Arrhythmias as Part of Long COVID Syndrome in Hospitalized Patients That Survived a Severe COVID-19 Infection and the Potential Protective Role of Metformin in These Patients
et al., Life, doi:10.3390/life16020319, Feb 2026
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 53 hospitalized COVID-19 patients showing a 41% prevalence of cardiac arrhythmias during long COVID, with metformin use associated with reduced arrhythmia risk. Authors hypothesize metformin's protective effect occurs through AMPK activation, improved calcium homeostasis, reduced inflammation, and enhanced electrical conduction via connexin-43 expression.
Morales-Vazquez et al., 12 Feb 2026, retrospective, Mexico, peer-reviewed, survey, 11 authors, study period January 2022 - February 2022.
Contact: david.cardona@academicos.udg.mx (corresponding author), morales.ninette08@gmail.com, tomas_miranda_a@hotmail.com, fernando.grover@academicos.udg.mx, guadalupe.ramos@academicos.udg.mx, jaime.camona@academicos.udg.mx, drjorgehdez@hotmail.com, dr.christian.glez@gmail.com, christopher.lgradilla@alumnos.udg.mx.
Arrhythmias as Part of Long COVID Syndrome in Hospitalized Patients That Survived a Severe COVID-19 Infection and the Potential Protective Role of Metformin in These Patients
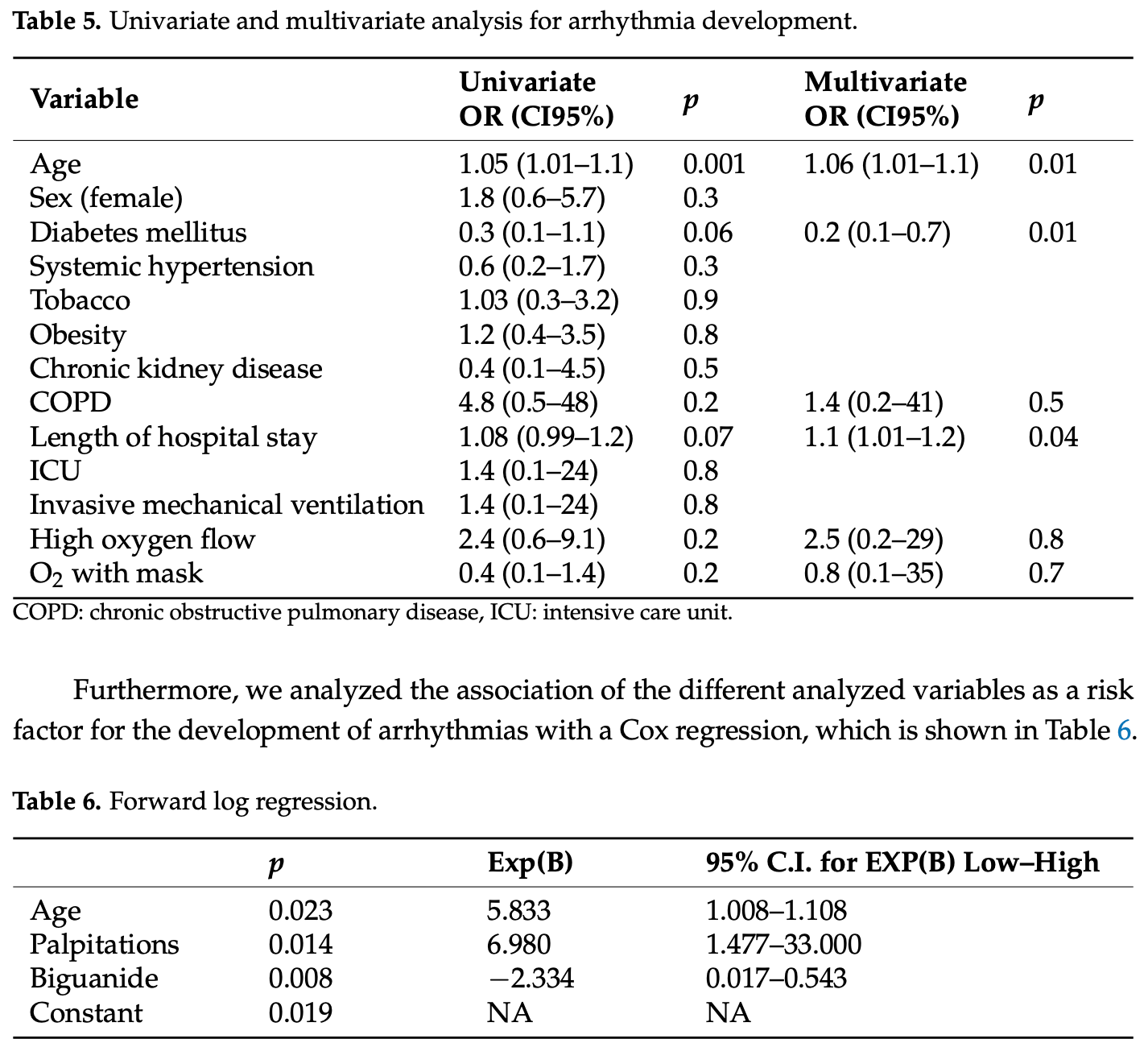
Life, doi:10.3390/life16020319
Background: Cardiac arrhythmias are a frequent complication of acute SARS-CoV-2 infection. However, their long-term prevalence and clinical determinants among patients with post-COVID-19 syndrome, especially those previously hospitalized, remain poorly defined. Objectives: To assess the prevalence and types of arrhythmias in long COVID patients following hospitalization and to identify associated clinical risk factors. Methods: In this cross-sectional study, 53 patients previously hospitalized with confirmed COVID-19 were evaluated ≥3 months post-infection. All participants underwent a standardized clinical assessment, 12-lead electrocardiography, and 24 h Holter monitoring. Logistic and Cox regression analyses were performed to identify predictors of arrhythmia. Results: Arrhythmias were identified in 41.5% (n = 22) of patients. Atrial fibrillation (32%) was the most frequent arrhythmia, followed by sinus bradycardia (27%) and sinus tachycardia (18%). Age (OR 1.06, 95% CI 1.01-1.10, p = 0.01) and length of hospital stay (OR 1.1, 95% CI 1.01-1.2, p = 0.04) were independently associated with arrhythmia. Biguanide (metformin) therapy was inversely associated with the occurrence of arrhythmia (Exp(B) = 0.017, p = 0.008). Dyspnea (82.4%) and palpitations (41.5%) were the most commonly reported symptoms. Conclusions: Arrhythmias are common in patients with long COVID following severe disease. Advanced age and prolonged hospitalization are significant risk factors, while biguanide use may offer a protective effect. These findings underscore the need for targeted cardiac surveillance in this population.
Conflicts of Interest: The authors declare no conflict of interest.
