Predictors of incident viral symptoms ascertained in the era of COVID-19
et al., PLOS ONE, doi:10.1371/journal.pone.0253120, Jun 2021
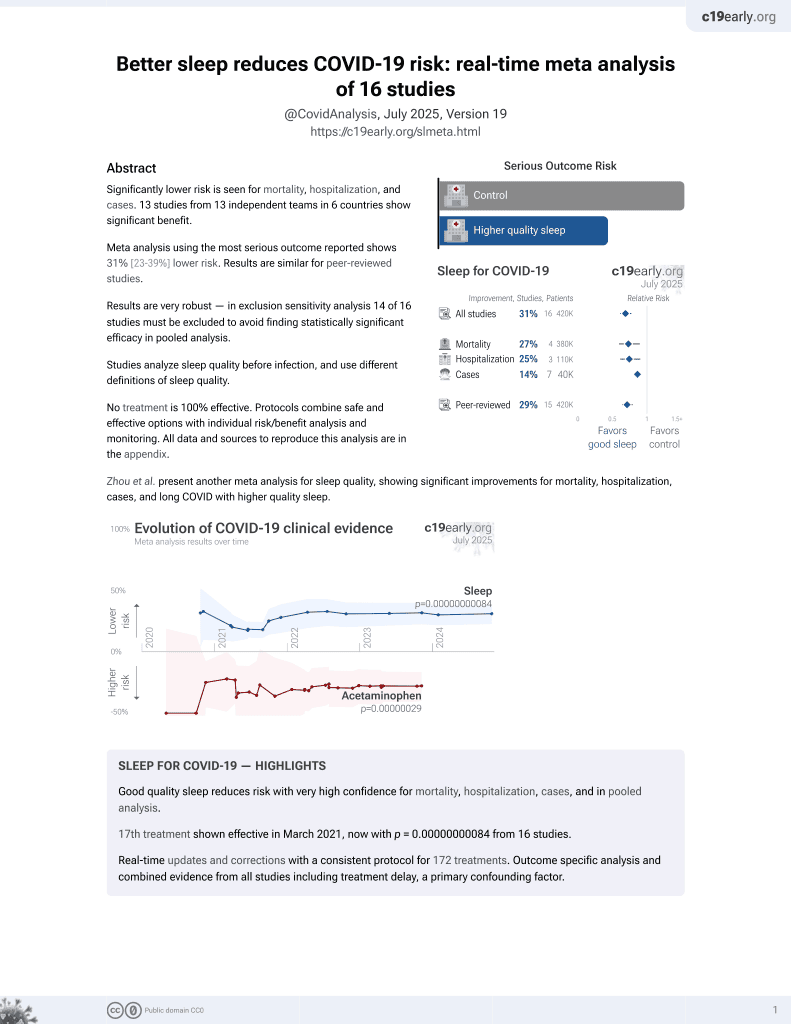
Sleep for COVID-19
18th treatment shown to reduce risk in
March 2021, now with p = 0.00000000084 from 16 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective survey based study with 14,335 participants, showing risk of viral symptoms associated with shorter sleep duration.
Study covers sleep and exercise.
|
risk of symptomatic case, 16.0% lower, OR 0.84, p < 0.001, adjusted per study, per extra hour sleep, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Marcus et al., 17 Jun 2021, prospective, multiple countries, peer-reviewed, survey, 12 authors, study period 26 March, 2020 - 3 May, 2020.
Predictors of incident viral symptoms ascertained in the era of COVID-19
PLOS ONE, doi:10.1371/journal.pone.0253120
Background In the absence of universal testing, effective therapies, or vaccines, identifying risk factors for viral infection, particularly readily modifiable exposures and behaviors, is required to identify effective strategies against viral infection and transmission.
Methods We conducted a world-wide mobile application-based prospective cohort study available to English speaking adults with a smartphone. We collected self-reported characteristics, exposures, and behaviors, as well as smartphone-based geolocation data. Our main outcome was incident symptoms of viral infection, defined as fevers and chills plus one other symptom previously shown to occur with SARS-CoV-2 infection, determined by daily surveys.
