The preventive and protective role of melatonin in SARS-CoV-2 infection: a retrospective study
et al., Melatonin Research, doi:10.32794/mr112500159, Sep 2023
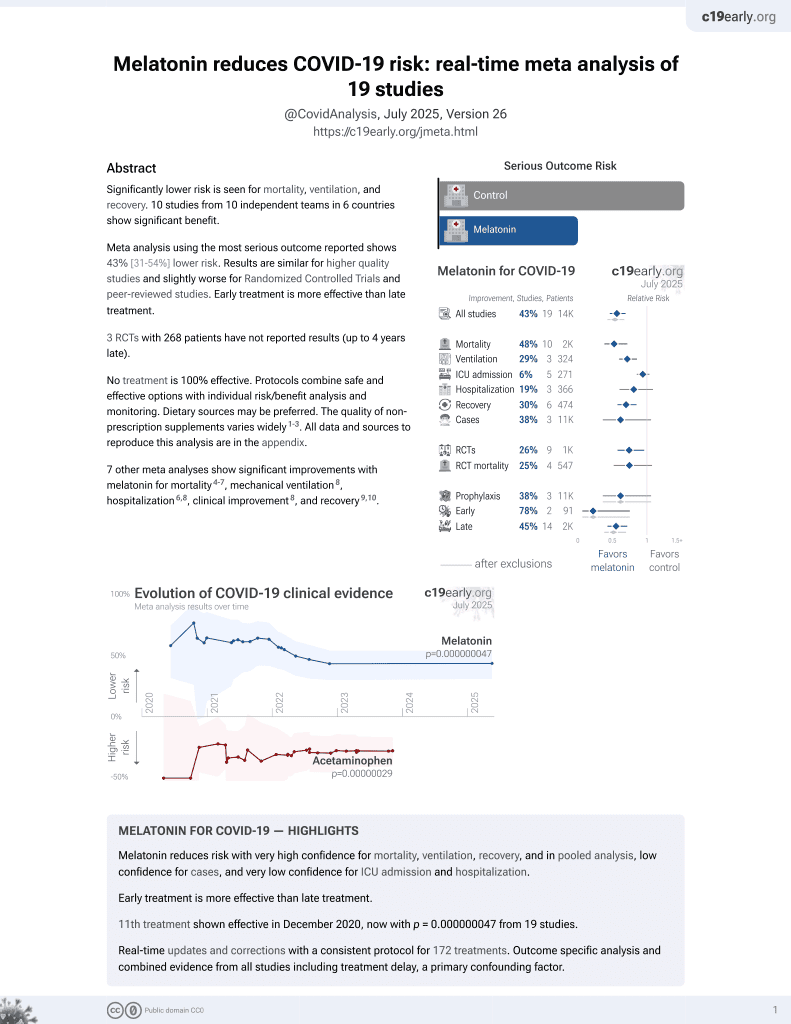
Melatonin for COVID-19
12th treatment shown to reduce risk in
December 2020, now with p = 0.0000000099 from 19 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 62 patients taking relatively high doses of melatonin since before the pandemic, showing relatively low incidence of COVID-19, and relatively mild cases. There were 7 PCR+ cases, 3 asymptomatic, 3 mild, and one moderate. Patients taking ≥40mg had lower incidence of cases, without statistical significance. There was no control group. A dose response relationship is seen in meta analysis of controlled studies to date:1.
|
risk of case, 69.1% lower, RR 0.31, p = 0.22, treatment 2 of 35 (5.7%), control 5 of 27 (18.5%), NNT 7.8, ≥40mg vs. <40mg.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Molina-Carballo et al., 30 Sep 2023, retrospective, Spain, peer-reviewed, survey, mean age 58.5, 6 authors.
Contact: amolinac@ugr.es (corresponding author), amunozh@ugr.es.
The preventive and protective role of melatonin in SARS-CoV-2 infection: a retrospective study
Melatonin Research, doi:10.32794/mr112500159
This study has investigated the protective role of melatonin against SARS-CoV-2 infection. For this purpose, 62 adults were recruited who were in daily relatively high doses of melatonin intaking, with the particularity that they started taking it before the beginning of the COVID-19 pandemic and continued to present. A continuous validation process has been carried out with a series of questionnaires to identify the risk factors, whether they were contacts, were infected, if yes, the level of disease severity, need for treatment, hospitalization, etc. According to the dose of melatonin the individuals took/are taking, they were divided into two groups: a) those taking 20 mg (n = 27) and, b) those taking ≥ 40 mg (n = 32). For statistical analysis, the shi2 test and Fisher's exact test were used. The number of infected subjects with positive PCR was 7 (11.9%). Only one required medication, the rest had a very favorable clinical evolution, mild in three cases and asymptomatic in three others. While in their environment this percentage is 22.05% (chi2 = 2.928; p < 0.087). Melatonin offers a good safety profile, is well tolerated and can play an important role in the different levels of COVID-19 prevention.
