Use of Ursodeoxycholic Acid and the Risk of Severe Coronavirus Disease 2019 in Elderly Patients with Viral Hepatitis
et al., Internal Medicine, doi:10.2169/internalmedicine.4856-24, Feb 2025
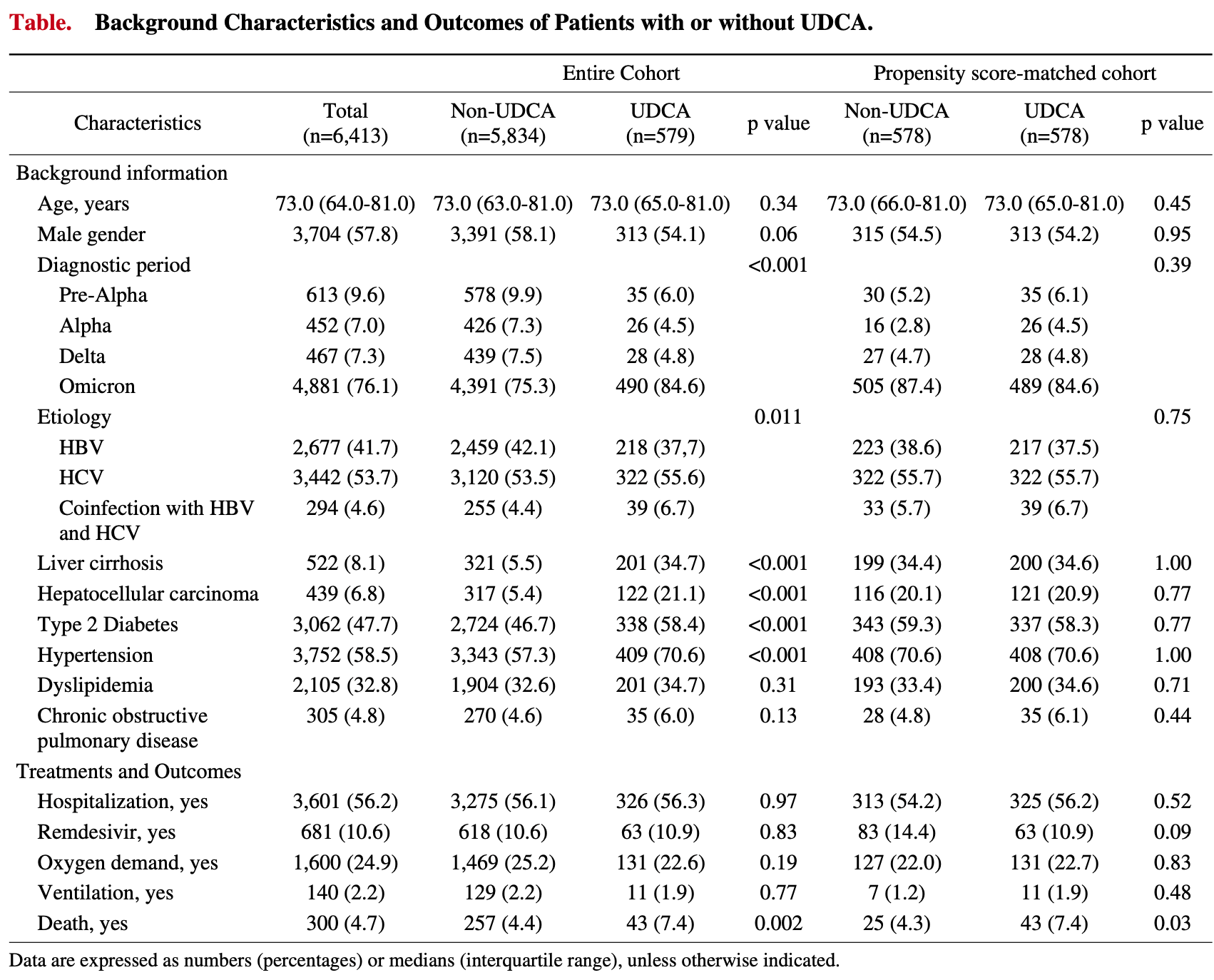
Retrospective 6,413 elderly patients with viral hepatitis in Japan showing increased mortality with ursodeoxycholic acid (UDCA) use in COVID-19 patients. There was no significant difference in hospitalization or oxygen therapy.
