A report on SARS-CoV-2 first wave in Ecuador: drug consumption dynamics
et al., Frontiers in Pharmacology, doi:10.3389/fphar.2023.1197973, Jun 2023
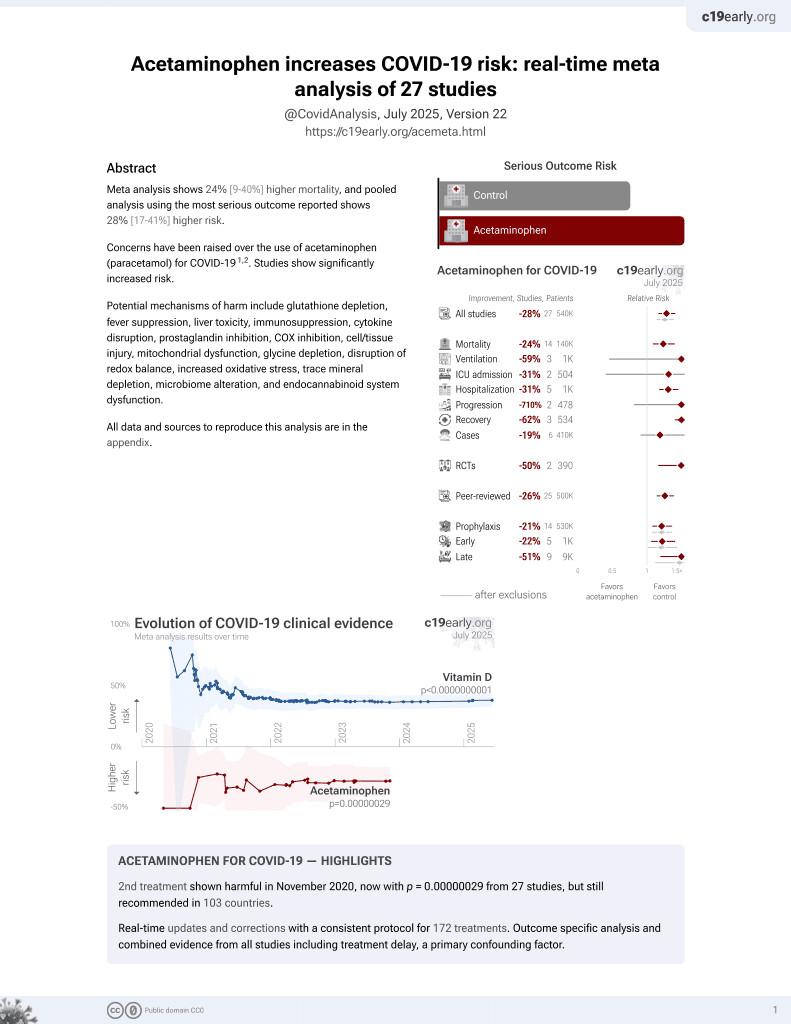
2nd treatment shown to increase risk in
November 2020, now with p = 0.00000029 from 27 studies, but still recommended in 103 countries.
