Pre-hospital antiplatelet medication use on COVID-19 disease severity
et al., Heart & Lung, doi:10.1016/j.hrtlng.2021.04.010, May 2021
Retrospective 762 COVID+ hospitalized patients in the USA, 239 on antiplatelet medication (199 aspirin), showing no significant differences in outcomes.
For more discussion see1.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments2.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
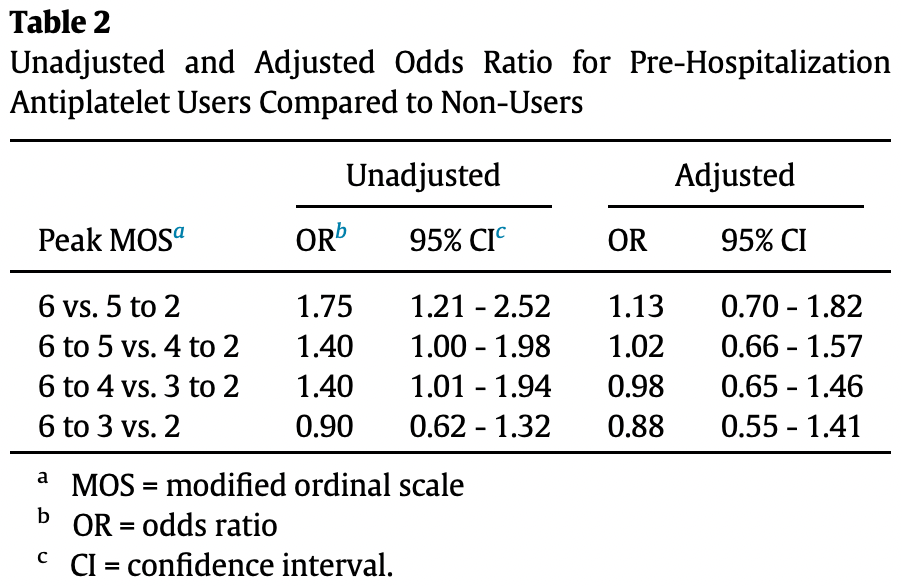
risk of death, 13.0% higher, OR 1.13, p = 0.63, treatment 239, control 523, adjusted per study, MOS 6 vs. <6, multivariable, RR approximated with OR.
|
|
risk of death/intubation, 2.0% higher, OR 1.02, p = 0.93, treatment 239, control 523, adjusted per study, MOS 5+ vs. <5, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Pan et al., 26 May 2021, retrospective, USA, peer-reviewed, 11 authors, study period 1 March, 2020 - 9 April, 2020.
Pre-hospital antiplatelet medication use on COVID-19 disease severity
Heart & Lung, doi:10.1016/j.hrtlng.2021.04.010
Measurements: We captured baseline demographic, pre-hospitalization antiplatelet medication use, and clinical encounter data for all patients who met inclusion criteria. The primary endpoint was peak score on a 6point modified ordinal scale (MOS), which is based on World Health Organization blueprint R&S groups, used to grade severity of illness through clinical outcomes of interest. Scores indicate the following: 1 À COVID-19 infection not requiring hospitalization, 2 À requiring hospitalization but not supplemental oxygen, 3 À hospitalization requiring supplemental oxygen, 4 À hospitalization requiring high-flow nasal cannula (HFNC) or non-invasive positive pressure ventilation (NIPPV), 5 À hospitalization requiring intubation or extracorporeal membrane oxygenation (ECMO), 6 À death. Multivariable adjusted partial proportional odds model (PPOM) was performed to examine the association between pre-hospitalization antiplatelet medication use and likelihood of each MOS score. Main Results: Of 762 people admitted with COVID-19, 239 (31.4%) used antiplatelet medications pre-hospitalization while 523 (68.6%) did not. Antiplatelet users were older and had more co-morbidities at baseline. Before adjusting for covariates, patients who used antiplatelet medications pre-hospitalization were more likely than non-users to have peak MOS score 6 (death, OR 1.75, 95% CI 1.21À2.52), peak MOS score 5 (intubation/ECMO or death, OR 1.4, 95% CI 1.00À1.98) and peak MOS score 4 (HFNC, NIPPV, intubation/ECMO or death, OR 1.40, 95% CI 1.01À1.94). On multivariable adjusted PPOM analysis controlling for 13 covariates, there were no longer any significant differences in peak MOS scores between users and non-users. Conclusions: After adjusting for covariates, pre-hospital antiplatelet use was not associated with COVID-19 severity in hospitalized patients.