CONFLICTS OF INTEREST: Authors declare no condlicts of interests.
References
Acuña-Castroviejo, Escames, Figueira, Clinical trial to test the efficacy of melatonin in COVID-19, J. Pineal Res
Acuña-Castroviejo, Escames, Macías, Cell protective role of melatonin in the brain, J. Pineal Res
Acuña-Castroviejo, Pablos, Menendez-Pelaez, Melatonin receptors in purified cell nuclei of liver, Res. Commun. Chem. Pathol. Pharmacol
Ahmadi, Ashrafizadeh, Melatonin as a potential modulator of Nrf2, Fundam. Clin. Pharmacol
Alghamdi, The neuroprotective role of melatonin in neurological disorders, J. Neurosci. Res
Allegra, Gentile, Tesoriere, Protective effect of melatonin against cytotoxic actions of malondialdehyde: an in vitro study on human erythrocytes, J. Pineal Res
Ameri, Asadi, Kamali, Evaluation of the effect of melatonin in patients with COVID-19-induced pneumonia admitted to the Intensive Care Unit: A structured summary of a study protocol for a randomized controlled trial, Trials
Andersen, Gögenur, Rosenberg, The safety of melatonin in humans, Clin. Drug Investig
Andersen, Werner, Rosenberg, A systematic review of peri-operative melatonin, Anaesthesia
Artigas, Coma, Matos-Filipe, In-silico drug repurposing study predicts the combination of pirfenidone and melatonin as a promising candidate therapy to reduce SARS-CoV-2 infection progression and respiratory distress caused by cytokine storm, PLoS One
Ayala, Muñoz, Argüelles, Lipid peroxidation: production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal, Oxid. Med. Cell Longev
Balduini, Weiss, Carloni, Melatonin pharmacokinetics and dose extrapolation after enteral infusion in neonates subjected to hypothermia, J. Pineal Res
Barthélémy, Limbourg, Collet, Impact of non-steroidal antiinflammatory drugs (NSAIDs) on cardiovascular outcomes in patients with stable atherothrombosis or multiple risk factors, Int. J. Cardiol
Bazyar, Gholinezhad, Moradi, The effects of melatonin supplementation in adjunct with non-surgical periodontal therapy on periodontal status, serum melatonin and inflammatory markers in type 2 diabetes mellitus patients with chronic periodontitis: a doubleblind, placebo-controlled trial, Inflammopharmacology
Becker-André, Wiesenberg, Schaeren-Wiemers, Pineal gland hormone melatonin binds and activates an orphan of the nuclear receptor superfamily, J. Biol. Chem
Benítez-King, Tay, Calmodulin mediates melatonin cytoskeletal effects, Experientia
Besag, Vasey, Lao, Adverse events associated with melatonin for the treatment of primary or secondary sleep disorders: A systematic review, CNS Drugs
Boga, Coto-Montes, Sa, Beneficial actions of melatonin in the management of viral infections: a new use for this "molecular handyman, Rev. Med. Virol
Bonmati-Carrion, Loba, Melatonin and cancer: A polyhedral network where the source matters, Antioxidants (Basel)
Brzezinski, Vangel, Wurtman, Effects of exogenous melatonin on sleep: a meta-analysis, Sleep Med. Rev
Bubenik, Localization, physiological significance and possible clinical implication of gastrointestinal melatonin, Biol. Signals Recept
Cardinali, Brown, Reiter, Elderly as a high-risk group during COVID-19 pandemic: Effect of circadian misalignment, sleep dysregulation and melatonin administration, sleep vigil
Cardinali, Brown, Sr, Can Melatonin Be a Potential "Silver Bullet, Treating COVID-19 Patients? Diseases
Cardinali, Melatonin and healthy aging, Vitam. Horm
Cardinali, Srinivasan, Brzezinski, Melatonin and its analogs in insomnia and depression, J. Pineal Res
Carrascal, Nunez-Abades, Ayala, Role of melatonin in the inflammatory process and its therapeutic potential, Curr. Pharm. Des
Carrillo-Vico, Reiter, Lardone, The modulatory role of melatonin on immune responsiveness, Curr. Opin. Investig. Drugs
Carvalho-Sousa, Pereira, Kinker, Immune-pineal axis protects rat lungs exposed to polluted air, J. Pineal Res
Castrillón, Esquifino, Varas, Effect of melatonin treatment on 24-h variations in responses to mitogens and lymphocyte subset populations in rat submaxillary lymph nodes, J. Neuroendocrinol
Castroviejo, Escames, Carazo, Melatonin, mitochondrial homeostasis and mitochondrial-related diseases, Curr. Top. Med. Chem