Standard of Care (SOC) for COVID-19 in the study country,
Japan, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 72.0% higher, RR 1.72, p = 0.03, treatment 43 of 578 (7.4%), control 25 of 578 (4.3%), propensity score matching.
|
|
risk of mechanical ventilation, 57.1% higher, RR 1.57, p = 0.48, treatment 11 of 578 (1.9%), control 7 of 578 (1.2%), propensity score matching.
|
|
risk of oxygen therapy, 3.1% higher, RR 1.03, p = 0.83, treatment 131 of 578 (22.7%), control 127 of 578 (22.0%), propensity score matching.
|
|
risk of hospitalization, 3.8% higher, RR 1.04, p = 0.52, treatment 325 of 578 (56.2%), control 313 of 578 (54.2%), propensity score matching.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Okushin et al., 1 Feb 2025, retrospective, Japan, peer-reviewed, median age 73.0, 10 authors, study period February 2020 - December 2022.
Contact: takeyatsutsumi@g.ecc.u-tokyo.ac.jp.
Use of Ursodeoxycholic Acid and the Risk of Severe Coronavirus Disease 2019 in Elderly Patients with Viral Hepatitis
doi:10.2169/internalmedicine.4856-24Intern
Objective Although the management of coronavirus disease 2019 (COVID-19) has improved, chemoprevention remains a challenge. We recently identified that ursodeoxycholic acid (UDCA) is associated with subclinical infection with severe acute respiratory syndrome coronavirus, implying a reduction in the severity of COVID-19. We analyzed a large medical database to assess the utility of UDCA in the reduction of COVID-19 severity. Methods This retrospective observational study was conducted using a large-scale healthcare administrative claims database. We extracted data on patients who were diagnosed with either chronic hepatitis B or C. Among them, patients >50 years of age diagnosed with COVID-19 before December 2022 were analyzed. Patients were divided into two groups: those with or without a prescription of UDCA. The primary outcome was the in-hospital mortality rate. A propensity score-matching analysis was performed using logistic regression. Results A total of 6,413 patients diagnosed with COVID-19 (UDCA group, n =579; non-UDCA group, n = 5,834) were analyzed. The median age was 73.0 (IQR, 64.0-81.0) years, and 57.8% of the patients were men. The UDCA group had significantly more complications with liver cirrhosis, hepatocellular carcinoma, type 2 diabetes, and hypertension. The UDCA group had a higher in-hospital mortality rate than the non-UDCA group, even after propensity score matching (7.4% vs. 4.3%, p =0.03), whereas there was no difference in the risks of hospitalization, oxygen therapy, or ventilation. Conclusions Although the observed increase in mortality among UDCA users could have been due to unmeasured confounding factors, UDCA did not reduce the severity of COVID-19 in viral hepatitis patients.