References
Al-Aly, Xie, Bowe, High-dimensional characterization of post-acute sequelae of COVID-19, Nature, doi:10.1038/s41586-021-03553-9
Apaijai, Chinda, Palee, Chattipakorn, Chattipakorn, Combined vildagliptin and metformin exert better cardioprotection than monotherapy against ischemia-reperfusion injury in obese-insulin resistant rats, PLoS ONE, doi:10.1371/journal.pone.0102374
Aponte-Hidalgo, Coelho-Lugo, Escalona-García, Figuera-Aparicio, Hernández-Cabanzo et al., Diagnóstico de arritmias ventriculares en pacientes con síndrome post COVID-19, Rev. Peruana Investig. Salud, doi:10.35839/repis.6.2.1326
Chang, Toh, Liao, Yu, Cardiac Involvement of COVID-19: A Comprehensive Review, Am. J. Med. Sci, doi:10.1016/j.amjms.2020.10.002
Davis, Assaf, Mccorkell, Wei, Low et al., Characterizing long COVID in an international cohort: 7 months of symptoms and their impact, EClinicalMedicine, doi:10.1016/j.eclinm.2021.101019
Dewland, Whitman, Win, Sanchez, Olgin et al., Prospective arrhythmia surveillance after a COVID-19 diagnosis, Open Heart
Frangogiannis, Cardiac fibrosis, Cardiovasc. Res, doi:10.1093/cvr/cvaa324
Grisanti, Diabetes and Arrhythmias: Pathophysiology, Mechanisms and Therapeutic Outcomes, Front. Physiol, doi:10.3389/fphys.2018.01669
Gupta, Madhavan, Sehgal, Nair, Mahajan et al., Extrapulmonary manifestations of COVID-19, Nat. Med, doi:10.1038/s41591-020-0968-3
Iam-Arunthai, Chamnanchanunt, Thungthong, Chinapha, Nakhahes et al., COVID-19 with high-sensitivity CRP associated with worse dynamic clinical parameters and outcomes, Front. Med
Kim, Park, Kim, Min, Cho et al., Association between antidiabetic drugs and the incidence of atrial fibrillation in patients with type 2 diabetes: A nationwide cohort study in South Korea, Diabetes Res. Clin. Pract, doi:10.1016/j.diabres.2023.110626
Kingma, Simard, Drolet, Overview of Cardiac Arrhythmias and Treatment Strategies, Pharmaceuticals, doi:10.3390/ph16060844
Korompoki, Gavriatopoulou, Hicklen, Ntanasis-Stathopoulos, Kastritis et al., Epidemiology and organ specific sequelae of post-acute COVID19: A narrative review, J. Infect, doi:10.1016/j.jinf.2021.05.004
Lazzerini, Laghi-Pasini, Boutjdir, Capecchi, Cardioimmunology of arrhythmias: The role of autoimmune and inflammatory cardiac channelopathies, Nat. Rev. Immunol, doi:10.1038/s41577-018-0098-z
Lee, Hui, Lee, Satti, Shum et al., Sulfonylurea Is Associated With Higher Risks of Ventricular Arrhythmia or Sudden Cardiac Death Compared With Metformin: A Population-Based Cohort Study, J. Am. Heart Assoc, doi:10.1161/JAHA.122.026289
Liu, Bai, Liu, Zhang, Qin et al., Metformin improves lipid metabolism and reverses the Warburg effect in a canine model of chronic atrial fibrillation, BMC Cardiovasc. Disord, doi:10.1186/s12872-020-01359-7
Liu, Hua, Fu, Pan, Li et al., Metformin regulates the expression of SK2 and SK3 in the atria of rats with type 2 diabetes mellitus through the NOX4/p38MAPK signaling pathway, J. Cardiovasc. Pharmacol, doi:10.1097/FJC.0000000000000615
