Smoking Status and Factors associated with COVID-19 In-Hospital Mortality among US Veterans
et al., Nicotine & Tobacco Research, doi:10.1093/ntr/ntab223, Oct 2021
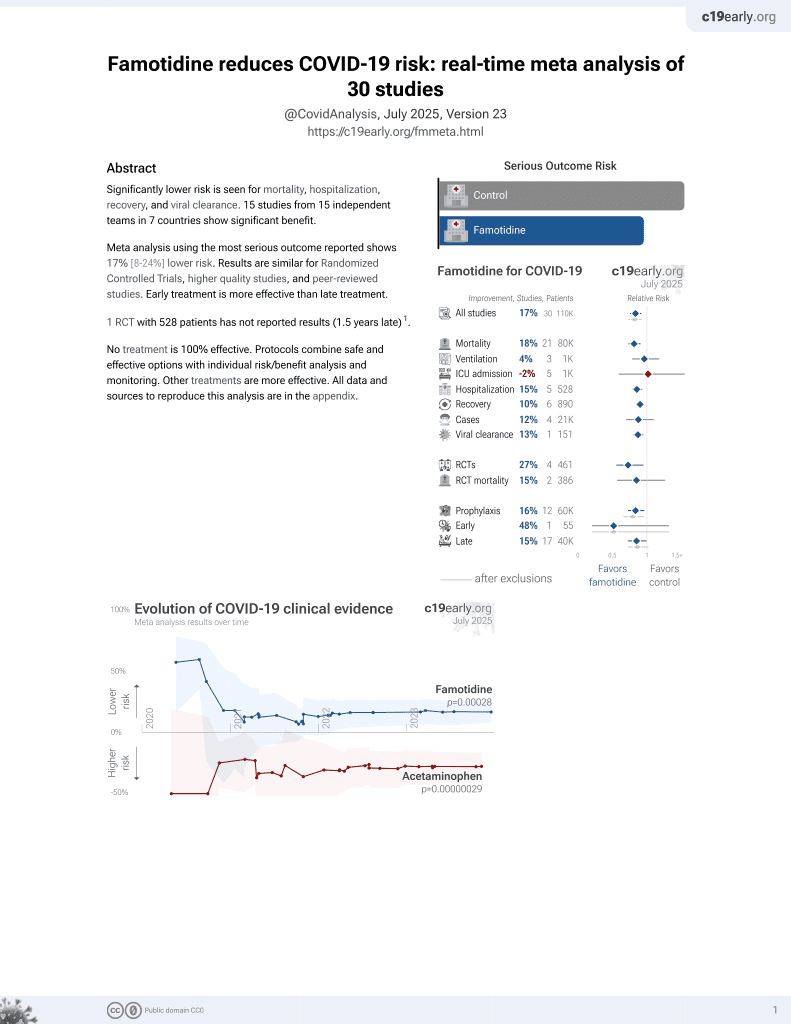
Famotidine for COVID-19
29th treatment shown to reduce risk in
October 2021, now with p = 0.00028 from 30 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 10,074 hospitalized veterans with COVID-19 in the USA, showing lower mortality with existing famotidine use.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
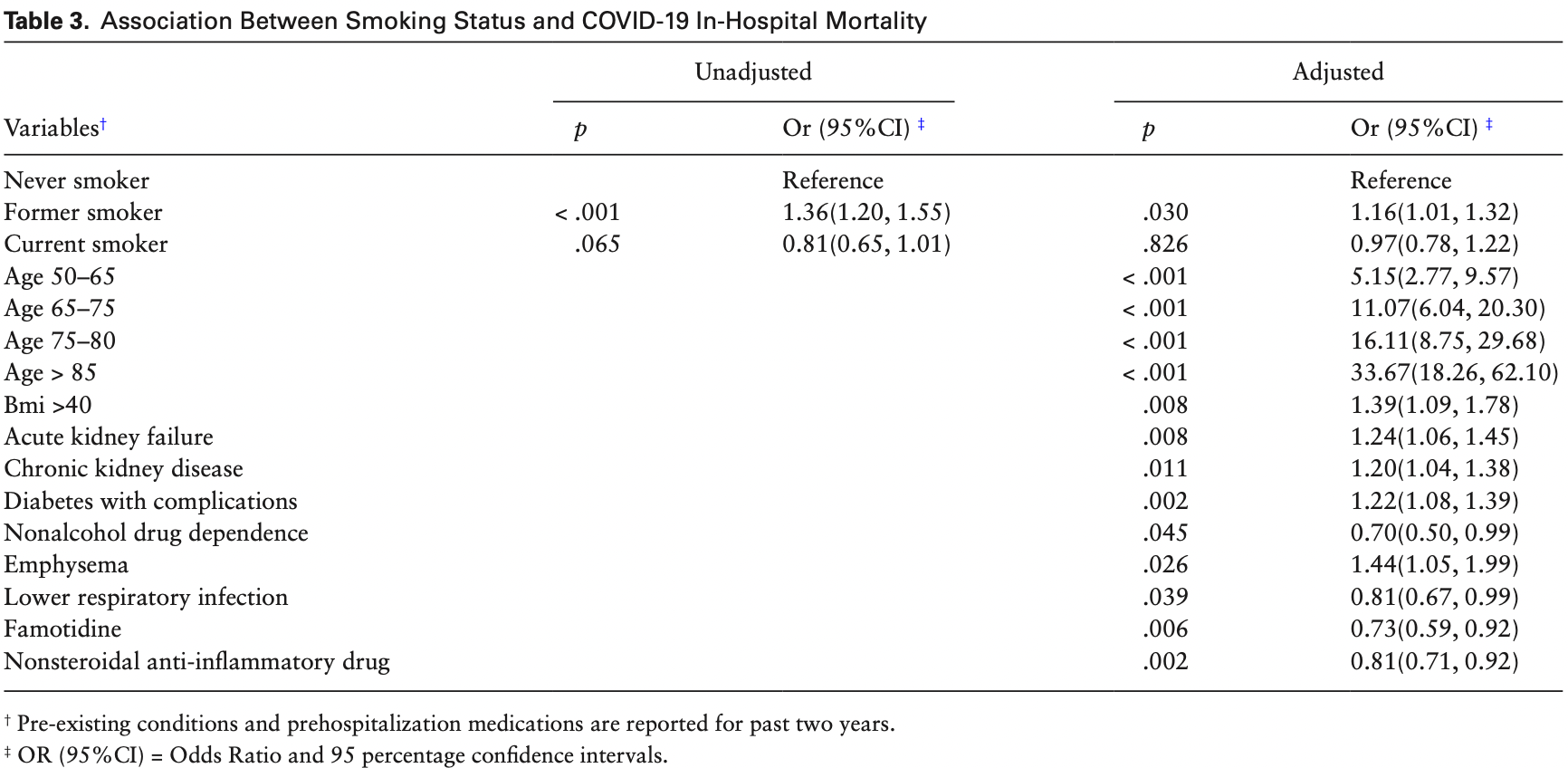
risk of death, 27.0% lower, OR 0.73, p = 0.006, treatment 93, control 9,981, adjusted per study, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Razjouyan et al., 25 Oct 2021, retrospective, USA, peer-reviewed, 7 authors.
Smoking Status and Factors associated with COVID-19 In-Hospital Mortality among US Veterans
Nicotine & Tobacco Research, doi:10.1093/ntr/ntab223
Introduction: The role of smoking in risk of death among patients with COVID-19 remains unclear. We examined the association between in-hospital mortality from COVID-19 and smoking status and other factors in the United States Veterans Health Administration (VHA). Methods: This is an observational, retrospective cohort study using the VHA COVID-19 shared data resources for February 1 to September 11, 2020. Veterans admitted to the hospital who tested positive for SARS-CoV-2 and hospitalized by VHA were grouped into Never (as reference, NS), Former (FS), and Current smokers (CS). The main outcome was