Exploring the rationale for thermotherapy in COVID-19
et al., International Journal of Hyperthermia, doi:10.1080/02656736.2021.1883127, Jan 2021
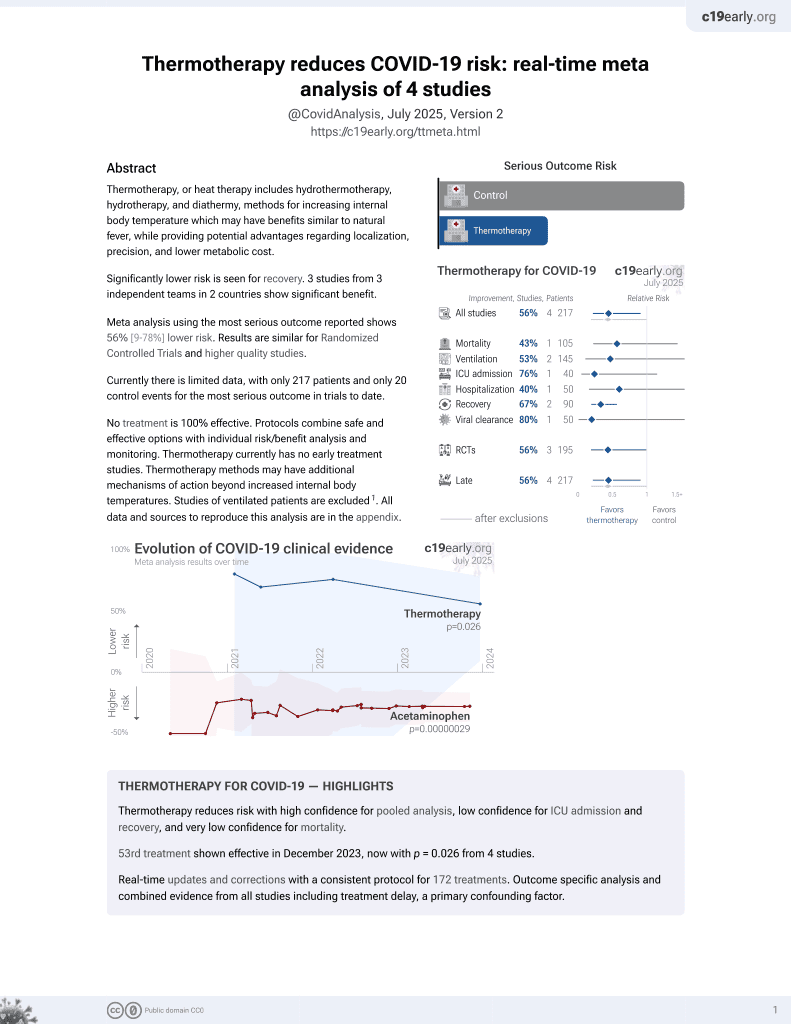
54th treatment shown to reduce risk in
December 2023, now with p = 0.026 from 4 studies.
Lower risk for recovery.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
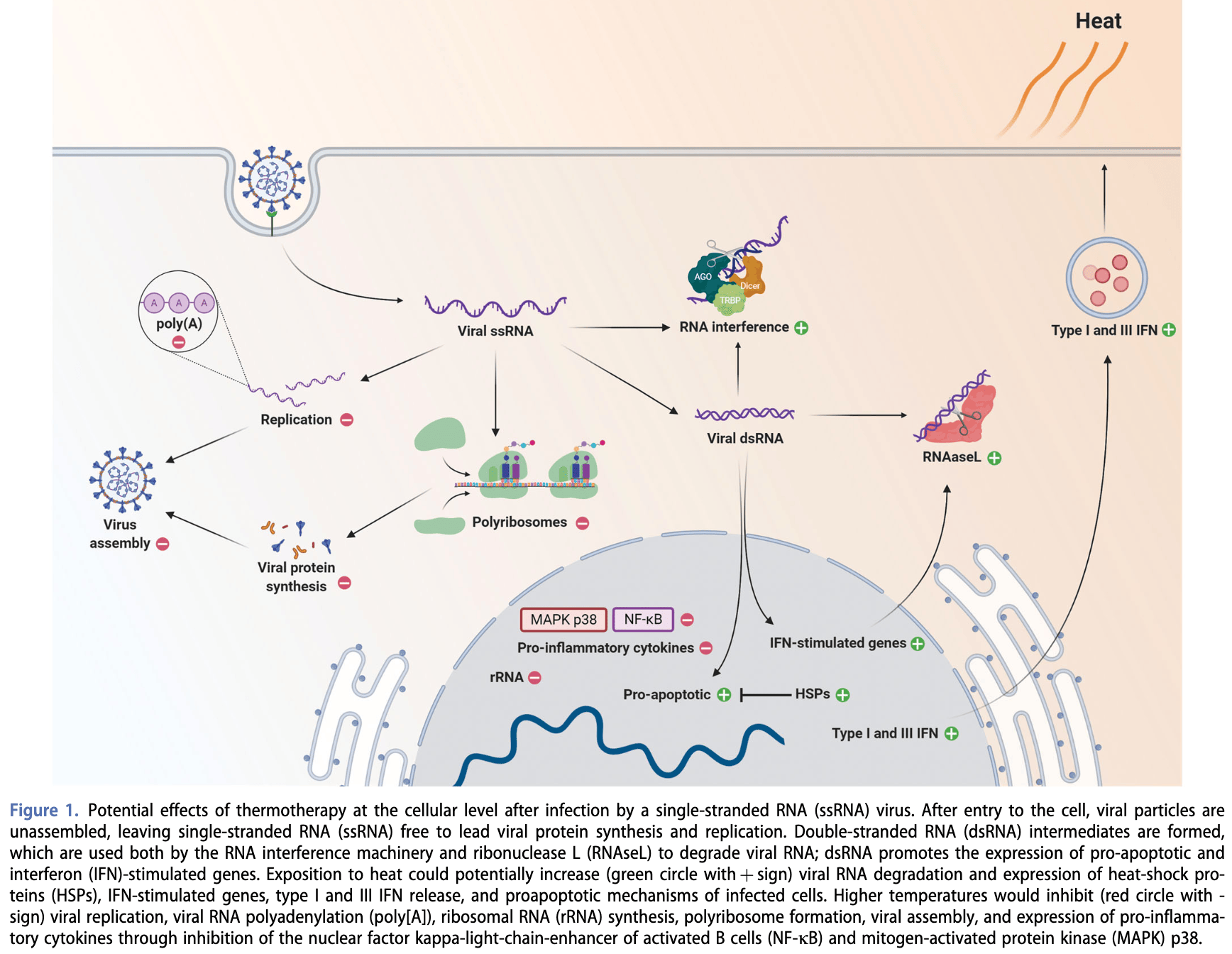
Review of thermotherapy (mild heat treatment) as a potential therapy for COVID-19. Authors review evidence showing SARS-CoV-2 is heat-sensitive, with reduced viral replication efficiency at body temperature compared to cooler upper airway temperatures. Several mechanisms are proposed by which mild hyperthermia could aid viral clearance and immunity in early stage COVID-19, including enhanced interferon responses, inhibition of viral enzymes/replication, increased antigen presentation, and effects on RNA interference.