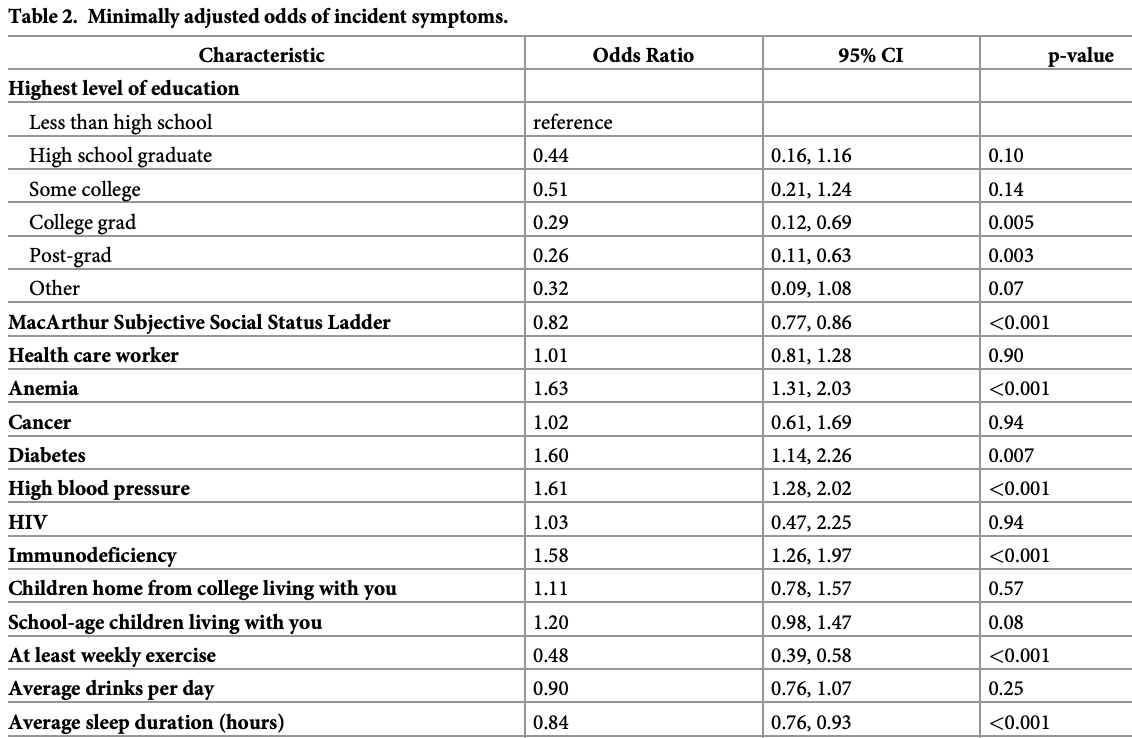
Findings Among 14, 335 participants residing in all 50 US states and 93 different countries followed for a median 21 days (IQR 10-26 days), 424 (3%) developed incident viral symptoms. In pooled multivariable logistic regression models, female biological sex (odds ratio [OR] 1.75, 95% CI 1.39-2.20, p<0.001), anemia (OR 1.45, 95% CI 1.16-1.81, p = 0.001), hypertension (OR 1.35, 95% CI 1.08-1.68, p = 0.007), cigarette smoking in the last 30 days (OR 1.86, p<0.001), any viral symptoms among household members 6-12 days prior (OR 2.06, 95% CI 1.67-2.55, p<0.001), and the maximum number of individuals the participant interacted with within 6 feet in the past 6-12 days (OR 1.15, 95% CI 1.06-1.25, p<0.001) were each associated with a higher risk of developing viral symptoms. Conversely, a higher subjective social status (OR 0.87, 95% CI 0.83-0.93, p<0.001), at least weekly exercise (OR 0.57, 95% CI 0.47-0.70, p<0.001), and sanitizing one's phone (OR 0.79, 95% CI 0.63-0.99, p = 0.037) were each associated with a lower risk of developing viral symptoms.