in-hospital mortality. Control factors were the most important variables (among all available) determined through a cascade of machine learning. We reported adjusted odds ratios (aOR) and 95% confidence intervals (95%CI) from logistic regression models, imputing missing smoking status in our primary analysis. Results: Out of 8 667 996 VHA enrollees, 505 143 were tested for SARS-CoV-2 (NS = 191 143; FS = 240 336; CS = 117 706; Unknown = 45 533). The aOR of in-hospital mortality was 1.16 (95%CI 1.01, 1.32) for FS vs. NS and 0.97 (95%CI 0.78, 1.22; p > .05) for CS vs. NS with imputed smoking status. Among other factors, famotidine and nonsteroidal anti-inflammatory drugs (NSAID) use before hospitalization were associated with lower risk while diabetes with complications, kidney disease, obesity, and advanced age were associated with higher risk of in-hospital mortality. Conclusions: In patients admitted to the hospital with SARS-CoV-2 infection, our data demonstrate that FS are at higher risk of in-hospital mortality than NS. However, this pattern was not seen Published by Oxford University Press on behalf of the Society for Research on Nicotine and Tobacco 2021. This work is written by (a) US Government employee(s) and is in the public domain in the US.
Supplementary Material A Contributorship Form detailing each author's specific involvement with this content, as well as any supplementary data, are available online at https:// academic.oup.com/ntr.
Declaration of Interests The authors do not have any competing interest.