1.
Smadja et al., Hyperthermia and targeting heat shock proteins: innovative approaches for neurodegenerative disorders and Long COVID, Frontiers in Neuroscience, doi:10.3389/fnins.2025.1475376.
2.
Kunutsor et al., Finnish sauna and COVID-19, Le Infezioni in Medicina, 1, www.infezmed.it/index.php/article?Anno=2021&numero=1&ArticoloDaVisualizzare=Vol_29_1_2021_160.
3.
Ramirez et al., Hydrothermotherapy in prevention and treatment of mild to moderate cases of COVID-19, Medical Hypotheses, doi:10.1016/j.mehy.2020.110363.
4.
Mancilla-Galindo et al., Exploring the rationale for thermotherapy in COVID-19, International Journal of Hyperthermia, doi:10.1080/02656736.2021.1883127.
5.
Larenas-Linnemann et al., Enhancing innate immunity against virus in times of COVID-19: Trying to untangle facts from fictions, World Allergy Organization Journal, doi:10.1016/j.waojou.2020.100476.
Mancilla-Galindo et al., 1 Jan 2021, peer-reviewed, 2 authors.
Contact: ngalindosevilla@hotmail.com.
Exploring the rationale for thermotherapy in COVID-19
International Journal of Hyperthermia, doi:10.1080/02656736.2021.1883127
Increased transmissibility of the pandemic severe acute respiratory coronavirus 2 (SARS-CoV-2) has been noted to occur at lower ambient temperatures. This is seemingly related to a better replication of most respiratory viruses, including SARS-CoV-2, at lower-than-core body temperatures (i.e., 33 C vs 37 C). Also, intrinsic characteristics of SARS-CoV-2 make it a heat-susceptible pathogen. Thermotherapy has successfully been used to combat viral infections in plants which could otherwise result in great economic losses; 90% of viruses causing infections in plants are positive-sense singlestranded ribonucleic acid (þssRNA) viruses, a characteristic shared by SARS-CoV-2. Thus, it is possible to envision the use of heat-based interventions (thermotherapy or mild-temperature hyperthermia) in patients with COVID-19 for which moderate cycles (every 8-12 h) of mild-temperature hyperthermia (1-2 h) have been proposed. However, there are potential safety and mechanistic concerns which could limit the use of thermotherapy only to patients with mild-to-moderate COVID-19 to prevent disease progression rather than to treat patients who have already progressed to severe-to-critical COVID-19. Here, we review the characteristics of SARS-CoV-2 which make it a heat-susceptible virus, potential host mechanisms which could be enhanced at higher temperatures to aid viral clearance, and how thermotherapy could be investigated as a modality of treatment in patients with COVID-19 while taking into consideration potential risks.