Supporting information
S1 Table. Proportion of participants completing at least one daily survey per week and the proportion completing weekly surveys. (DOCX)
S2
References
Adorni, Prinelli, Bianchi, Self-reported symptoms of SARS-CoV-2 infection in a non-hospitalized population: results from the large Italian web-based EPICOVID19 cross-sectional survey, JMIR Public Health Surveill
Alene, Yismaw, Assemie, Ketema, Gietaneh et al., Serial interval and incubation period of COVID-19: a systematic review and meta-analysis, BMC Infect Dis, doi:10.1186/s12879-021-05950-x
Bastiani, Fortunato, Pieroni, Rapid COVID-19 Screening Based on Self-Reported Symptoms: Psychometric Assessment and Validation of the EPICOVID19 Short Diagnostic Scale, J Med Internet Res, doi:10.2196/23897
Benjamin, Blaha, Chiuve, Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association, Circulation, doi:10.1161/CIR.0000000000000485
Bhatraju, Ghassemieh, Nichols, COVID-19 in Critically Ill Patients in the Seattle Region -Case Series, N Engl J Med, doi:10.1056/NEJMoa2004500
Burton, Fort, Seoane, Hospitalization and Mortality among Black Patients and White Patients with COVID-19, N Engl J Med, doi:10.1056/NEJMsa2011686
Cai, Sex difference and smoking predisposition in patients with COVID-19, The Lancet Respiratory medicine, doi:10.1016/S2213-2600%2820%2930117-X
Castro Gertrudes, Zimek, Sander, Campello, A unified view of density-based methods for semisupervised clustering and classification, Data Min Knowl Discov, doi:10.1007/s10618-019-00651-1
Cooper, Milic, Mills, Bardwell, Ziegler et al., Endothelial function: the impact of objective and subjective socioeconomic status on flow-mediated dilation, Ann Behav Med, doi:10.1007/s12160-010-9181-9
Dawson, Rabold, Laws, Loss of Taste and Smell as Distinguishing Symptoms of COVID-19, Clin Infect Dis
Farsalinos, Barbouni, Poulas, Polosa, Caponnetto et al., Current smoking, former smoking, and adverse outcome among hospitalized COVID-19 patients: a systematic review and meta-analysis, Ther Adv Chronic Dis, doi:10.1177/2040622320935765
Gangaputra, Patel, Ocular Symptoms among Nonhospitalized Patients Who Underwent COVID-19 Testing, Ophthalmology, doi:10.1016/j.ophtha.2020.06.037
Gold, Sehayek, Gabrielli, Zhang, Mccusker et al., COVID-19 and comorbidities: a systematic review and meta-analysis, Postgrad Med, doi:10.1080/00325481.2020.1786964
Goodman, Adler, Kawachi, Frazier, Huang et al., Adolescents' perceptions of social status: development and evaluation of a new indicator, Pediatrics, doi:10.1542/peds.108.2.e31
Goyal, Choi, Pinheiro, Clinical Characteristics of COVID-19 in New York City, N Engl J Med, doi:10.1056/NEJMc2010419
Grant, Geoghegan, Arbyn, The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries, PLoS One, doi:10.1371/journal.pone.0234765
Haddad, Malhab, Sacre, Salameh, Smoking and COVID-19: A Scoping Review, Tob Use Insights, doi:10.1177/1179173X21994612
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736%2820%2930183-5
Islam, Sharp, Chowell, Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries, BMJ, doi:10.1136/bmj.m2743
Juster, Sindi, Marin, A clinical allostatic load index is associated with burnout symptoms and hypocortisolemic profiles in healthy workers, Psychoneuroendocrinology, doi:10.1016/j.psyneuen.2010.11.001
Kutter, Spronken, Fraaij, Fouchier, Herfst, Transmission routes of respiratory viruses among humans, Curr Opin Virol, doi:10.1016/j.coviro.2018.01.001
Lan, Filler, Mathew, COVID-19 symptoms predictive of healthcare workers' SARS-CoV-2 PCR results, PLoS One, doi:10.1371/journal.pone.0235460
Lan, Filler, Mathew, Evolving virulence? Decreasing COVID-19 complications among Massachusetts healthcare workers: a cohort study, Pathog Glob Health, doi:10.1080/20477724.2020.1847778
Lessler, Brookmeyer, Reich, Nelson, Cummings et al., Identifying the probable timing and setting of respiratory virus infections, Infect Control Hosp Epidemiol, doi:10.1086/655023
Liu, Blet, Smyth, Li, The Science Underlying COVID-19: Implications for the Cardiovascular System, Circulation, doi:10.1161/CIRCULATIONAHA.120.047549
Liu, Cui, Yang, Yao, Correlation between gastrointestinal symptoms and disease severity in patients with COVID-19: a systematic review and meta-analysis, BMJ Open Gastroenterol, doi:10.1136/bmjgast-2020-000437
Martı ´n-Sa ´nchez, Toro, Cardassay, Clinical presentation and outcome across age categories among patients with COVID-19 admitted to a Spanish Emergency Department, Eur Geriatr Med, doi:10.1007/s41999-020-00359-2