Author Contributions Darren Pan and Ada Ip performed chart review and wrote the manuscript. Serena Zhan performed statistical analysis and contributed to writing and editing. Isaac Wasserman, Daniel J. Snyder, Alexandra Z. Agathis, Nikhil Shamapant, Jeong Yun Yang, and Akila Pai performed chart review and contributed to editing. Madhu Mazumdar contributed to editing and provided critical feedback which helped to shape the manuscript. Hooman Poor edited, provided guidance regarding overall direction, and contributed to writing the manuscript.
References
Ackermann, Verleden, Kuehnel, Haverich, Welte et al., Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19, N Engl J Med
Ashraf, Mazloom, Nimkar, Patel, Kalsi et al., Evaluation of Antiplatelet and Anticoagulation Therapy in High-Risk COVID-19 Patients
Banik, Mezera, K€ Ohler, Schmidtmann, Antiplatelet therapy in patients with Covid-19: a retrospective observational study, Thrombosis Update
Chow, Khanna, Kethireddy, Yamane, Levine et al., Aspirin use is associated with decreased mechanical ventilation, intensive care unit admission, and in-hospital mortality in hospitalized patients with coronavirus disease 2019, Anesthesia Analgesia
Desai, Gyawali, Endpoints used in phase III randomized controlled trials of treatment options for COVID-19, EClinicalMedicine
Gattinoni, Coppola, Cressoni, Busana, Rossi et al., Covid-19 does not lead to a "typical" acute respiratory distress syndrome, Am J Respir Crit Care Med
Long, Brady, Koyfman, Gottlieb, Cardiovascular complications in COVID-19, Am J Emerg Med
Magro, Mulvey, Berlin, Nuovo, Salvatore et al., Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases, Transl Res
Ortega-Paz, Capodanno, Montalescot, Angiolillo, Coronavirus Disease 2019Àassociated thrombosis and coagulopathy: review of the pathophysiological characteristics and implications for antithrombotic management, J Am Heart Assoc
Oxley, Mocco, Majidi, Kellner, Shoirah et al., Large-vessel stroke as a presenting feature of Covid-19 in the young, N Engl J Med
Paranjpe, Fuster, Russak, Glicksberg, Levin, Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19, J Am Coll Cardiol
Sivaloganathan, Ladikou, Chevassut, COVID-19 mortality in patients on anticoagulants and antiplatelet agents, Br J Haematol
Tang, Li, Wang, Sun, Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia, J Thromb Haemost
Thomas, Outteridge, Ajjan, Phoenix, Sangha et al., Platelet P2Y12 inhibitors reduce systemic inflammation and its prothrombotic effects in an experimental human model, Arterioscler Thromb Vasc Biol
Wang, Ao, Nasr, Qi, Effect of antiplatelet treatments on patients with COVID-19 infection: A systematic review and meta-analysis, Am J Emerg Med
Zaid, Puhm, Allaeys, Naya, Oudghiri et al., Platelets can associate with SARS-Cov-2 RNA and are hyperactivated in COVID-19, Circ Res
Zarbock, Ley, The role of platelets in acute lung injury (ALI), Front Biosci
Zhou, Yu, Du, Fan, Liu et al., a retrospective cohort study
DOI record:
{
"DOI": "10.1016/j.hrtlng.2021.04.010",
"ISSN": [
"0147-9563"
],
"URL": "http://dx.doi.org/10.1016/j.hrtlng.2021.04.010",
"alternative-id": [
"S0147956321001758"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Pre-hospital antiplatelet medication use on COVID-19 disease severity"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Heart & Lung"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.hrtlng.2021.04.010"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Elsevier Inc. All rights reserved."