References
Adiliaghdam, Basavappa, Saunders, A requirement for argonaute 4 in mammalian antiviral defense, Cell Rep
Ameri, Rahnama, Bozorgmehr, Low-dose whole-lung irradiation for COVID-19 pneumonia: Short Course Results, Int J Radiation Oncol Biol Phys
Bassi, Hwenda, COVID-19: time to plan for prompt universal access to diagnostics and treatments, Lancet Glob Heal
Bester, Matshailwe, Pretorius, Simultaneous presence of hypercoagulation and increased clot lysis time due to IL-1b, IL-6 and IL-8, Cytokine
Blanco-Melo, Nilsson-Payant, Liu, Imbalanced host response to SARS-CoV-2 drives development of COVID-19, Cell
Bolhassani, Agi, Heat shock proteins in infection, Clin Chim Acta
Brosseau, Yonge, Welch, Thermotherapy for treatment of osteoarthritis, Cochrane Database Syst Rev
Cao, Li, COVID-19: towards understanding of pathogenesis, Cell Res
Carpinteiro, Edwards, Hoffmann, Pharmacological inhibition of acid sphingomyelinase prevents uptake of SARS-CoV-2 by epithelial cells, Cell Reports Med
Cerutti, Casas-Mollano, On the origin and functions of RNA-mediated silencing: from protists to man, Curr Genet
Chan, Siu, Chin, Modulation of the unfolded protein response by the severe acute respiratory syndrome coronavirus spike protein, J Virol
Chellappan, Vanitharani, Ogbe, Effect of temperature on geminivirus-induced RNA silencing in plants, Plant Physiol
Chen, Fisher, Clancy, Fever-range thermal stress promotes lymphocyte trafficking across high endothelial venules via an interleukin 6 trans-signaling mechanism, Nat Immunol
Chen, Liu, Guo, Emerging coronaviruses: genome structure, replication, and pathogenesis, J Med Virol
Chin, Chu, Perera, Stability of SARS-CoV-2 in different environmental conditions, Lancet Microbe
Connors, Levy, Thromboinflammation and the hypercoagulability of COVID-19, J Thromb Haemost
Cortese, Lee, Cerikan, Integrative imaging reveals SARS-CoV-2 induced reshaping of subcellular morphologies, Cell Host Microbe
Cui, Wang, Ji, The nucleocapsid protein of coronaviruses acts as a viral suppressor of RNA silencing in mammalian cells, J Virol
Davalos, Akassoglou, Fibrinogen as a key regulator of inflammation in disease, Semin Immunopathol
Dediego, Nieto-Torres, Enez-Guardeño, Severe acute respiratory syndrome coronavirus envelope protein regulates cell stress response and apoptosis, PLoS Pathog
Dewhirst, Vujaskovic, Jones, Re-setting the biologic rationale for thermal therapy, Int J Hyperthermia
Duan, Zhao, Wen, Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation, Biomed Environ Sci
Dunne, Regenold, Allen, Hyperthermia can alter tumor physiology and improve chemo-and radio-therapy efficacy, Adv Drug Deliv Rev
Fabri, Np, Malavazi, The dynamics and role of sphingolipids in eukaryotic organisms upon thermal adaptation, Prog Lipid Res
Foxman, Storer, Fitzgerald, Temperature-dependent innate defense against the common cold virus limits viral replication at warm temperature in mouse airway cells, Proc Natl Acad Sci
Foxman, Storer, Vanaja, Two interferon-independent double-stranded RNA-induced host defense strategies suppress the common cold virus at warm temperature, Proc Natl Acad Sci U S A
Gandhi, Lynch, Del Rio, Mild or moderate Covid-19, N Engl J Med
Gantier, Processing of double-stranded RNA in mammalian cells: a direct antiviral role?, J Interferon Cytokine Res
Gaythorpe, Imai, Cuomo-Dannenburg, Symptom progression of COVID-19
Gazel, Yı Lmaz M, Are infectious diseases and microbiology new fields for thermal therapy research?, Int J Hyperthermia
Ghiringhelli, Garrido, Can the hyperthermia-mediated Heat Shock Factor (HSF)/Heat Shock Protein (HSP) 70 pathway dampen the cytokine storm during SARS-CoV-2 infection?, Br J Pharmacol, doi:10.1111/bph.15343
Ghosh, Dellibovi-Ragheb, Kerviel, b-Coronaviruses use lysosomes for egress instead of the biosynthetic secretory pathway, Cell
Giammartino, Shi, Manley, PARP1 Represses PAP and Inhibits Polyadenylation during Heat Shock, Mol Cell
Gorbalenya, Baker, Baric, The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2, Nat Microbiol
Guan, Ni, Hu, Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med
Guihur, Rebeaud, Fauvet, Moderate fever cycles as a potential mechanism to protect the respiratory system in COVID-19 patients, Front Med
Gupta, Hayek, Wang, Factors Associated With Death in Critically Ill Patients With Coronavirus Disease 2019 in the US, JAMA Intern Med
Gupta, Therapeutic" facemasks, Med Hypotheses
Hadjadj, Yatim, Barnabei, Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients, Science
Hasday, Shah, Mackowiak, Fever, hyperthermia, and the lung: it's all about context and timing, Trans Am Clin Climatol Assoc
Hatzfeld-Charbonnier, Lasek, Castera, Influence of heat stress on human monocyte-derived dendritic cell functions with immunotherapeutic potential for antitumor vaccines, J Leukoc Biol
Hauptmann, Kater, Generation of catalytic human Ago4 identifies structural elements important for RNA cleavage, RNA
