and chronic kidney disease and risk of all-cause death after COVID-19 during the first three waves of the pandemic in comparison with influenza outbreaks in Sweden: a registry-based, retrospective, case–control study
et al., BMJ Open, doi:10.1136/bmjopen-2022-069037, Apr 2023
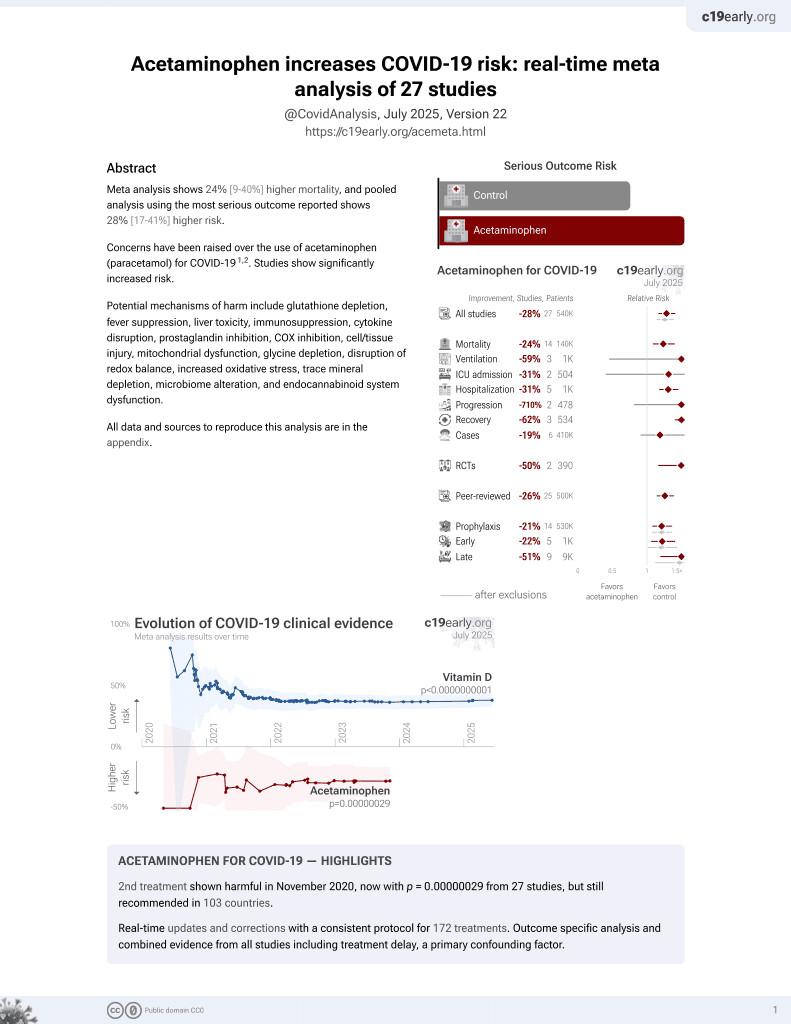
2nd treatment shown to increase risk in
November 2020, now with p = 0.00000029 from 27 studies, but still recommended in 103 countries.
