Vitamin D Levels among Hospitalized and Non-Hospitalized COVID-19 Patients in Dr. M. Djamil General Hospital Padang
et al., European Journal of Medical and Health Sciences, doi:10.24018/ejmed.2021.3.6.1131, Dec 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
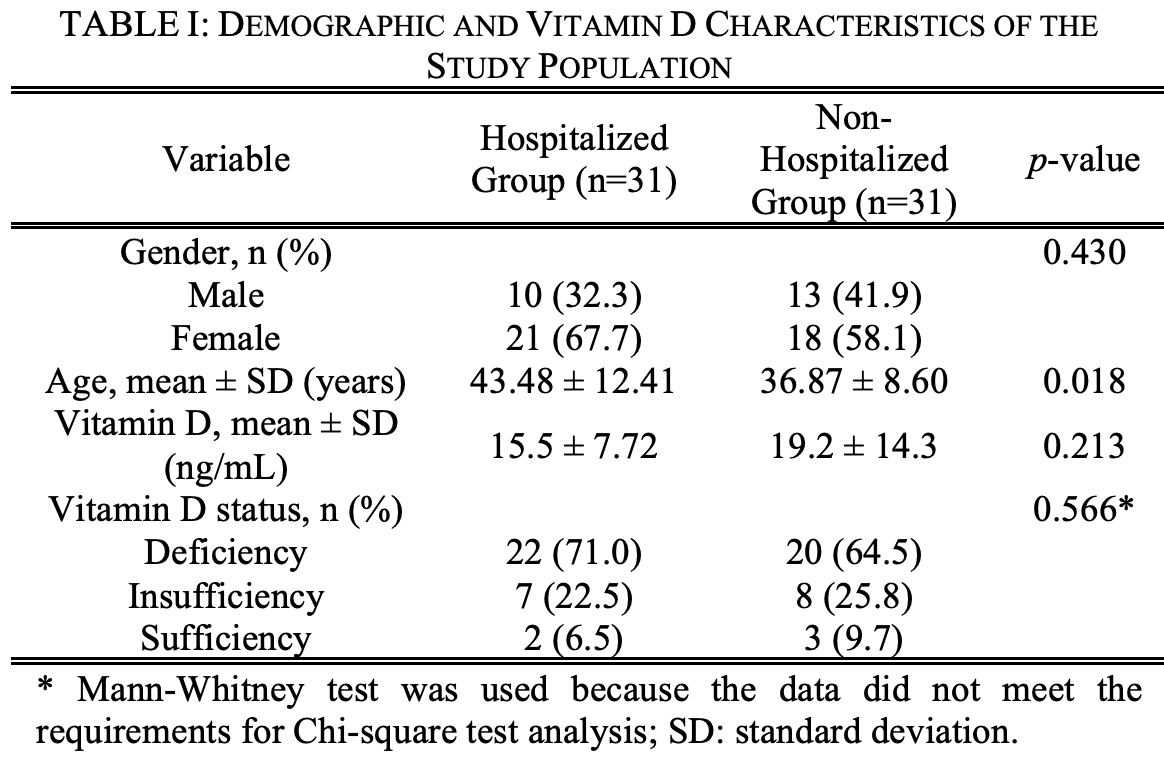
Case control study in Indonesia with 31 moderate to critical hospitalized COVID-19 patients, and 31 asymptomatic or mild non-hospitalized COVID-19 patients, showing lower vitamin D levels in the hospitalized patients, without reaching statistical significance.
This is the 111th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of hospitalization, 25.6% lower, OR 0.74, p = 0.59, high D levels 9 of 31 (29.0%) cases,
11 of 31 (35.5%) controls, NNT 14, case control OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Putra et al., 10 Dec 2021, retrospective, Indonesia, peer-reviewed, 3 authors, study period February 2020 - September 2020.