6,400+ studies for
210+ treatments. c19early.org
|
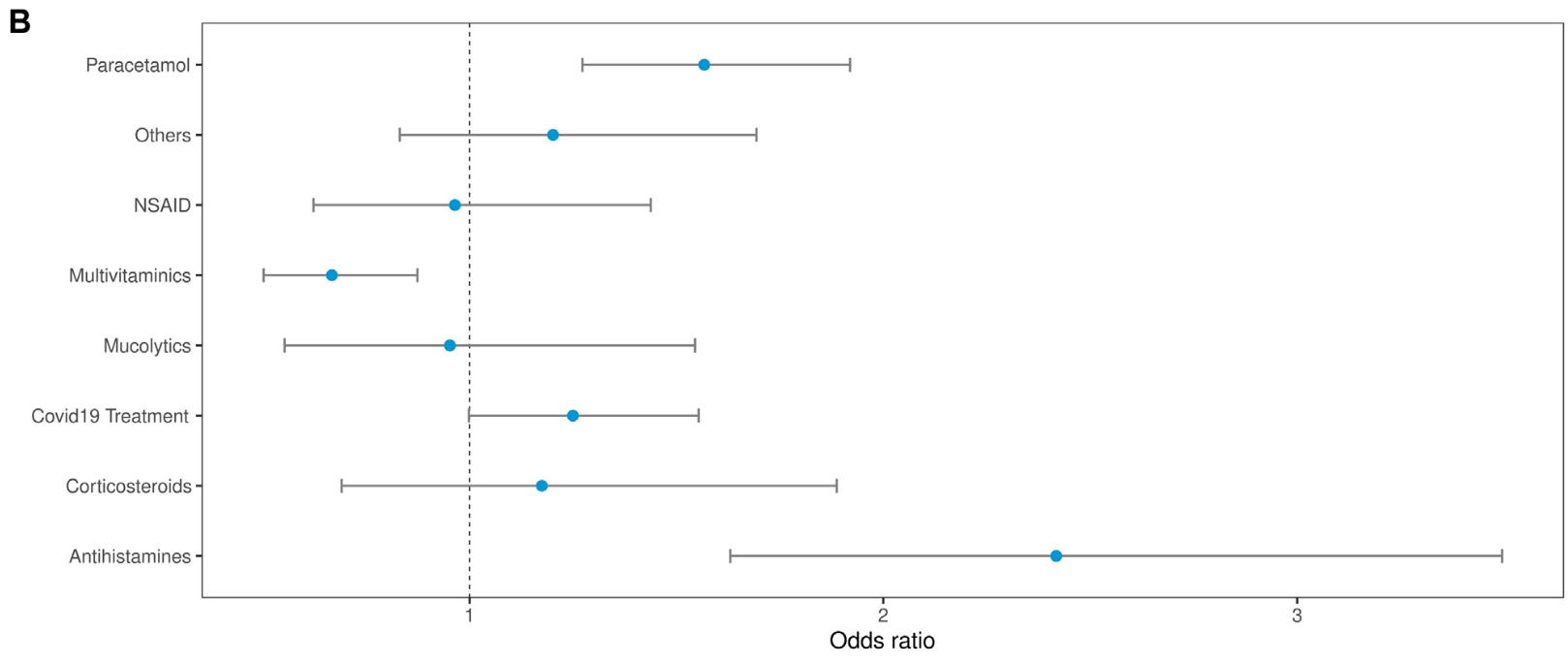
Retrospective 10,175 people PCR tested in Ecuador, showing lower risk of PCR+ with multivitamin use and suggesting higher risk with acetaminophen use.
The study analyzed drug consumption for COVID-19 symptoms during the 14 days before the PCR test, which biases the results towards greater use in PCR+ patients, i.e., the actual ORs may be lower. Therefore the increased risk with acetaminophen may be overestimated, although comparison with COVID-19 treatment, other, and NSAIDs still suggests higher risk with acetaminophen. On the other hand, the decreased risk with multivitamin use is expected to underestimate the true benefit.
Acetaminophen is also known as paracetamol, Tylenol, Panadol, Calpol, Tempra, Calprofen, Doliprane, Efferalgan, Grippostad C, Dolo, Acamol, Fevadol, Crocin, and Perfalgan.
Orellana-Manzano et al., 14 Jun 2023, retrospective, Ecuador, peer-reviewed, survey, 11 authors, study period July 2020 - November 2020.
Contact: akorella@espol.edu.ec.
A report on SARS-CoV-2 first wave in Ecuador: drug consumption dynamics
Frontiers in Pharmacology, doi:10.3389/fphar.2023.1197973
Introduction: The first COVID-19 wave in Ecuador started in March 2020 and extended until November. Several types of drugs have been proposed as a potential treatment during this period, and some affected people have selfmedicated. Method: A retrospective study was conducted with 10,175 individuals who underwent RT-PCR tests for SARS-CoV-2 from July to November 2020. We compared the number of positive and negative cases in Ecuador with symptoms and drug consumption. The Chi-square test of independence compared clinical and demographic data and PCR test results. Odds ratios analyzed drug consumption dynamics. Results: Of 10,175 cases, 570 were positive for COVID-19, while 9,605 were negative. In positive cases, there was no association between the RT-PCR result and sex, age, or comorbidities. When considering demographic data, Cotopaxi and Napo had the highest rates of positive cases (25.7% and 18.8%, respectively). Manabí, Santa Elena, and Guayas regions had fewer than 10% positive cases. The Drug consumption dynamic analysis showed that negative COVID-19 cases presented higher drug consumption than positive cases. In both groups, the most consumed medication was acetaminophen. Acetaminophen and Antihistamines had higher odds of consumption in positive PCR cases than in negative. Symptoms like fever and cough were more related to positive RT-PCR results.