References
Akl, Gaddam, Gunukula, Honeine, Jaoude et al., The effects of waterpipe tobacco smoking on health outcomes: a systematic review, Int J Epidemiol
Azur, Stuart, Frangakis, Leaf, Multiple imputation by chained equations: what is it and how does it work?, Int J Methods Psychiatr Res, doi:10.1002/mpr.329
Bhandari, Rankawat, Singh, Gupta, Kakkar, Impact of glycemic control in diabetes mellitus on management of COVID-19 infection
Bhargava, Kim, Quine, Hauser, A 20-year evaluation of LOINC in the United States' largest integrated health system, Arch Pathol Lab Med
Cai, Bossé, Xiao, Kheradmand, Amos, Tobacco smoking increases the lung gene expression of ACE2, the receptor of SARS-CoV-2, Am J Respir Crit Care Med
Calhoun, Wilson, Hertzberg, VA Mid-Atlantic MIRECC Workgroup. Validation of veterans affairs electronic medical record smoking data among Iraq-and Afghanistan-era veterans, J Gen Intern Med
Charlson, Szatrowski, Peterson, Gold, Validation of a combined comorbidity index, J Clin Epidemiol
Covid Tc, Team, Severe outcomes among patients with Coronavirus Disease 2019 (COVID-19)-United States, MMWR Morb Mortal Wkly Rep
Del Sole, Farcomeni, Loffredo, Features of severe COVID-19: A systematic review and meta-analysis, Eur J Clin Invest
Duvall, Introduction to the VA COVID-19 Shared Data Resource and its Use for Research
Farsalinos, Angelopoulou, Alexandris, Poulas, COVID-19 and the nicotinic cholinergic system, Eur Respir J, doi:10.1183/13993003.01589-2020
Freedberg, Conigliaro, Wang, Tracey, Callahan et al., Famotidine use is associated with improved clinical outcomes in hospitalized COVID-19 patients: a propensity score matched retrospective cohort study, Gastroenterology
Golden, Hooker, Shull, Validity of Veterans Health Administration structured data to determine accurate smoking status, Health Informatics J
Hasan, Paray, Hussain, A review on the cleavage priming of the spike protein on coronavirus by angiotensin-converting enzyme-2 and furin, J Biomol Struct Dyn
Health Organization, The use of non-steroidal anti-inflammatory drugs (NSAIDs) in patients with COVID-19: scientific brief, doi:10.1007/s40615-021-00982-0
Higham, Mathioudakis, Vestbo, Singh, COVID-19 and COPD: a narrative review of the basic science and clinical outcomes, Eur Respir Rev, doi:10.1183/16000617.0199-2020
Hussain, Mahawar, Xia, Yang, El-Hasani, Obesity and mortality of COVID-19. Meta-analysis, Obes Res Clin Pract
Kickbusch, Leung, Response to the emerging novel coronavirus outbreak, BMJ
Lagoumintzis, Chasapis, Alexandris, Nicotinic cholinergic system and COVID-19: In silico identification of interactions between α7 nicotinic acetylcholine receptor and the cryptic epitopes of SARS-Co-V and SARS-CoV-2 Spike glycoproteins, Food Chem Toxicol
Leung, Niikura, Yang, Sin, COVID-19 and COPD, Eur Respir J, doi:10.1183/13993003.02108-2020
Leung, Yang, Sin, COVID-19 and nicotine as a mediator of ACE-2, Eur Respir J, doi:10.1183/13993003.01261-2020
Levin, Hanage, Owusu-Boaitey, Cochran, Walsh et al., Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications, Eur J Epidemiol, doi:10.1007/s40615-021-00982-0
Luo, Jeyapalina, Stoddard, Kwok, Agarwal, Coronavirus disease 2019 in veterans receiving care at veterans health administration facilities, Ann Epidemiol
Martinez, Han, Allinson, At the root: defining and halting progression of early chronic obstructive pulmonary disease, Am J Respir Crit Care Med
Mather, Seip, Mckay, Impact of famotidine use on clinical outcomes of hospitalized patients with COVID-19, Am J Gastroenterol
Maynard, Ascertaining Veterans' Vital Status: VA data sources for mortality ascertainment and cause of death
Mcginnis, Brandt, Skanderson, Validating smoking data from the Veteran's Affairs Health Factors dataset, an electronic data source, Nicotine Tob Res
Murphy, Rohsenow, Johnson, Wing, Smoking and weight loss among smokers with overweight and obesity in Look AHEAD, Health Psychol
Neira, Watts, Seashore, Polychronopoulou, Kuo et al., Smoking and risk of COVID-19 hospitalization, Respir Med
Oliveira, Ibarra, Bermudez, A potential interaction between the SARS-CoV-2 spike protein and nicotinic acetylcholine receptors, Biophys J, doi:10.1183/13993003.01589-2020
Pal, Banerjee, Are people with uncontrolled diabetes mellitus at high risk of reinfections with COVID-19?, Prim Care Diabetes
Pettit, Mackenzie, Ridgway, Obesity is associated with increased risk for mortality among hospitalized patients with COVID-19, Obesity
Polverino, Cigarette smoking and COVID-19: a complex interaction, Am J Respir Crit Care Med