Cernysiov, Gerasimcik, Mauricas, Regulation of T-cell-independent and T-cell-dependent antibody production by circadian rhythm and melatonin, Int. Immunol
Chahbouni, López, Molina-Carballo, Melatonin treatment reduces oxidative damage and normalizes plasma pro-inflammatory cytokines in patients suffering from charcot-marie-tooth neuropathy: A pilot study in three children, Molecules
Checa-Ros, Muñoz-Gallego, Muñoz-Gallego, Clinical considerations derived from the administration of melatonin to children with sleep disorders, Pediatr. Neurol
Checa-Ros, Muñoz-Hoyos, Molina-Carballo, Analysis of different melatonin secretion patterns in children with sleep disorders: melatonin secretion patterns in children, J. Child. Neurol
Chen, Zhou, Chen, Knowledge, perceived beliefs, and preventive behaviors related to COVID-19 among chinese older adults: Cross-sectional web-based survey, J. Med. Internet. Res
Chitimus, Popescu, Voiculescu, Melatonin's impact on antioxidative and anti-inflammatory reprogramming in homeostasis and disease, Biomolecules
Ciftçi, Bilici, Küfrevioğlu, Effects of melatonin on enzyme activities of glucose-6-phosphate dehydrogenase from human erythrocytes in vitro and from rat erythrocytes in vivo, Pharmacol. Res
Citera, Arias, Maldonado-Cocco, The effect of melatonin in patients with fibromyalgia: a pilot study, Clin. Rheumatol
Crespo, Fernández-Palanca, San-Miguel, Melatonin modulates mitophagy, innate immunity and circadian clocks in a model of viral-induced fulminant hepatic failure, J. Cell Mol. Med
Cross, Landis, Sehgal, Melatonin for the early treatment of COVID-19: A narrative review of current evidence and possible efficacy, Endocr. Pract
Csaba, The pineal regulation of the immune system: 40 years since the discovery, Acta Microbiol. Immunol. Hung
Cuesta, Cerezuela, In vivo actions of melatonin on the innate immune parameters in the teleost fish gilthead seabream, J. Pineal Res
Duan, Guo, Yang, Modeling COVID-19 with human pluripotent stem cell-derived cells reveals synergistic effects of anti-inflammatory macrophages with ACE2 inhibition Against SARS-CoV-2, Res. Sq
Dubocovich, Melatonin receptors: are there multiple subtypes?, Trends Pharmacol. Sci
Ekmekcioglu, Melatonin receptors in humans: biological role and clinical relevance, Biomed. Pharmacother
El-Missiry, El-Missiry, Othman, Melatonin is a potential adjuvant to improve clinical outcomes in individuals with obesity and diabetes with coexistence of Covid-19, Eur. J. Pharmacol
Estaras, Moreno, Santofimia-Castaño, Melatonin induces reactive oxygen species generation and changes in glutathione levels and reduces viability in human pancreatic stellate cells, J. Physiol. Biochem
Fan, He, Guan, Involvement of the nitric oxide in melatonin-mediated protection against injury, Life Sci
Feng, Adeniran, Huang, The ameliorative effect of melatonin on LPSinduced Sertoli cells inflammatory and tight junctions damage via suppression of the TLR4/MyD88/NF-κB signaling pathway in newborn calf, Theriogenology
Fernandes, Kinker, Navarro, Melatonin-Index as a biomarker for predicting the distribution of presymptomatic and asymptomatic SARS-CoV-2 carriers, Melatonin Res
Ferracioli-Oda, Qawasmi, Bloch, Meta-analysis: Melatonin for the treatment of primary sleep disorders, Focus (Am Psychiatr Publ)
Fischer, Kleszczyński, Hardkop, Melatonin enhances antioxidative enzyme gene expression (CAT, GPx, SOD), prevents their UVR-induced depletion, and protects against the formation of DNA damage (8-hydroxy-2'-deoxyguanosine) in ex vivo human skin, J. Pineal Res
Fischer, Scholz, Knöll, Melatonin suppresses reactive oxygen species induced by UV irradiation in leukocytes, J. Pineal Res
Foley, Steel, Adverse events associated with oral administration of melatonin: A critical systematic review of clinical evidence, Complement. Ther. Med
Fulia, Gitto, Cuzzocrea, Increased levels of malondialdehyde and nitrite/nitrate in the blood of asphyxiated newborns: reduction by melatonin, J. Pineal Res
Galano, Tan, Reiter, Melatonin as a natural ally against oxidative stress: a physicochemical examination, J. Pineal Res