6,400+ studies for
210+ treatments. c19early.org
|
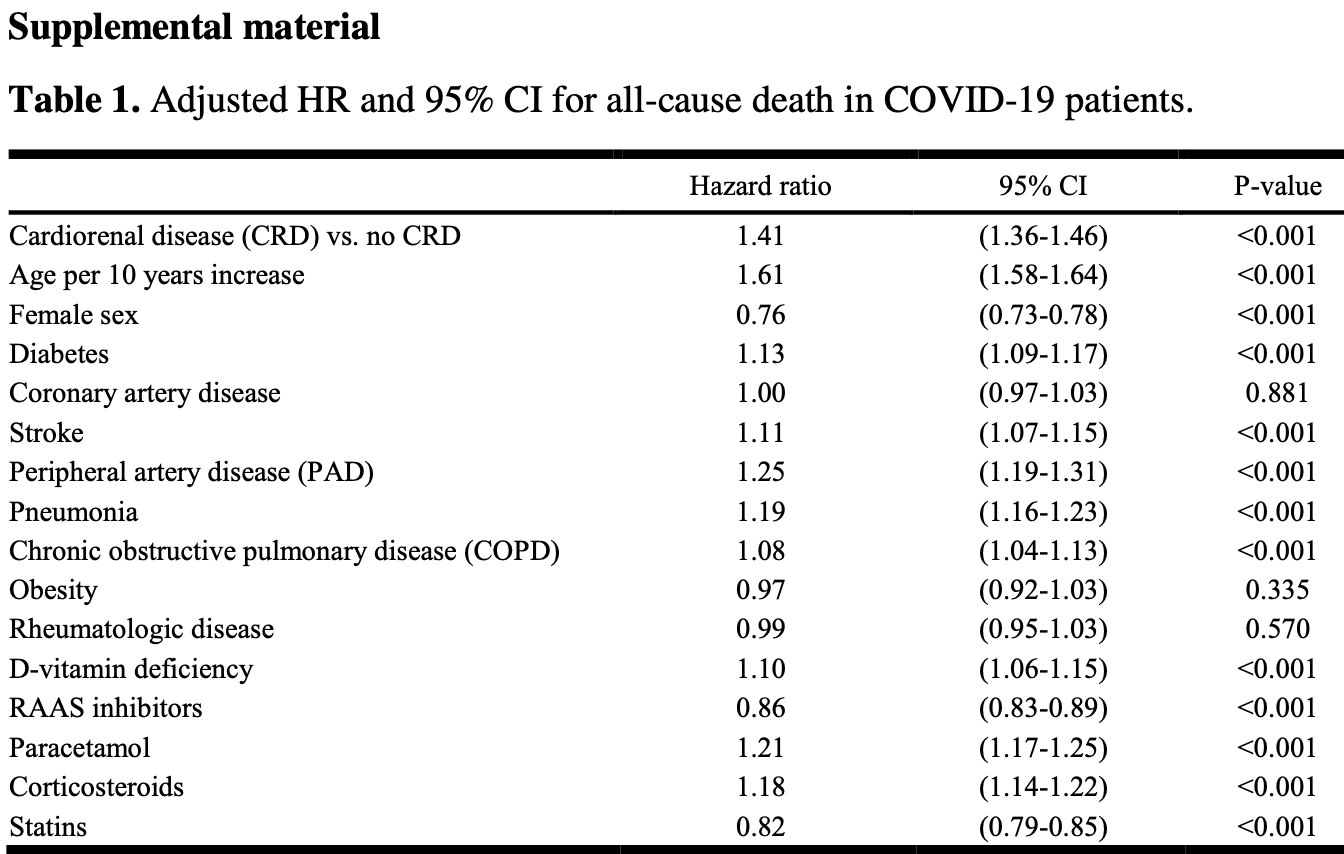
Retrospective 44,866 hospitalized COVID-19 patients in Sweden, showing higher mortality with vitamin D deficiency and with acetaminophen use.
The study focuses on cardiorenal disease, finding higher risk of mortality with CRD. Authors also show that COVID-19 mortality was about 1.5x higher when compared with influenza in the first two pandemic waves, but there was no significant difference in the third wave (HR 1.53 [1.45-1.62] and 1.52 [1.44-1.61] in the first two waves and 1.07 [0.99-1.14] in the third).
Acetaminophen is also known as paracetamol, Tylenol, Panadol, Calpol, Tempra, Calprofen, Doliprane, Efferalgan, Grippostad C, Dolo, Acamol, Fevadol, Crocin, and Perfalgan.
Study covers acetaminophen and vitamin D.
|
risk of death, 21.0% higher, HR 1.21, p < 0.001, treatment 24,641, control 20,225.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ritsinger et al., 28 Apr 2023, retrospective, Sweden, peer-reviewed, mean age 79.8, 8 authors, study period 1 January, 2020 - 9 September, 2021.