Razjouyan, Helmer, Li, Differences in COVID-19-related testing and healthcare utilization by race and ethnicity in the veterans health administration
Reddy, Charles, Sklavounos, Dutt, Seed et al., The effect of smoking on COVID-19 severity: a systematic review and metaanalysis, J Med Virol
Ryu, Colby, Hartman, Vassallo, Smoking-related interstitial lung diseases: a concise review, Eur Respir J
Shahid, Kalayanamitra, Mcclafferty, COVID-19 and older adults: what we know, J Am Geriatr Soc
Sharma, Estimating older adult mortality from COVID-19, J Gerontol B Psychol Sci Soc Sci
Sy, Qian, King, Outcomes for patients With COVID-19 and acute kidney injury: a systematic review and metaanalysis, Kidney Int Rep, doi:10.1183/13993003.02108-2020
Tang, Alelyani, Liu, Feature selection for classification: A review
Tartof, Qian, Hong, Obesity and mortality among patients diagnosed with COVID-19: results from an integrated health care organization, Ann Intern Med
Vardavas, Nikitara, COVID-19 and smoking: a systematic review of the evidence, Tob Induc Dis, doi:10.1183/13993003.01261-2020
Viernes, Lynch, Robison, Gatsby, Duvall et al., SNOMED CT Disease Hierarchies and the Charlson Comorbidity Index (CCI): An analysis of OHDSI methods for determining CCI
Vosu, Britton, Is the risk of ibuprofen or other non-steroidal anti-inflammatory drugs increased in COVID-19?, J Paediatr Child Health
Williams, Jylhävä, Pedersen, Hägg, A Frailty index for UK biobank participants, J Gerontol A Biol Sci Med Sci
Wulff, Ejlskov, Multiple imputation by chained equations in praxis: guidelines and review, Electron J Bus Res Methods
DOI record:
{
"DOI": "10.1093/ntr/ntab223",
"ISSN": [
"1469-994X"
],
"URL": "http://dx.doi.org/10.1093/ntr/ntab223",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:sec>\n <jats:title>Introduction</jats:title>\n <jats:p>The role of smoking in risk of death among patients with COVID-19 remains unclear. We examined the association between in-hospital mortality from COVID-19 and smoking status and other factors in the United States Veterans Health Administration (VHA).</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>This is an observational, retrospective cohort study using the VHA COVID-19 shared data resources for February 1 to September 11, 2020. Veterans admitted to the hospital who tested positive for SARS-CoV-2 and hospitalized by VHA were grouped into Never (as reference, NS), Former (FS), and Current smokers (CS). The main outcome was in-hospital mortality. Control factors were the most important variables (among all available) determined through a cascade of machine learning. We reported adjusted odds ratios (aOR) and 95% confidence intervals (95%CI) from logistic regression models, imputing missing smoking status in our primary analysis.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Out of 8 667 996 VHA enrollees, 505 143 were tested for SARS-CoV-2 (NS = 191 143; FS = 240 336; CS = 117 706; Unknown = 45 533). The aOR of in-hospital mortality was 1.16 (95%CI 1.01, 1.32) for FS vs. NS and 0.97 (95%CI 0.78, 1.22; p &gt; .05) for CS vs. NS with imputed smoking status. Among other factors, famotidine and nonsteroidal anti-inflammatory drugs (NSAID) use before hospitalization were associated with lower risk while diabetes with complications, kidney disease, obesity, and advanced age were associated with higher risk of in-hospital mortality.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>In patients admitted to the hospital with SARS-CoV-2 infection, our data demonstrate that FS are at higher risk of in-hospital mortality than NS. However, this pattern was not seen among CS highlighting the need for more granular analysis with high-quality smoking status data to further clarify our understanding of smoking risk and COVID-19-related mortality. Presence of comorbidities and advanced age were also associated with increased risk of in-hospital mortality.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Implications</jats:title>\n <jats:p>Veterans who were former smokers were at higher risk of in-hospital mortality compared to never smokers. Current smokers and never smokers were at similar risk of in-hospital mortality. The use of famotidine and nonsteroidal anti-inflammatory drugs (NSAIDs) before hospitalization were associated with lower risk while uncontrolled diabetes mellitus, advanced age, kidney disease, and obesity were associated with higher risk of in-hospital mortality.</jats:p>\n </jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0003-1157-159X",
"affiliation": [
{
"name": "VA HSR&D Center for Innovations in Quality, Effectiveness and Safety, Michael E. DeBakey VA Medical Center, Houston, TX, USA"
},