Vitamin D Levels among Hospitalized and Non-Hospitalized COVID-19 Patients in Dr. M. Djamil General Hospital Padang
European Journal of Medical and Health Sciences, doi:10.24018/ejmed.2021.3.6.1131
Coronavirus Disease 2019 (COVID-19) causes immune system dysregulation and an exaggerated systemic inflammatory response. Vitamin D acts as an immunomodulator that enhances the immunity defense. Degression of vitamin D levels affect the severity of COVID-19 infection Our case-control study compared the vitamin D levels between hospitalized and non-hospitalized COVID-19 patients at RSUP dr. M. Djamil, Padang from February to September 2020. Serum vitamin D levels were categorized as deficiency if the level was less than 20 ng/mL based on the Chemiluminescent Microparticle Immunoassay. The hospitalized group consisted of moderate to critical COVID-19 patients, whereas the nonhospitalized group consisted of the asymptomatic and mild COVID-19 patients according to the Indonesian Ministry of Health Guidelines. Data analysis were performed using T-test and Chi-square with a significant pvalue of less than 0.05. The results showed that most subjects were women between 21-60 years. The mean level of vitamin D (ng/mL) in the hospitalized group was lower than in the non-hospitalized group (15.5 ± 7.72 vs. 19.2 ± 14.30; 95% CI -9.509-2.167; p=0.213). Vitamin D deficiency was found more among hospitalized group than the non-hospitalized group, but not statistically significant (71% vs. 64.5%, p=0.566). It indicated the role of vitamin D in preventing immune system hyperactivation causing COVID-19 cytokine storm. This study concluded no difference in vitamin D levels among the study groups. Nevertheless, further research on vitamin D is needed to determine its role and benefits against COVID-19 infection.
References
Ali, Role of vitamin D in preventing of COVID-19 infection, progression, and severity, Journal of Infection and Public Health
Amrein, Scherkl, Hoffmann, Neuwersch-Sommeregger, Köstenberger et al., Vitamin D deficiency 2.0: an update on the current status worldwide, European Journal of Clinical Nutrition
Annweiler, Corvaisier, Gautier, Dubée, Legrand et al., Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study, Nutrients
Bourgonje, Abdulle, Timens, Hillebrands, Navis et al., Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19), Journal of Pathology
Cutolo, Paolino, Smith, Evidence for a protective role of vitamin D in COVID-19, RMD Open
Dankers, Colin, Van Hamburg, Lubberts, Vitamin D in Autoimmunity: Molecular Mechanisms and Therapeutic Potential, Frontiers in Immunology
Edis, Bloukh, Vitamin D deficiency: main factors affecting the serum 25-hydroxyvitamin d ([25(OH)D]) status and treatment options, International Journal of Research
Efrida, Rofinda, Dr, Hubungan vitamin D dengan kadar adiponektin, Hs-CRP, dan profil lipid pada subjek berat badan berlebih
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, European Journal of Nutrition
Hernández, Nan, Fernandez-Ayala, García-Unzueta, Hernández-Hernández et al., Vitamin D status in hospitalized patients with SARS-CoV-2 infection, Journal of Clinical Endocrinology & Metabolism
Ling, Broad, Murphy, Pappachan, Pardesi-Newton et al., High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: a crosssectional multi-centre observational study, Nutrients
Macaya, Espejo, Valls, Ortiz, Castillo et al., Interaction between age and vitamin D deficiency in severe COVID-19 infection, Nutricion Hospitalaria
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS J
Pinzon, Pradana, Vitamin D deficiency among patients with COVID-19: case series and recent literature review, Troical Medical Health
Pusparini, Defisiensi vitamin D terhadap penyakit, Indonesian Journal of Clinical Pathology and Medical Laboratory
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger, Vitamin D deficiency and outcome of COVID-19 patients, Nutrients
Raharusuna, Priambada, Budiarti, Agung, Budi, Patterns of COVID-19 mortality and vitamin D: an indonesian study, SSRN Electronic Journal