References
Al-Aly, Davis, Mccorkell, Long COVID science, research and policy, Nature medicine
Attaway, Zein, Hatipoglu, SARS-CoV-2 infection in the COPD population is associated with increased healthcare utilization: An analysis of Cleveland clinic's COVID-19 registry, EClini-calMedicine
Brevini, Maes, Webb, FXR inhibition may protect from SARS-CoV-2 infection by reducing ACE2, Nature
Colapietro, Angelotti, Masetti, Ursodeoxycholic Acid Does Not Improve COVID-19 Outcome in Hospitalized Patients, Viruses
Collaborators, Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21, Lancet
Corpechot, Verdoux, Frank-Soltysiak, Vallee, Grimaldi, Exploring the impact of ursodeoxycholic acid therapy on COVID-19 in a real-word setting, Journal of medical virology
Delgado, Vidal, Julia, Validation of N Protein Antibodies to Diagnose Previous SARS-CoV-2 Infection in a Large Cohort of Healthcare Workers: Use of Roche Elecsys((R)) Immunoassay in the S Protein Vaccination Era, Viruses
Dessie, Zewotir, Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients, BMC infectious diseases
Domovitz, Ayoub, Werbner, HCV Infection Increases the Expression of ACE2 Receptor, Leading to Enhanced Entry of Both HCV and SARS-CoV-2 into Hepatocytes and a Coinfection State, Microbiol Spectr
Ge, Far, Digitale, Pletcher, Lai et al., Decreasing Case Fatality Rates for Patients With Cirrhosis Infected With SARS-CoV-2: A National COVID Cohort Collaborative
Guo, Shi, Zhang, Comorbid diabetes and the risk of disease severity or death among 8807 COVID-19 patients in China: A meta-analysis, Diabetes research and clinical practice
Huang, Wang, Liu, COVID-19 patients with hypertension have more severe disease: a multicenter retrospective observational study, Hypertens Res
John, Bastaich, Webb, Ursodeoxycholic acid is associated with a reduction in SARS-CoV-2 infection and reduced severity of COVID-19 in patients with cirrhosis, J Intern Med
Kutsuna, Onozuka, Asano, Matsunami, Matsuoka, Cross-sectional surveillance study of long COVID in Toyonaka city, Osaka prefecture, Japan. Journal of infection and chemotherapy, official journal of the Japan Society of Chemotherapy
Lee, Kim, Yeom, Association Between Ursodeoxycholic Acid and Clinical Outcomes in Patients With COVID-19 Infection: Population-Based Cohort Study, JMIR Public Health Surveill
Li, Hu, Qu, Molecular epidemiology and population immunity of SARS-CoV-2 in Guangdong (2022-2023) following a pivotal shift in the pandemic, Nature communications
Liu, Pan, Yin, Li, Association of dyslipidemia with the severity and mortality of coronavirus disease 2019 (COVID-19): a meta-analysis, Virol J
Marrone, Covino, Merra, Ursodeoxycholic acid does not affect the clinical outcome of SARS-CoV-2 infection: A retrospective study of propensity score-matched cohorts, Liver international : official journal of the International Association for the Study of the Liver
Mdv Ebm Insight, MDV EBM insight
Okushin, Kurano, Group, Ursodeoxycholic acid for coronavirus disease 2019 prevention, J Intern Med
Schilling, Mukaka, Callery, Evaluation of hydroxychloroquine or chloroquine for the prevention of COVID-19 (COPCOV): A double-blind, randomised, placebo-controlled trial, PLoS medicine
Shaikh, Yan, Rogal, Butt, The impact of COVID-19 on the clinical course and outcome of patients with cirrhosis: An observational study, Health Sci Rep
Singh, Mobeen, Chandra, Joshi, Ramachandran, A meta-analysis of comorbidities in COVID-19: Which diseases increase the susceptibility of SARS-CoV-2 infection?, Comput Biol Med
Yamana, Moriwaki, Horiguchi, Kodan, Fushimi et al., Validity of diagnoses, procedures, and laboratory data in Japanese administrative data, J Epidemiol
Yasunaga, Real World Data in Japan: Chapter II The Diagnosis Procedure Combination Database, Annals of Clinical Epidemiology
DOI record:
{
"DOI": "10.2169/internalmedicine.4856-24",
"ISSN": [
"0918-2918",
"1349-7235"
],
"URL": "http://dx.doi.org/10.2169/internalmedicine.4856-24",
"article-number": "4856-24",
"author": [
{
"affiliation": [
{
"name": "Department of Infection Control and Prevention, Graduate School of Medicine, The University of Tokyo, Japan"
},
{
"name": "Department of Gastroenterology, Graduate School of Medicine, The University of Tokyo, Japan"
}
],
"family": "Okushin",
"given": "Kazuya",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Infectious Diseases, Graduate School of Medicine, The University of Tokyo, Japan"
}
],
"family": "Ikeuchi",