Conclusion: The first COVID-19 wave in Ecuador has affected the provinces differently. At a national level, the consumption of drugs has been highly associated with self-medication.
Ethics statement The studies involving human participants were reviewed and approved by "Comité Nacional Expedito para Investigación sobre COVID-19" under protocol No. 024-2020. The patients/participants provided their written informed consent to participate in this study.
Author contributions AO-M, FC, AG-A, and EC contributed to the conception and design of the study. RM and SP organized the database. AG-A performed the statistical analysis. AO-M wrote the first draft of the manuscript. WC, DA-M, MM, MV-T, SM, IJ, FC, and EC wrote sections of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1197973/ full#supplementary-material
References
Alyammahi, Abdin, Alhamad, Elgendy, Altell et al., The dynamic association between COVID-19 and chronic disorders: An updated insight into prevalence, mechanisms and therapeutic modalities, Infect. Genet. Evol, doi:10.1016/J.MEEGID.2020.104647
Arias, Izquierdo-Condoy, Naranjo-Lara, Alarcón, Bonilla et al., A cross-sectional analysis of self-medication patterns during the COVID-19 pandemic in Ecuador, Med. (B Aires), doi:10.3390/medicina58111678
Baracaldo-Santamaría, Pabón-Londoño, Rojas-Rodriguez, Drug safety of frequently used drugs and substances for self-medication in COVID-19
Bennadi, Pharmacologic prevention and management of nonhospitalized adults with COVID-19* BJC COVID-19 outpatient treatment options see table 2 for more information and BJC criteria for use pre-exposure prophylaxis, Centers for Disease Control and Prevention, doi:10.4103/0976-0105.128253
Chu, Pan, Cheng, Hui, Krishnan et al., Molecular diagnosis of a novel coronavirus (2019-nCoV) causing an outbreak of pneumonia, Clin. Chem, doi:10.1093/clinchem/hvaa029
Cuschieri, Grech, COVID-19 and diabetes: The why, the what and the how, J. Diabetes Complicat, doi:10.1016/J.JDIACOMP.2020.107637
Domingo-Echaburu, Irazola, Prieto, Rocano, None
Dyer, FDA cautions against use of hydroxychloroquine or chloroquine for COVID-19 outside of the hospital setting or a clinical trial due to risk of heart rhythm problems | FDA, BMJ, doi:10.1136/BMJ.M4057
Greenberg, Pemmasani, Yandrapalli, Frishman, Cardiovascular and cerebrovascular complications with COVID-19, Cardiol. Rev, doi:10.1097/CRD.0000000000000385
Hipertens, Vasc, None, doi:10.1016/J.HIPERT.2020.06.003
Hughes, Mcelnay, Fleming, Benefits and risks of self medication, Drug Saf, doi:10.2165/00002018-200124140-00002
Kaur, Thakur, Paika, Advani, Impact of underlying comorbidities on mortality in SARS-COV-2 infected cancer patients: A systematic review and meta-analysis. Asian Pac, J. Cancer Prev, doi:10.31557/APJCP.2021.22.5.1333
Lai, Liu, Wang, Wang, Hsueh et al., Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARSCoV-2): Facts and myths, J. Microbiol. Immunol. Infect, doi:10.1016/j.jmii.2020.02.012
Ma, Holt, COVID-19 and diabetes, Diabet. Med, doi:10.1111/DME.14300
Martins-Filho, Campos Ferreira, Heimfarth, Antunes De Souza Araújo, José Quintans-Júnior, Efficacy and safety of hydroxychloroquine as pre-and post-exposure prophylaxis and treatment of COVID-19: A systematic review and meta-analysis of blinded, placebo-controlled, randomized clinical trials, Lancet Regional Health -Am, doi:10.1016/j.lana.2021.100062
Mohan, Tiwari, Suri, Mittal, Patel et al., Singledose oral ivermectin in mild and moderate COVID-19 (RIVET-COV): A single-centre randomized, placebo-controlled trial, J. Infect. Chemother, doi:10.1016/J.JIAC.2021.08.021
Molento, COVID-19 and the rush for self-medication and self-dosing with ivermectin: A word of caution, One Health, doi:10.1016/J.ONEHLT.2020.100148
Montaño, Covid-19 en Ecuador: Indígenas enfrentan el riesgo de la automedicación, Mongabay