Genario, Giacomini, De Abreu, Sex differences in adult zebrafish anxiolytic-like responses to diazepam and melatonin, Eur. J. Clin. Pharmacol
Genario, Morello, Bueno, The usefulness of melatonin in the field of obstetrics and gynecology, Pharmacol. Res
Gibbs, Dallon, Lewis, Diesel exhaust particle exposure compromises alveolar macrophage mitochondrial bioenergetics, Int. J. Mol. Sci
Goc, Szaroma, Kapusta, Protective effects of melatonin on the activity of SOD, CAT, GSH-Px and GSH content in organs of mice after administration of SNP, Chin. J. Physiol
González, Jirano, Martínez, A comparative study of melatonin and immunomodulatory therapy with interferon beta and glatiramer acetate in a mouse model of multiple sclerosis, Neurologia (Engl Ed)
Guerrero, Reiter, Melatonin-immune system relationships, Curr. Top. Med. Chem
Gupta, Gupta, Agarwal, A randomized, double-blind, placebo controlled trial of melatonin add-on therapy in epileptic children on valproate monotherapy: effect on glutathione peroxidase and glutathione reductase enzymes, Br. J. Clin. Pharmacol
Gurunathan, Kang, Choi, Melatonin: A potential therapeutic agent against COVID-19, Melatonin Res
Habtemariam, Daglia, Sureda, Melatonin and respiratory diseases: A review, Curr. Top. Med. Chem
Hardeland, Aging, melatonin, and the pro-and anti-inflammatory networks, Int. J. Mol. Sci
Hardeland, Taxon-and Site-specific melatonin catabolism, Molecules
Hardeland, Wang, Yang, Peng, Ginsenoside Rg1 regulates SIRT1 to ameliorate sepsis-induced lung inflammation and injury via inhibiting endoplasmic reticulum stress and inflammation, Mediators Inflamm
Hasan, Atrakji, Mehuaiden, The Effect of Melatonin on thrombosis, sepsis and mortality rate in COVID-19 patients, Int. J. Infect. Dis
Hasan, Islam, Matsumoto, Meta-analysis of single-cell RNA-seq data reveals phenotypic switching of immune cells in severe COVID-19 patients, Comput. Biol. Med
He, Wu, Zhang, Bacteriostatic potential of melatonin: therapeutic standing and mechanistic insights, Front. Immunol
Herxheimer, Petrie, Melatonin for the prevention and treatment of jet lag, Cochrane Database Syst. Rev
Hilli, Korhonen, Turpeinen, The effect of oral contraceptives on the pharmacokinetics of melatonin in healthy subjects with CYP1A2 g.-163C>A polymorphism, J. Clin. Pharmacol
Huang, Cao, Liu, Inhibitory effect of melatonin on lung oxidative stress induced by respiratory syncytial virus infection in mice, J. Pineal Res
Huggard, Kelly, Worrall, Melatonin as an immunomodulator in children with Down syndrome, Pediatr. Res
Härtter, Grözinger, Weigmann, Increased bioavailability of oral melatonin after fluvoxamine coadministration, Clin. Pharmacol. Ther
Härtter, Nordmark, Rose, Effects of caffeine intake on the pharmacokinetics of melatonin, a probe drug for CYP1A2 activity, Br. J. Clin. Pharmacol
Ingrasciotta, Sultana, Giorgianni, Association of individual non-steroidal anti-inflammatory drugs and chronic kidney disease: a population-based case control study, PLoS One
Jahnke, Marr, Myers, Maternal and developmental toxicity evaluation of melatonin administered orally to pregnant Sprague-Dawley rats, Toxicol. Sci
Jamilian, Foroozanfard, Mirhosseini, Effects of melatonin supplementation on hormonal, inflammatory, genetic, and oxidative stress parameters in women with polycystic ovary syndrome, Front. Endocrinol
Jauhari, Baranov, Suofu, Melatonin inhibits cytosolic mitochondrial DNA-induced neuroinflammatory signaling in accelerated aging and neurodegeneration, J. Clin. Invest
Jerez-Calero, Salvatierra-Cuenca, Benitez-Feliponi, The benefits of four weeks of melatonin treatment on circadian patterns in resistance-trained athletes, Pediatr. Crit. Care Med
Kakhaki, Ostadmohammadi, Kouchaki, Melatonin supplementation and the effects on clinical and metabolic status in Parkinson's disease: A randomized, double-blind, placebo-controlled trial, Clin. Neurol. Neurosurg
Kehlet, Postoperative opioid sparing to hasten recovery: what are the issues?, Anesthesiology
Kehlet, Wilmore, Evidence-based surgical care and the evolution of fasttrack surgery, Ann. Surg
Klein, Gögenur, Rosenberg, Davis, Postoperative use of non-steroidal antiinflammatory drugs in patients with anastomotic leakage requiring reoperation after colorectal resection: cohort study based on prospective data, Clin. Dermatol