Mascarenhas, Downey, Schwartz, Adabag, Antiarrhythmic effects of metformin, Heart Rhythm O, doi:10.1016/j.hroo.2024.04.003
Peretto, Sala, Rizzo, De Luca, Campochiaro et al., Arrhythmias in myocarditis: State of the art, Heart Rhythm, doi:10.1016/j.hrthm.2018.11.024
Puntmann, Carerj, Wieters, Fahim, Arendt et al., Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19), JAMA Cardiol, doi:10.1001/jamacardio.2020.3557
Reynbakh, Braunstein, Hsu, Ellis, Crosson et al., Arrhythmia patterns during and after hospitalization for COVID-19 infection detected via patch-based mobile cardiac telemetry, Am. Heart J. Plus Cardiol. Res. Pract, doi:10.1016/j.ahjo.2022.100084
Rizos, Rigopoulos, Kalogeropoulos, Tsiodras, Dragomanovits et al., Hypertension and paroxysmal atrial fibrillation: A novel predictive role of high sensitivity C-reactive protein in cardioversion and long-term recurrence, J. Hum. Hypertens, doi:10.1038/jhh.2009.89
Rodríguez Rodríguez, Gómez Gómez-Acebo, Del Olmo, Rodriguez Ledo, Pacheco Delgado et al., Guía Clínica para la Atención al Paciente LONG COVID/COVID Persistente
Saha, Russo, Chung, Deering, Lakkireddy et al., COVID-19 and Cardiac Arrhythmias: A Contemporary Review, Curr. Treat. Options Cardiovasc. Med, doi:10.1007/s11936-022-00964-3
Vetrone, Zaccardi, Webb, Seidu, Gholap et al., Cardiovascular and mortality events in type 2 diabetes cardiovascular outcomes trials: A systematic review with trend analysis, Acta Diabetol, doi:10.1007/s00592-018-1253-5
Wang, Hu, Hu, Zhu, Liu et al., Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China, JAMA, doi:10.1001/jama.2020.1585
Zamani, Tabatabizadeh, Gilasi, Yazdani, Effects of pioglitazone and linagliptin on glycemic control, lipid profile and hs-CRP in metformin-treated patients with type 2 diabetes: A comparative study, Horm. Mol. Biol. Clin. Investig, doi:10.1515/hmbci-2022-0070
DOI record:
{
"DOI": "10.3390/life16020319",
"ISSN": [
"2075-1729"
],
"URL": "http://dx.doi.org/10.3390/life16020319",
"abstract": "<jats:p>Background: Cardiac arrhythmias are a frequent complication of acute SARS-CoV-2 infection. However, their long-term prevalence and clinical determinants among patients with post-COVID-19 syndrome, especially those previously hospitalized, remain poorly defined. Objectives: To assess the prevalence and types of arrhythmias in long COVID patients following hospitalization and to identify associated clinical risk factors. Methods: In this cross-sectional study, 53 patients previously hospitalized with confirmed COVID-19 were evaluated ≥3 months post-infection. All participants underwent a standardized clinical assessment, 12-lead electrocardiography, and 24 h Holter monitoring. Logistic and Cox regression analyses were performed to identify predictors of arrhythmia. Results: Arrhythmias were identified in 41.5% (n = 22) of patients. Atrial fibrillation (32%) was the most frequent arrhythmia, followed by sinus bradycardia (27%) and sinus tachycardia (18%). Age (OR 1.06, 95% CI 1.01–1.10, p = 0.01) and length of hospital stay (OR 1.1, 95% CI 