The Influence of SARS-CoV-2 Infection on the Development of Selected Neurological Diseases
et al., International Journal of Molecular Sciences, doi:10.3390/ijms25168715, Aug 2024
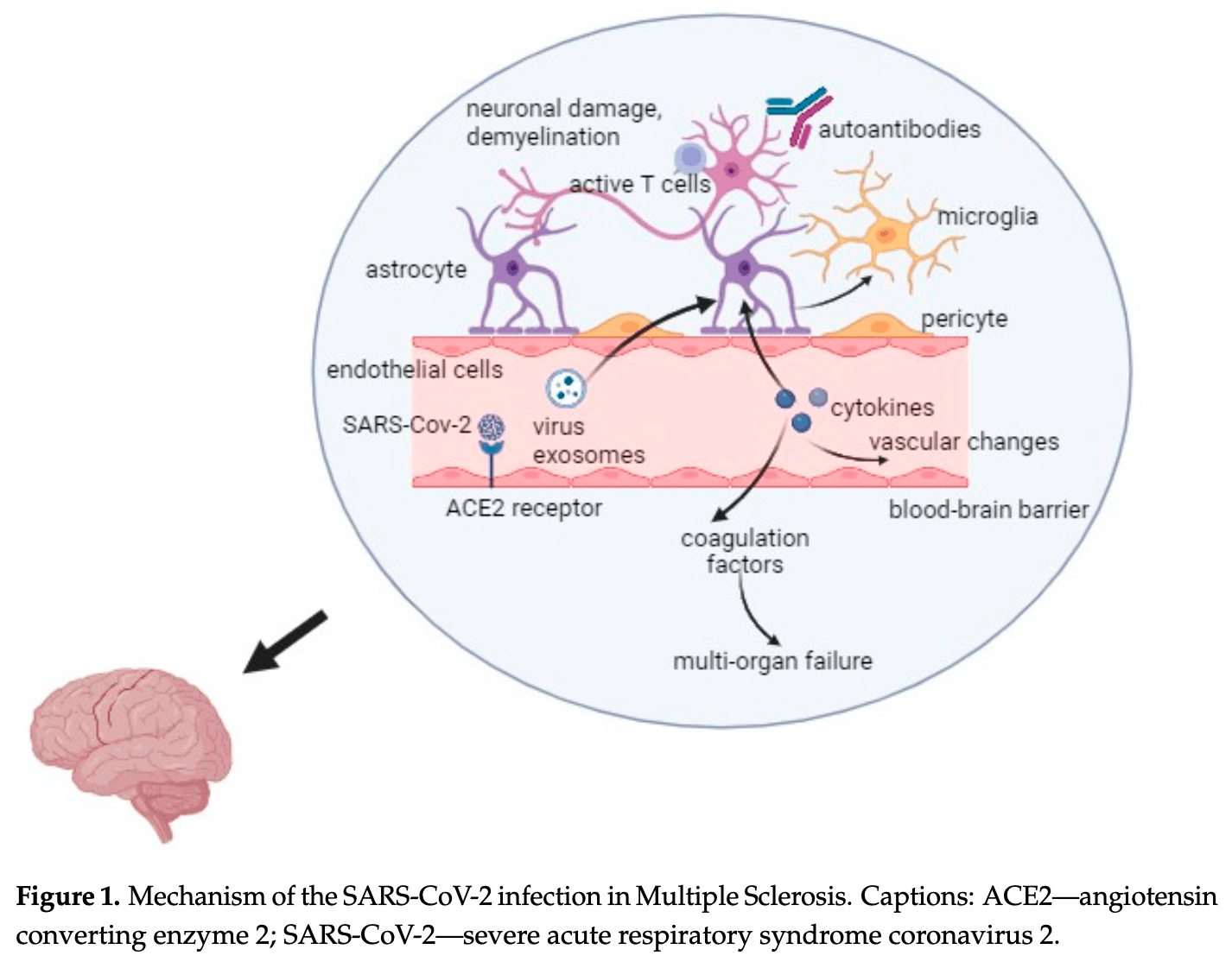
Review of the influence of SARS-CoV-2 infection on the development of selected neurological diseases, including multiple sclerosis (MS), ischemic stroke (IS), and Alzheimer's disease (AD). Authors report that SARS-CoV-2 causes activation of the NLRP3 inflammasome and production of interferons and neurotoxic cytokines that harm myelin sheaths, leading to synthesis of autoantibodies that attack glial cells and neurons, contributing to MS onset. In individuals already suffering from MS, SARS-CoV-2 exacerbates the disease through inflammation and nerve cell destruction. The release of pro-inflammatory cytokines may contribute to increased blood clotting, leading to thrombosis and ischemic stroke. AD is characterized by severe inflammation and increased oxidative stress, both of which are exacerbated during SARS-CoV-2 infection. Authors note that the virus enters cells more easily when the ACE2 receptor, already elevated in AD, and the ApoE ε4 allele are present, worsening the disease and increasing mortality in AD patients. Authors also report that mitochondrial dysfunction caused by SARS-CoV-2 infection contributes to the development of neurodegenerative diseases.