}
],
"author": [
{
"affiliation": [],
"family": "Pan",
"given": "Darren",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ip",
"given": "Ada",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhan",
"given": "Serena",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wasserman",
"given": "Isaac",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Snyder",
"given": "Daniel J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Agathis",
"given": "Alexandra Z.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shamapant",
"given": "Nikhil",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yang",
"given": "Jeong Yun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pai",
"given": "Akila",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mazumdar",
"given": "Madhu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Poor",
"given": "Hooman",
"sequence": "additional"
}
],
"container-title": [
"Heart & Lung"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"heartandlung.org",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.fr",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
5,
27
]
],
"date-time": "2021-05-27T13:34:08Z",
"timestamp": 1622122448000
},
"deposited": {
"date-parts": [
[
2021,
7,
30
]
],
"date-time": "2021-07-30T11:15:52Z",
"timestamp": 1627643752000
},
"funder": [
{
"DOI": "10.13039/100000054",
"award": [
"P30 CA 196521"
],
"doi-asserted-by": "publisher",
"name": "National Cancer Institute"
}
],
"indexed": {
"date-parts": [
[
2022,
1,
12
]
],
"date-time": "2022-01-12T17:08:13Z",
"timestamp": 1642007293224
},
"is-referenced-by-count": 2,
"issn-type": [
{
"type": "print",
"value": "0147-9563"
}
],
"issue": "5",
"issued": {
"date-parts": [
[
2021,
9
]
]
},
"journal-issue": {
"issue": "5",
"published-print": {
"date-parts": [
[
2021,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
1
]
],
"date-time": "2021-09-01T00:00:00Z",
"timestamp": 1630454400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0147956321001758?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0147956321001758?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "618-621",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
9
]
]
},
"published-print": {
"date-parts": [
[
2021,
9
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study",
"author": "Zhou",
"doi-asserted-by": "crossref",
"journal-title": "Lancet",
"key": "10.1016/j.hrtlng.2021.04.010_bib0001",
"year": "2020"
},
{
"DOI": "10.1164/rccm.202003-0817LE",
"article-title": "Covid-19 does not lead to a “typical” acute respiratory distress syndrome",
"author": "Gattinoni",
"doi-asserted-by": "crossref",
"first-page": "1299",
"issue": "10",
"journal-title": "Am J Respir Crit Care Med",
"key": "10.1016/j.hrtlng.2021.04.010_bib0002",
"volume": "201",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2015432",
"article-title": "Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19",
"author": "Ackermann",
"doi-asserted-by": "crossref",
"journal-title": "N Engl J Med",
"key": "10.1016/j.hrtlng.2021.04.010_bib0003",
"year": "2020"
},
{
"DOI": "10.1111/jth.14768",
"article-title": "Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia",
"author": "Tang",
"doi-asserted-by": "crossref",
"journal-title": "J Thromb Haemost",
"key": "10.1016/j.hrtlng.2021.04.010_bib0004",
"year": "2020"
},
{
"DOI": "10.1016/j.trsl.2020.04.007",
"article-title": "Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases",
"author": "Magro",
"doi-asserted-by": "crossref",
"journal-title": "Transl Res",
"key": "10.1016/j.hrtlng.2021.04.010_bib0005",
"year": "2020"
},
{
"DOI": "10.2741/3236",
"article-title": "The role of platelets in acute lung injury (ALI)",
"author": "Zarbock",
"doi-asserted-by": "crossref",
"first-page": "150",
"journal-title": "Front Biosci",
"key": "10.1016/j.hrtlng.2021.04.010_bib0006",
"volume": "14",
"year": "2009"
},
{
"DOI": "10.1056/NEJMc2009787",
"article-title": "Large-vessel stroke as a presenting feature of Covid-19 in the young",
"author": "Oxley",
"doi-asserted-by": "crossref",
"first-page": "e60",
"issue": "20",
"journal-title": "N Engl J Med",
"key": "10.1016/j.hrtlng.2021.04.010_bib0007",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/j.ajem.2020.04.048",
"article-title": "Cardiovascular complications in COVID-19",
"author": "Long",
"doi-asserted-by": "crossref",
"journal-title": "Am J Emerg Med",
"key": "10.1016/j.hrtlng.2021.04.010_bib0008",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2020.05.001",
"article-title": "Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19",
"author": "Paranjpe",
"doi-asserted-by": "crossref",
"first-page": "122",
"issue": "1",
"journal-title": "J Am Coll Cardiol",
"key": "10.1016/j.hrtlng.2021.04.010_bib0009",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1161/CIRCRESAHA.120.317703",
"article-title": "Platelets can associate with SARS-Cov-2 RNA and are hyperactivated in COVID-19",
"author": "Zaid",
"doi-asserted-by": "crossref",
"first-page": "1404",
"issue": "11",
"journal-title": "Circ Res",
"key": "10.1016/j.hrtlng.2021.04.010_bib0010",
"volume": "127",
"year": "2020"
},
{
"DOI": "10.1161/JAHA.120.019650",
"article-title": "Coronavirus Disease 2019–associated thrombosis and coagulopathy: review of the pathophysiological characteristics and implications for antithrombotic management",
"author": "Ortega-Paz",
"doi-asserted-by": "crossref",
"issue": "3",
"journal-title": "J Am Heart Assoc",
"key": "10.1016/j.hrtlng.2021.04.010_bib0011",
"volume": "10",
"year": "2021"
},
{
"key": "10.1016/j.hrtlng.2021.04.010_bib0012",
"unstructured": "Coronavirus disease (COVID-2019) R&D. Geneva: World Health Organization (http://www.who.int/blueprint/priority-diseases/key-action/novel-coronavirus/en/)."