Mcanulty, Ward, Suppressing the Epidemic in New South Wales, N Engl J Med, doi:10.1056/NEJMc2011592
Melvin, Godwin, Berenhaut, Salsbury, Visualizing correlated motion with HDBSCAN clustering, Protein Sci, doi:10.1002/pro.3268
Menachemi, Yiannoutsos, Dixon, Population Point Prevalence of SARS-CoV-2 Infection Based on a Statewide Random Sample-Indiana, April 25, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6929e1
Menni, Valdes, Freidin, Real-time tracking of self-reported symptoms to predict potential COVID-19, Nat Med, doi:10.1038/s41591-020-0916-2
Pagani, Conti, Giacomelli, Seroprevalence of SARS-CoV-2 significantly varies with age: Preliminary results from a mass population screening, J Infect, doi:10.1016/j.jinf.2020.09.021
Peckham, De Gruijter, Raine, Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission, Nat Commun, doi:10.1038/s41467-020-19741-6
Pollan, Perez-Gomez, Pastor-Barriuso, Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study, Lancet, doi:10.1016/S0140-6736%2820%2931483-5
Richardson, Hirsch, Narasimhan, Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area, JAMA
Rouse, Sehrawat, Immunity and immunopathology to viruses: what decides the outcome?, Nat Rev Immunol, doi:10.1038/nri2802
Scalinci, Battagliola, Conjunctivitis can be the only presenting sign and symptom of COVID-19, IDCases, doi:10.1016/j.idcr.2020.e00774
Silverman, Hupert, Washburne, Using influenza surveillance networks to estimate state-specific prevalence of SARS-CoV-2 in the United States, Sci Transl Med, doi:10.1126/scitranslmed.abc1126
Simpson, Kunz, Agha, Graff, Exercise and the Regulation of Immune Functions, Prog Mol Biol Transl Sci, doi:10.1016/bs.pmbts.2015.08.001
Tostmann, Bradley, Bousema, Strong associations and moderate predictive value of early symptoms for SARS-CoV-2 test positivity among healthcare workers, the Netherlands, Euro Surveill, doi:10.2807/1560-7917.ES.2020.25.16.2000508
Tromberg, Schwetz, ´rez-Stable, Rapid Scaling Up of COVID-19 Diagnostic Testing in the United States-The NIH RADx Initiative, N Engl J Med, doi:10.1056/NEJMsr2022263
Wang, Li, Liu, An overview of the safety, clinical application and antiviral research of the COVID-19 therapeutics, J Infect Public Health
Wang, Pan, Tang, Ji, Shi, Mask use during COVID-19: A risk adjusted strategy, Environ Pollut, doi:10.1016/j.envpol.2020.115099
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Williamson, Walker, Bhaskaran, OpenSAFELY: factors associated with COVID-19 death in 17 million patients, Nature
Wynants, Van Calster, Collins, Prediction models for diagnosis and prognosis of covid-19 infection: systematic review and critical appraisal, BMJ, doi:10.1136/bmj.m1328
DOI record:
{
"DOI": "10.1371/journal.pone.0253120",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0253120",
"abstract": "<jats:sec id=\"sec001\">\n<jats:title>Background</jats:title>\n<jats:p>In the absence of universal testing, effective therapies, or vaccines, identifying risk factors for viral infection, particularly readily modifiable exposures and behaviors, is required to identify effective strategies against viral infection and transmission.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec002\">\n<jats:title>Methods</jats:title>\n<jats:p>We conducted a world-wide mobile application-based prospective cohort study available to English speaking adults with a smartphone. We collected self-reported characteristics, exposures, and behaviors, as well as smartphone-based geolocation data. Our main outcome was incident symptoms of viral infection, defined as fevers and chills plus one other symptom previously shown to occur with SARS-CoV-2 infection, determined by daily surveys.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec003\">\n<jats:title>Findings</jats:title>\n<jats:p>Among 14, 335 participants residing in all 50 US states and 93 different countries followed for a median 21 days (IQR 10–26 days), 424 (3%) developed incident viral symptoms. In pooled multivariable logistic regression models, female biological sex (odds ratio [OR] 1.75, 95% CI 1.39–2.20, p<0.001), anemia (OR 1.45, 95% CI 1.16–1.81, p = 0.001), hypertension (OR 1.35, 95% CI 1.08–1.68, p = 0.007), cigarette smoking in the last 30 days (OR 1.86, 95% CI 1.35–2.55, p<0.001), any viral symptoms among household members 6–12 days prior (OR 2.06, 95% CI 1.67–2.55, p<0.001), and the maximum number of individuals the participant interacted with within 6 feet in the past 6–12 days (OR 1.15, 95% CI 1.06–1.25, p<0.001) were each associated with a higher risk of developing viral symptoms. Conversely, a higher subjective social status (OR 0.87, 95% CI 0.83–0.93, p<0.001), at least weekly exercise (OR 0.57, 95% CI 0.47–0.70, p<0.001), and sanitizing one’s phone (OR 0.79, 95% CI 0.63–0.99, p = 0.037) were each associated with a lower risk of developing viral symptoms.