Knapp, Leemans, Florquin, Alveolar macrophages have a protective antiinflammatory role during murine pneumococcal pneumonia, Am. J. Respir. Crit. Care Med
Kow, Ramachandram, Hasan, Melatonin: Revisited role as vaccine adjuvant during outbreaks of COVID-19 caused by the delta variant, J. Neuroimmune Pharmacol
Kücükakin, Lykkesfeldt, Nielsen, Utility of melatonin to treat surgical stress after major vascular surgery--a safety study, J. Pineal Res
Lader, Benzodiazepine harm: how can it be reduced?, Br. J. Clin. Pharmacol
Lanas, Carrera-Lasfuentes, Arguedas, Risk of upper and lower gastrointestinal bleeding in patients taking nonsteroidal anti-inflammatory drugs, antiplatelet agents, or anticoagulants, Clin. Gastroenterol. Hepatol
Leavel, Clark, Preventive Medicine for the Doctor in His Community
Li, Li, Niu, Several considerations on the establishment of a new public health and preventive medicine system in national level, Zhonghua Yu Fang Yi Xue Za Zhi
Ling, Li, Zhang, MicroRNA-494 inhibition alleviates acute lung injury through Nrf2 signaling pathway via NQO1 in sepsis-associated acute respiratory distress syndrome, Life Sci
Liu, Gan, Xu, Melatonin alleviates inflammasome-induced pyroptosis through inhibiting NF-κB/GSDMD signal in mice adipose tissue, J. Pineal Res
Liu, Wang, Zhao, The effect and mechanisms of melatonin on the proliferation and apoptosis of lung cancer cells, Bioengineered
Loren, Sánchez, Arias, Melatonin scavenger properties against oxidative and nitrosative stress: impact on gamete handling and in vitro embryo production in humans and other mammals, Int. J. Mol. Sci
Luo, Song, Zhang, Melatonin mediated Foxp3-downregulation decreases cytokines production via the TLR2 and TLR4 pathways in H. pylori infected mice, Int. Immunopharmacol
Maestroni, The immunoneuroendocrine role of melatonin, J. Pineal Res
Majima, Oberley, Furukawa, Prevention of mitochondrial injury by manganese superoxide dismutase reveals a primary mechanism for alkaline-induced cell death, J. Biol. Chem
Maldonado, García-Moreno, Yanes, Possible involvement of the inhibition of NF-κB factor in anti-inflammatory actions that melatonin exerts on mast cells, J. Cell Biochem
Maldonado, Mora-Santos, Naji, Evidence of melatonin synthesis and release by mast cells. Possible modulatory role on inflammation, Pharmacol. Res
Markus, Sousa, Da, Cruz-Machado, Possible role of pineal and extra-pineal melatonin in surveillance, immunity, and first-line defense, Int. J. Mol. Sci
Mehrzadi, Karimi, Fatemi, SARS-CoV-2 and other coronaviruses negatively influence mitochondrial quality control: beneficial effects of melatonin, Pharmacol. Ther
Mehrzadi, Safa, Kamrava, Protective mechanisms of melatonin against hydrogen-peroxide-induced toxicity in human bone-marrow-derived mesenchymal stem cells, Can. J. Physiol. Pharmacol
Menczel Schrire, Phillips, Chapman, Safety of higher doses of melatonin in adults: A systematic review and meta-analysis, J. Pineal Res
Mills, Wu, Seely, Melatonin in the treatment of cancer: a systematic review of randomized controlled trials and meta-analysis, J. Pineal Res
Molina-Carballo, Jerez-Calero, Fernández-López, Augustin-Morales, Del et al., The preventive and protective role of melatonin in SARS-CoV-2 infection: a retrospective study, Melatonin Research
Morgan, Barrett, Howell, Melatonin receptors: localization, molecular pharmacology and physiological significance, Neurochem. Int
Morvaridzadeh, Sadeghi, Agah, Effect of melatonin on enzyme activities of glutathione reductase from human erythrocytes in vitro and from rat erythrocytes in vivo, Eur. J. Pharmacol
Mousavi, Heydari, Mehravaran, Melatonin effects on sleep quality and outcomes of COVID-19 patients: An open-label, randomized, controlled trial, J. Med. Virol
Muxel, Pires-Lapa, Monteiro, NF-κB drives the synthesis of melatonin in RAW 264.7 macrophages by inducing the transcription of the arylalkylamine-Nacetyltransferase (AA-NAT) gene, PLoS One
Muñoz, Palomo, Jerez-Calero, Use of an ANN to value MTF and melatonin effect on ADHD affected children, IEEE Access