1.01–1.2, p = 0.04) were independently associated with arrhythmia. Biguanide (metformin) therapy was inversely associated with the occurrence of arrhythmia (Exp(B) = 0.017, p = 0.008). Dyspnea (82.4%) and palpitations (41.5%) were the most commonly reported symptoms. Conclusions: Arrhythmias are common in patients with long COVID following severe disease. Advanced age and prolonged hospitalization are significant risk factors, while biguanide use may offer a protective effect. These findings underscore the need for targeted cardiac surveillance in this population.</jats:p>",
"alternative-id": [
"life16020319"
],
"author": [
{
"affiliation": [
{
"name": "Unidad de Cardiología, Del Hospital Civil Fray Antonio Alcalde, Guadalajara 44200, Mexico"
}
],
"family": "Morales-Vazquez",
"given": "Haydee Ninette",
"sequence": "first"
},
{
"ORCID": "https://orcid.org/0000-0002-9470-2489",
"affiliation": [
{
"name": "Instituto de Terapéutica Experimental y Clínica, Centro Universitario de Ciencias de La Salud, Universidad de Guadalajara, Guadalajara 44340, Mexico"
}
],
"authenticated-orcid": false,
"family": "Cardona-Müller",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Instituto de Terapéutica Experimental y Clínica, Centro Universitario de Ciencias de La Salud, Universidad de Guadalajara, Guadalajara 44340, Mexico"
}
],
"family": "Grover-Paez",
"given": "Fernando",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Instituto de Terapéutica Experimental y Clínica, Centro Universitario de Ciencias de La Salud, Universidad de Guadalajara, Guadalajara 44340, Mexico"
}
],
"family": "Ramos-Becerra",
"given": "Carlos Gerardo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Instituto de Terapéutica Experimental y Clínica, Centro Universitario de Ciencias de La Salud, Universidad de Guadalajara, Guadalajara 44340, Mexico"
}
],
"family": "Cardona-Muñoz",
"given": "Ernesto Germán",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Instituto de Terapéutica Experimental y Clínica, Centro Universitario de Ciencias de La Salud, Universidad de Guadalajara, Guadalajara 44340, Mexico"
}
],
"family": "Ramos-Zavala",
"given": "Maria Guadalupe",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Instituto de Terapéutica Experimental y Clínica, Centro Universitario de Ciencias de La Salud, Universidad de Guadalajara, Guadalajara 44340, Mexico"
}
],
"family": "Carmona-Huerta",
"given": "Jaime",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0009-0005-4438-5875",
"affiliation": [
{
"name": "Instituto de Terapéutica Experimental y Clínica, Centro Universitario de Ciencias de La Salud, Universidad de Guadalajara, Guadalajara 44340, Mexico"
}
],
"authenticated-orcid": false,
"family": "Hernandez-del-Rio",
"given": "Jorge Eduardo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Unidad de Cardiología, Del Hospital Civil Fray Antonio Alcalde, Guadalajara 44200, Mexico"
}
],
"family": "Miranda-Aquino",
"given": "Tomas",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-7086-2966",
"affiliation": [