},
{
"article-title": "Endpoints used in phase III randomized controlled trials of treatment options for COVID-19",
"author": "Desai",
"first-page": "23",
"journal-title": "EClinicalMedicine",
"key": "10.1016/j.hrtlng.2021.04.010_bib0013",
"year": "2020"
},
{
"key": "10.1016/j.hrtlng.2021.04.010_bib0014",
"unstructured": "RECOVERY Trial, Nuffield Department of Population Health. Updated November 6, 2020. Accessed April 4, 2021. https://www.recoverytrial.net/news/aspirin-to-be-investigated-as-a-possible-treatment-for-covid-19-in-the-recovery-trial."
},
{
"DOI": "10.1213/ANE.0000000000005292",
"article-title": "Aspirin use is associated with decreased mechanical ventilation, intensive care unit admission, and in-hospital mortality in hospitalized patients with coronavirus disease 2019",
"author": "Chow",
"doi-asserted-by": "crossref",
"first-page": "930",
"issue": "4",
"journal-title": "Anesthesia Analgesia",
"key": "10.1016/j.hrtlng.2021.04.010_bib0015",
"volume": "132",
"year": "2021"
},
{
"DOI": "10.1182/blood-2020-137282",
"doi-asserted-by": "crossref",
"key": "10.1016/j.hrtlng.2021.04.010_bib0016",
"unstructured": "Ashraf F, Mazloom A, Nimkar N, Patel N, Kalsi A, Singh A, et al., editors. Evaluation of Antiplatelet and Anticoagulation Therapy in High-Risk COVID-19 Patients. BLOOD; 2020: AMER SOC HEMATOLOGY 2021 L ST NW, SUITE 900, WASHINGTON, DC 20036 USA."
},
{
"DOI": "10.1111/bjh.16968",
"article-title": "COVID-19 mortality in patients on anticoagulants and antiplatelet agents",
"author": "Sivaloganathan",
"doi-asserted-by": "crossref",
"first-page": "e192",
"issue": "4",
"journal-title": "Br J Haematol",
"key": "10.1016/j.hrtlng.2021.04.010_bib0017",
"volume": "190",
"year": "2020"
},
{
"DOI": "10.1016/j.tru.2020.100026",
"article-title": "Antiplatelet therapy in patients with Covid-19: a retrospective observational study",
"author": "Banik",
"doi-asserted-by": "crossref",
"journal-title": "Thrombosis Update",
"key": "10.1016/j.hrtlng.2021.04.010_bib0018",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1016/j.ajem.2021.01.016",
"article-title": "Effect of antiplatelet treatments on patients with COVID-19 infection: A systematic review and meta-analysis",
"author": "Wang",
"doi-asserted-by": "crossref",
"journal-title": "Am J Emerg Med",
"key": "10.1016/j.hrtlng.2021.04.010_bib0019",
"year": "2021"
},
{
"DOI": "10.1161/ATVBAHA.115.306528",
"article-title": "Platelet P2Y12 inhibitors reduce systemic inflammation and its prothrombotic effects in an experimental human model",
"author": "Thomas",
"doi-asserted-by": "crossref",
"first-page": "2562",
"issue": "12",
"journal-title": "Arterioscler Thromb Vasc Biol",
"key": "10.1016/j.hrtlng.2021.04.010_bib0020",
"volume": "35",
"year": "2015"
}
],
"reference-count": 20,
"references-count": 20,
"relation": {},
"score": 1,
"short-container-title": [
"Heart & Lung"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Cardiology and Cardiovascular Medicine",
"Critical Care and Intensive Care Medicine",
"Pulmonary and Respiratory Medicine"
],
"subtitle": [],
"title": [
"Pre-hospital antiplatelet medication use on COVID-19 disease severity"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "50"
}