Muñoz-Hoyos, Sánchez-Forte, Molina-Carballo, Melatonin's role as an anticonvulsant and neuronal protector: experimental and clinical evidence, J. Child. Neurol
Nair, Perioperative melatonin in COVID-19 patients: benefits beyond sedation and analgesia, Med. Gas Res
Naveenkumar, Hemshekhar, Jagadish, Melatonin restores neutrophil functions and prevents apoptosis amid dysfunctional glutathione redox system, J. Pineal Res
Nunes Oda, Rde, Regression of herpes viral infection symptoms using melatonin and SB-73: comparison with Acyclovir, J. Pineal Res
Okatani, Wakatsuki, Shinohara, Melatonin stimulates glutathione peroxidase activity in human chorion, J. Res. Med. Sci
Olsen, Fosbøl, Lindhardsen, Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: a nationwide cohort study, Circulation
Otmani, Demazières, Staner, Effects of prolonged-release melatonin, zolpidem, and their combination on psychomotor functions, memory recall, and driving skills in healthy middle aged and elderly volunteers, Hum. Psychopharmacol
Ozturk, Coşkun, Erbaş, The effect of melatonin on liver superoxide dismutase activity, serum nitrate and thyroid hormone levels, Jpn. J. Physiol
Parlakpinar, Polat, Acet, Pharmacological agents under investigation in the treatment of coronavirus disease 2019 and the importance of melatonin, Fundam. Clin. Pharmacol
Pedrosa, Weinlich, Mognol, Melatonin protects CD4+ T cells from activation-induced cell death by blocking NFAT-mediated CD95 ligand upregulation, J. Immunol
Pierrefiche, Laborit, Oxygen free radicals, melatonin, and aging, Exp. Gerontol
Porta, A dictionary of epidemiology
Purushothaman, Sheeja, Janardanan, Hydroxyl radical scavenging activity of melatonin and its related indolamines, Free Radic. Res
Ramlall, Zucker, Tatonetti, Melatonin is significantly associated with survival of intubated COVID-19 patients, medRxiv
Ramos, Farré-Alins, Egea, Melatonin's efficacy in stroke patients; a matter of dose? A systematic review, Toxicol. Appl. Pharmacol
Ramos, Míguez, Morgado, Melatonin enhances responsiveness to Dichelobacter nodosus vaccine in sheep and increases peripheral blood CD4 T lymphocytes and IgG-expressing B lymphocytes, Vet. Immunol. Immunopathol
Regodón, Martín-Palomino, Fernández-Montesinos, The use of melatonin as a vaccine agent, Vaccine
Regodón, Ramos, Morgado, Melatonin enhances the immune response to vaccination against A1 and C strains of Dichelobacter nodosus, Vaccine
Regodón, Ramos, Míguez, Vaccination prepartum enhances the beneficial effects of melatonin on the immune response and reduces platelet responsiveness in sheep, BMC Vet. Res
Reina, Martínez, A new free radical scavenging cascade involving melatonin and three of its metabolites (3OHM, AFMK and AMK), Computational Theoretical Chem
Reiter, Abreu-Gonzalez, Marik, Therapeutic algorithm for use of melatonin in patients with COVID-19, Front. Med
Reiter, Aging and oxygen toxicity: Relation to changes in melatonin, Age (Omaha)
Reiter, Pineal melatonin: cell biology of its synthesis and of its physiological interactions, Endocr. Rev
Reiter, Rosales-Corral, Tan, Melatonin as a mitochondria-targeted antioxidant: one of evolution's best ideas, Cell Mol. Life Sci
Reiter, Sharma, Ma, Plasticity of glucose metabolism in activated immune cells: advantages for melatonin inhibition of COVID-19 disease, Melatonin Res
Reiter, Tan, Sainz, Melatonin: reducing the toxicity and increasing the efficacy of drugs, J. Pharm. Pharmacol
Reiter, Tang, Garcia, Pharmacological actions of melatonin in oxygen radical pathophysiology, Life Sci
Ren, Sun, Li, Exogenous melatonin inhibits neutrophil migration through suppression of ERK activation, J. Endocrinol
Rodríguez-Rubio, Figueira, Acuña-Castroviejo, A phase II, single-center, double-blind, randomized placebo-controlled trial to explore the efficacy and safety of intravenous melatonin in patients with COVID-19 admitted to the intensive care unit (MelCOVID study): a structured summary of a study protocol for a randomized controlled trial, Trials
Rubins, Alveolar macrophages: wielding the double-edged sword of inflammation, Am. J. Respir. Crit. Care Med