{
"name": "Instituto de Terapéutica Experimental y Clínica, Centro Universitario de Ciencias de La Salud, Universidad de Guadalajara, Guadalajara 44340, Mexico"
}
],
"authenticated-orcid": false,
"family": "Gonzalez-Padilla",
"given": "Christian",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0003-0563-5294",
"affiliation": [
{
"name": "Instituto de Terapéutica Experimental y Clínica, Centro Universitario de Ciencias de La Salud, Universidad de Guadalajara, Guadalajara 44340, Mexico"
}
],
"authenticated-orcid": false,
"family": "Lopez-Gradilla",
"given": "Christopher Josue",
"sequence": "additional"
}
],
"container-title": "Life",
"container-title-short": "Life",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2026,
2,
12
]
],
"date-time": "2026-02-12T09:48:34Z",
"timestamp": 1770889714000
},
"deposited": {
"date-parts": [
[
2026,
2,
12
]
],
"date-time": "2026-02-12T10:16:48Z",
"timestamp": 1770891408000
},
"indexed": {
"date-parts": [
[
2026,
2,
12
]
],
"date-time": "2026-02-12T11:14:43Z",
"timestamp": 1770894883278,
"version": "3.50.1"
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2026,
2,
12
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2026,
2
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2026,
2,
12
]
],
"date-time": "2026-02-12T00:00:00Z",
"timestamp": 1770854400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2075-1729/16/2/319/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "319",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2026,
2,
12
]
]
},
"published-online": {
"date-parts": [
[
2026,
2,
12
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.3390/ph16060844",
"doi-asserted-by": "crossref",
"key": "ref_1",
"unstructured": "Kingma, J., Simard, C., and Drolet, B. (2023). Overview of Cardiac Arrhythmias and Treatment Strategies. Pharmaceuticals, 16."
},
{
"DOI": "10.1016/j.ahjo.2022.100084",
"article-title": "Arrhythmia patterns during and after hospitalization for COVID-19 infection detected via patch-based mobile cardiac telemetry",
"author": "Reynbakh",
"doi-asserted-by": "crossref",
"first-page": "100084",
"journal-title": "Am. Heart J. Plus Cardiol. Res. Pract.",
"key": "ref_2",
"volume": "13",
"year": "2022"
},
{
"key": "ref_3",
"unstructured": "Rodríguez Rodríguez, E., Gómez Gómez-Acebo, F., Armenteros del Olmo, L., Rodriguez Ledo, M., Pacheco Delgado, M., Prieto Menchero, S., Gras Nieto, E., Nuño González, A., Ramos Gómez, F., and Inglés Novvell, M. (2021). Guía Clínica para la Atención al Paciente LONG COVID/COVID Persistente, Sociedad Española de Médicos Generales y de Familia (SEMG). (Documento colaborativo entre colectivos de pacientes y sociedades cientificas N.° 1; Guía clínica para la atención al paciente long covid/covid persistente)."
},
{
"key": "ref_4",
"unstructured": "National Institute for Health and Care Excellence (NICE), Scottish Intercollegiate Guidelines Network (SIGN), and Royal College of General Practitioners (RCGP) (2022). COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19, NICE.org."
