Association of cannabis with chronic obstructive pulmonary disease and COVID-19 infection
et al., Chronic Diseases and Translational Medicine, doi:10.1002/cdt3.38, Jun 2022
UK Biobank retrospective showing a higher risk of COVID-19 cases with a history of cannabis use.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
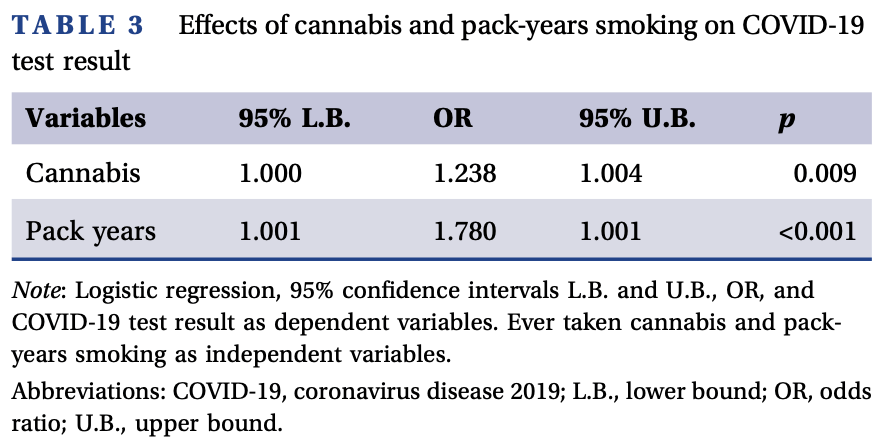
risk of case, 23.8% higher, OR 1.24, p = 0.009, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Lehrer et al., 22 Jun 2022, retrospective, United Kingdom, peer-reviewed, mean age 57.0, 3 authors, study period 16 March, 2020 - 26 April, 2020.
Contact: stevenlehrer@hotmail.com.
Abstract: Received: 14 April 2022
| Accepted: 7 June 2022
DOI: 10.1002/cdt3.38
BRIEF REPORT
Association of cannabis with chronic obstructive pulmonary
disease and COVID‐19 infection
Steven Lehrer1
|
Peter H. Rheinstein2
1
Department of Radiation Oncology, Icahn School of Medicine at Mount Sinai, New York, New York, USA
2
Severn Health Solutions, Severna Park, Maryland, USA
Correspondence: Steven Lehrer, Mt Sinai Medical Center, Box 1236 Radiation Oncology, 1 Gustave L. Levy Pl, New York, NY 10029, USA.
Email: stevenlehrer@hotmail.com
Edited by: Yi Cui
Funding information
Office of Research Infrastructure of the National Institutes of Health, Grant/Award Number: S10OD018522, S10OD026880
K E Y W O R DS
cannabis, COPD, COVID‐19, lungs, tobacco
In a 2012 study, occasional and low cumulative cannabis
use was not associated with adverse effects on pulmonary
function.1 With tobacco, the more used, the more loss of air
flow rate and lung volume. The same was not true with
cannabis use. Air flow rate increased rather than decreased
with increased exposure to cannabis up to a certain level.
An important factor that helped explain the difference in effects from tobacco and cannabis was the
amount of each that was smoked. Tobacco users
typically smoked 10–20 cigarettes daily, some even
more. Cannabis smokers, on average, smoked only two
to three times a month, so the average exposure to
cannabis was much lower than for tobacco. People
experiment with cannabis in their late teens and 20s,
and some consume relatively low levels for years.
Although heavy exposure to cannabis might damage
the lungs, reliable estimates of the effects of heavy
use were not available in the 2012 study, as heavy users
were relatively rare in the study population.
In the current analysis, we used data from UK
Biobank (UKB) to assess the effect of cannabis on
coronavirus disease (COVID‐19) infection and to determine whether cannabis lung damage might facilitate
COVID‐19 infection in formerly heavy users.
The UKB is a large prospective observational study
comprising about 500,000 men and women (N = 229,134
men, N = 273,402 women), more than 90% White, aged
40–69 years at enrollment. Participants were recruited
from across 22 centers located throughout England, Wales,
and Scotland, between 2006 and 2010, and continue to be
longitudinally followed for capture of subsequent health
events.2 This methodology is like that of the Framingham
Heart Study,3 with the exception that the UKB program
collects postmortem samples, which Framingham did not.
Our UKB application was approved as UKB project
57,245 (S.L. and P.H.R.).
Doctor‐diagnosed chronic obstructive pulmonary
disease (COPD) is from UKB data field 22,130. At
enrollment, the subject was asked on a touchscreen,
“Has a doctor ever told you that you have had any of the
conditions below?” COPD (Chronic Obstructive Pulmonary Disease) was one of the options listed.
The subject was asked, “Have you taken cannabis
(marijuana, grass, hash, ganja, blow, draw, skunk,
weed, spliff, dope), even if it was a long time ago?”
If the answer was “yes,” cannabis use was recorded in
the UKB data field 20,454, maximum frequency of
taking cannabis, question asked: “Considering when
you were taking cannabis most regularly, how often did
you take it?” Answers were 1 = Less than once a month,
2 = Once a month or more, but not every week, 3 = Once
a week or more, but not every day, and 4 = Every day.
Subject was then asked (UKB data field 20455) “About
how old..