History of heart failure and chronic kidney disease and risk of all-cause death after COVID-19 during the first three waves of the pandemic in comparison with influenza outbreaks in Sweden: a registry-based, retrospective, case–control study
BMJ Open, doi:10.1136/bmjopen-2022-069037
Objectives To explore how cardiorenal disease (CRD; heart failure and/or chronic kidney disease) impacted mortality in men and women hospitalised for COVID-19 during the first three waves of the pandemic in Sweden in comparison to previous influenza outbreaks. Design A registry-based, retrospective, case-control study. Setting Hospital care in Sweden. Participants All patients in Sweden with a main hospital diagnosis of COVID-19 (January 2020-September 2021) or influenza (January 2015-December 2019) with previous CRD were identified in registries and compared with a reference group free from CRD but with COVID-19 or influenza. Primary outcome measure Associated risk of all-cause death during the first year was analysed using adjusted Cox proportional hazards models. Results In COVID-19 patients with and without prior history of CRD (n=44 866), mean age was 79.8 years (SD 11.8) and 43% were women. In influenza patients (n=8897), mean age was 80.6 years (SD 11.5) and 45% were women. COVID-19 versus influenza was associated with higher mortality risk during the first two COVID-19 waves (HR 1.53; 95% CI 1.45 to 1.62, p<0.001 and HR 1.52; 95% CI 1.44 to 1.61, p<0.001), but not in the third wave (HR 1.07; 95% CI 0.99 to 1.14, p=0.072). CRD was an independent risk factor for all-cause death after COVID-19 in men and women (men: 1.37; 95% CI 1.31 to 1.44, p<0.001; women: 1.46; 95% CI 1.38 to 1.54, p<0.001). At ages <70 years, women with CRD had a similar mortality rate to men with CRD, while at ages ≥70 years, the mortality rate was higher in men. Conclusions Outcome after COVID-19 is worse if CRD is present. In women at ages <70 years, the presence of CRD attenuates the protective effect of female sex. COVID-19 was associated with higher mortality risk than influenza during the first two pandemic waves. ⇒ This study includes all patients with cardiorenal disease hospitalised for COVID-19 during the first three pandemic waves in Sweden. ⇒ This study compares mortality associated with COVID-19 to previous influenza outbreaks. ⇒ Sex-based analyses by age group were performed to explore the importance of sex as a risk factor. ⇒ This was a national registry-based study that lacked data regarding the proportion of patients vaccinated for influenza. ⇒ The study also lacked information on laboratory analyses and variables such as body mass index and type of heart failure.
Competing interests The authors declared the following potential conflicts of interest with respect to the research, authorship and publication of this article: VR has received honoraria on expert group participation from Astra Zeneca, Novo Nordisk and Boehringer Ingelheim. AN has received honoraria from Astra Zeneca, Merck Sharp & Dohme, Eli Lilly and Company, Novo Nordisk and Boehringer Ingelheim on expert group participation. TN has received unrestricted grants from AstraZeneca and NovoNordisk and has served on national advisory boards of Abbot, Amgen, Novo Nordisk, Sanofi-Aventis, Eli Lilly, MSD and Boehringer Ingelheim. JE has received research support or honoraria from AstraZeneca, NovoNordisk, Bayer, Ilya Pharma, Merck-Sharp & Dohme, Boehringer-Ingelheim. RK and DN reports no conflicts of interest. JB holds a full-time position at AstraZeneca as an epidemiologist. MT holds a full-time position by an independent statistical consultant company, Statisticon AB, Uppsala, Sweden, of which AstraZeneca Nordic is a client. Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research. Patient consent for publication Not applicable.
Ethics approval The study was approved by the Stockholm Regional Ethics Committee (reference numbers 2020-05714 and 2013/2206-31). Ethical permission approved a reference group to a collected population with cardiorenal disease (CRD; heart..