},
{
"DOI": "10.1136/openhrt-2021-001758",
"article-title": "Prospective arrhythmia surveillance after a COVID-19 diagnosis",
"author": "Dewland",
"doi-asserted-by": "crossref",
"first-page": "e001758",
"journal-title": "Open Heart",
"key": "ref_5",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1038/s41591-020-0968-3",
"article-title": "Extrapulmonary manifestations of COVID-19",
"author": "Gupta",
"doi-asserted-by": "crossref",
"first-page": "1017",
"journal-title": "Nat. Med.",
"key": "ref_6",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.amjms.2020.10.002",
"article-title": "Cardiac Involvement of COVID-19: A Comprehensive Review",
"author": "Chang",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "Am. J. Med. Sci.",
"key": "ref_7",
"volume": "361",
"year": "2021"
},
{
"DOI": "10.1007/s11936-022-00964-3",
"article-title": "COVID-19 and Cardiac Arrhythmias: A Contemporary Review",
"author": "Saha",
"doi-asserted-by": "crossref",
"first-page": "87",
"journal-title": "Curr. Treat. Options Cardiovasc. Med.",
"key": "ref_8",
"volume": "24",
"year": "2022"
},
{
"DOI": "10.35839/repis.6.2.1326",
"article-title": "Diagnóstico de arritmias ventriculares en pacientes con síndrome post COVID-19",
"doi-asserted-by": "crossref",
"first-page": "101",
"journal-title": "Rev. Peruana Investig. Salud",
"key": "ref_9",
"volume": "6",
"year": "2022"
},
{
"DOI": "10.1038/s41586-021-03553-9",
"article-title": "High-dimensional characterization of post-acute sequelae of COVID-19",
"author": "Xie",
"doi-asserted-by": "crossref",
"first-page": "259",
"journal-title": "Nature",
"key": "ref_10",
"volume": "594",
"year": "2021"
},
{
"DOI": "10.1038/s41577-018-0098-z",
"article-title": "Cardioimmunology of arrhythmias: The role of autoimmune and inflammatory cardiac channelopathies",
"author": "Lazzerini",
"doi-asserted-by": "crossref",
"first-page": "63",
"journal-title": "Nat. Rev. Immunol.",
"key": "ref_11",
"volume": "19",
"year": "2019"
},
{
"DOI": "10.1016/j.jinf.2021.05.004",
"article-title": "Epidemiology and organ specific sequelae of post-acute COVID19: A narrative review",
"author": "Korompoki",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "J. Infect.",
"key": "ref_12",
"volume": "83",
"year": "2021"
},
{
"DOI": "10.1093/cvr/cvaa324",
"article-title": "Cardiac fibrosis",
"author": "Frangogiannis",
"doi-asserted-by": "crossref",
"first-page": "1450",
"journal-title": "Cardiovasc. Res.",
"key": "ref_13",
"volume": "117",
"year": "2021"
},
{
"DOI": "10.1016/j.hrthm.2018.11.024",
"article-title": "Arrhythmias in myocarditis: State of the art",
"author": "Peretto",
"doi-asserted-by": "crossref",
"first-page": "793",
"journal-title": "Heart Rhythm.",
"key": "ref_14",
"volume": "16",
"year": "2019"
},
{
"DOI": "10.1001/jamacardio.2020.3557",
"article-title": "Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19)",
"author": "Puntmann",
"doi-asserted-by": "crossref",
"first-page": "1265",
"journal-title": "JAMA Cardiol.",
"key": "ref_15",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.1585",
"article-title": "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1061",
"journal-title": "JAMA",
"key": "ref_16",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1007/s00592-018-1253-5",
"article-title": "Cardiovascular and mortality events in type 2 diabetes cardiovascular outcomes trials: A systematic review with trend analysis",
"author": "Vetrone",
"doi-asserted-by": "crossref",
"first-page": "331",
"journal-title": "Acta Diabetol.",
"key": "ref_17",
"volume": "56",
"year": "2019"
},
{
"DOI": "10.1016/j.diabres.2023.110626",
"article-title": "Association between antidiabetic drugs and the incidence of atrial fibrillation in patients with type 2 diabetes: A nationwide cohort study in South Korea",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "110626",
"journal-title": "Diabetes Res. Clin. Pract.",
"key": "ref_18",
"volume": "198",
"year": "2023"
},
{
"DOI": "10.1161/JAHA.122.026289",
"article-title": "Sulfonylurea Is Associated With Higher Risks of Ventricular Arrhythmia or Sudden Cardiac Death Compared With Metformin: A Population-Based Cohort Study",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "e026289",
"journal-title": "J. Am. Heart Assoc.",
"key": "ref_19",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1016/j.hroo.2024.04.003",
"article-title": "Antiarrhythmic effects of metformin",
"author": "Mascarenhas",
"doi-asserted-by": "crossref",
"first-page": "310",
"journal-title": "Heart Rhythm O2",
"key": "ref_20",
"volume": "5",
"year": "2024"
},
{
"DOI": "10.3389/fphys.2018.01669",
"doi-asserted-by": "crossref",
"key": "ref_21",
"unstructured": "Grisanti, L.A. (2018). Diabetes and Arrhythmias: Pathophysiology, Mechanisms and Therapeutic Outcomes. Front. Physiol., 9."