"given": "Kazuhiko",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Diseases, Advanced Clinical Research Center, Institute of Medical Science, The University of Tokyo, Japan"
}
],
"family": "Saito",
"given": "Makoto",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Infectious Diseases, Graduate School of Medicine, The University of Tokyo, Japan"
}
],
"family": "Kishida",
"given": "Toshiyuki",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Gastroenterology, Graduate School of Medicine, The University of Tokyo, Japan"
}
],
"family": "Kado",
"given": "Akira",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Gastroenterology, Graduate School of Medicine, The University of Tokyo, Japan"
}
],
"family": "Fujishiro",
"given": "Mitsuhiro",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infection Control and Prevention, Education Research Center, The Tokyo Health Care University, Japan"
}
],
"family": "Moriya",
"given": "Kyoji",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Diseases, Advanced Clinical Research Center, Institute of Medical Science, The University of Tokyo, Japan"
}
],
"family": "Yotsuyanagi",
"given": "Hiroshi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Kanto Central Hospital, Japan"
}
],
"family": "Koike",
"given": "Kazuhiko",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Infection Control and Prevention, Graduate School of Medicine, The University of Tokyo, Japan"
},
{
"name": "Department of Infectious Diseases, Graduate School of Medicine, The University of Tokyo, Japan"
}
],
"family": "Tsutsumi",
"given": "Takeya",
"sequence": "additional"
}
],
"container-title": "Internal Medicine",
"container-title-short": "Intern. Med.",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2025,
1,
31
]
],
"date-time": "2025-01-31T22:13:45Z",
"timestamp": 1738361625000
},
"deposited": {
"date-parts": [
[
2025,
2,
1
]
],
"date-time": "2025-02-01T03:32:58Z",
"timestamp": 1738380778000
},
"indexed": {
"date-parts": [
[
2025,
2,
1
]
],
"date-time": "2025-02-01T05:33:49Z",
"timestamp": 1738388029376,
"version": "3.35.0"
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2025
]
]
},
"language": "en",
"link": [
{
"URL": "https://www.jstage.jst.go.jp/article/internalmedicine/advpub/0/advpub_4856-24/_pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "962",
"original-title": [],
"prefix": "10.2169",
"published": {
"date-parts": [
[
2025
]
]
},
"published-print": {
"date-parts": [
[
2025
]
]
},
"publisher": "Japanese Society of Internal Medicine",
"reference": [
{
"DOI": "10.1016/S0140-6736(21)02796-3",
"doi-asserted-by": "publisher",
"key": "1",
"unstructured": "1. Collaborators C-EM. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet 399: 1513-1536, 2022 (in eng)."
},
{
"DOI": "10.1038/s41467-024-51141-y",
"ISSN": "https://id.crossref.org/issn/2041-1723",
"author": "Z Li",
"doi-asserted-by": "crossref",
"first-page": "7033",
"issn-type": "print",
"journal-title": "Nature Communications",
"key": "2",
"unstructured": "2. Li Z, Hu P, Qu L, et al. Molecular epidemiology and population immunity of SARS-CoV-2 in Guangdong (2022-2023) following a pivotal shift in the pandemic. Nature communications 15: 7033, 2024 (in eng).",
"volume": "15",
"year": "2024"
},
{
"DOI": "10.1038/s41591-024-03173-6",
"doi-asserted-by": "publisher",
"key": "3",
"unstructured": "3. Al-Aly Z, Davis H, McCorkell L, et al. Long COVID science, research and policy. Nature medicine 30: 2148-2164, 2024 (in eng)."
},
{
"DOI": "10.1371/journal.pmed.1004428",
"ISSN": "https://id.crossref.org/issn/1549-1277",
"author": "WHK Schilling",
"doi-asserted-by": "crossref",
"first-page": "e1004428",
"issn-type": "print",
"journal-title": "PLoS Medicine",
"key": "4",
"unstructured": "4. Schilling WHK, Mukaka M, Callery JJ, et al. Evaluation of hydroxychloroquine or chloroquine for the prevention of COVID-19 (COPCOV): A double-blind, randomised, placebo-controlled trial. PLoS medicine 21: e1004428, 2024 (in eng).",
"volume": "21",
"year": "2024"
},
{
"key": "5",
"unstructured": "5. Brevini T, Maes M, Webb GJ, et al. FXR inhibition may protect from SARS-CoV-2 infection by reducing ACE2. Nature 2022 (in eng)."
},
{
"DOI": "10.1111/joim.13630",
"doi-asserted-by": "crossref",
"key": "6",
"unstructured": "6. John BV, Bastaich D, Webb G, et al. Ursodeoxycholic acid is associated with a reduction in SARS-CoV-2 infection and reduced severity of COVID-19 in patients with cirrhosis. J Intern Med 293: 636-647, 2023 (in eng)."