{
"name": "Department of Medicine, Baylor College of Medicine, Houston, TX, USA"
},
{
"name": "VA Quality Scholars Coordinating Center, IQuESt, Michael E. DeBakey VA Medical Center, Houston, TX, USA"
},
{
"name": "Big Data Scientist Training Enhancement Program (BD-STEP), VA Office of Research and Development, Washington, DC, USA"
}
],
"authenticated-orcid": false,
"family": "Razjouyan",
"given": "Javad",
"sequence": "first"
},
{
"affiliation": [
{
"name": "VA HSR&D Center for Innovations in Quality, Effectiveness and Safety, Michael E. DeBakey VA Medical Center, Houston, TX, USA"
},
{
"name": "Department of Medicine, Baylor College of Medicine, Houston, TX, USA"
}
],
"family": "Helmer",
"given": "Drew A",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "VA Salt Lake City Health Care System and Division of Epidemiology, University of Utah, Salt Lake City, UT, USA"
}
],
"family": "Lynch",
"given": "Kristine E",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "VA Salt Lake City Health Care System and Department of Internal Medicine, University of Utah School of Medicine, Salt Lake City, UT, USA"
}
],
"family": "Hanania",
"given": "Nicola A",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Integrative Molecular and Biomedical Sciences Program, Baylor College of Medicine, Houston, TX, USA"
},
{
"name": "Margaret M. and Albert B. Alkek Department of Medicine, Nephrology, Baylor College of Medicine, Houston, TX, USA"
}
],
"family": "Klotman",
"given": "Paul E",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "VA HSR&D Center for Innovations in Quality, Effectiveness and Safety, Michael E. DeBakey VA Medical Center, Houston, TX, USA"
},
{
"name": "Department of Medicine, Baylor College of Medicine, Houston, TX, USA"
},
{
"name": "Medical Care Line, Section of Pulmonary, Critical Care and Sleep Medicine, Michael E. DeBakey VA Medical Center, Houston, TX, USA"
}
],
"family": "Sharafkhaneh",
"given": "Amir",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8540-7023",
"affiliation": [
{
"name": "Department of Medicine, Baylor College of Medicine, Houston, TX, USA"
}
],
"authenticated-orcid": false,
"family": "Amos",
"given": "Christopher I",
"sequence": "additional"
}
],
"container-title": [
"Nicotine & Tobacco Research"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
10,
20
]
],
"date-time": "2021-10-20T22:47:57Z",
"timestamp": 1634770077000
},
"deposited": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T04:34:32Z",
"timestamp": 1638333272000
},
"funder": [
{
"DOI": "10.13039/100015620",
"award": [
"CIN 13–413"
],
"doi-asserted-by": "publisher",
"name": "Center for Innovations in Quality, Effectiveness and Safety"
},
{
"DOI": "10.13039/100000050",
"award": [
"1K25HL152006-01"
],
"doi-asserted-by": "publisher",
"name": "National Heart, Lung, and Blood Institute"
}
],
"indexed": {
"date-parts": [
[
2022,
1,
4
]
],
"date-time": "2022-01-04T05:39:05Z",
"timestamp": 1641274745984
},
"is-referenced-by-count": 1,
"issn-type": [
{
"type": "electronic",
"value": "1469-994X"
}
],
"issued": {
"date-parts": [
[
2021,
10,
25
]
]
},
"language": "en",
"link": [
{
"URL": "https://academic.oup.com/ntr/advance-article-pdf/doi/10.1093/ntr/ntab223/41274375/ntab223.pdf",
"content-type": "application/pdf",
"content-version": "am",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/ntr/advance-article-pdf/doi/10.1093/ntr/ntab223/41274375/ntab223.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "286",
"original-title": [],
"prefix": "10.1093",
"published": {
"date-parts": [
[
2021,
10,
25
]
]
},
"published-online": {
"date-parts": [
[
2021,
10,
25
]
]
},
"publisher": "Oxford University Press (OUP)",
"reference": [
{
"DOI": "10.1164/rccm.202005-1646LE",
"article-title": "Cigarette smoking and COVID-19: a complex interaction",
"author": "Polverino",
"doi-asserted-by": "crossref",
"first-page": "471",
"issue": "3",
"journal-title": "Am J Respir Crit Care Med.",
"key": "2021120104020554600_CIT0001",
"volume": "202",
"year": "2020"
},
{
"DOI": "10.1093/ije/dyq002",
"article-title": "The effects of waterpipe tobacco smoking on health outcomes: a systematic review",
"author": "Akl",
"doi-asserted-by": "crossref",
"first-page": "834",
"issue": "3",
"journal-title": "Int J Epidemiol.",
"key": "2021120104020554600_CIT0002",
"volume": "39",
"year": "2010"
},
{
"DOI": "10.1183/09031936.01.17101220",
"article-title": "Smoking-related interstitial lung diseases: a concise review",
"author": "Ryu",
"doi-asserted-by": "crossref",
"first-page": "122",
"issue": "1",
"journal-title": "Eur Respir J.",
"key": "2021120104020554600_CIT0003",
"volume": "17",
"year": "2001"
},
{