References
Al-Salameh, Lanoix, Bennis, Characteristics and outcomes of COVID-19 in hospitalized patients with and without diabetes, Diabetes Metab Res Rev, doi:10.1002/dmrr.3388
Arbs, angiotensin receptor blockers
Arni, angiotensin receptor-neprilysin inhibitors; DVT, deep vein thrombosis
Ballin, Bergman, Kivipelto, Excess mortality after covid-19 in Swedish long-term care facilities, J Am Med Dir Assoc, doi:10.1016/j.jamda.2021.06.010
Barron, Bakhai, Kar, Associations of type 1 and type 2 diabetes with covid-19-related mortality in England: a wholepopulation study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30272-2
Bergman, Ballin, Nordström, Risk factors for COVID-19 diagnosis, hospitalization, and subsequent all-cause mortality in Sweden: a nationwide study, Eur J Epidemiol, doi:10.1007/s10654-021-00732-w
Cummings, Baldwin, Abrams, Epidemiology, clinical course, and outcomes of critically ill adults with covid-19 in New York City: a prospective cohort study, Lancet, doi:10.1016/S0140-6736(20)31189-2
Gasparini, Evans, Coresh, Prevalence and recognition of chronic kidney disease in Stockholm healthcare, Nephrol Dial Transplant, doi:10.1093/ndt/gfw354
Grasselli, Greco, Zanella, Risk factors associated with mortality among patients with covid-19 in intensive care units in lombardy, Italy, JAMA Intern Med, doi:10.1001/jamainternmed.2020.3539
Guan, Ni, Hu, Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med, doi:10.1056/NEJMoa2002032
Holman, Knighton, Kar, Risk factors for covid-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30271-0
House, Wanner, Sarnak, Heart failure in chronic kidney disease: conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference, Kidney Int, doi:10.1016/j.kint.2019.02.022
Mra, mineralocorticoid receptor antagonists; PE, pulmonary embolism; RAAS, renin-angiotensin system inhibitors; SGLT2, sodium-glucose cotransporter-2
Phelan, Katz, Lo, The novel coronavirus originating in Wuhan, China: challenges for global health governance, JAMA, doi:10.1001/jama.2020.1097
Piroth, Cottenet, Mariet, Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study, Lancet Respir Med, doi:10.1016/S2213-2600(20)30527-0
Rangaswami, Bhalla, Blair, American heart association Council on the kidney in cardiovascular disease and Council on clinical cardiology. cardiorenal syndrome: classification, pathophysiology, diagnosis, and treatment strategies: a scientific statement from the American heart association, Circulation, doi:10.1161/CIR.0000000000000664
Rawshani, Kjölhede, Rawshani, Severe COVID-19 in people with type 1 and type 2 diabetes in Sweden: a nationwide retrospective cohort study, Lancet Reg Health Eur, doi:10.1016/j.lanepe.2021.100105
Reilev, Kristensen, Pottegård, Characteristics and predictors of hospitalization and death in the first 11 122 cases with a positive RT-PCR test for SARS-cov-2 in Denmark: a nationwide cohort, Int J Epidemiol, doi:10.1093/ije/dyaa140
Ritsinger, Brismar, Malmberg, Elevated levels of adipokines predict outcome after acute myocardial infarction-a long-term follow up of the GAMI cohort, Diab Vasc Dis Res, doi:10.1177/1479164116678156
Seferović, Vardas, Jankowska, The heart failure association atlas: heart failure epidemiology and management statistics 2019, Eur J Heart Fail, doi:10.1002/ejhf.2143
Svensson, Hofmann, Häbel, Association between cardiometabolic disease and severe COVID-19: a nationwide casecontrol study of patients requiring invasive mechanical ventilation, BMJ Open, doi:10.1136/bmjopen-2020-044486
Szummer, Wallentin, Lindhagen, Improved outcomes in patients with ST-elevation myocardial infarction during the last 20 years are related to implementation of evidence-based treatments: experiences from the SWEDEHEART registry 1995-2014, Eur Heart J, doi:10.1093/eurheartj/ehx515
Szummer, Wallentin, Lindhagen, Relations between implementation of new treatments and improved outcomes in patients with non-ST-elevation myocardial infarction during the last 20 years: experiences from SWEDEHEART registry 1995 to 2014, Eur Heart J, doi:10.1093/eurheartj/ehy554
