Incidence and Mortality Associated with Cardiovascular Medication among Hypertensive COVID-19 Patients in South Korea
et al., Yonsei Medical Journal, doi:10.3349/ymj.2021.62.7.577, Jun 2021
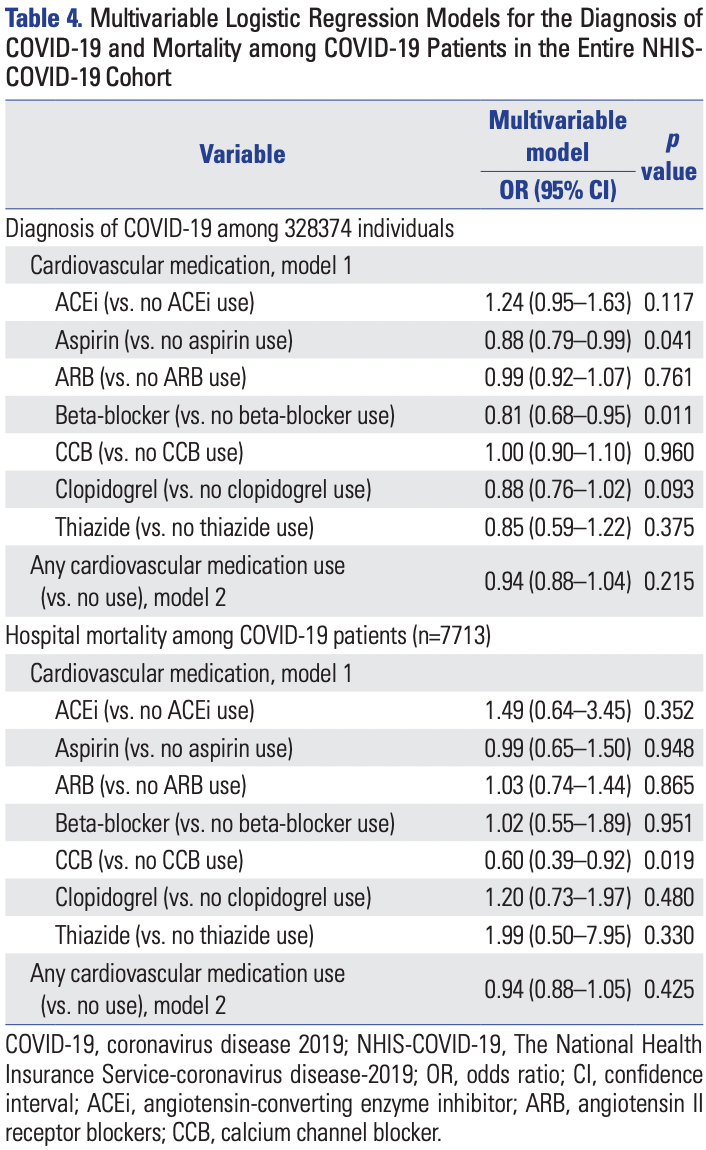
Retrospective database analysis of 328,374 adults in South Korea, showing lower risk of COVID-19 cases with aspirin use, but no difference in mortality for COVID-19 patients.
|
risk of death, 1.0% lower, OR 0.99, p = 0.95, adjusted per study, multivariable, RR approximated with OR.
|
|
risk of case, 12.0% lower, RR 0.88, p = 0.04, adjusted per study, odds ratio converted to relative risk, multivariable, control prevalance approximated with overall prevalence.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Oh et al., 17 Jun 2021, retrospective, database analysis, South Korea, peer-reviewed, 4 authors.
Incidence and Mortality Associated with Cardiovascular Medication among Hypertensive COVID-19 Patients in South Korea
Yonsei Medical Journal, doi:10.3349/ymj.2021.62.7.577
Purpose: We aimed to investigate whether the use of cardiovascular drugs in coronavirus disease 2019 (COVID-19) patients with hypertension as a comorbidity has a significant effect on the incidence and associated mortality rate of COVID-19. Materials and Methods: Data covering the period between January 1, 2020 and June 4, 2020 were extracted from The National Health Insurance Service-COVID-19 (NHIS-COVID-19) database in South Korea and analyzed as a population-based cohort study. Results: A total of 101657 hypertensive adults aged 20 years or older were included for final analysis. Among them, 1889 patients (1.9%) were diagnosed with COVID-19 between January 1, 2020 and June 4, 2020, and hospital mortality occurred in 193 patients (10.2%). In a multivariable model, the use of beta-blockers was associated with an 18% lower incidence of COVID-19 [odds ratio (OR): 0.82, 95% confidence interval (CI): 0.69-0.98; p=0.029]. Among 1889 hypertensive patients diagnosed with COVID-19, the use of a calcium channel blocker (CCB) was associated with a 42% lower hospital mortality rate (OR: 0.58, 95% CI: 0.38-0.89; p=0.012). The use of other cardiovascular drugs was not associated with the incidence of COVID-19 or hospital mortality rate among COVID-19 patients. Similar results were observed in all 328374 adults in the NHIS-COVID-19 database, irrespective of the presence of hypertension.