Kryńska et al., 9 Aug 2024, peer-reviewed, 6 authors.
Contact: monika.gudowska-sawczuk@umb.edu.pl (corresponding author), barbara.mroczko@umb.edu.pl, monika.zajkowska@umb.edu.pl.
The Influence of SARS-CoV-2 Infection on the Development of Selected Neurological Diseases
International Journal of Molecular Sciences, doi:10.3390/ijms25168715
In 2024, over 775 million cases of COVID-19 were recorded, including approximately 7 million deaths, indicating its widespread and dangerous nature. The disease is caused by the SARS-CoV-2 virus, which can manifest a wide spectrum of symptoms, from mild infection to respiratory failure and even death. Neurological symptoms, such as headaches, confusion, and impaired consciousness, have also been reported in some COVID-19 patients. These observations suggest the potential of SARS-CoV-2 to invade the central nervous system and induce neuroinflammation during infection. This review specifically explores the relationship between SARS-CoV-2 infection and selected neurological diseases such as multiple sclerosis (MS), ischemic stroke (IS), and Alzheimer's disease (AD). It has been observed that the SARS-CoV-2 virus increases the production of cytokines whose action can cause the destruction of the myelin sheaths of nerve cells. Subsequently, the body may synthesize autoantibodies that attack nerve cells, resulting in damage to the brain's anatomical elements, potentially contributing to the onset of multiple sclerosis. Additionally, SARS-CoV-2 exacerbates inflammation, worsening the clinical condition in individuals already suffering from MS. Moreover, the secretion of pro-inflammatory cytokines may lead to an escalation in blood clot formation, which can result in thrombosis, obstructing blood flow to the brain and precipitating an ischemic stroke. AD is characterized by intense inflammation and heightened oxidative stress, both of which are exacerbated during SARS-CoV-2 infection. It has been observed that the SARS-CoV-2 demonstrates enhanced cell entry in the presence of both the ACE2 receptor, which is already elevated in AD and the ApoE ε4 allele. Consequently, the condition worsens and progresses more rapidly, increasing the mortality rate among AD patients. The above information underscores the numerous connections between SARS-CoV-2 infection and neurological diseases.
Conflicts of Interest: The authors declare no conflict of interest.