Morales-Jadán, Vallejo-Janeta, Bastidas, Paredes-Espinosa, Freire-Paspuel et al., High SARS-CoV-2 infection rates and viral loads in community-dwelling individuals from rural indigenous and mestizo communities from the Andes during the first wave of the COVID-19 pandemic in Ecuador, doi:10.3389/FMED.2023.1001679
Onchonga, Omwoyo, Nyamamba, Assessing the prevalence of self-medication among healthcare workers before and during the 2019 SARS-CoV-2 (COVID-19) pandemic in Kenya, Saudi Pharm. J, doi:10.1016/J.JSPS.2020.08.003
Orellana Manzano, Orellana Manzano, Dorado Sanchez, Vizcaino, Gomez-Franco et al., Self-medication risk during SARS-COV-2 confinement pandemic, FASEB J, doi:10.1096/fasebj.2021.35.S1.04814
Ortiz-Prado, Henriquez-Trujillo, Rivera-Olivero, Freire-Paspuel, Vallejo-Janeta et al., Massive SARS-CoV-2 RT-PCR testing on rural communities in manabi province (Ecuador) reveals severe COVID-19 outbreaks, Am. J. Trop. Med. Hyg, doi:10.4269/AJTMH.20-1208
Oshikoya, Wharton, Avant, Van Driest, Fenn et al., Serious adverse events associated with off-label use of azithromycin or fentanyl in children in intensive care units: A retrospective chart review, Pediatr. Drugs, doi:10.1007/s40272-018-0318-9
Pandolfi, Simonetti, Ricevuti, Chirumbolo, Paracetamol in the home treatment of early COVID-19 symptoms: A possible foe rather than a friend for elderly patients?, J. Med. Virol, doi:10.1002/JMV.27158
Quincho-Lopez, Benites-Ibarra, Hilario-Gomez, Quijano-Escate, Taype-Rondan, Self-medication practices to prevent or manage COVID-19: A systematic review, PLoS One, doi:10.1371/JOURNAL.PONE.0259317
Quintana, Drugs used during the COVID-19 first wave in Vitoria-Gasteiz (Spain) and their presence in the environment, Sci. Total Environ, doi:10.1016/j.scitotenv.2022.153122
Quispe-Cañari, Fidel-Rosales, Manrique, Mascaró-Zan, Huamán-Castillón et al., Self-medication practices during the COVID-19 pandemic among the adult population in Peru: A cross-sectional survey, Saudi Pharm. J, doi:10.1016/J.JSPS.2020.12.001
Ramireddy, Chugh, Reinier, Ebinger, Park et al., Experience with hydroxychloroquine and azithromycin in the coronavirus disease 2019 pandemic: Implications for qt interval monitoring, J. Am. Heart Assoc, doi:10.1161/JAHA.120.017144
Salazar, Barochiner, Espeche, Ennis, COVID-19 and its relationship with hypertension and cardiovascular disease]
Sestili, Fimognari, Calvo Pita, Maderuelo-Fernández, Paracetamol use in COVID-19: Friend or enemy? Torijano Casalengua, doi:10.1016/j.aprim.2021.102223
Ther, Adv, None, Drug Saf, doi:10.1177/20420986221094141
Vallejo-Janeta, Morales-Jadan, Paredes-Espinosa, Coronel, Galvis et al., Sustained COVID-19 community transmission and potential super spreading events at neglected afro-ecuadorian communities assessed by massive RT-qPCR and serological testing of community dwelling population, Front. Med. (Lausanne), doi:10.3389/fmed.2022.933260
Vargas Patiño, Factores asociados a la automedicación y consumo de medicamentos durante la pandemia del coronavirus (SARS-COV2) en países de América Latina
Voinsky, Baristaite, Gurwitz, Effects of age and sex on recovery from COVID-19: Analysis of 5769 Israeli patients, J. Infect, doi:10.1016/j.jinf.2020.05.026
Yang, Yu, Xu, Shu, Xia et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in wuhan, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30079-5
Zhao, Zhang, Zheng, Thai, Simpson et al., Serious cardiovascular adverse events associated with hydroxychloroquine/chloroquine alone or with azithromycin in patients with COVID-19: A pharmacovigilance analysis of the FDA adverse event reporting system (faers), Drugs Real World Outcomes, doi:10.1007/s40801-022-00300-y
DOI record:
{
"DOI": "10.3389/fphar.2023.1197973",
"ISSN": [
"1663-9812"
],
"URL": "http://dx.doi.org/10.3389/fphar.2023.1197973",