"DOI": "10.1037/hea0000607",
"article-title": "Smoking and weight loss among smokers with overweight and obesity in Look AHEAD",
"author": "Murphy",
"doi-asserted-by": "crossref",
"first-page": "399",
"issue": "5",
"journal-title": "Health Psychol.",
"key": "2021120104020554600_CIT0004",
"volume": "37",
"year": "2018"
},
{
"DOI": "10.7326/M20-3742",
"article-title": "Obesity and mortality among patients diagnosed with COVID-19: results from an integrated health care organization",
"author": "Tartof",
"doi-asserted-by": "crossref",
"first-page": "773",
"issue": "10",
"journal-title": "Ann Intern Med.",
"key": "2021120104020554600_CIT0005",
"volume": "173",
"year": "2020"
},
{
"DOI": "10.1183/13993003.01589-2020",
"article-title": "COVID-19 and the nicotinic cholinergic system",
"author": "Farsalinos",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "Eur Respir J.",
"key": "2021120104020554600_CIT0006",
"volume": "56",
"year": "2020"
},
{
"DOI": "10.1016/j.bpj.2021.01.037",
"article-title": "A potential interaction between the SARS-CoV-2 spike protein and nicotinic acetylcholine receptors",
"author": "Oliveira",
"doi-asserted-by": "crossref",
"first-page": "983",
"issue": "6",
"journal-title": "Biophys J.",
"key": "2021120104020554600_CIT0007",
"volume": "120",
"year": "2021"
},
{
"DOI": "10.1183/13993003.01261-2020",
"article-title": "COVID-19 and nicotine as a mediator of ACE-2",
"author": "Leung",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "Eur Respir J.",
"key": "2021120104020554600_CIT0008",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m406",
"article-title": "Response to the emerging novel coronavirus outbreak",
"author": "Kickbusch",
"doi-asserted-by": "crossref",
"first-page": "m406",
"journal-title": "BMJ.",
"key": "2021120104020554600_CIT0009",
"volume": "368",
"year": "2020"
},
{
"DOI": "10.18332/tid/119324",
"article-title": "COVID-19 and smoking: a systematic review of the evidence",
"author": "Vardavas",
"doi-asserted-by": "crossref",
"first-page": "20",
"journal-title": "Tob Induc Dis.",
"key": "2021120104020554600_CIT0010",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26389",
"article-title": "The effect of smoking on COVID-19 severity: a systematic review and meta-analysis",
"author": "Reddy",
"doi-asserted-by": "crossref",
"first-page": "1045",
"issue": "2",
"journal-title": "J Med Virol.",
"key": "2021120104020554600_CIT0011",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1016/j.fct.2021.112009",
"article-title": "Nicotinic cholinergic system and COVID-19: In silico identification of interactions between α7 nicotinic acetylcholine receptor and the cryptic epitopes of SARS-Co-V and SARS-CoV-2 Spike glycoproteins",
"author": "Lagoumintzis",
"doi-asserted-by": "crossref",
"first-page": "112009",
"journal-title": "Food Chem Toxicol.",
"key": "2021120104020554600_CIT0012",
"volume": "149",
"year": "2021"
},
{
"DOI": "10.1016/j.rmed.2021.106414",
"article-title": "Smoking and risk of COVID-19 hospitalization",
"author": "Puebla Neira",
"doi-asserted-by": "crossref",
"first-page": "106414",
"journal-title": "Respir Med.",
"key": "2021120104020554600_CIT0013",
"volume": "182",
"year": "2021"
},
{
"author": "Development OoR",
"key": "2021120104020554600_CIT0014",
"year": "2020"
},
{
"DOI": "10.5858/arpa.2019-0055-OA",
"article-title": "A 20-year evaluation of LOINC in the United States’ largest integrated health system",
"author": "Bhargava",
"doi-asserted-by": "crossref",
"first-page": "478",
"issue": "4",
"journal-title": "Arch Pathol Lab Med.",
"key": "2021120104020554600_CIT0015",
"volume": "144",
"year": "2020"
},
{
"author": "Development OoR",
"key": "2021120104020554600_CIT0016",
"year": "2020"
},
{
"DOI": "10.1016/j.annepidem.2020.12.003",
"article-title": "Coronavirus disease 2019 in veterans receiving care at veterans health administration facilities",
"author": "Luo",
"doi-asserted-by": "crossref",
"first-page": "10",
"journal-title": "Ann Epidemiol.",
"key": "2021120104020554600_CIT0017",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.1007/s11606-017-4144-5",
"article-title": "Validation of veterans affairs electronic medical record smoking data among Iraq- and Afghanistan-era veterans",
"author": "Calhoun",
"doi-asserted-by": "crossref",
"first-page": "1228",
"issue": "11",
"journal-title": "J Gen Intern Med.",
"key": "2021120104020554600_CIT0018",
"volume": "32",
"year": "2017"
},
{
"DOI": "10.1177/1460458219882259",
"article-title": "Validity of Veterans Health Administration structured data to determine accurate smoking status",
"author": "Golden",
"doi-asserted-by": "crossref",
"first-page": "1507",