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec004\">\n<jats:title>Interpretation</jats:title>\n<jats:p>While several immutable characteristics were associated with the risk of developing viral symptoms, multiple immediately modifiable exposures and habits that influence risk were also observed, potentially identifying readily accessible strategies to mitigate risk in the COVID-19 era.</jats:p>\n</jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5197-7696",
"affiliation": [],
"authenticated-orcid": true,
"family": "Marcus",
"given": "Gregory M.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Olgin",
"given": "Jeffrey E.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Peyser",
"given": "Noah D.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8535-0920",
"affiliation": [],
"authenticated-orcid": true,
"family": "Vittinghoff",
"given": "Eric",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yang",
"given": "Vivian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Joyce",
"given": "Sean",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8490-0270",
"affiliation": [],
"authenticated-orcid": true,
"family": "Avram",
"given": "Robert",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tison",
"given": "Geoffrey H.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1986-2164",
"affiliation": [],
"authenticated-orcid": true,
"family": "Wen",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Butcher",
"given": "Xochitl",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Eitel",
"given": "Helena",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pletcher",
"given": "Mark J.",
"sequence": "additional"
}
],
"container-title": [
"PLOS ONE"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2021,
6,
17
]
],
"date-time": "2021-06-17T17:37:24Z",
"timestamp": 1623951444000
},
"deposited": {
"date-parts": [
[
2021,
6,
17
]
],
"date-time": "2021-06-17T17:37:59Z",
"timestamp": 1623951479000
},
"editor": [
{
"affiliation": [],
"family": "Palazón-Bru",
"given": "Antonio",
"sequence": "first"
}
],
"funder": [
{
"DOI": "10.13039/100000070",
"award": [
"IU2CEB021881-01"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Biomedical Imaging and Bioengineering"
},
{
"DOI": "10.13039/100000070",
"award": [
"IU2CEB021881-01"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Biomedical Imaging and Bioengineering"
},
{
"DOI": "10.13039/100000070",
"award": [
"IU2CEB021881-01"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Biomedical Imaging and Bioengineering"
},
{
"DOI": "10.13039/100000070",
"award": [
"3U2CEB021881-05S1"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Biomedical Imaging and Bioengineering"
},
{
"DOI": "10.13039/100000070",
"award": [
"3U2CEB021881-05S1"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Biomedical Imaging and Bioengineering"
},
{
"DOI": "10.13039/100000070",
"award": [
"3U2CEB021881-05S1"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Biomedical Imaging and Bioengineering"
}
],
"indexed": {
"date-parts": [
[
2022,
4,
4
]
],
"date-time": "2022-04-04T17:21:59Z",
"timestamp": 1649092919717
},
"is-referenced-by-count": 1,
"issn-type": [
{
"type": "electronic",
"value": "1932-6203"
}
],
"issue": "6",
"issued": {
"date-parts": [
[
2021,
6,
17
]
]
},
"journal-issue": {
"issue": "6",
"published-online": {
"date-parts": [
[
2021,
6,
17
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
17
]
],
"date-time": "2021-06-17T00:00:00Z",
"timestamp": 1623888000000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0253120",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0253120",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2021,
6,
17
]
]
},
"published-online": {
"date-parts": [
[
2021,
6,
17
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"DOI": "10.1056/NEJMc2011592",
"article-title": "Suppressing the Epidemic in New South Wales",
"author": "JM McAnulty",
"doi-asserted-by": "crossref",
"first-page": "e74",
"journal-title": "N Engl J Med",
"key": "pone.0253120.ref001",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/j.envpol.2020.115099",
"article-title": "Mask use during COVID-19: A risk adjusted strategy",
"author": "J Wang",
"doi-asserted-by": "crossref",