Hess, Buchwald, Stokes, Low-dose whole-lung radiation for COVID-19 pneumonia: planned day 7 interim analysis of a registered clinical trial, Cancer
Holwerda, Kelly, Laloli, Determining the replication kinetics and cellular tropism of influenza D virus on primary well-differentiated human airway epithelial cells, Viruses
Hurwitz, Hyperthermia and immunotherapy: clinical opportunities, Int J Hyperthermia
Jasi Nska-Konior, Sarna, Increased elasticity of melanoma cells after low-LET proton beam due to actin cytoskeleton rearrangements, Sci Rep
Kang, Yang, Hong, Crystal structure of SARS-CoV-2 nucleocapsid protein RNA binding domain reveals potential unique drug targeting sites, Acta Pharm Sin B
Kappel, Diamant, Hansen, Klokker, Effects of in vitro hyperthermia on the proliferative response of blood mononuclear cell subsets, and detection of interleukins 1 and 6, tumour necrosis factor-alpha and interferon-gamma, Immunology
Kappel, Stadeager, Tvede, Effects of in vivo hyperthermia on natural killer cell activity, in vitro proliferative responses and blood mononuclear cell subpopulations, Clin Exp Immunol
Karjee, Minhas, Sood, The 7a accessory protein of severe acute respiratory syndrome coronavirus acts as an RNA silencing suppressor, J Virol
Karjee, Mukherjee, RNAi suppressor: the hidden weapon of SARS-CoV, J Biosci
Knippertz, Stein, Mild hyperthermia enhances human monocyte-derived dendritic cell functions and offers potential for applications in vaccination strategies, Int J Hyperthermia
Koosha, Pourbagheri-Sigaroodi, Bakhshandeh, Lowdose radiotherapy (LD-RT) for COVID-19-induced pneumopathy: a worth considering approach, Int J Radiat Biol
Laporte, Stevaert, Raeymaekers, The SARS-CoV-2 and other human coronavirus spike proteins are fine-tuned towards temperature and proteases of the human airways, bioRxiv, doi:10.1101/2020.11.09.374603
Lee, Channappanavar, Kanneganti, Coronaviruses: innate immunity, inflammasome activation, inflammatory cell death, and cytokines, Trends Immunol
Li, Lu, Han, RNA interference functions as an antiviral immunity mechanism in mammals, Science
Li, Mitigating coronavirus-induced acute respiratory distress syndrome by radiotherapy, iScience
Lin, Chen, Regulation of immune cell trafficking by febrile temperatures, Int J Hyperthermia
Lipsitch, Perlman, Waldor, Testing COVID-19 therapies to prevent progression of mild disease, Lancet Infect Dis
Liso, Castellani, Massenzio, Human monocyte-derived dendritic cells exposed to hyperthermia show a distinct gene expression profile and selective upregulation of IGFBP6, Oncotarget
Liu, Zhang, Yang, Characterization of virus-derived small interfering RNAs in Apple stem grooving virus-infected in vitro-cultured Pyrus pyrifolia shoot tips in response to high temperature treatment, Virol J
Maillard, Ciaudo, Marchais, Antiviral RNA interference in mammalian cells, Science
Maillard, Van Der Veen, Deddouche-Grass, Inactivation of the type I interferon pathway reveals long double-stranded RNA-mediated RNA interference in mammalian cells, Embo J
Maillard, Veen, Poirier, Slicing and dicing viruses: antiviral RNA interference in mammals, Embo J
Mao, Liang, Gao, A photostable Si-rhodaminebased near-infrared fluorescent probe for monitoring lysosomal pH during heat stroke, Anal Chim Acta
Mccormick, Penman, Regulation of protein synthesis in HeLa cells: translation at elevated temperatures, J Mol Biol
Modzelewski, Holmes, Hilz, AGO4 regulates entry into meiosis and influences silencing of sex chromosomes in the male mouse germline, Dev Cell
Mu, Xu, Zhang, SARS-CoV-2-encoded nucleocapsid protein acts as a viral suppressor of RNA interference in cells, Sci China Life Sci
Nakamura, Hall, The mechanism by which body temperature inhibits protein biosynthesis in spermatids of rat testes, J Biol Chem
Pawlik, Nowak, Grzanka, Hyperthermia induces cytoskeletal alterations and mitotic catastrophe in p53-deficient H1299 lung cancer cells, Acta Histochem
Peng, Hyde, Pai, Monocyte-derived DC primed with TLR agonists secrete IL-12p70 in a CD40-dependent manner under hyperthermic conditions, J Immunother
Peng, Lin, Lin, Characterization of the role of hexamer AGUAAA and poly(A) tail in coronavirus polyadenylation, PLoS One
Peng, Peng, Yuan, Structural and biochemical characterization of the nsp12-nsp7-nsp8 core polymerase complex from SARS-CoV-2, Cell Rep
Petri, Dueck, Lehmann, Increased siRNA duplex stability correlates with reduced off-target and elevated on-target effects, RNA
Philip, Gultom, Steiner, Disparate temperaturedependent virushost dynamics for SARS-CoV-2 and SARS-CoV in the human respiratory epithelium, bioRxiv, doi:10.1101/2020.04.27.062315
Pierce, Preston-Hurlburt, Dai, Immune responses to SARS-CoV-2 infection in hospitalized pediatric and adult patients, Sci Transl Med
Prow, Tang, Gardner, Lower temperatures reduce type I interferon activity and promote alphaviral arthritis, PLoS Pathog