"abstract": "<jats:p><jats:bold>Introduction:</jats:bold> The first COVID-19 wave in Ecuador started in March 2020 and extended until November. Several types of drugs have been proposed as a potential treatment during this period, and some affected people have self-medicated.</jats:p><jats:p><jats:bold>Method:</jats:bold> A retrospective study was conducted with 10,175 individuals who underwent RT-PCR tests for SARS-CoV-2 from July to November 2020. We compared the number of positive and negative cases in Ecuador with symptoms and drug consumption. The Chi-square test of independence compared clinical and demographic data and PCR test results. Odds ratios analyzed drug consumption dynamics.</jats:p><jats:p><jats:bold>Results:</jats:bold> Of 10,175 cases, 570 were positive for COVID-19, while 9,605 were negative. In positive cases, there was no association between the RT-PCR result and sex, age, or comorbidities. When considering demographic data, Cotopaxi and Napo had the highest rates of positive cases (25.7% and 18.8%, respectively). Manabí, Santa Elena, and Guayas regions had fewer than 10% positive cases. The Drug consumption dynamic analysis showed that negative COVID-19 cases presented higher drug consumption than positive cases. In both groups, the most consumed medication was acetaminophen. Acetaminophen and Antihistamines had higher odds of consumption in positive PCR cases than in negative. Symptoms like fever and cough were more related to positive RT-PCR results.</jats:p><jats:p><jats:bold>Conclusion:</jats:bold> The first COVID-19 wave in Ecuador has affected the provinces differently. At a national level, the consumption of drugs has been highly associated with self-medication.</jats:p>",
"alternative-id": [
"10.3389/fphar.2023.1197973"
],
"author": [
{
"affiliation": [],
"family": "Orellana-Manzano",
"given": "Andrea",
"sequence": "first"
},
{
"affiliation": [],
"family": "Cordeiro",
"given": "Fernanda B.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garcia-Angulo",
"given": "Andrea",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Centeno",
"given": "Elizabeth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vizcaíno-Tumbaco",
"given": "María José",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Poveda",
"given": "Sebastián",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Murillo",
"given": "Ricardo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Andrade-Molina",
"given": "Derly",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mirabá",
"given": "Mariuxi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mehta",
"given": "Saurabh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cárdenas",
"given": "Washington",
"sequence": "additional"
}
],
"container-title": "Frontiers in Pharmacology",
"container-title-short": "Front. Pharmacol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2023,
6,
14
]
],
"date-time": "2023-06-14T04:25:47Z",
"timestamp": 1686716747000
},
"deposited": {
"date-parts": [
[
2023,
6,
14
]
],
"date-time": "2023-06-14T04:25:56Z",
"timestamp": 1686716756000
},
"indexed": {
"date-parts": [
[
2023,
6,
14
]
],
"date-time": "2023-06-14T04:40:32Z",
"timestamp": 1686717632416
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
6,
14
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
14
]
],
"date-time": "2023-06-14T00:00:00Z",
"timestamp": 1686700800000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fphar.2023.1197973/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2023,
6,
14
]
]
},
"published-online": {
"date-parts": [
[
2023,
6,
14
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"author": "Agencia Nacional de Regulación",
"key": "B1",
"volume-title": "Resolución ARCSA-DE-002-2020-LDCL la dirección ejecutiva de la agencia nacional de regulación, control Y vigilancia sanitaria-arcsa",
"year": "2020"
},
{
"DOI": "10.1016/J.MEEGID.2020.104647",
"article-title": "The dynamic association between COVID-19 and chronic disorders: An updated insight into prevalence, mechanisms and therapeutic modalities",
"author": "Alyammahi",
"doi-asserted-by": "publisher",
"first-page": "104647",