"first-page": "115099",
"journal-title": "Environ Pollut",
"key": "pone.0253120.ref002",
"volume": "266",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m2743",
"article-title": "Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries",
"author": "N Islam",
"doi-asserted-by": "crossref",
"first-page": "m2743",
"journal-title": "BMJ",
"key": "pone.0253120.ref003",
"volume": "370",
"year": "2020"
},
{
"DOI": "10.1056/NEJMsa2011686",
"article-title": "Hospitalization and Mortality among Black Patients and White Patients with COVID-19",
"author": "EG Price-Haywood",
"doi-asserted-by": "crossref",
"first-page": "2534",
"journal-title": "N Engl J Med",
"key": "pone.0253120.ref004",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2010419",
"article-title": "Clinical Characteristics of COVID-19 in New York City",
"author": "P Goyal",
"doi-asserted-by": "crossref",
"first-page": "2372",
"journal-title": "N Engl J Med",
"key": "pone.0253120.ref005",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2004500",
"article-title": "COVID-19 in Critically Ill Patients in the Seattle Region—Case Series",
"author": "PK Bhatraju",
"doi-asserted-by": "crossref",
"first-page": "2012",
"journal-title": "N Engl J Med",
"key": "pone.0253120.ref006",
"volume": "382",
"year": "2020"
},
{
"article-title": "Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area",
"author": "S Richardson",
"journal-title": "JAMA",
"key": "pone.0253120.ref007",
"year": "2020"
},
{
"article-title": "OpenSAFELY: factors associated with COVID-19 death in 17 million patients",
"author": "EJ Williamson",
"journal-title": "Nature",
"key": "pone.0253120.ref008",
"year": "2020"
},
{
"article-title": "Using influenza surveillance networks to estimate state-specific prevalence of SARS-CoV-2 in the United States",
"author": "JD Silverman",
"journal-title": "Sci Transl Med",
"key": "pone.0253120.ref009",
"year": "2020"
},
{
"article-title": "Clinical presentation and outcome across age categories among patients with COVID-19 admitted to a Spanish Emergency Department",
"author": "FJ Martín-Sánchez",
"journal-title": "Eur Geriatr Med",
"key": "pone.0253120.ref010",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "C Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "pone.0253120.ref011",
"volume": "395",
"year": "2020"
},
{
"article-title": "Correlation between gastrointestinal symptoms and disease severity in patients with COVID-19: a systematic review and meta-analysis",
"author": "J Liu",
"journal-title": "BMJ Open Gastroenterol",
"key": "pone.0253120.ref012",
"volume": "7",
"year": "2020"
},
{
"article-title": "Self-reported symptoms of SARS-CoV-2 infection in a non-hospitalized population: results from the large Italian web-based EPICOVID19 cross-sectional survey",
"author": "F Adorni",
"journal-title": "JMIR Public Health Surveill",
"key": "pone.0253120.ref013",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0235460",
"article-title": "COVID-19 symptoms predictive of healthcare workers’ SARS-CoV-2 PCR results",
"author": "FY Lan",
"doi-asserted-by": "crossref",
"first-page": "e0235460",
"journal-title": "PLoS One",
"key": "pone.0253120.ref014",
"volume": "15",
"year": "2020"
},
{
"article-title": "Ocular Symptoms among Nonhospitalized Patients Who Underwent COVID-19 Testing",
"author": "SS Gangaputra",
"journal-title": "Ophthalmology",
"key": "pone.0253120.ref015",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0234765",
"article-title": "The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries",
"author": "MC Grant",
"doi-asserted-by": "crossref",
"first-page": "e0234765",
"journal-title": "PLoS One",
"key": "pone.0253120.ref016",
"volume": "15",
"year": "2020"
},
{
"article-title": "Loss of Taste and Smell as Distinguishing Symptoms of COVID-19",
"author": "P Dawson",
"journal-title": "Clin Infect Dis",
"key": "pone.0253120.ref017",
"year": "2020"
},
{
"DOI": "10.1016/j.idcr.2020.e00774",
"article-title": "Conjunctivitis can be the only presenting sign and symptom of COVID-19",
"author": "SZ Scalinci",
"doi-asserted-by": "crossref",
"first-page": "e00774",
"journal-title": "IDCases",
"key": "pone.0253120.ref018",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1542/peds.108.2.e31",
"article-title": "Adolescents’ perceptions of social status: development and evaluation of a new indicator",
"author": "E Goodman",
"doi-asserted-by": "crossref",
"first-page": "E31",
"journal-title": "Pediatrics",
"key": "pone.0253120.ref019",
"volume": "108",
"year": "2001"
},
{