Qian, Zhou, Shu, The capsid protein of Semliki forest virus antagonizes RNA interference in mammalian cells, J Virol
Qiu, Xu, Wang, Flavivirus induces and antagonizes antiviral RNA interference in both mammals and mosquitoes, Sci Adv
Ran, Zhao, Han, A re-analysis in exploring the association between temperature and COVID-19 transmissibility: an ecological study with 154 Chinese cities, Eur Respir J
Sadis, Hickey, Weber, Effect of heat shock on RNA metabolism in HeLa cells, J Cell Physiol
Sajadi, Habibzadeh, Vintzileos, Temperature, humidity, and latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (COVID-19), JAMA Netw Open
Schuster, Overheul, Bauer, No evidence for viral small RNA production and antiviral function of Argonaute 2 in human cells, Sci Rep
Schuster, Tholen, Overheul, Deletion of cytoplasmic double-stranded RNA sensors does not uncover viral small interfering RNA production in human cells, mSphere
Sette, Crotty, Adaptive immunity to SARS-CoV-2 and COVID-19, Cell, doi:10.1016/j.cell.2021.01.007
Shabalina, Koonin, Origins and evolution of eukaryotic RNA interference, Trends Ecol Evol
Shalgi, Hurt, Lindquist, Widespread inhibition of posttranscriptional splicing shapes the cellular transcriptome following heat shock, Cell Rep
Shen, Lu, Young, Influence of elevated temperature on natural killer cell activity, lymphokine-activated killer cell activity and lectin-dependent cytotoxicity of human umbilical cord blood and adult blood cells, Int J Radiat Oncol Biol Phys
Singh, Hasday, Fever, hyperthermia and the heat shock response, Int J Hyperthermia
Stuhlmeier, Short term hyperthermia prevents the activation of mitogen-activated protein kinase p38, Exp Gerontol
Tan, Linster, Tan, Early induction of SARS-CoV-2 specific T cells associates with rapid viral clearance and mild disease in COVID-19 patients, Cell Reports, doi:10.1016/j.celrep.2021.108728
Tharakan, Nomoto, Miyashita, Body temperature correlates with mortality in COVID-19 patients, Crit Care
Tilocca, Soggiu, Sanguinetti, Comparative computational analysis of SARS-CoV-2 nucleocapsid protein epitopes in taxonomically related coronaviruses, Microbes Infect
Torigoe, Tamura, Sato, Heat shock proteins and immunity: application of hyperthermia for immunomodulation, Int J Hyperthermia
Tulapurkar, Asiegbu, Singh, Hyperthermia in the febrile range induces HSP72 expression proportional to exposure temperature but not to HSF-1 DNA-binding activity in human lung epithelial A549 cells, Cell Stress Chaperones
Umar, Das, Gupta, Febrile temperature change modulates CD4 T cell differentiation via a TRPV channel-regulated Notch-dependent pathway, Proc Natl Acad Sci
Valle, Kim-Schulze, Huang, An inflammatory cytokine signature predicts COVID-19 severity and survival, Nat Med
Van Leeuwen, Crezee, Oei, The effect of time interval between radiotherapy and hyperthermia on planned equivalent radiation dose, Int J Hyperthermia
Voinnet, RNA silencing as a plant immune system against viruses, Trends Genet
Walter, Hanna-Jumma, Carraretto, The pathophysiological basis and consequences of fever, Crit Care
Wang, Cui, Li, In vitro thermotherapy-based methods for plant virus eradication, Plant Methods
Wang, Ni, Wan, Febrile temperature critically controls the differentiation and pathogenicity of T helper 17 cells, Immunity
Wang, Wu, Wang, Low stability of nucleocapsid protein in SARS virus, Biochemistry
Waterhouse, Wang, Lough, Gene silencing as an adaptive defence against viruses, Nature
Welch, Brosseau, Casimiro, Thermotherapy for treating rheumatoid arthritis, Cochrane Database Syst Rev
Wheeler, Wong, Heat shock response and acute lung injury, Free Radic Biol Med
Wilk, Rustagi, Zhao, A single-cell atlas of the peripheral immune response in patients with severe COVID-19, Nat Med
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature
Wu, Jing, Liu, Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries, Sci Total Environ
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention, JAMA
Wynant, Santos, Broeck, The evolution of animal Argonautes: evidence for the absence of antiviral AGO Argonautes in vertebrates, Sci Rep
Yao, Pan, Liu, No association of COVID-19 transmission with temperature or UV radiation in Chinese cities, Eur Respir J
Yap, Liu, Shveda, A predictive model of the temperature-dependent inactivation of coronaviruses, Appl Phys Lett
Yarmolenko, Moon, Landon, Thresholds for thermal damage to normal tissues: an update, Int J Hyperthermia
Zhang, Mehta, Cohen, Hyperthermia on immune regulation: a temperature's story, Cancer Lett
Zhang, Zhang, Singh, Temperature-dependent survival of turnip crinkle virus-infected arabidopsis plants relies on an RNA silencing-based defense that requires DCL2, AGO2, and HEN1, J Virol
Zhao, Dammert, Hoppe, Heat shock represses rRNA synthesis by inactivation of TIF-IA and lncRNA-dependent changes in nucleosome positioning, Nucleic Acids Res
Zhou, Yang, Wang, A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature