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using opensafely, Nature, doi:10.1038/s41586-020-2521-4
Yang, Dzayee, Beiki, Incidence and case fatality after day 28 of first time myocardial infarction in Sweden 1987-2008, Eur J Prev Cardiol, doi:10.1177/1741826711425340
Zarrinkoub, Wettermark, Wändell, The epidemiology of heart failure, based on data for 2.1 million inhabitants in Sweden, Eur J Heart Fail, doi:10.1093/eurjhf/hft064
DOI record:
{
"DOI": "10.1136/bmjopen-2022-069037",
"ISSN": [
"2044-6055",
"2044-6055"
],
"URL": "http://dx.doi.org/10.1136/bmjopen-2022-069037",
"abstract": "<jats:sec><jats:title>Objectives</jats:title><jats:p>To explore how cardiorenal disease (CRD; heart failure and/or chronic kidney disease) impacted mortality in men and women hospitalised for COVID-19 during the first three waves of the pandemic in Sweden in comparison to previous influenza outbreaks.</jats:p></jats:sec><jats:sec><jats:title>Design</jats:title><jats:p>A registry-based, retrospective, case–control study.</jats:p></jats:sec><jats:sec><jats:title>Setting</jats:title><jats:p>Hospital care in Sweden.</jats:p></jats:sec><jats:sec><jats:title>Participants</jats:title><jats:p>All patients in Sweden with a main hospital diagnosis of COVID‐19 (January 2020–September 2021) or influenza (January 2015–December 2019) with previous CRD were identified in registries and compared with a reference group free from CRD but with COVID-19 or influenza.</jats:p></jats:sec><jats:sec><jats:title>Primary outcome measure</jats:title><jats:p>Associated risk of all-cause death during the first year was analysed using adjusted Cox proportional hazards models.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>In COVID-19 patients with and without prior history of CRD (n=44 866), mean age was 79.8 years (SD 11.8) and 43% were women. In influenza patients (n=8897), mean age was 80.6 years (SD 11.5) and 45% were women. COVID-19 versus influenza was associated with higher mortality risk during the first two COVID-19 waves (HR 1.53; 95% CI 1.45 to 1.62, p<0.001 and HR 1.52; 95% CI 1.44 to 1.61, p<0.001), but not in the third wave (HR 1.07; 95% CI 0.99 to 1.14, p=0.072). CRD was an independent risk factor for all-cause death after COVID-19 in men and women (men: 1.37; 95% CI 1.31 to 1.44, p<0.001; women: 1.46; 95% CI 1.38 to 1.54, p<0.001). At ages <70 years, women with CRD had a similar mortality rate to men with CRD, while at ages ≥70 years, the mortality rate was higher in men.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>Outcome after COVID-19 is worse if CRD is present. In women at ages <70 years, the presence of CRD attenuates the protective effect of female sex. COVID-19 was associated with higher mortality risk than influenza during the first two pandemic waves.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjopen-2022-069037"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3385-4777",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ritsinger",
"given": "Viveca",
"sequence": "first"
},
{
"affiliation": [],
"family": "Bodegård",
"given": "Johan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kristofi",
"given": "Robin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thuresson",
"given": "Marcus",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nathanson",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nyström",
"given": "Thomas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Eriksson",
"given": "Jan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Norhammar",
"given": "Anna",
"sequence": "additional"
}
],
"container-title": "BMJ Open",
"container-title-short": "BMJ Open",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2023,
4,
28
]
],
"date-time": "2023-04-28T17:32:08Z",
"timestamp": 1682703128000
},
"deposited": {
"date-parts": [
[
2023,
4,
28
]
],
"date-time": "2023-04-28T17:32:29Z",
"timestamp": 1682703149000
},
"funder": [
{
"award": [
"N/A"
],
"name": "Family Kamprad Foundation"
},
{
"award": [
"N/A"
],
"name": "Department of Research and Development Region Kronoberg"
},
{
"DOI": "10.13039/100004325",