"issue": "3",
"journal-title": "Health Informatics J.",
"key": "2021120104020554600_CIT0019",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1093/ntr/ntr206",
"article-title": "Validating smoking data from the Veteran’s Affairs Health Factors dataset, an electronic data source",
"author": "McGinnis",
"doi-asserted-by": "crossref",
"first-page": "1233",
"issue": "12",
"journal-title": "Nicotine Tob Res.",
"key": "2021120104020554600_CIT0020",
"volume": "13",
"year": "2011"
},
{
"author": "Maynard",
"key": "2021120104020554600_CIT0021",
"volume-title": "Ascertaining Veterans’ Vital Status: VA data sources for mortality ascertainment and cause of death",
"year": "2017"
},
{
"DOI": "10.1093/gerona/gly094",
"article-title": "A Frailty index for UK biobank participants",
"author": "Williams",
"doi-asserted-by": "crossref",
"first-page": "582",
"issue": "4",
"journal-title": "J Gerontol A Biol Sci Med Sci.",
"key": "2021120104020554600_CIT0022",
"volume": "74",
"year": "2019"
},
{
"DOI": "10.1002/mpr.329",
"article-title": "Multiple imputation by chained equations: what is it and how does it work?",
"author": "Azur",
"doi-asserted-by": "crossref",
"first-page": "40",
"issue": "1",
"journal-title": "Int J Methods Psychiatr Res.",
"key": "2021120104020554600_CIT0023",
"volume": "20",
"year": "2011"
},
{
"article-title": "Multiple imputation by chained equations in praxis: guidelines and review",
"author": "Wulff",
"issue": "1",
"journal-title": "Electron J Bus Res Methods",
"key": "2021120104020554600_CIT0024",
"volume": "15",
"year": "2017"
},
{
"author": "Scott DuVall",
"key": "2021120104020554600_CIT0025",
"volume-title": "Introduction to the VA COVID-19 Shared Data Resource and its Use for Research",
"year": "2020"
},
{
"DOI": "10.1016/0895-4356(94)90129-5",
"article-title": "Validation of a combined comorbidity index",
"author": "Charlson",
"doi-asserted-by": "crossref",
"first-page": "1245",
"issue": "11",
"journal-title": "J Clin Epidemiol.",
"key": "2021120104020554600_CIT0026",
"volume": "47",
"year": "1994"
},
{
"author": "Viernes",
"key": "2021120104020554600_CIT0027"
},
{
"article-title": "Feature selection for classification: A review.",
"author": "Tang",
"key": "2021120104020554600_CIT0028",
"volume-title": "Data classification: Algorithms and applications"
},
{
"DOI": "10.1111/eci.13378",
"article-title": "Features of severe COVID-19: A systematic review and meta-analysis",
"author": "Del Sole",
"doi-asserted-by": "crossref",
"first-page": "e13378",
"issue": "10",
"journal-title": "Eur J Clin Invest.",
"key": "2021120104020554600_CIT0029",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1080/07391102.2020.1754293",
"article-title": "A review on the cleavage priming of the spike protein on coronavirus by angiotensin-converting enzyme-2 and furin",
"author": "Hasan",
"doi-asserted-by": "crossref",
"first-page": "3025",
"issue": "8",
"journal-title": "J Biomol Struct Dyn.",
"key": "2021120104020554600_CIT0030",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.1164/rccm.202003-0693LE",
"article-title": "Tobacco smoking increases the lung gene expression of ACE2, the receptor of SARS-CoV-2",
"author": "Cai",
"doi-asserted-by": "crossref",
"first-page": "1557",
"issue": "12",
"journal-title": "Am J Respir Crit Care Med.",
"key": "2021120104020554600_CIT0031",
"volume": "201",
"year": "2020"
},
{
"DOI": "10.1164/rccm.201710-2028PP",
"article-title": "At the root: defining and halting progression of early chronic obstructive pulmonary disease",
"author": "Martinez",
"doi-asserted-by": "crossref",
"first-page": "1540",
"issue": "12",
"journal-title": "Am J Respir Crit Care Med.",
"key": "2021120104020554600_CIT0032",
"volume": "197",
"year": "2018"
},
{
"author": "CDC",
"key": "2021120104020554600_CIT0033",
"year": "2020"
},
{
"article-title": "Differences in COVID-19-related testing and healthcare utilization by race and ethnicity in the veterans health administration",
"author": "Razjouyan",
"key": "2021120104020554600_CIT0034"
},
{
"DOI": "10.1007/s10654-020-00698-1",
"article-title": "Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications",
"author": "Levin",
"doi-asserted-by": "crossref",
"first-page": "1123",
"issue": "12",
"journal-title": "Eur J Epidemiol.",
"key": "2021120104020554600_CIT0035",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6912e2",
"article-title": "Severe outcomes among patients with Coronavirus Disease 2019 (COVID-19)-United States, February 12-March 16, 2020",
"author": "COVID TC, Team R",
"doi-asserted-by": "crossref",
"first-page": "343",