Schagat, Wofford, Wright, Surfactant protein A enhances alveolar macrophage phagocytosis of apoptotic neutrophils, J. Immunol
Seabra, Bignotto, Pinto, Randomized, double-blind clinical trial, controlled with placebo, of the toxicology of chronic melatonin treatment, J. Pineal Res
Sehirli, Sayiner, Serakinci, Role of melatonin in the treatment of COVID-19; as an adjuvant through cluster differentiation 147 (CD147), Mol. Biol. Rep
Shafiei, Bahtoei, Effects of N-acetyl cysteine and melatonin on early reperfusion injury in patients undergoing coronary artery bypass grafting: A randomized, open-labeled, placebo-controlled trial, Medicine (Baltimore)
Shang, Xu, Wu, Melatonin reduces acute lung injury in endotoxemic rats, Chin. Med. J. (Engl)
Shchetinin, Baturin, Arushanyan, Potential and possible therapeutic effects of melatonin on SARS-CoV-2 infection, Antioxidants (Basel)
Shiu, Reiter, Tan, Urgent search for safe and effective treatments of severe acute respiratory syndrome: is melatonin a promising candidate drug?, J. Pineal Res
Sileri, Sica, Gentileschi, Melatonin reduces bacterial translocation after intestinal ischemia-reperfusion injury, Transplant. Proc
Slominski, Tobin, Zmijewski, Melatonin in the skin: synthesis, metabolism and functions, Trends Endocrinol. Metab
Sun, Lee, Kao, Systemic combined melatonin-mitochondria treatment improves acute respiratory distress syndrome in the rat, J. Pineal Res
Suwanjang, Abramov, Charngkaew, Melatonin prevents cytosolic calcium overload, mitochondrial damage and cell death due to toxically high doses of dexamethasone-induced oxidative stress in human neuroblastoma SH-SY5Y cells, Neurochem. Int
Sygitowicz, Sitkiewicz, Molecular mechanisms of organ damage in sepsis: an overview, Braz J. Infect. Dis
Sánchez-Barceló, Mediavilla, Tan, Clinical uses of melatonin: evaluation of human trials, Curr. Med. Chem
Sánchez-González, Mahíllo-Fernández, Villar-Álvarez, What if melatonin could help patients with severe COVID-19?, J. Clin. Sleep Med
Sánchez-López, Ortiz, Pacheco-Moises, Efficacy of melatonin on serum pro-inflammatory cytokines and oxidative stress markers in relapsing remitting multiple sclerosis, Arch. Med. Res
Tan, Manchester, Reiter, Identification of highly elevated levels of melatonin in bone marrow: its origin and significance, Biochim. Biophys. Acta
Tan, Reiter, Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality, Life Sci
Tate, Ong, Dowling, Reassessing the role of the NLRP3 inflammasome during pathogenic influenza A virus infection via temporal inhibition, Sci. Rep
Touitou, Reinberg, Touitou, Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: Health impacts and mechanisms of circadian disruption, Life Sci
Uberos, Mc, Carballo, Normalization of the sleepwake pattern and melatonin and 6-sulphatoxy-melatonin levels after a therapeutic trial with melatonin in children with severe epilepsy, J. Pineal Res
Ursing, Bahr, Brismar, Influence of cigarette smoking on melatonin levels in man, Eur. J. Clin. Pharmacol
Wang, Yang, Zhang, Melatonin as immune potentiator for enhancing subunit vaccine efficacy against bovine viral diarrhea virus, Vaccines
Woo, Jeong, Chung, Development and functions of alveolar macrophages, Mol. Cells
Wu, Ji, Wang, Melatonin alleviates radiation-induced lung injury via regulation of miR-30e/NLRP3 axis, Oxid. Med. Cell Longev
Wu, Xie, Zhao, Melatonin biosynthesis restored by CpG oligodeoxynucleotides attenuates allergic airway inflammation via regulating NLRP3 inflammasome, Life Sci
Xia, Yang, Li, Melatonin alleviates Ochratoxin A-induced liver inflammation involved intestinal microbiota homeostasis and microbiota-independent manner, J. Hazard. Mater
Xu, Wang, Melatonin suppresses TLR9-triggered proinflammatory cytokine production in macrophages by inhibiting ERK1/2 and AKT activation, Sci. Rep
Yang, Chen, Yiang, Targeting host defense system and rescuing compromised mitochondria to increase tolerance against pathogens by melatonin may impact outcome of deadly virus infection pertinent to COVID-19, Int. J. Mol. Sci
Yeum, Russell, Krinsky, Biomarkers of antioxidant capacity in the hydrophilic and lipophilic compartments of human plasma, Arch. Biochem. Biophys