Conclusion: In South Korea, beta-blockers exhibited potential benefits in lowering the incidence of COVID-19 among hypertensive patients. Furthermore, CCBs may lower the hospital mortality rate among hypertensive COVID-19 patients. These findings were also applied to the general adult population, regardless of hypertension.
AUTHOR CONTRIBUTIONS Conceptualization: Tak Kyu Oh and In-Ae Song. Data curation: Hyoung-Won Cho and Jung-Won Suh. Formal analysis: Tak Kyu Oh. Investigation: Hyoung-Won Cho and Tak Kyu Oh. Methodology: Tak Kyu Oh and In-Ae Song. Supervision:In-Ae Song. Validation: Tak Kyu Oh and In-Ae Song. Visualization: Hyoung-Won Cho and Jung-Won Suh. Writing-original draft: Tak Kyu Oh. Writing-review & editing: Jung-Won Suh and In-Ae Song. Approval of final manuscript: all authors.
References
Alegbeleye, Akpoveso, Alegbeleye, Mohammed, Zubero, The novel aspirin as breakthrough drug for COV-ID-19: a narrative review, Iberoam J
Baigent, Blackwell, Collins, Emberson, Godwin, Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials, Lancet
Bedford, Enria, Giesecke, Heymann, Ihekweazu et al., COVID-19: towards controlling of a pandemic, Lancet
Bianconi, Violi, Fallarino, Pignatelli, Sahebkar et al., Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19?, Drugs
Chen, Wu, Chen, Yang, Chen, Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study, BMJ
Dagan, Barda, Kepten, Miron, Perchik et al., BNT162b2 mRNA covid-19 vaccine in a nationwide mass vaccination setting, N Engl J Med
Devaux, Rolain, Raoult, ACE2 receptor polymorphism: susceptibility to SARS-CoV-2, hypertension, multi-organ failure, and COVID-19 disease outcome, J Microbiol Immunol Infect
Drager, Pio-Abreu, Lopes, Bortolotto, Is hypertension a real risk factor for poor prognosis in the COVID-19 pandemic?, Curr Hypertens Rep
Fontanet, Cauchemez, COVID-19 herd immunity: where are we?, Nat Rev Immunol
Gao, Cai, Zhang, Zhou, Zhang et al., Association of hypertension and antihypertensive treatment with COVID-19 mortality: a retrospective observational study, Eur Heart J
Giannis, Ziogas, Gianni, Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past, J Clin Virol
Knoll, Wonodi, Oxford-AstraZeneca COVID-19 vaccine efficacy, Lancet
Kreutz, Algharably, Azizi, Dobrowolski, Guzik et al., Hypertension, the renin-angiotensin system, and the risk of lower respiratory tract infections and lung injury: implications for COVID-19, Cardiovasc Res
Kuster, Pfister, Burkard, Zhou, Twerenbold et al., SARS-CoV2: should inhibitors of the renin-angiotensin system be withdrawn in patients with COVID-19?, Eur Heart J
Lai, Millet, Daniel, Freed, Whittaker, The SARS-CoV fusion peptide forms an extended bipartite fusion platform that perturbs membrane order in a calcium-dependent manner, J Mol Biol
Liu, Huang, Xu, Yang, Qin et al., Anti-hypertensive angiotensin II receptor blockers associated to mitigation of disease severity in elderly COVID-19 patients, medRxiv, doi:10.1101/2020.03.20.20039586
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., COVID-19: consider cytokine storm syndromes and immunosuppression, Lancet
Natesan, SARS-CoV-2 host cell entry might involve beta adrenergic receptors, OSF Preprints, doi:10.31219/osf.io/d2g8k
Noveanu, Breidthardt, Reichlin, Gayat, Potocki et al., Effect of oral β-blocker on short and long-term mortality in patients with acute respiratory failure: results from the BASEL-II-ICU study, Crit Care
Rezel-Potts, Douiri, Chowienczyk, Gulliford, Antihypertensive medications and COVID-19 diagnosis and mortality: population-based case-control analysis in the United Kingdom, Br J Clin Pharmacol, doi:Availableat:10.1111/bcp.14873
Sardu, Maggi, Messina, Iuliano, Sardu et al., Could anti-hypertensive drug therapy affect the clinical prognosis of hypertensive patients with COVID-19 infection? Data from centers of Southern Italy, J Am Heart Assoc
Schiffrin, Flack, Ito, Muntner, Webb, Hypertension and COVID-19, Am J Hypertens
South, Diz, Chappell, COVID-19, ACE2, and the cardiovascular consequences, Am J Physiol Heart Circ Physiol
Straus, Bidon, Tang, Whittaker, Daniel, FDA approved calcium channel blockers inhibit SARS-CoV-2 infectivity in epithelial lung cells, bioRxiv, doi:10.1101/2020.07.21.214577
Tan, Harazim, Tang, Mclean, Nalos, The association between premorbid beta blocker exposure and mortality in sepsis-a systematic review, Crit Care
Vasanthakumar, Can beta-adrenergic blockers be used in the treatment of COVID-19?, Med Hypotheses