Zhu, Gao, Qi, Local hyperthermia could induce antiviral activity by endogenous interferon-dependent pathway in condyloma acuminata, Antiviral Res
DOI record:
{
"DOI": "10.1080/02656736.2021.1883127",
"ISSN": [
"0265-6736",
"1464-5157"
],
"URL": "http://dx.doi.org/10.1080/02656736.2021.1883127",
"alternative-id": [
"10.1080/02656736.2021.1883127"
],
"assertion": [
{
"label": "Peer Review Statement",
"name": "peerreview_statement",
"order": 1,
"value": "The publishing and review policy for this title is described in its Aims & Scope."
},
{
"URL": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=ihyt20",
"label": "Aim & Scope",
"name": "aims_and_scope_url",
"order": 2,
"value": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=ihyt20"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2020-08-10"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Revised",
"name": "revised",
"order": 1,
"value": "2021-01-14"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "2021-01-22"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 3,
"value": "2021-03-07"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-0718-467X",
"affiliation": [
{
"name": "Facultad de Medicina, División de Investigación, Unidad de Investigación UNAM-INC, Instituto Nacional de Cardiología Ignacio Chávez, Mexico City, Mexico"
}
],
"authenticated-orcid": false,
"family": "Mancilla-Galindo",
"given": "Javier",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-6639-8475",
"affiliation": [
{
"name": "Departamento de Infectología e Inmunología, Instituto Nacional de Perinatología, Mexico City, Mexico"
}
],
"authenticated-orcid": false,
"family": "Galindo-Sevilla",
"given": "Norma",
"sequence": "additional"
}
],
"container-title": "International Journal of Hyperthermia",
"container-title-short": "International Journal of Hyperthermia",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"www.tandfonline.com"
]
},
"created": {
"date-parts": [
[
2021,
3,
8
]
],
"date-time": "2021-03-08T07:31:43Z",
"timestamp": 1615188703000
},
"deposited": {
"date-parts": [
[
2022,
8,
5
]
],
"date-time": "2022-08-05T03:14:10Z",
"timestamp": 1659669250000
},
"funder": [
{
"DOI": "10.13039/501100007686",
"award": [
"INPer 2020-1-19"
],
"doi-asserted-by": "crossref",
"name": "Instituto Nacional de Perinatología ‘Isidro Espinosa de los Reyes’"
}
],
"indexed": {
"date-parts": [
[
2023,
12,
22
]
],
"date-time": "2023-12-22T05:26:54Z",
"timestamp": 1703222814820
},
"is-referenced-by-count": 6,
"issue": "1",
"issued": {
"date-parts": [
[
2021,
1,
1
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2021,
1,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
}
],
"link": [
{
"URL": "https://www.tandfonline.com/doi/pdf/10.1080/02656736.2021.1883127",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "202-212",
"prefix": "10.1080",
"published": {
"date-parts": [
[
2021,
1,
1
]
]
},
"published-online": {
"date-parts": [
[
2021,
3,
7
]
]
},
"published-print": {
"date-parts": [
[
2021,
1,
1
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1183/13993003.00517-2020",
"doi-asserted-by": "publisher",
"key": "CIT0001"
},
{
"DOI": "10.1183/13993003.01253-2020",
"doi-asserted-by": "publisher",
"key": "CIT0002"
},
{
"DOI": "10.1001/jamanetworkopen.2020.11834",
"doi-asserted-by": "publisher",
"key": "CIT0003"
},
{
"DOI": "10.1016/j.scitotenv.2020.139051",
"doi-asserted-by": "publisher",
"key": "CIT0004"
},
{
"DOI": "10.1016/j.mehy.2020.109855",
"doi-asserted-by": "publisher",
"key": "CIT0005"
},
{
"author": "Bassi LL",
"first-page": "e756–7",
"issue": "6",
"journal-title": "Lancet Glob Heal",
"key": "CIT0006",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1038/s41564-020-0695-z",
"doi-asserted-by": "publisher",
"key": "CIT0007"
},
{
"DOI": "10.1002/jmv.25681",
"doi-asserted-by": "publisher",
"key": "CIT0008"
},
{
"DOI": "10.1038/s41586-020-2012-7",
"doi-asserted-by": "publisher",
"key": "CIT0009"
},
{
"DOI": "10.1016/j.apsb.2020.04.009",
"doi-asserted-by": "publisher",
"key": "CIT0010"
},
{
"DOI": "10.1016/j.micinf.2020.04.002",
"doi-asserted-by": "publisher",
"key": "CIT0011"
},
{
"DOI": "10.1021/bi049194b",
"doi-asserted-by": "publisher",
"key": "CIT0012"
},
{
"author": "Duan S-M",
"first-page": "246",
"issue": "3",
"journal-title": "Biomed Environ Sci",
"key": "CIT0013",
"volume": "16",
"year": "2003"
},
{
"DOI": "10.1016/S2666-5247(20)30003-3",
"doi-asserted-by": "publisher",
"key": "CIT0014"
},
{
"DOI": "10.1016/j.celrep.2020.107774",
"doi-asserted-by": "publisher",
"key": "CIT0015"
},
{
"DOI": "10.1063/5.0020782",
"doi-asserted-by": "publisher",
"key": "CIT0016"
},
{
"DOI": "10.1073/pnas.1411030112",
"doi-asserted-by": "publisher",
"key": "CIT0017"
},
{
"DOI": "10.3390/v11040377",
"doi-asserted-by": "publisher",
"key": "CIT0018"
},
{
"DOI": "10.1101/2020.04.27.062315",
"doi-asserted-by": "publisher",
"key": "CIT0019"
},
{
"author": "Laporte M",
"journal-title": "bioRxiv",
"key": "CIT0020"
},
{
"DOI": "10.1073/pnas.1601942113",
