The Association between COVID-19 Infection and Gabrin Sign: A Case-Control Study
et al., Indian Dermatology Online Journal, doi:10.4103/idoj.idoj_222_23, Feb 2024
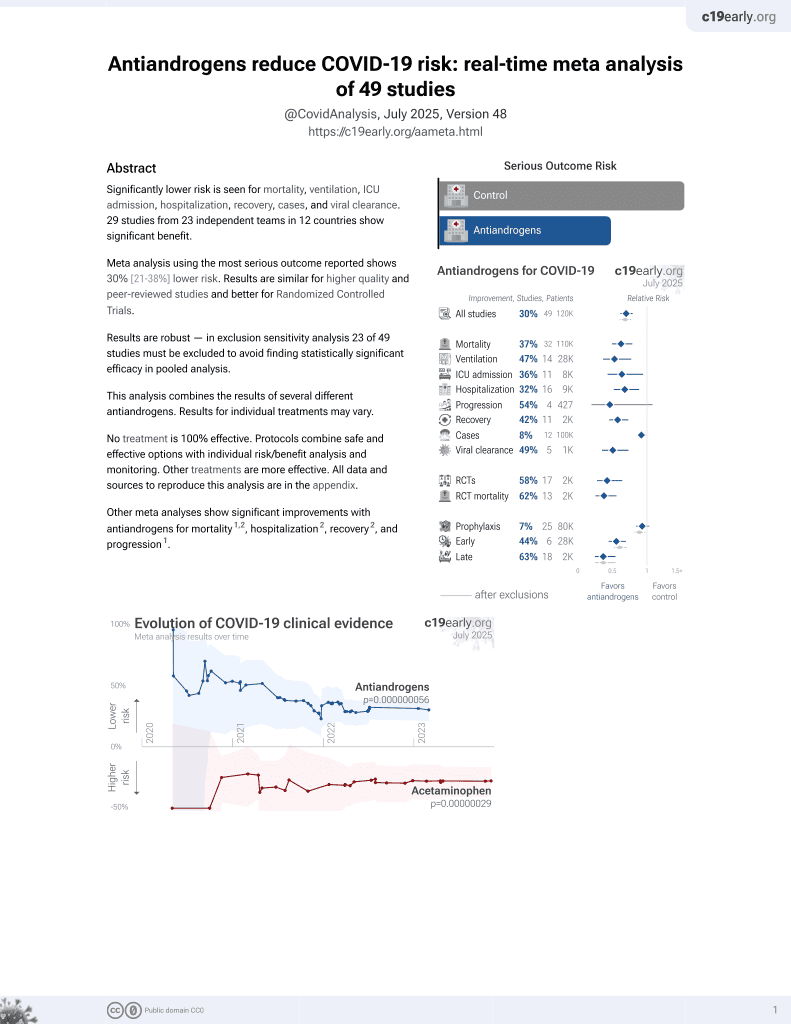
7th treatment shown to reduce risk in
September 2020, now with p = 0.000000056 from 49 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
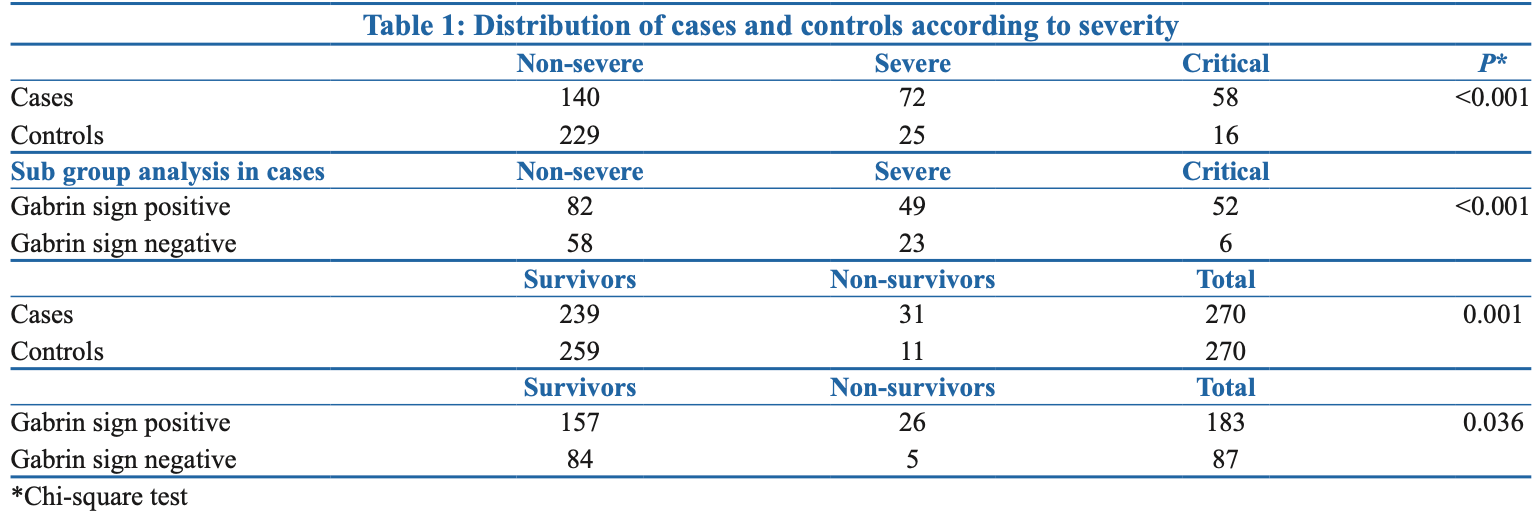
Retrospective case-control study of 540 COVID-19 patients hospitalized in India, showing higher COVID-19 severity and mortality among those with androgenetic alopecia. Cases were further divided into those with more severe alopecia (Gabrin sign positive) and less severe alopecia (Gabrin sign negative). More cases had severe/critical COVID-19 than controls (p<0.001) and Gabrin sign positive cases had higher severity than Gabrin sign negative (p<0.001). Mortality was 11.4% for cases vs 4.2% for controls (p=0.001) and higher for Gabrin sign positive vs negative cases (14.2% vs 5.7%, p=0.036). The results suggest a possible role of androgens in COVID-19 severity, supporting potential benefits of anti-androgen therapy.
Mohta et al., 13 Feb 2024, peer-reviewed, 4 authors.
Abstract: Letter to the Editor
The Association between COVID‑19 Infection and Gabrin Sign:
A Case‑Control Study
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8K2+Ya6H515kE= on 02/20/2024
Dear Editor,
The COVID‑19 pandemic has claimed countless lives,
including that of Dr. Frank Gabrin, who battled bilateral
testicular cancer and androgenetic alopecia before
succumbing to the virus. In his memory, Wambier et al.
conducted a study highlighting a novel symptom of
COVID‑19: the Gabrin sign.[1]
Recent research has shown that the SARS‑CoV‑2 virus
primarily infects type II pneumocytes through binding with
their angiotensin converting enzyme (ACE)-2 receptors,
which is facilitated by the proteolytic priming of viral
spike proteins by TMPRSS2. Studies of SARS‑CoV‑1 have
suggested that inhibiting serine proteases can decrease
the likelihood of virus attachment to ACE‑2 receptors.
Furthermore, TMPRSS2 gene transcription is regulated by
androgenic promoters.[2]
Studies show that COVID‑19 patients have a higher
incidence of androgenetic alopecia (AGA), making it
critical to investigate AGA in both male and female patients