},
{
"DOI": "10.2196/59274",
"doi-asserted-by": "crossref",
"key": "7",
"unstructured": "7. Lee H, Kim MG, Yeom SW, et al. Association Between Ursodeoxycholic Acid and Clinical Outcomes in Patients With COVID-19 Infection: Population-Based Cohort Study. JMIR Public Health Surveill 10: e59274, 2024 (in eng)."
},
{
"DOI": "10.3390/v15081738",
"doi-asserted-by": "crossref",
"key": "8",
"unstructured": "8. Colapietro F, Angelotti G, Masetti C, et al. Ursodeoxycholic Acid Does Not Improve COVID-19 Outcome in Hospitalized Patients. Viruses 15: 2023 (in eng)."
},
{
"DOI": "10.1111/liv.15736",
"doi-asserted-by": "publisher",
"key": "9",
"unstructured": "9. Marrone G, Covino M, Merra G, et al. Ursodeoxycholic acid does not affect the clinical outcome of SARS-CoV-2 infection: A retrospective study of propensity score-matched cohorts. Liver international : official journal of the International Association for the Study of the Liver 44: 83-92, 2024 (in eng)."
},
{
"DOI": "10.1002/jmv.29418",
"ISSN": "https://id.crossref.org/issn/0146-6615",
"author": "C Corpechot",
"doi-asserted-by": "crossref",
"first-page": "e29418",
"issn-type": "print",
"journal-title": "Journal of Medical Virology",
"key": "10",
"unstructured": "10. Corpechot C, Verdoux M, Frank-Soltysiak M, Duclos-Vallee JC, Grimaldi L. Exploring the impact of ursodeoxycholic acid therapy on COVID-19 in a real-word setting. Journal of medical virology 96: e29418, 2024 (in eng).",
"volume": "96",
"year": "2024"
},
{
"DOI": "10.1111/joim.13704",
"doi-asserted-by": "crossref",
"key": "11",
"unstructured": "11. Okushin K, Kurano M, Group U-US, et al. Ursodeoxycholic acid for coronavirus disease 2019 prevention. J Intern Med 295: 106-109, 2024 (in eng)."
},
{
"DOI": "10.3390/v15040930",
"doi-asserted-by": "crossref",
"key": "12",
"unstructured": "12. Delgado JF, Vidal M, Julia G, et al. Validation of N Protein Antibodies to Diagnose Previous SARS-CoV-2 Infection in a Large Cohort of Healthcare Workers: Use of Roche Elecsys ((R) ) Immunoassay in the S Protein Vaccination Era. Viruses 15: 2023 (in eng)."
},
{
"key": "13",
"unstructured": "13. Medical Data Vision Co. L. MDV EBM insight. In: MDV EBM insight."
},
{
"DOI": "10.1016/j.je.2016.09.009",
"doi-asserted-by": "crossref",
"key": "14",
"unstructured": "14. Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol 27: 476-482, 2017 (in eng)."
},
{
"DOI": "10.37737/ace.1.3_76",
"doi-asserted-by": "publisher",
"key": "15",
"unstructured": "15. Yasunaga H. Real World Data in Japan: Chapter II The Diagnosis Procedure Combination Database. Annals of Clinical Epidemiology 1: 76-79, 2019."
},
{
"DOI": "10.1016/j.diabres.2020.108346",
"doi-asserted-by": "publisher",
"key": "16",
"unstructured": "16. Guo L, Shi Z, Zhang Y, et al. Comorbid diabetes and the risk of disease severity or death among 8807 COVID-19 patients in China: A meta-analysis. Diabetes research and clinical practice 166: 108346, 2020 (in eng)."
},
{
"DOI": "10.1038/s41440-020-0485-2",
"doi-asserted-by": "crossref",
"key": "17",
"unstructured": "17. Huang S, Wang J, Liu F, et al. COVID-19 patients with hypertension have more severe disease: a multicenter retrospective observational study. Hypertens Res 43: 824-831, 2020 (in eng)."