},
{
"DOI": "10.1097/FJC.0000000000000615",
"article-title": "Metformin regulates the expression of SK2 and SK3 in the atria of rats with type 2 diabetes mellitus through the NOX4/p38MAPK signaling pathway",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "205",
"journal-title": "J. Cardiovasc. Pharmacol.",
"key": "ref_22",
"volume": "72",
"year": "2018"
},
{
"DOI": "10.1186/s12872-020-01359-7",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "Liu, Y., Bai, F., Liu, N., Zhang, B., Qin, F., Tu, T., Li, B., Li, J., Ma, Y., and Ouyang, F. (2020). Metformin improves lipid metabolism and reverses the Warburg effect in a canine model of chronic atrial fibrillation. BMC Cardiovasc. Disord., 20."
},
{
"DOI": "10.1371/journal.pone.0102374",
"doi-asserted-by": "crossref",
"key": "ref_24",
"unstructured": "Apaijai, N., Chinda, K., Palee, S., Chattipakorn, S., and Chattipakorn, N. (2014). Combined vildagliptin and metformin exert better cardioprotection than monotherapy against ischemia-reperfusion injury in obese-insulin resistant rats. PLoS ONE, 9."
},
{
"DOI": "10.1038/jhh.2009.89",
"article-title": "Hypertension and paroxysmal atrial fibrillation: A novel predictive role of high sensitivity C-reactive protein in cardioversion and long-term recurrence",
"author": "Rizos",
"doi-asserted-by": "crossref",
"first-page": "447",
"journal-title": "J. Hum. Hypertens.",
"key": "ref_25",
"volume": "24",
"year": "2010"
},
{
"DOI": "10.3389/fmed.2024.1346646",
"doi-asserted-by": "crossref",
"key": "ref_26",
"unstructured": "Iam-Arunthai, K., Chamnanchanunt, S., Thungthong, P., Chinapha, A., Nakhahes, C., Suwanban, T., and Umemura, T. (2024). COVID-19 with high-sensitivity CRP associated with worse dynamic clinical parameters and outcomes. Front. Med., 11."
},
{
"DOI": "10.1515/hmbci-2022-0070",
"article-title": "Effects of pioglitazone and linagliptin on glycemic control, lipid profile and hs-CRP in metformin-treated patients with type 2 diabetes: A comparative study",
"author": "Zamani",
"doi-asserted-by": "crossref",
"first-page": "385",
"journal-title": "Horm. Mol. Biol. Clin. Investig.",
"key": "ref_27",
"volume": "44",
"year": "2024"
},
{
"DOI": "10.1016/j.eclinm.2021.101019",
"article-title": "Characterizing long COVID in an international cohort: 7 months of symptoms and their impact",
"author": "Davis",
"doi-asserted-by": "crossref",
"first-page": "101019",
"journal-title": "EClinicalMedicine",
"key": "ref_28",
"volume": "38",
"year": "2021"
}
],
"reference-count": 28,
"references-count": 28,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2075-1729/16/2/319"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Arrhythmias as Part of Long COVID Syndrome in Hospitalized Patients That Survived a Severe COVID-19 Infection and the Potential Protective Role of Metformin in These Patients",
"type": "journal-article",
"update-policy": "https://doi.org/10.3390/mdpi_crossmark_policy",
"volume": "16"
}