"doi-asserted-by": "publisher",
"key": "CIT0021"
},
{
"DOI": "10.1016/j.cell.2020.04.026",
"doi-asserted-by": "publisher",
"key": "CIT0022"
},
{
"DOI": "10.1126/science.abc6027",
"doi-asserted-by": "publisher",
"key": "CIT0023"
},
{
"DOI": "10.1016/S0021-9258(19)85826-X",
"doi-asserted-by": "publisher",
"key": "CIT0024"
},
{
"DOI": "10.1016/0022-2836(69)90320-9",
"doi-asserted-by": "publisher",
"key": "CIT0025"
},
{
"DOI": "10.1002/jcp.1041350304",
"doi-asserted-by": "publisher",
"key": "CIT0026"
},
{
"DOI": "10.1093/nar/gkw496",
"doi-asserted-by": "publisher",
"key": "CIT0027"
},
{
"DOI": "10.1016/j.celrep.2014.04.044",
"doi-asserted-by": "publisher",
"key": "CIT0028"
},
{
"DOI": "10.1016/j.molcel.2012.11.005",
"doi-asserted-by": "publisher",
"key": "CIT0029"
},
{
"DOI": "10.1371/journal.pone.0165077",
"doi-asserted-by": "publisher",
"key": "CIT0030"
},
{
"DOI": "10.1016/j.chom.2020.11.003",
"doi-asserted-by": "publisher",
"key": "CIT0031"
},
{
"DOI": "10.1016/j.acthis.2012.02.006",
"doi-asserted-by": "publisher",
"key": "CIT0032"
},
{
"DOI": "10.1038/s41598-019-43453-7",
"doi-asserted-by": "publisher",
"key": "CIT0033"
},
{
"DOI": "10.1016/j.cell.2020.10.039",
"doi-asserted-by": "publisher",
"key": "CIT0034"
},
{
"DOI": "10.1016/j.aca.2019.09.053",
"doi-asserted-by": "publisher",
"key": "CIT0035"
},
{
"DOI": "10.1080/02656736.2019.1653499",
"doi-asserted-by": "publisher",
"key": "CIT0036"
},
{
"DOI": "10.1080/02656736.2018.1440015",
"doi-asserted-by": "publisher",
"key": "CIT0037"
},
{
"DOI": "10.1080/02656736.2019.1647357",
"doi-asserted-by": "publisher",
"key": "CIT0038"
},
{
"DOI": "10.1016/j.freeradbiomed.2006.08.028",
"doi-asserted-by": "publisher",
"key": "CIT0039"
},
{
"author": "Rébé C",
"first-page": "1",
"journal-title": "Br J Pharmacol",
"key": "CIT0040",
"year": "2020"
},
{
"DOI": "10.1016/j.cca.2019.08.015",
"doi-asserted-by": "publisher",
"key": "CIT0041"
},
{
"DOI": "10.1128/JVI.00659-06",
"doi-asserted-by": "publisher",
"key": "CIT0042"
},
{
"DOI": "10.1371/journal.ppat.1002315",
"doi-asserted-by": "publisher",
"key": "CIT0043"
},
{
"DOI": "10.1016/j.xcrm.2020.100142",
"doi-asserted-by": "publisher",
"key": "CIT0044"
},
{
"DOI": "10.1016/j.plipres.2020.101063",
"doi-asserted-by": "publisher",
"key": "CIT0045"
},
{
"DOI": "10.1111/j.1365-2249.1991.tb08144.x",
"doi-asserted-by": "publisher",
"key": "CIT0046"
},
{
"DOI": "10.1016/0360-3016(94)90571-1",
"doi-asserted-by": "publisher",
"key": "CIT0047"
},
{
"DOI": "10.3109/02656736.2011.589234",
"doi-asserted-by": "publisher",
"key": "CIT0048"
},
{
"DOI": "10.18632/oncotarget.18338",
"doi-asserted-by": "publisher",
"key": "CIT0049"
},
{
"DOI": "10.1097/01.cji.0000211308.82997.4e",
"doi-asserted-by": "publisher",
"key": "CIT0050"
},
{
"DOI": "10.1189/jlb.0506347",
"doi-asserted-by": "publisher",
"key": "CIT0051"
},
{
"DOI": "10.1073/pnas.1922683117",
"doi-asserted-by": "publisher",
"key": "CIT0052"
},
{
"author": "Sette A",
"first-page": "1",
"journal-title": "Cell",
"key": "CIT0053",
"year": "2021"
},
{
"author": "Tan AT",
"first-page": "1",
"journal-title": "Cell Reports",
"key": "CIT0054",
"year": "2021"
},
{
"DOI": "10.1126/scitranslmed.abd5487",
"doi-asserted-by": "publisher",
"key": "CIT0055"
},
{
"DOI": "10.1016/j.immuni.2020.01.006",
"doi-asserted-by": "publisher",
"key": "CIT0056"
},
{
"DOI": "10.1038/s41591-020-1051-9",
"doi-asserted-by": "publisher",
"key": "CIT0057"
},
{
"DOI": "10.1016/j.it.2020.10.005",
"doi-asserted-by": "publisher",
"key": "CIT0058"
},
{
"DOI": "10.1007/s00281-011-0290-8",
"doi-asserted-by": "publisher",
"key": "CIT0059"
},
{
"DOI": "10.1016/j.cyto.2018.01.007",
"doi-asserted-by": "publisher",
"key": "CIT0060"
},
{
"DOI": "10.1111/jth.14849",
"doi-asserted-by": "publisher",
"key": "CIT0061"
},
{
"DOI": "10.1016/j.exger.2009.03.002",
"doi-asserted-by": "publisher",
"key": "CIT0062"
},
{
"author": "Kappel M",
"first-page": "304",
"issue": "3",
"journal-title": "Immunology",
"key": "CIT0063",
"volume": "73",
"year": "1991"
},
{
"DOI": "10.1016/S0168-9525(01)02367-8",
"doi-asserted-by": "publisher",
"key": "CIT0064"
},
{
"DOI": "10.1038/35081168",
"doi-asserted-by": "publisher",
"key": "CIT0065"
},
{
"DOI": "10.1089/jir.2014.0003",
"doi-asserted-by": "publisher",
"key": "CIT0066"
},
{
"DOI": "10.1007/s00294-006-0078-x",
"doi-asserted-by": "publisher",
"key": "CIT0067"
},
{
"DOI": "10.1016/j.tree.2008.06.005",
"doi-asserted-by": "publisher",
"key": "CIT0068"
},
{
"DOI": "10.1126/science.1241911",
"doi-asserted-by": "publisher",
"key": "CIT0069"
},
{
"DOI": "10.1126/science.1241930",
"doi-asserted-by": "publisher",
"key": "CIT0070"
},
{
"DOI": "10.15252/embj.201695086",
"doi-asserted-by": "publisher",
"key": "CIT0071"
},
{
"DOI": "10.1128/mSphere.00333-17",
"doi-asserted-by": "publisher",
"key": "CIT0072"
},
{
"DOI": "10.1038/s41598-019-50287-w",
"doi-asserted-by": "publisher",
"key": "CIT0073"
},
{
"DOI": "10.1038/s41598-017-08043-5",
"doi-asserted-by": "publisher",
"key": "CIT0074"