Rosa, Malaguarnera, Nicoletti, Malaguarnera, Vitamin D3: a helpful immuno-modulator, Immunology
Turrubiates-Hernández, Sánchez-Zuno, González-Estevez, Hernández-Bello, Macedo-Ojeda et al., Potential immunomodulatory effects of vitamin D in the prevention of severe coronavirus disease 2019: An ally for Latin America (Review), International Journal of Molecular Medicine
Wang, Gwee, Pang, Micronutrients deficiency, supplementation and novel coronavirus infections-a systematic review and meta-analysis, Nutrients
DOI record:
{
"DOI": "10.24018/ejmed.2021.3.6.1131",
"ISSN": [
"2593-8339"
],
"URL": "http://dx.doi.org/10.24018/ejmed.2021.3.6.1131",
"abstract": "<jats:p>Coronavirus Disease 2019 (COVID-19) causes immune system dysregulation and an exaggerated systemic inflammatory response. Vitamin D acts as an immunomodulator that enhances the immunity defense. Low levels of vitamin D affect the severity of COVID-19 infection. This study aims to determine vitamin D levels in hospitalized and non-hospitalized COVID-19 patients. A case-control study was conducted involving 62 COVID-19 patients, equally divided into hospitalized and non-hospitalized groups at RSUP dr. M. Djamil, Padang from February to September 2020. Serum vitamin D levels were measured using the Chemiluminescent Microparticle Immunoassay. Vitamin D deficiency was defined as a level less than 20 ng/mL. The hospitalized group consisted of moderate to critical COVID-19 patients, whereas the non-hospitalized group consisted of the asymptomatic and mild COVID-19 patients according to the Indonesian Ministry of Health Guidelines. All data were analyzed using a T-test and Chi-square with a significant p-value of 0.05. The results showed that most subjects were women between 21–60 years. The mean level of vitamin D (ng/mL) in the hospitalized group was lower than in the non-hospitalized group (15.5 ± 7.72 vs. 19.2 ± 14.30; 95% CI -9.509–2.167; p=0.213). Vitamin D deficiency affected hospitalized group more than the non-hospitalized group, but not statistically significant (71% vs. 64.5%, p=0.566). It indicated the role of vitamin D in preventing immune system hyperactivation causing COVID-19 cytokine storm. This study concluded no difference in vitamin D levels among the study groups. Nevertheless, further research on vitamin D is needed to determine its role and benefits against COVID-19 infection.</jats:p>",
"author": [
{
"affiliation": [],
"family": "Putra",
"given": "Harika",
"sequence": "first"
},
{
"affiliation": [],
"family": "Efrida",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yaswir",
"given": "Rismawati",
"sequence": "additional"
}
],
"container-title": "European Journal of Medical and Health Sciences",
"container-title-short": "EJMED",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
1,
6
]
],
"date-time": "2022-01-06T13:59:59Z",
"timestamp": 1641477599000
},
"deposited": {
"date-parts": [
[
2022,
1,
6
]
],
"date-time": "2022-01-06T14:00:15Z",
"timestamp": 1641477615000
},
"indexed": {
"date-parts": [
[
2022,
3,
30
]
],
"date-time": "2022-03-30T04:15:35Z",
"timestamp": 1648613735423
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2021,
12,
10
]
]
},
"journal-issue": {
"issue": "6",
"published-online": {
"date-parts": [
[
2021,
11,
1
]
]
}
},
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
10
]
],
"date-time": "2021-12-10T00:00:00Z",
"timestamp": 1639094400000
}
}
],
"link": [
{
"URL": "https://www.ej-med.org/index.php/ejmed/article/download/1131/678",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.ej-med.org/index.php/ejmed/article/download/1131/678",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "10105",
"original-title": [],
"page": "78-81",
"prefix": "10.24018",
"published": {
"date-parts": [
[
2021,
12,
10
]
]
},
"published-online": {
"date-parts": [
[
2021,
12,
10
]
]
},
"publisher": "European Open Science Publishing",
"reference": [
{
"DOI": "10.1016/j.jiph.2020.06.021",
"doi-asserted-by": "crossref",
"key": "17183",
"unstructured": "Ali N. Role of vitamin D in preventing of COVID-19 infection, progression, and severity. Journal of Infection and Public Health. 2020; 13(10): 1373–1380."