DOI record:
{
"DOI": "10.1002/cdt3.38",
"ISSN": [
"2589-0514",
"2589-0514"
],
"URL": "http://dx.doi.org/10.1002/cdt3.38",
"alternative-id": [
"10.1002/cdt3.38"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2022-04-14"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2022-06-07"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2022-06-22"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-4850-094X",
"affiliation": [
{
"name": "Department of Radiation Oncology Icahn School of Medicine at Mount Sinai New York New York USA"
}
],
"authenticated-orcid": false,
"family": "Lehrer",
"given": "Steven",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Severn Health Solutions Severna Park Maryland USA"
}
],
"family": "Rheinstein",
"given": "Peter H.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cui",
"given": "Yi",
"sequence": "additional"
}
],
"container-title": "Chronic Diseases and Translational Medicine",
"container-title-short": "Chronic Diseases and Translational Medicine",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2022,
6,
22
]
],
"date-time": "2022-06-22T15:53:11Z",
"timestamp": 1655913191000
},
"deposited": {
"date-parts": [
[
2022,
6,
22
]
],
"date-time": "2022-06-22T15:53:17Z",
"timestamp": 1655913197000
},
"indexed": {
"date-parts": [
[
2022,
6,
24
]
],
"date-time": "2022-06-24T00:12:14Z",
"timestamp": 1656029534088
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
6,
22
]
]
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
6,
22
]
],
"date-time": "2022-06-22T00:00:00Z",
"timestamp": 1655856000000
}
},
{
"URL": "http://doi.wiley.com/10.1002/tdm_license_1.1",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
6,
22
]
],
"date-time": "2022-06-22T00:00:00Z",
"timestamp": 1655856000000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/cdt3.38",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/full-xml/10.1002/cdt3.38",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/cdt3.38",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"prefix": "10.1002",
"published": {
"date-parts": [
[
2022,
6,
22
]
]
},
"published-online": {
"date-parts": [
[
2022,
6,
22
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.1001/jama.2011.1961",
"doi-asserted-by": "publisher",
"key": "e_1_2_7_2_1"
},
{
"DOI": "10.1093/jnci/djz241",
"doi-asserted-by": "publisher",
"key": "e_1_2_7_3_1"
},
{
"DOI": "10.1016/S0140-6736(13)61752-3",
"doi-asserted-by": "publisher",
"key": "e_1_2_7_4_1"
},
{
"DOI": "10.1093/gerona/glaa183",
"doi-asserted-by": "publisher",
"key": "e_1_2_7_5_1"
},
{
"author": "Zhu A",
"first-page": "2813",
"key": "e_1_2_7_6_1",
"volume-title": "The UK Biobank Data Parser: a tool with built in and customizable filters for brain studies",
"year": "2019"
},
{
"DOI": "10.1016/S2213-2600(20)30239-3",
"doi-asserted-by": "publisher",
"key": "e_1_2_7_7_1"
},
{
"DOI": "10.1136/thoraxjnl-2020-216422",
"doi-asserted-by": "publisher",
"key": "e_1_2_7_8_1"
},
{
"DOI": "10.1007/5584_2016_71",
"article-title": "Damaging effects of cannabis use on the lungs",
"author": "Yayan J",
"doi-asserted-by": "crossref",
"first-page": "31",
"journal-title": "Adv Exp Med Biol",
"key": "e_1_2_7_9_1",
"volume": "952",
"year": "2016"
},
{
"DOI": "10.1186/s13722-021-00214-0",
"article-title": "Multiple clinical risks for cannabis users during the COVID‐19 pandemic",
"author": "Borgonhi EM",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "1",
"journal-title": "Addict Sci Clin Pract",
"key": "e_1_2_7_10_1",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1126/sciadv.abi6110",
"article-title": "Cannabidiol inhibits SARS‐CoV‐2 replication through induction of the host ER stress and innate immune responses",
"author": "Nguyen LC",
"doi-asserted-by": "crossref",
"first-page": "eabi6110",
"journal-title": "Sci Adv",
"key": "e_1_2_7_11_1",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1016/j.bbi.2020.04.079",
"doi-asserted-by": "publisher",
"key": "e_1_2_7_12_1"
},
{
"DOI": "10.1038/s41598-021-81049-2",
"doi-asserted-by": "publisher",
"key": "e_1_2_7_13_1"
},
{
"article-title": "Quitting smoking among adults‐United States, 2001‐2010",
"author": "Centers for Disease Control and Prevention (CDC)",
"first-page": "1513",
"issue": "44",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "e_1_2_7_14_1",
"volume": "60",
"year": "2011"
},
{
"key": "e_1_2_7_15_1",
"unstructured": "American Cancer Society.2021. Health benefits of quitting smoking over time. Accessed 30 March 2021.https://www.cancer.org/healthy/stay-away-from-tobacco/benefits-of-quitting-smoking-over-time.html"
},
{
"key": "e_1_2_7_16_1",
"unstructured": "National Institute on Drug Abuse (NIDA).2021. What are marijuana's effects on lung health? Accessed March 30 2021.https://nida.nih.gov/publications/research-reports/marijuana/what-are-marijuanas-effects-lung-health"
}
],
"reference-count": 15,
"references-count": 15,
"relation": {},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1002/cdt3.38"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"title": "Association of cannabis with chronic obstructive pulmonary disease and COVID‐19 infection",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy"
}