Zarezadeh, Khorshidi, Emami, Melatonin supplementation and proinflammatory mediators: a systematic review and meta-analysis of clinical trials, Eur. J. Nutr
Zhang, Li, Grailer, Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome, J. Pineal Res
Zhang, Wang, Ni, COVID-19: Melatonin as a potential adjuvant treatment, Life Sci
Zhao, Lu, Li, The protective effect of melatonin on brain ischemia and reperfusion in rats and humans: In vivo assessment and a randomized controlled trial, J. Pineal Res
Zhao, Yu, Shen, Melatonin synthesis and function: evolutionary history in animals and plants, Front. Endocrinol
Ziaadini, Aminae, Rastegar, Melatonin supplementation decreases aerobic exercise training induced-lipid peroxidation and malondialdehyde in sedentary young women, Polish J. Food Nutr. Sci
Ziaei, Davoodian, Dadvand, Evaluation of the efficacy and safety of Melatonin in moderately ill patients with COVID-19: A structured summary of a study protocol for a randomized controlled trial, Trials
DOI record:
{
"DOI": "10.32794/mr112500159",
"ISSN": [
"2641-0281"
],
"URL": "http://dx.doi.org/10.32794/mr112500159",
"abstract": "<jats:p>This study has investigated the protective role of melatonin against SARS-CoV-2 infection. For this purpose, 62 adults were recruited who were in daily relatively high doses of melatonin intaking, with the particularity that they started taking it before the beginning of the COVID-19 pandemic and continued to present. A continuous validation process has been carried out with a series of questionnaires to identify the risk factors, whether they were contacts, were infected, if yes, the level of disease severity, need for treatment, hospitalization, etc. According to the dose of melatonin the individuals took/are taking, they were divided into two groups: a) those taking 20 mg (n = 27) and, b) those taking ≥ 40 mg (n = 32). For statistical analysis, the shi2 test and Fisher&#39;s exact test were used. The number of infected subjects with positive PCR was 7 (11.9%). Only one required medication, the rest had a very favorable clinical evolution, mild in three cases and asymptomatic in three others. While in their environment this percentage is 22.05% (chi2 = 2.928; p < 0.087). Melatonin offers a good safety profile, is well tolerated and can play an important role in the different levels of COVID-19 prevention.</jats:p>",
"author": [
{
"affiliation": [],
"family": "Molina-Carballo",
"given": "Antonio",
"sequence": "first"
},
{
"affiliation": [],
"family": "Jerez-Calero",
"given": "Antonio Emilio",
"sequence": "first"
},
{
"affiliation": [],
"family": "Fernández-López",
"given": "Luisa",
"sequence": "first"
},
{
"affiliation": [],
"family": "Augustin-Morales",
"given": "María del Carmen",
"sequence": "first"
},
{
"affiliation": [],
"family": "Muñoz-Hoyos",
"given": "Antonio",
"sequence": "first"
},
{
"affiliation": [],
"family": "Agil",
"given": "Ahmad",
"sequence": "first"
}
],
"container-title": "Melatonin Research",
"container-title-short": "Melatonin Res.",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
9,
29
]
],
"date-time": "2023-09-29T15:58:59Z",
"timestamp": 1696003139000
},
"deposited": {
"date-parts": [
[
2023,
9,
29
]
],
"date-time": "2023-09-29T15:59:01Z",
"timestamp": 1696003141000
},
"indexed": {
"date-parts": [
[
2023,
9,
30
]
],
"date-time": "2023-09-30T16:44:10Z",
"timestamp": 1696092250070
},
"is-referenced-by-count": 0,
"issue": "3",
"issued": {
"date-parts": [
[
2023,
9,
30
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2023,
9,
29
]
]
}
},
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
30
]
],
"date-time": "2023-09-30T00:00:00Z",
"timestamp": 1696032000000
}
}
],
"member": "18079",
"original-title": [],
"page": "372-396",
"prefix": "10.32794",
"published": {
"date-parts": [
[
2023,
9,
30
]
]
},
"published-online": {
"date-parts": [
[
2023,
9,
30
]
]
},
"publisher": "ST Bio-life",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.melatonin-research.net/index.php/MR/article/view/236"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "The preventive and protective role of melatonin in SARS-CoV-2 infection: a retrospective study",
"type": "journal-article",
"volume": "6"
}