"award": [
"N/A"
],
"doi-asserted-by": "publisher",
"name": "AstraZeneca"
}
],
"indexed": {
"date-parts": [
[
2023,
4,
29
]
],
"date-time": "2023-04-29T04:32:39Z",
"timestamp": 1682742759043
},
"is-referenced-by-count": 0,
"issue": "4",
"issued": {
"date-parts": [
[
2023,
4
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2023,
4,
28
]
]
},
"published-print": {
"date-parts": [
[
2023,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 27,
"start": {
"date-parts": [
[
2023,
4,
28
]
],
"date-time": "2023-04-28T00:00:00Z",
"timestamp": 1682640000000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjopen-2022-069037",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e069037",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2023,
4
]
]
},
"published-online": {
"date-parts": [
[
2023,
4,
28
]
]
},
"published-print": {
"date-parts": [
[
2023,
4
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1001/jama.2020.1097",
"article-title": "The novel coronavirus originating in Wuhan, China: challenges for global health governance",
"author": "Phelan",
"doi-asserted-by": "crossref",
"first-page": "709",
"journal-title": "JAMA",
"key": "2023042810301895000_13.4.e069037.1",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2002032",
"doi-asserted-by": "publisher",
"key": "2023042810301895000_13.4.e069037.2"
},
{
"DOI": "10.1001/jamainternmed.2020.3539",
"article-title": "Risk factors associated with mortality among patients with covid-19 in intensive care units in lombardy, Italy",
"author": "Grasselli",
"doi-asserted-by": "crossref",
"first-page": "1345",
"journal-title": "JAMA Intern Med",
"key": "2023042810301895000_13.4.e069037.3",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"doi-asserted-by": "publisher",
"key": "2023042810301895000_13.4.e069037.4"
},
{
"DOI": "10.1093/ije/dyaa140",
"article-title": "Characteristics and predictors of hospitalization and death in the first 11 122 cases with a positive RT-PCR test for SARS-cov-2 in Denmark: a nationwide cohort",
"author": "Reilev",
"doi-asserted-by": "crossref",
"first-page": "1468",
"journal-title": "Int J Epidemiol",
"key": "2023042810301895000_13.4.e069037.5",
"volume": "49",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)31189-2",
"doi-asserted-by": "publisher",
"key": "2023042810301895000_13.4.e069037.6"
},
{
"DOI": "10.1136/bmjopen-2020-044486",
"doi-asserted-by": "crossref",
"key": "2023042810301895000_13.4.e069037.7",
"unstructured": "Svensson P , Hofmann R , Häbel H , et al . Association between cardiometabolic disease and severe COVID-19: a nationwide case-control study of patients requiring invasive mechanical ventilation. BMJ Open 2021;11:e044486. doi:10.1136/bmjopen-2020-044486"
},
{
"DOI": "10.1007/s10654-021-00732-w",
"doi-asserted-by": "publisher",
"key": "2023042810301895000_13.4.e069037.8"
},
{
"DOI": "10.1002/dmrr.3388",
"doi-asserted-by": "crossref",
"key": "2023042810301895000_13.4.e069037.9",
"unstructured": "Al-Salameh A , Lanoix JP , Bennis Y , et al . Characteristics and outcomes of COVID-19 in hospitalized patients with and without diabetes. Diabetes Metab Res Rev 2021;37:e3388. doi:10.1002/dmrr.3388"
},
{
"DOI": "10.1016/j.lanepe.2021.100105",
"doi-asserted-by": "crossref",
"key": "2023042810301895000_13.4.e069037.10",
"unstructured": "Rawshani A , Kjölhede EA , Rawshani A , et al . Severe COVID-19 in people with type 1 and type 2 diabetes in Sweden: a nationwide retrospective cohort study. Lancet Reg Health Eur 2021;4:100105. doi:10.1016/j.lanepe.2021.100105"
},
{
"DOI": "10.1016/S2213-8587(20)30272-2",
"article-title": "Associations of type 1 and type 2 diabetes with covid-19-related mortality in England: a whole-population study",
"author": "Barron",
"doi-asserted-by": "crossref",
"first-page": "813",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2023042810301895000_13.4.e069037.11",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"article-title": "Risk factors for covid-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study",
"author": "Holman",
"doi-asserted-by": "crossref",