},
{
"DOI": "10.1186/s12985-021-01604-1",
"doi-asserted-by": "crossref",
"key": "18",
"unstructured": "18. Liu Y, Pan Y, Yin Y, Chen W, Li X. Association of dyslipidemia with the severity and mortality of coronavirus disease 2019 (COVID-19): a meta-analysis. Virol J 18: 157, 2021 (in eng)."
},
{
"DOI": "10.1016/j.eclinm.2020.100515",
"doi-asserted-by": "crossref",
"key": "19",
"unstructured": "19. Attaway AA, Zein J, Hatipoglu US. SARS-CoV-2 infection in the COPD population is associated with increased healthcare utilization: An analysis of Cleveland clinic's COVID-19 registry. EClinicalMedicine 26: 100515, 2020 (in eng)."
},
{
"DOI": "10.1016/j.jiac.2023.12.006",
"doi-asserted-by": "publisher",
"key": "20",
"unstructured": "20. Kutsuna S, Onozuka D, Asano K, Matsunami K, Matsuoka T. Cross-sectional surveillance study of long COVID in Toyonaka city, Osaka prefecture, Japan. Journal of infection and chemotherapy : official journal of the Japan Society of Chemotherapy 30: 511-515, 2024 (in eng)."
},
{
"key": "21",
"unstructured": "21. Ministry of Health, Labour and Welfare. Visualizing the data: information on COVID-19 infections [Internet]. [cited 2024 Sep 16]. Available from: https://covid19.mhlw.go.jp/en/."
},
{
"DOI": "10.1186/s12879-021-06536-3",
"ISSN": "https://id.crossref.org/issn/1471-2334",
"author": "ZG Dessie",
"doi-asserted-by": "crossref",
"first-page": "855",
"issn-type": "print",
"journal-title": "BMC Infectious Diseases",
"key": "22",
"unstructured": "22. Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC infectious diseases 21: 855, 2021 (in eng).",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1128/spectrum.01150-22",
"doi-asserted-by": "crossref",
"key": "23",
"unstructured": "23. Domovitz T, Ayoub S, Werbner M, et al. HCV Infection Increases the Expression of ACE2 Receptor, Leading to Enhanced Entry of Both HCV and SARS-CoV-2 into Hepatocytes and a Coinfection State. Microbiol Spectr 10: e0115022, 2022 (in eng)."
},
{
"DOI": "10.1016/j.compbiomed.2021.104219",
"doi-asserted-by": "crossref",
"key": "24",
"unstructured": "24. Singh MK, Mobeen A, Chandra A, Joshi S, Ramachandran S. A meta-analysis of comorbidities in COVID-19: Which diseases increase the susceptibility of SARS-CoV-2 infection? Comput Biol Med 130: 104219, 2021 (in eng)."
},
{
"DOI": "10.1002/hsr2.2207",
"doi-asserted-by": "crossref",
"key": "25",
"unstructured": "25. Shaikh OS, Yan P, Rogal S, Butt AA. The impact of COVID-19 on the clinical course and outcome of patients with cirrhosis: An observational study. Health Sci Rep 7: e2207, 2024 (in eng)."
},
{
"key": "26",
"unstructured": "26. Ge J, Far AT, Digitale JC, Pletcher MJ, Lai JC; National CCCC. Decreasing Case Fatality Rates for Patients With Cirrhosis Infected With SARS-CoV-2: A National COVID Cohort Collaborative Study. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association 2024 (in eng)."
},
{
"DOI": "10.1007/s40801-022-00296-5",
"doi-asserted-by": "crossref",
"key": "27",
"unstructured": "27. Laurent T, Simeone J, Kuwatsuru R, et al. Context and Considerations for Use of Two Japanese Real-World Databases in Japan: Medical Data Vision and Japanese Medical Data Center. Drugs Real World Outcomes 9: 175-187, 2022 (in eng)."
}
],
"reference-count": 27,
"references-count": 27,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.jstage.jst.go.jp/article/internalmedicine/advpub/0/advpub_4856-24/_article"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Use of Ursodeoxycholic Acid and the Risk of Severe Coronavirus Disease 2019 in Elderly Patients with Viral Hepatitis",
"type": "journal-article"
}