"journal-title": "Infect. Genet. Evol.",
"key": "B2",
"volume": "87",
"year": "2021"
},
{
"DOI": "10.3390/medicina58111678",
"article-title": "A cross-sectional analysis of self-medication patterns during the COVID-19 pandemic in Ecuador",
"author": "Arias",
"doi-asserted-by": "publisher",
"first-page": "1678",
"journal-title": "Med. (B Aires)",
"key": "B3",
"volume": "58",
"year": "2022"
},
{
"DOI": "10.1177/20420986221094141",
"article-title": "Drug safety of frequently used drugs and substances for self-medication in COVID-19",
"author": "Baracaldo-Santamaría",
"doi-asserted-by": "publisher",
"first-page": "20420986221094141",
"journal-title": "Ther. Adv. Drug Saf.",
"key": "B4",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.4103/0976-0105.128253",
"article-title": "Self-medication: A current challenge",
"author": "Bennadi",
"doi-asserted-by": "publisher",
"first-page": "19",
"journal-title": "J. Basic Clin. Pharm.",
"key": "B5",
"volume": "5",
"year": "2013"
},
{
"key": "B6",
"volume-title": "Pharmacologic prevention and management of non-hospitalized adults with COVID-19* BJC COVID-19 outpatient treatment options see table 2 for more information and BJC criteria for use pre-exposure prophylaxis",
"year": "2023"
},
{
"key": "B7",
"volume-title": "Specific primers and probes for detection 2019 novel coronavirus. China",
"year": "2020"
},
{
"DOI": "10.1093/clinchem/hvaa029",
"article-title": "Molecular diagnosis of a novel coronavirus (2019-nCoV) causing an outbreak of pneumonia",
"author": "Chu",
"doi-asserted-by": "publisher",
"first-page": "549",
"journal-title": "Clin. Chem.",
"key": "B8",
"volume": "66",
"year": "2020"
},
{
"DOI": "10.1016/J.JDIACOMP.2020.107637",
"article-title": "COVID-19 and diabetes: The why, the what and the how",
"author": "Cuschieri",
"doi-asserted-by": "publisher",
"first-page": "107637",
"journal-title": "J. Diabetes Complicat.",
"key": "B9",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1016/j.scitotenv.2022.153122",
"article-title": "Drugs used during the COVID-19 first wave in Vitoria-Gasteiz (Spain) and their presence in the environment",
"author": "Domingo-Echaburu",
"doi-asserted-by": "publisher",
"first-page": "153122",
"journal-title": "Sci. Total Environ.",
"key": "B10",
"volume": "820",
"year": "2022"
},
{
"DOI": "10.1136/BMJ.M4057",
"article-title": "Covid-19: Remdesivir has little or no impact on survival, WHO trial shows",
"author": "Dyer",
"doi-asserted-by": "publisher",
"first-page": "m4057",
"journal-title": "BMJ",
"key": "B11",
"volume": "371",
"year": "2020"
},
{
"key": "B12",
"unstructured": "FDA cautions against use of hydroxychloroquine or chloroquine for COVID-19 outside of the hospital setting or a clinical trial due to risk of heart rhythm problems | FDA2020"
},
{
"DOI": "10.1097/CRD.0000000000000385",
"article-title": "Cardiovascular and cerebrovascular complications with COVID-19",
"author": "Greenberg",
"doi-asserted-by": "publisher",
"first-page": "143",
"journal-title": "Cardiol. Rev.",
"key": "B13",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.2165/00002018-200124140-00002",
"article-title": "Benefits and risks of self medication",
"author": "Hughes",
"doi-asserted-by": "publisher",
"first-page": "1027",
"journal-title": "Drug Saf.",
"key": "B14",
"volume": "24",
"year": "2001"
},
{
"DOI": "10.31557/APJCP.2021.22.5.1333",
"article-title": "Impact of underlying comorbidities on mortality in SARS-COV-2 infected cancer patients: A systematic review and meta-analysis",
"author": "Kaur",
"doi-asserted-by": "publisher",
"first-page": "1333",
"journal-title": "Asian Pac. J. Cancer Prev.",
"key": "B15",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1016/j.jmii.2020.02.012",
"article-title": "Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARSCoV-2): Facts and myths",
"author": "Lai",
"doi-asserted-by": "publisher",
"first-page": "404",
"journal-title": "J. Microbiol. Immunol. Infect.",