"first-page": "823",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2023042810301895000_13.4.e069037.12",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1161/CIR.0000000000000664",
"article-title": "American heart association Council on the kidney in cardiovascular disease and Council on clinical cardiology. cardiorenal syndrome: classification, pathophysiology, diagnosis, and treatment strategies: a scientific statement from the American heart association",
"author": "Rangaswami",
"doi-asserted-by": "crossref",
"first-page": "e840",
"journal-title": "Circulation",
"key": "2023042810301895000_13.4.e069037.13",
"volume": "139",
"year": "2019"
},
{
"DOI": "10.1002/ejhf.2143",
"article-title": "The heart failure association atlas: heart failure epidemiology and management statistics 2019",
"author": "Seferović",
"doi-asserted-by": "crossref",
"first-page": "906",
"journal-title": "Eur J Heart Fail",
"key": "2023042810301895000_13.4.e069037.14",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1093/eurjhf/hft064",
"doi-asserted-by": "publisher",
"key": "2023042810301895000_13.4.e069037.15"
},
{
"DOI": "10.1093/ndt/gfw354",
"doi-asserted-by": "publisher",
"key": "2023042810301895000_13.4.e069037.16"
},
{
"DOI": "10.1016/S2213-2600(20)30527-0",
"article-title": "Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study",
"author": "Piroth",
"doi-asserted-by": "crossref",
"first-page": "251",
"journal-title": "Lancet Respir Med",
"key": "2023042810301895000_13.4.e069037.17",
"volume": "9",
"year": "2021"
},
{
"key": "2023042810301895000_13.4.e069037.18",
"unstructured": "The public health agency of Sweden. n.d. Available: https://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/statistikdatabaser-och-visualisering/vaccinationsstatistik/statistik-for-influensavaccinationer"
},
{
"DOI": "10.1177/1741826711425340",
"doi-asserted-by": "publisher",
"key": "2023042810301895000_13.4.e069037.19"
},
{
"DOI": "10.1093/eurheartj/ehx515",
"article-title": "Improved outcomes in patients with ST-elevation myocardial infarction during the last 20 years are related to implementation of evidence-based treatments: experiences from the SWEDEHEART registry 1995-2014",
"author": "Szummer",
"doi-asserted-by": "crossref",
"first-page": "3056",
"journal-title": "Eur Heart J",
"key": "2023042810301895000_13.4.e069037.20",
"volume": "38",
"year": "2017"
},
{
"DOI": "10.1093/eurheartj/ehy554",
"article-title": "Relations between implementation of new treatments and improved outcomes in patients with non-ST-elevation myocardial infarction during the last 20 years: experiences from SWEDEHEART registry 1995 to 2014",
"author": "Szummer",
"doi-asserted-by": "crossref",
"first-page": "3766",
"journal-title": "Eur Heart J",
"key": "2023042810301895000_13.4.e069037.21",
"volume": "39",
"year": "2018"
},
{
"DOI": "10.1016/j.kint.2019.02.022",
"article-title": "Heart failure in chronic kidney disease: conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference",
"author": "House",
"doi-asserted-by": "crossref",
"first-page": "1304",
"journal-title": "Kidney Int",
"key": "2023042810301895000_13.4.e069037.22",
"volume": "95",
"year": "2019"
},
{
"DOI": "10.1016/j.jamda.2021.06.010",
"doi-asserted-by": "publisher",
"key": "2023042810301895000_13.4.e069037.23"
},
{
"DOI": "10.1177/1479164116678156",
"article-title": "Elevated levels of adipokines predict outcome after acute myocardial infarction-a long-term follow up of the GAMI cohort",
"author": "Ritsinger",
"doi-asserted-by": "crossref",
"first-page": "77",
"journal-title": "Diab Vasc Dis Res",
"key": "2023042810301895000_13.4.e069037.24",
"volume": "14",
"year": "2017"
}
],
"reference-count": 24,
"references-count": 24,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2022-069037"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "History of heart failure and chronic kidney disease and risk of all-cause death after COVID-19 during the first three waves of the pandemic in comparison with influenza outbreaks in Sweden: a registry-based, retrospective, case–control study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "13"
}