},
{
"DOI": "10.1261/rna.045203.114",
"doi-asserted-by": "publisher",
"key": "CIT0075"
},
{
"DOI": "10.1261/rna.2348111",
"doi-asserted-by": "publisher",
"key": "CIT0076"
},
{
"DOI": "10.1016/j.devcel.2012.07.003",
"doi-asserted-by": "publisher",
"key": "CIT0077"
},
{
"DOI": "10.1016/j.celrep.2020.01.021",
"doi-asserted-by": "publisher",
"key": "CIT0078"
},
{
"DOI": "10.15252/embj.2018100941",
"doi-asserted-by": "publisher",
"key": "CIT0079"
},
{
"DOI": "10.1007/s12038-020-00071-0",
"doi-asserted-by": "publisher",
"key": "CIT0080"
},
{
"DOI": "10.1104/pp.105.066563",
"doi-asserted-by": "publisher",
"key": "CIT0081"
},
{
"DOI": "10.1128/JVI.00497-12",
"doi-asserted-by": "publisher",
"key": "CIT0082"
},
{
"DOI": "10.1186/s12985-016-0625-0",
"doi-asserted-by": "publisher",
"key": "CIT0083"
},
{
"DOI": "10.1186/s13007-018-0355-y",
"doi-asserted-by": "publisher",
"key": "CIT0084"
},
{
"DOI": "10.1080/02656730500271668",
"doi-asserted-by": "publisher",
"key": "CIT0085"
},
{
"DOI": "10.3109/02656736.2010.534527",
"doi-asserted-by": "publisher",
"key": "CIT0086"
},
{
"DOI": "10.1038/ni1406",
"doi-asserted-by": "publisher",
"key": "CIT0087"
},
{
"DOI": "10.1007/s12192-009-0103-3",
"doi-asserted-by": "publisher",
"key": "CIT0088"
},
{
"DOI": "10.3109/02656730903315831",
"doi-asserted-by": "publisher",
"key": "CIT0089"
},
{
"DOI": "10.1016/j.canlet.2008.05.026",
"doi-asserted-by": "publisher",
"key": "CIT0090"
},
{
"author": "Welch V",
"first-page": "CD002826",
"issue": "2",
"journal-title": "Cochrane Database Syst Rev",
"key": "CIT0091",
"volume": "2002",
"year": "2002"
},
{
"author": "Brosseau L",
"first-page": "CD004522",
"issue": "4",
"journal-title": "Cochrane Database Syst Rev",
"key": "CIT0092",
"volume": "2003",
"year": "2003"
},
{
"DOI": "10.1371/journal.ppat.1006788",
"doi-asserted-by": "publisher",
"key": "CIT0093"
},
{
"DOI": "10.1016/j.antiviral.2010.08.012",
"doi-asserted-by": "publisher",
"key": "CIT0094"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"doi-asserted-by": "publisher",
"key": "CIT0095"
},
{
"DOI": "10.1038/s41591-020-0944-y",
"doi-asserted-by": "publisher",
"key": "CIT0096"
},
{
"DOI": "10.1001/jama.2020.2648",
"doi-asserted-by": "publisher",
"key": "CIT0097"
},
{
"DOI": "10.1056/NEJMcp2009249",
"doi-asserted-by": "publisher",
"key": "CIT0098"
},
{
"DOI": "10.1038/s41422-020-0327-4",
"doi-asserted-by": "publisher",
"key": "CIT0099"
},
{
"DOI": "10.1016/S1473-3099(20)30372-8",
"doi-asserted-by": "publisher",
"key": "CIT0100"
},
{
"DOI": "10.1186/s13054-020-03045-8",
"doi-asserted-by": "publisher",
"key": "CIT0101"
},
{
"DOI": "10.1186/s13054-016-1375-5",
"doi-asserted-by": "publisher",
"key": "CIT0102"
},
{
"author": "Hasday JD",
"first-page": "34",
"journal-title": "Trans Am Clin Climatol Assoc",
"key": "CIT0103",
"volume": "122",
"year": "2011"
},
{
"DOI": "10.3109/02656736.2013.808766",
"doi-asserted-by": "publisher",
"key": "CIT0104"
},
{
"DOI": "10.3389/fmed.2020.564170",
"author": "Guihur A",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Front Med",
"key": "CIT0105",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.addr.2020.07.007",
"doi-asserted-by": "publisher",
"key": "CIT0106"
},
{
"DOI": "10.1080/02656736.2018.1468930",
"doi-asserted-by": "publisher",
"key": "CIT0107"
},
{
"DOI": "10.1016/j.isci.2020.101215",
"doi-asserted-by": "publisher",
"key": "CIT0108"
},
{
"DOI": "10.1080/09553002.2021.1864049",
"doi-asserted-by": "publisher",
"key": "CIT0109"
},
{
"DOI": "10.1002/cncr.33130",
"doi-asserted-by": "publisher",
"key": "CIT0110"
},
{
"DOI": "10.1016/j.ijrobp.2020.07.026",
"doi-asserted-by": "publisher",
"key": "CIT0111"
},
{
"DOI": "10.1056/NEJMoa2002032",
"doi-asserted-by": "publisher",
"key": "CIT0112"
},
{
"key": "CIT0113",
"unstructured": "Gaythorpe K, Imai N, Cuomo-Dannenburg G, et al. Symptom progression of COVID-19 [Internet]. Imperial College London. London; 2020 [2020 Mar 11; vols 2020-03–11]. Available from: https://spiral.imperial.ac.uk/handle/10044/1/77344."
},
{
"DOI": "10.1001/jamainternmed.2020.3596",
"doi-asserted-by": "publisher",
"key": "CIT0114"
},
{
"DOI": "10.1128/JVI.01233-19",
"doi-asserted-by": "publisher",
"key": "CIT0115"
},
{
"DOI": "10.1126/sciadv.aax7989",
"doi-asserted-by": "publisher",
"key": "CIT0116"
},
{
"DOI": "10.1128/JVI.01331-15",
"doi-asserted-by": "publisher",
"key": "CIT0117"
},
{
"DOI": "10.1128/JVI.00748-10",
"doi-asserted-by": "publisher",
"key": "CIT0118"
},
{
"DOI": "10.1007/s11427-020-1692-1",
"doi-asserted-by": "publisher",
"key": "CIT0119"
}
],
"reference-count": 119,
"references-count": 119,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.tandfonline.com/doi/full/10.1080/02656736.2021.1883127"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cancer Research",
"Physiology (medical)",
"Physiology"
],
"subtitle": [],
"title": "Exploring the rationale for thermotherapy in COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1080/tandf_crossmark_01",
"volume": "38"
}