"DOI": "10.1007/s12160-010-9181-9",
"article-title": "Endothelial function: the impact of objective and subjective socioeconomic status on flow-mediated dilation",
"author": "DC Cooper",
"doi-asserted-by": "crossref",
"first-page": "222",
"journal-title": "Ann Behav Med",
"key": "pone.0253120.ref020",
"volume": "39",
"year": "2010"
},
{
"DOI": "10.1002/pro.3268",
"article-title": "Visualizing correlated motion with HDBSCAN clustering",
"author": "RL Melvin",
"doi-asserted-by": "crossref",
"first-page": "62",
"journal-title": "Protein Sci",
"key": "pone.0253120.ref021",
"volume": "27",
"year": "2018"
},
{
"DOI": "10.1007/s10618-019-00651-1",
"article-title": "A unified view of density-based methods for semi-supervised clustering and classification",
"author": "J Castro Gertrudes",
"doi-asserted-by": "crossref",
"first-page": "1894",
"journal-title": "Data Min Knowl Discov",
"key": "pone.0253120.ref022",
"volume": "33",
"year": "2019"
},
{
"DOI": "10.1186/s12879-021-05950-x",
"article-title": "Serial interval and incubation period of COVID-19: a systematic review and meta-analysis",
"author": "M Alene",
"doi-asserted-by": "crossref",
"first-page": "257",
"journal-title": "BMC Infect Dis",
"key": "pone.0253120.ref023",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1086/655023",
"article-title": "Identifying the probable timing and setting of respiratory virus infections",
"author": "J Lessler",
"doi-asserted-by": "crossref",
"first-page": "809",
"journal-title": "Infect Control Hosp Epidemiol",
"key": "pone.0253120.ref024",
"volume": "31",
"year": "2010"
},
{
"DOI": "10.2807/1560-7917.ES.2020.25.16.2000508",
"article-title": "Strong associations and moderate predictive value of early symptoms for SARS-CoV-2 test positivity among healthcare workers, the Netherlands, March 2020",
"author": "A Tostmann",
"doi-asserted-by": "crossref",
"journal-title": "Euro Surveill",
"key": "pone.0253120.ref025",
"volume": "25",
"year": "2020"
},
{
"key": "pone.0253120.ref026",
"unstructured": "Center for Systems Science and Engineering at Johns Hopkins University. COVID-19 dashboard. (https://coronavirus.jhu.edu/map.html). 2020."
},
{
"article-title": "Rapid Scaling Up of COVID-19 Diagnostic Testing in the United States—The NIH RADx Initiative",
"author": "BJ Tromberg",
"journal-title": "N Engl J Med",
"key": "pone.0253120.ref027",
"year": "2020"
},
{
"article-title": "An overview of the safety, clinical application and antiviral research of the COVID-19 therapeutics",
"author": "D Wang",
"journal-title": "J Infect Public Health",
"key": "pone.0253120.ref028",
"year": "2020"
},
{
"DOI": "10.1038/s41563-020-0758-9",
"article-title": "COVID-19 therapies and vaccine landscape",
"doi-asserted-by": "crossref",
"first-page": "809",
"journal-title": "Nature materials",
"key": "pone.0253120.ref029",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1016/j.coviro.2018.01.001",
"article-title": "Transmission routes of respiratory viruses among humans",
"author": "JS Kutter",
"doi-asserted-by": "crossref",
"first-page": "142",
"journal-title": "Curr Opin Virol",
"key": "pone.0253120.ref030",
"volume": "28",
"year": "2018"
},
{
"DOI": "10.1038/nri2802",
"article-title": "Immunity and immunopathology to viruses: what decides the outcome?",
"author": "BT Rouse",
"doi-asserted-by": "crossref",
"first-page": "514",
"journal-title": "Nat Rev Immunol",
"key": "pone.0253120.ref031",
"volume": "10",
"year": "2010"
},
{
"DOI": "10.1136/bmj.m1328",
"article-title": "Prediction models for diagnosis and prognosis of covid-19 infection: systematic review and critical appraisal",
"author": "L Wynants",
"doi-asserted-by": "crossref",
"first-page": "m1328",
"journal-title": "BMJ",
"key": "pone.0253120.ref032",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1038/s41591-020-0916-2",
"article-title": "Real-time tracking of self-reported symptoms to predict potential COVID-19",
"author": "C Menni",
"doi-asserted-by": "crossref",
"first-page": "1037",
"journal-title": "Nat Med",
"key": "pone.0253120.ref033",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"article-title": "Factors associated with COVID-19-related death using OpenSAFELY",
"author": "EJ Williamson",
"doi-asserted-by": "crossref",
"first-page": "430",
"journal-title": "Nature",
"key": "pone.0253120.ref034",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1038/s41467-020-19741-6",
"article-title": "Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission",
"author": "H Peckham",
"doi-asserted-by": "crossref",
"first-page": "6317",