},
{
"DOI": "10.3892/ijmm.2021.4865",
"doi-asserted-by": "crossref",
"key": "17184",
"unstructured": "Turrubiates‑Hernández FJ, Sánchez‑Zuno GA, González‑Estevez G, Hernández‑Bello J, Macedo‑Ojeda G, Muñoz‑Valle JF. Potential immunomodulatory effects of vitamin D in the prevention of severe coronavirus disease 2019: An ally for Latin America (Review). International Journal of Molecular Medicine. 2021; 47(4): 32."
},
{
"DOI": "10.1136/rmdopen-2020-001454",
"doi-asserted-by": "crossref",
"key": "17185",
"unstructured": "Cutolo M, Paolino S, Smith V. Evidence for a protective role of vitamin D in COVID-19. RMD Open. 2020; 6: e001454."
},
{
"DOI": "10.24293/ijcpml.v21i1.1265",
"doi-asserted-by": "crossref",
"key": "17186",
"unstructured": "Pusparini. Defisiensi vitamin D terhadap penyakit. Indonesian Journal of Clinical Pathology and Medical Laboratory. 2014; 21(1): 90–95. Indonesian."
},
{
"DOI": "10.1038/s41430-020-0558-y",
"doi-asserted-by": "crossref",
"key": "17187",
"unstructured": "Amrein K, Scherkl M, Hoffmann M, Neuwersch-Sommeregger S, Köstenberger M, Berisha AT, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. European Journal of Clinical Nutrition. 2020; 74: 1498–1513."
},
{
"DOI": "10.1111/j.1365-2567.2011.03482.x",
"doi-asserted-by": "crossref",
"key": "17188",
"unstructured": "Di Rosa M, Malaguarnera M, Nicoletti F, Malaguarnera L. Vitamin D3: a helpful immuno-modulator. Immunology. 2011; 134(2): 123–139."
},
{
"DOI": "10.3389/fimmu.2016.00697",
"doi-asserted-by": "crossref",
"key": "17189",
"unstructured": "Dankers W, Colin EM, van Hamburg JP, Lubberts E. Vitamin D in Autoimmunity: Molecular Mechanisms and Therapeutic Potential. Frontiers in Immunology. 2017; 7: 697."
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "crossref",
"key": "17190",
"unstructured": "Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020; 12(4): 988."
},
{
"DOI": "10.3390/nu12113377",
"doi-asserted-by": "crossref",
"key": "17191",
"unstructured": "Annweiler G, Corvaisier M, Gautier J, Dubée V, Legrand E, Sacco G, et al. Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study. Nutrients. 2020; 12(11): 3377."
},
{
"DOI": "10.3390/nu12123799",
"doi-asserted-by": "crossref",
"key": "17192",
"unstructured": "Ling SF, Broad E, Murphy R, Pappachan JM, Pardesi-Newton S, Kong MF, et al. High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: a cross-sectional multi-centre observational study. Nutrients. 2020; 12(12): 3799."
},
{
"DOI": "10.2139/ssrn.3585561",
"doi-asserted-by": "crossref",
"key": "17193",
"unstructured": "Raharusuna P, Priambada S, Budiarti C, Agung E, Budi C. Patterns of COVID-19 mortality and vitamin D: an indonesian study. SSRN Electronic Journal. 2020: 1-14."