"key": "B16",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1111/DME.14300",
"article-title": "COVID‐19 and diabetes",
"author": "Ma",
"doi-asserted-by": "publisher",
"first-page": "723",
"journal-title": "Diabet. Med.",
"key": "B18",
"volume": "37",
"year": "2020"
},
{
"key": "B19",
"unstructured": "Consenso Multidisciplinario informado en la evidencia sobre el tratamiento de Covid-19 – Ministerio de Salud Pública2021"
},
{
"DOI": "10.1016/J.JIAC.2021.08.021",
"article-title": "Single-dose oral ivermectin in mild and moderate COVID-19 (RIVET-COV): A single-centre randomized, placebo-controlled trial",
"author": "Mohan",
"doi-asserted-by": "publisher",
"first-page": "1743",
"journal-title": "J. Infect. Chemother.",
"key": "B21",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/J.ONEHLT.2020.100148",
"article-title": "COVID-19 and the rush for self-medication and self-dosing with ivermectin: A word of caution",
"author": "Molento",
"doi-asserted-by": "publisher",
"first-page": "100148",
"journal-title": "One Health",
"key": "B22",
"volume": "10",
"year": "2020"
},
{
"key": "B23",
"unstructured": "Covid-19 en Ecuador: Indígenas enfrentan el riesgo de la automedicación. Mongabay1\n MontañoD.\n 2020"
},
{
"DOI": "10.3389/FMED.2023.1001679",
"article-title": "High SARS-CoV-2 infection rates and viral loads in community-dwelling individuals from rural indigenous and mestizo communities from the Andes during the first wave of the COVID-19 pandemic in Ecuador",
"author": "Morales-Jadán",
"doi-asserted-by": "publisher",
"first-page": "1001679",
"journal-title": "Front. Med. (Lausanne)",
"key": "B24",
"volume": "10",
"year": "2023"
},
{
"key": "B25",
"unstructured": "Lineamientos Operativos de respuesta frente a coronavirus COVID-192020"
},
{
"key": "B26",
"unstructured": "Provincias | coronavirus Ecuador. Observatorio Social del Ecuador2022"
},
{
"DOI": "10.1016/J.JSPS.2020.08.003",
"article-title": "Assessing the prevalence of self-medication among healthcare workers before and during the 2019 SARS-CoV-2 (COVID-19) pandemic in Kenya",
"author": "Onchonga",
"doi-asserted-by": "publisher",
"first-page": "1149",
"journal-title": "Saudi Pharm. J.",
"key": "B27",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1096/fasebj.2021.35.S1.04814",
"article-title": "Self‐medication risk during SARS‐COV‐2 confinement pandemic",
"author": "Orellana Manzano",
"doi-asserted-by": "publisher",
"first-page": "04814",
"journal-title": "FASEB J.",
"key": "B28",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.4269/AJTMH.20-1208",
"article-title": "Massive SARS-CoV-2 RT-PCR testing on rural communities in manabi province (Ecuador) reveals severe COVID-19 outbreaks",
"author": "Ortiz-Prado",
"doi-asserted-by": "publisher",
"first-page": "1493",
"journal-title": "Am. J. Trop. Med. Hyg.",
"key": "B29",
"volume": "104",
"year": "2021"
},
{
"DOI": "10.1007/s40272-018-0318-9",
"article-title": "Serious adverse events associated with off-label use of azithromycin or fentanyl in children in intensive care units: A retrospective chart review",
"author": "Oshikoya",
"doi-asserted-by": "publisher",
"first-page": "47",
"journal-title": "Pediatr. Drugs",
"key": "B30",
"volume": "21",
"year": "2019"
},
{
"DOI": "10.1002/JMV.27158",
"article-title": "Paracetamol in the home treatment of early COVID‐19 symptoms: A possible foe rather than a friend for elderly patients?",
"author": "Pandolfi",
"doi-asserted-by": "publisher",
"first-page": "5704",
"journal-title": "J. Med. Virol.",
"key": "B31",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1371/JOURNAL.PONE.0259317",
"article-title": "Self-medication practices to prevent or manage COVID-19: A systematic review",
"author": "Quincho-Lopez",
"doi-asserted-by": "publisher",
"first-page": "e0259317",
"journal-title": "PLoS One",
"key": "B32",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1016/J.JSPS.2020.12.001",