"journal-title": "Nat Commun",
"key": "pone.0253120.ref035",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.09.021",
"article-title": "Seroprevalence of SARS-CoV-2 significantly varies with age: Preliminary results from a mass population screening",
"author": "G Pagani",
"doi-asserted-by": "crossref",
"first-page": "e10",
"journal-title": "J Infect",
"key": "pone.0253120.ref036",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)31483-5",
"article-title": "Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study",
"author": "M Pollan",
"doi-asserted-by": "crossref",
"first-page": "535",
"journal-title": "Lancet",
"key": "pone.0253120.ref037",
"volume": "396",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30117-X",
"article-title": "Sex difference and smoking predisposition in patients with COVID-19",
"author": "H Cai",
"doi-asserted-by": "crossref",
"first-page": "e20",
"journal-title": "The Lancet Respiratory medicine",
"key": "pone.0253120.ref038",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6929e1",
"article-title": "Population Point Prevalence of SARS-CoV-2 Infection Based on a Statewide Random Sample—Indiana, April 25–29, 2020",
"author": "N Menachemi",
"doi-asserted-by": "crossref",
"first-page": "960",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "pone.0253120.ref039",
"volume": "69",
"year": "2020"
},
{
"article-title": "COVID-19 and comorbidities: a systematic review and meta-analysis",
"author": "MS Gold",
"first-page": "1",
"journal-title": "Postgrad Med",
"key": "pone.0253120.ref040",
"year": "2020"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047549",
"article-title": "The Science Underlying COVID-19: Implications for the Cardiovascular System",
"author": "PP Liu",
"doi-asserted-by": "crossref",
"first-page": "68",
"journal-title": "Circulation",
"key": "pone.0253120.ref041",
"volume": "142",
"year": "2020"
},
{
"DOI": "10.1161/CIR.0000000000000485",
"article-title": "Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association",
"author": "EJ Benjamin",
"doi-asserted-by": "crossref",
"first-page": "e146",
"journal-title": "Circulation",
"key": "pone.0253120.ref042",
"volume": "135",
"year": "2017"
},
{
"DOI": "10.1177/1179173X21994612",
"article-title": "Smoking and COVID-19: A Scoping Review",
"author": "C Haddad",
"doi-asserted-by": "crossref",
"journal-title": "Tob Use Insights",
"key": "pone.0253120.ref043",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1177/2040622320935765",
"article-title": "Current smoking, former smoking, and adverse outcome among hospitalized COVID-19 patients: a systematic review and meta-analysis",
"author": "K Farsalinos",
"doi-asserted-by": "crossref",
"first-page": "2040622320935765",
"journal-title": "Ther Adv Chronic Dis",
"key": "pone.0253120.ref044",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.psyneuen.2010.11.001",
"article-title": "A clinical allostatic load index is associated with burnout symptoms and hypocortisolemic profiles in healthy workers",
"author": "RP Juster",
"doi-asserted-by": "crossref",
"first-page": "797",
"journal-title": "Psychoneuroendocrinology",
"key": "pone.0253120.ref045",
"volume": "36",
"year": "2011"
},
{
"DOI": "10.1016/bs.pmbts.2015.08.001",
"article-title": "Exercise and the Regulation of Immune Functions",
"author": "RJ Simpson",
"doi-asserted-by": "crossref",
"first-page": "355",
"journal-title": "Prog Mol Biol Transl Sci",
"key": "pone.0253120.ref046",
"volume": "135",
"year": "2015"
},
{
"DOI": "10.2196/23897",
"article-title": "Rapid COVID-19 Screening Based on Self-Reported Symptoms: Psychometric Assessment and Validation of the EPICOVID19 Short Diagnostic Scale",
"author": "L Bastiani",
"doi-asserted-by": "crossref",
"first-page": "e23897",
"journal-title": "J Med Internet Res",
"key": "pone.0253120.ref047",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1080/20477724.2020.1847778",
"article-title": "Evolving virulence? Decreasing COVID-19 complications among Massachusetts healthcare workers: a cohort study",
"author": "FY Lan",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "Pathog Glob Health",
"key": "pone.0253120.ref048",
"volume": "115",
"year": "2021"
}
],
"reference-count": 48,
"references-count": 48,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0253120"
}
},
"score": 1,
"short-container-title": [
"PLoS ONE"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": [
"Predictors of incident viral symptoms ascertained in the era of COVID-19"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "16"
}
marcus