as a potential risk factor.[3,4]
The aim of this prospective case‑control study was to
explore the potential correlation between COVID‑19
severity and androgenic alopecia in hospitalized male and
female patients.
We conducted this case‑control study at our tertiary
care centre between March 2021 and August
2021, with institutional ethical committee approval
(F/SPMC/IERB/0904) and informed consent from
participants. Hospitalized males and females with
COVID‑19 infection requiring oxygen support were
included, and the virus was detected using real‑time reverse
transcription‑polymerase chain reaction (RT‑qPCR) and
COVID‑19 rapid antigen test (RAT).
Cases included subjects with androgenic alopecia. This group
was further divided into ‘positive Gabrin sign’ including
Hamilton–Norwood scale (HNS) graded from 3 to 7 for men
and Ludwig scale (LS) grade from 2 to 3 for women; and
‘negative Gabrin sign’ including HNS 1‑2 and LS‑1.
Controls were recruited for this case‑control study by
selecting individuals without androgenic alopecia who had
been diagnosed with lab‑proven COVID‑19 from the same
ward as the cases. Controls were also matched to cases on
important variables that may affect the risk of COVID‑19
severity, such as age, gender, ethnicity, and comorbidities.
Matching controls to cases helped to reduce the effects of
confounding variables that may have impacted the study
results.
In our study, patients were categorized into three groups
according to type of oxygen assistance required, namely
those who needed simple oxygen masks (non‑severe),
those who required high‑flow devices such as
continuous positive airway pressure or high‑flow nasal
cannulas (severe), and those who needed mechanical
ventilation (critical). The outcomes were: survivor and
non‑survivor.
To further assess the effect of androgens on infection’s
severity, for males, we noted the presence or absence of
any prostate disease or history of consuming antiandrogens,
while for females, we recorded the history of hormone
replacement therapy and signs of hyperandrogenism, such
as polycystic ovarian disease and virilization.
The sample size calculation assumed a prevalence of 50%
and an odds ratio of 1.7 according to previous studies,
a power of 80%, and a significance level of..