"issue": "12",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "2021120104020554600_CIT0036",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1093/geronb/gbaa161",
"article-title": "Estimating older adult mortality from COVID-19",
"author": "Sharma",
"doi-asserted-by": "crossref",
"first-page": "e68",
"issue": "3",
"journal-title": "J Gerontol B Psychol Sci Soc Sci.",
"key": "2021120104020554600_CIT0037",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1111/jgs.16472",
"article-title": "COVID-19 and older adults: what we know",
"author": "Shahid",
"doi-asserted-by": "crossref",
"first-page": "926",
"issue": "5",
"journal-title": "J Am Geriatr Soc.",
"key": "2021120104020554600_CIT0038",
"volume": "68",
"year": "2020"
},
{
"author": "CDC",
"key": "2021120104020554600_CIT0039",
"year": "2021"
},
{
"DOI": "10.1016/j.orcp.2020.07.002",
"article-title": "Obesity and mortality of COVID-19. Meta-analysis",
"author": "Hussain",
"doi-asserted-by": "crossref",
"first-page": "295",
"issue": "4",
"journal-title": "Obes Res Clin Pract.",
"key": "2021120104020554600_CIT0040",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1002/oby.22941",
"article-title": "Obesity is associated with increased risk for mortality among hospitalized patients with COVID-19",
"author": "Pettit",
"doi-asserted-by": "crossref",
"first-page": "1806",
"issue": "10",
"journal-title": "Obesity",
"key": "2021120104020554600_CIT0041",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1007/s13410-020-00868-7",
"article-title": "Impact of glycemic control in diabetes mellitus on management of COVID-19 infection",
"author": "Bhandari",
"doi-asserted-by": "crossref",
"key": "2021120104020554600_CIT0042"
},
{
"DOI": "10.1016/j.pcd.2020.08.002",
"article-title": "Are people with uncontrolled diabetes mellitus at high risk of reinfections with COVID-19?",
"author": "Pal",
"doi-asserted-by": "crossref",
"first-page": "18",
"issue": "1",
"journal-title": "Prim Care Diabetes.",
"key": "2021120104020554600_CIT0043",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1183/16000617.0199-2020",
"article-title": "COVID-19 and COPD: a narrative review of the basic science and clinical outcomes",
"author": "Higham",
"doi-asserted-by": "crossref",
"issue": "158",
"journal-title": "Eur Respir Rev",
"key": "2021120104020554600_CIT0044",
"volume": "29",
"year": "2020"
},
{
"DOI": "10.1183/13993003.02108-2020",
"article-title": "COVID-19 and COPD",
"author": "Leung",
"doi-asserted-by": "crossref",
"issue": "2",
"journal-title": "Eur Respir J",
"key": "2021120104020554600_CIT0045",
"volume": "56",
"year": "2020"
},
{
"DOI": "10.1016/j.ekir.2020.06.013",
"article-title": "Outcomes for patients With COVID-19 and acute kidney injury: a systematic review and meta-analysis",
"author": "Robbins-Juarez",
"doi-asserted-by": "crossref",
"first-page": "1149",
"issue": "8",
"journal-title": "Kidney Int Rep.",
"key": "2021120104020554600_CIT0046",
"volume": "5",
"year": "2020"
},
{
"author": "CDC",
"key": "2021120104020554600_CIT0047",
"year": "2021"
},
{
"DOI": "10.1053/j.gastro.2020.05.053",
"article-title": "Famotidine use is associated with improved clinical outcomes in hospitalized COVID-19 patients: a propensity score matched retrospective cohort study",
"author": "Freedberg",
"doi-asserted-by": "crossref",
"first-page": "1129",
"issue": "3",
"journal-title": "Gastroenterology.",
"key": "2021120104020554600_CIT0048",
"volume": "159",
"year": "2020"
},
{
"DOI": "10.14309/ajg.0000000000000832",
"article-title": "Impact of famotidine use on clinical outcomes of hospitalized patients with COVID-19",
"author": "Mather",
"doi-asserted-by": "crossref",
"first-page": "1617",
"issue": "10",
"journal-title": "Am J Gastroenterol.",
"key": "2021120104020554600_CIT0049",
"volume": "115",
"year": "2020"
},
{
"key": "2021120104020554600_CIT0050",
"volume-title": "The use of non-steroidal anti-inflammatory drugs (NSAIDs) in patients with COVID-19: scientific brief, 19 April 2020",
"year": "2020"
},
{
"DOI": "10.1111/jpc.15159",
"article-title": "Is the risk of ibuprofen or other non-steroidal anti-inflammatory drugs increased in COVID-19?",
"author": "Vosu",
"doi-asserted-by": "crossref",
"first-page": "1645",
"issue": "10",
"journal-title": "J Paediatr Child Health.",
"key": "2021120104020554600_CIT0051",
"volume": "56",
"year": "2020"
}
],
"reference-count": 51,
"references-count": 51,
"relation": {},
"score": 1,
"short-container-title": [],
"short-title": [],
"source": "Crossref",
"subject": [
"Public Health, Environmental and Occupational Health"
],
"subtitle": [],
"title": [
"Smoking Status and Factors associated with COVID-19 In-Hospital Mortality among US Veterans"
],
"type": "journal-article"
}