"article-title": "Self-medication practices during the COVID-19 pandemic among the adult population in Peru: A cross-sectional survey",
"author": "Quispe-Cañari",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Saudi Pharm. J.",
"key": "B33",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1161/JAHA.120.017144",
"article-title": "Experience with hydroxychloroquine and azithromycin in the coronavirus disease 2019 pandemic: Implications for qt interval monitoring",
"author": "Ramireddy",
"doi-asserted-by": "publisher",
"first-page": "e017144",
"journal-title": "J. Am. Heart Assoc.",
"key": "B34",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.lana.2021.100062",
"article-title": "Efficacy and safety of hydroxychloroquine as pre-and post-exposure prophylaxis and treatment of COVID-19: A systematic review and meta-analysis of blinded, placebo-controlled, randomized clinical trials",
"author": "Ricardo Martins-Filho",
"doi-asserted-by": "publisher",
"first-page": "100062",
"journal-title": "Lancet Regional Health - Am.",
"key": "B35",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1016/J.HIPERT.2020.06.003",
"article-title": "COVID-19 and its relationship with hypertension and cardiovascular disease",
"author": "Salazar",
"doi-asserted-by": "publisher",
"first-page": "176",
"journal-title": "Hipertens. Riesgo Vasc.",
"key": "B36",
"volume": "37",
"year": "2020"
},
{
"article-title": "Paracetamol use in COVID-19: Friend or enemy?",
"author": "Sestili",
"key": "B37",
"year": "2020"
},
{
"DOI": "10.1016/j.aprim.2021.102223",
"article-title": "A safe use of medications in Primary Care, in COVID-19 pandemic as well",
"author": "Torijano Casalengua",
"doi-asserted-by": "publisher",
"first-page": "102223",
"journal-title": "Aten. Primaria",
"key": "B38",
"volume": "53",
"year": "2021"
},
{
"DOI": "10.3389/fmed.2022.933260",
"article-title": "Sustained COVID-19 community transmission and potential super spreading events at neglected afro-ecuadorian communities assessed by massive RT-qPCR and serological testing of community dwelling population",
"author": "Vallejo-Janeta",
"doi-asserted-by": "publisher",
"first-page": "2326",
"journal-title": "Front. Med. (Lausanne)",
"key": "B39",
"volume": "9",
"year": "2022"
},
{
"key": "B40",
"unstructured": "Factores asociados a la automedicación y consumo de medicamentos durante la pandemia del coronavirus (SARS-COV2) en países de América Latina\n Vargas PatiñoK. N.\n 2021"
},
{
"DOI": "10.1016/j.jinf.2020.05.026",
"article-title": "Effects of age and sex on recovery from COVID-19: Analysis of 5769 Israeli patients",
"author": "Voinsky",
"doi-asserted-by": "publisher",
"first-page": "e102",
"journal-title": "J. Infect.",
"key": "B41",
"volume": "81",
"year": "2020"
},
{
"key": "B42",
"volume-title": "WHO in-house assays COVID-19 RT-qPCR 202",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"article-title": "Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in wuhan, China: A single-centered, retrospective, observational study",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "475",
"journal-title": "Lancet Respir. Med.",
"key": "B43",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1007/s40801-022-00300-y",
"article-title": "Serious cardiovascular adverse events associated with hydroxychloroquine/chloroquine alone or with azithromycin in patients with COVID-19: A pharmacovigilance analysis of the FDA adverse event reporting system (faers)",
"author": "Zhao",
"doi-asserted-by": "publisher",
"first-page": "231",
"journal-title": "Drugs Real World Outcomes",
"key": "B44",
"volume": "9",
"year": "2022"
}
],
"reference-count": 42,
"references-count": 42,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fphar.2023.1197973/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology (medical)",
"Pharmacology"
],
"subtitle": [],
"title": "A report on SARS-CoV-2 first wave in Ecuador: drug consumption dynamics",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "14"
}