Von Elm, Altman, Egger, Pocock, Gøtzsche et al., The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies, Int J Surg
White, Anderson, Outcomes in patients with COVID-19 infection taking ACEI/ARB, Curr Cardiol Rep
Yang, Tan, Zhou, Yang, Peng et al., Effects of angiotensin II receptor blockers and ACE (angiotensin-converting enzyme) inhibitors on virus infection, inflammatory status, and clinical outcomes in patients with COVID-19 and hypertension: a single-center retrospective study, Hypertension
Zhang, Sun, Zeng, Wang, Jiang et al., Calcium channel blocker amlodipine besylate therapy is associated with reduced case fatality rate of COVID-19 patients with hypertension, Cell Discov
Zhang, Zhu, Cai, Lei, Qin et al., Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19, Circ Res
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.3349/ymj.2021.62.7.577",
"ISSN": [
"0513-5796",
"1976-2437"
],
"URL": "http://dx.doi.org/10.3349/ymj.2021.62.7.577",
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"value": "2021-01-14"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Revised",
"name": "revised",
"value": "2021-03-15"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"value": "2021-04-06"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published online",
"name": "published_online",
"value": "2021-06-17"
},
{
"group": {
"label": "Copyright and Licensing",
"name": "Copyright_and_licensing"
},
"label": "Copyright",
"name": "copyright",
"value": "© Copyright: Yonsei University College of Medicine 2021"
},
{
"explanation": {
"URL": "https://creativecommons.org/licenses/by-nc/4.0/"
},
"group": {
"label": "Copyright and Licensing",
"name": "Copyright_and_licensing"
},
"label": "License",
"name": "license",
"value": "This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-4027-4423",
"affiliation": [
{
"name": "Department of Anesthesiology and Pain Medicine Center, Seoul National University Bundang Hospital, Seongnam, Korea."
}
],
"authenticated-orcid": false,
"family": "Oh",
"given": "Tak Kyu",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-6095-8569",
"affiliation": [
{
"name": "Department of Cardiology, Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea."
}
],
"authenticated-orcid": false,
"family": "Cho",
"given": "Hyoung-Won",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0397-6071",
"affiliation": [
{
"name": "Department of Cardiology, Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea."
}
],
"authenticated-orcid": false,
"family": "Suh",
"given": "Jung-Won",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7814-4253",
"affiliation": [
{
"name": "Department of Anesthesiology and Pain Medicine Center, Seoul National University Bundang Hospital, Seongnam, Korea."
}
],
"authenticated-orcid": false,
"family": "Song",
"given": "In-Ae",
"sequence": "additional"
}
],
"container-title": [
"Yonsei Medical Journal"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"eymj.org"
]
},
"created": {
"date-parts": [
[
2021,
6,
22
]
],
"date-time": "2021-06-22T06:44:11Z",
"timestamp": 1624344251000
},
"deposited": {
"date-parts": [
[
2021,
6,
22
]
],
"date-time": "2021-06-22T06:53:25Z",
"timestamp": 1624344805000
},
"indexed": {
"date-parts": [
[
2022,
1,
18
]
],
"date-time": "2022-01-18T09:25:20Z",
"timestamp": 1642497920513
},
"is-referenced-by-count": 1,
"issn-type": [
{
"type": "print",
"value": "0513-5796"
},
{
"type": "electronic",
"value": "1976-2437"
}
],
"issue": "7",
"issued": {
"date-parts": [
[
2021
]
]
},
"journal-issue": {
"issue": "7",
"published-print": {
"date-parts": [
[
2021
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
}
],
"link": [
{
"URL": "https://eymj.org/pdf/10.3349/ymj.2021.62.7.577",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://eymj.org/DOIx.php?id=10.3349/ymj.2021.62.7.577",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://eymj.org/DOIx.php?id=10.3349/ymj.2021.62.7.577",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1901",
"original-title": [],
"page": "577",
"prefix": "10.3349",
"published": {
"date-parts": [
[
2021
]
]
},
"published-print": {
"date-parts": [
[
2021
]
]
},
"publisher": "Yonsei University College of Medicine",
"reference-count": 33,
"references-count": 33,
"relation": {},
"score": 1,
"short-container-title": [
"Yonsei Med J"
],
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": [
"Incidence and Mortality Associated with Cardiovascular Medication among Hypertensive COVID-19 Patients in South Korea"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3349/crossmark_policy",
"volume": "62"
}