},
{
"DOI": "10.20960/nh.03193",
"doi-asserted-by": "crossref",
"key": "17194",
"unstructured": "Macaya F, Espejo C, Valls A, Ortiz AF, Castillo JG, Martin J, et al. Interaction between age and vitamin D deficiency in severe COVID-19 infection. Nutricion Hospitalaria. 2020; 37(5): 1039–1042."
},
{
"key": "17195",
"unstructured": "Kementerian Kesehatan Republik Indonesia. Pedoman pencegahan dan pengendalian coronavirus disease (COVID-19) revisi Ke-5. Kementerian Kesehatan Republik Indonesia. Jakarta. 2020; 1–214. Indonesian."
},
{
"key": "17196",
"unstructured": "Edis Z, Bloukh SH. Vitamin D deficiency: main factors affecting the serum 25-hydroxyvitamin d ([25(OH)D]) status and treatment options. International Journal of Research. 2016; 3(1): 197–210."
},
{
"key": "17197",
"unstructured": "Abbott Laboratories. Architect 25-OH Vitamin D, B5P020 25-OH Vitamin D 5P02 G5-6832/R03e, Lake Forest, Illinois, USA. 2020:1–8."
},
{
"DOI": "10.1111/febs.15495",
"doi-asserted-by": "crossref",
"key": "17198",
"unstructured": "Merzon E, Tworowski D, Gorohovski A, Vinker S, Golan Cohen A, Green I, et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J. 2020; 287(17): 3693–3702."
},
{
"DOI": "10.1186/s41182-020-00277-w",
"doi-asserted-by": "crossref",
"key": "17199",
"unstructured": "Pinzon RT, Angela, Pradana AW. Vitamin D deficiency among patients with COVID-19: case series and recent literature review. Troical Medical Health. 2020; 48: 102."
},
{
"DOI": "10.1007/s00394-020-02372-4",
"doi-asserted-by": "crossref",
"key": "17200",
"unstructured": "Hastie CE, Pell JP, Sattar N. Vitamin D and COVID-19 infection and mortality in UK Biobank. European Journal of Nutrition. 2021; 60(1): 545–548."
},
{
"DOI": "10.1210/clinem/dgaa733",
"doi-asserted-by": "crossref",
"key": "17201",
"unstructured": "Hernández JL, Nan D, Fernandez-Ayala M, García-Unzueta M, Hernández-Hernández MA, López-Hoyos M, et al. Vitamin D status in hospitalized patients with SARS-CoV-2 infection. Journal of Clinical Endocrinology & Metabolism. 2021; 106(3): e1343-e1353."
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "crossref",
"key": "17202",
"unstructured": "Radujkovic A, Hippchen T, Tiwari-Heckler S, Dreher S, Boxberger M, Merle U. Vitamin D deficiency and outcome of COVID-19 patients. Nutrients. 2020; 12(9): 2757."
},
{
"DOI": "10.3390/nu13051589",
"doi-asserted-by": "crossref",
"key": "17203",
"unstructured": "Wang MX, Gwee SXW, Pang J. Micronutrients deficiency, supplementation and novel coronavirus infections-a systematic review and meta-analysis. Nutrients. 2021; 13(5): 1589."
},
{
"DOI": "10.1002/path.5471",
"doi-asserted-by": "crossref",
"key": "17204",
"unstructured": "Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, et al. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). Journal of Pathology. 2020; 251(3): 228–248."
},
{
"key": "17205",
"unstructured": "Efrida, Yaswir R, Rofinda ZD. Hubungan vitamin D dengan kadar adiponektin, Hs-CRP, dan profil lipid pada subjek berat badan berlebih di RSUP Dr. M. Djamil Padang. Jurnal Kesehatan Andalas. 2018. Indonesian."
}
],
"reference-count": 23,
"references-count": 23,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.ej-med.org/index.php/ejmed/article/view/1131"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"title": "Vitamin D Levels among Hospitalized and Non-Hospitalized COVID-19 Patients in Dr. M. Djamil General Hospital Padang",
"type": "journal-article",
"volume": "3"
}