References
Adil, Rahman, Whitelaw, Jain, Al-Taan et al., SARS-CoV-2 and the pandemic of COVID-19, Postgrad. Med. J, doi:10.1136/postgradmedj-2020-138386
Ahmad, Rathore, Neurological manifestations and complications of COVID-19: A literature review, J. Clin. Neurosci, doi:10.1016/j.jocn.2020.05.017
Alam, Czajkowsky, SARS-CoV-2 infection and oxidative stress: Pathophysiological insight into thrombosis and therapeutic opportunities, Cytokine Growth Factor Rev, doi:10.1016/j.cytogfr.2021.11.001
Andersen, Rambaut, Lipkin, Holmes, Garry, The proximal origin of SARS-CoV-2, Nat. Med, doi:10.1038/s41591-020-0820-9
Atkins, Masoli, Delgado, Pilling, Kuo et al., Preexisting Comorbidities Predicting Severe COVID-19 in Older Adults in the UK Biobank Community Cohort, J. Gerontol. Ser. A, doi:10.1093/gerona/glaa183
Axisa, Hafler, Multiple sclerosis: Genetics, biomarkers, treatments, Curr. Opin. Neurol, doi:10.1097/WCO.0000000000000319
Bahouth, Venkatesan, Acute Viral Illnesses and Ischemic Stroke: Pathophysiological Considerations in the Era of the COVID-19 Pandemic, Stroke, doi:10.1161/STROKEAHA.120.030630
Baranova, Cao, Zhang, Causal effect of COVID-19 on Alzheimer's disease: A Mendelian randomization study, J. Med. Virol, doi:10.1002/jmv.28107
Bartas, Volná, Beaudoin, Poulsen, Červe Ň et al., Unheeded SARS-CoV-2 proteins? A deep look into negative-sense RNA, Brief Bioinform, doi:10.1093/bib/bbac045
Barthels, Das, Current advances in ischemic stroke research and therapies, Biochim. Biophys. Acta Mol. Basis Dis, doi:10.1016/j.bbadis.2018.09.012
Bazylewicz, Gudowska-Sawczuk, Mroczko, Kochanowicz, Kułakowska, COVID-19: The Course, Vaccination and Immune Response in People with Multiple Sclerosis: Systematic Review, Int. J. Mol. Sci, doi:10.3390/ijms24119231
Bellucci, Rinaldi, Buscarinu, Reniè, Bigi et al., Multiple Sclerosis and SARS-CoV-2: Has the Interplay Started?, Front. Immunol, doi:10.3389/fimmu.2021.755333
Bianchetti, Rozzini, Guerini, Boffelli, Ranieri et al., Clinical Presentation of COVID19 in Dementia Patients, J. Nutr. Health Aging, doi:10.1007/s12603-020-1389-1
Bianchi, Borsetti, Ciccozzi, Pascarella, SARS-Cov-2 ORF3a: Mutability and function, Int. J. Biol. Macromol, doi:10.1016/j.ijbiomac.2020.12.142
Bostancıklıo Glu, Temporal Correlation Between Neurological and Gastrointestinal Symptoms of SARS-CoV-2, Inflamm. Bowel Dis, doi:10.1093/ibd/izaa131
Brola, Wilski, Neurological consequences of COVID-19, Pharmacol. Rep, doi:10.1007/s43440-022-00424-6
Capozzi, Riitano, Recalchi, Manganelli, Longo et al., Antiphospholipid antibodies in patients with stroke during COVID-19: A role in the signaling pathway leading to platelet activation, Front. Immunol, doi:10.3389/fimmu.2023.1129201
Cavezzi, Troiani, Corrao, COVID-19: Hemoglobin, iron, and hypoxia beyond inflammation. A narrative review, Clin. Pract, doi:10.4081/cp.2020.1271
Cecchini, Cecchini, SARS-CoV-2 infection pathogenesis is related to oxidative stress as a response to aggression, Med. Hypotheses, doi:10.1016/j.mehy.2020.110102
Chavhan, Wanjari, Kumar, Acharya, Rathod et al., A Comprehensive Review on Navigating the Neurological Landscape of COVID-19: Insights into Etiopathogenesis and Clinical Management, Cureus, doi:10.7759/cureus.60079
Chugh, Acute Ischemic Stroke: Management Approach, Indian J. Crit. Care Med, doi:10.5005/jp-journals-10071-23192
Cotsapas, Mitrovic, Hafler, Multiple sclerosis, Handb. Clin. Neurol, doi:10.1016/B978-0-444-64076-5.00046-6
Cui, Li, Shi, Origin and evolution of pathogenic coronaviruses, Nat. Rev. Microbiol, doi:10.1038/s41579-018-0118-9
Ding, Shults, Gychka, Harris, Suzuki, Protein Expression of Angiotensin-Converting Enzyme 2 (ACE2) is Upregulated in Brains with Alzheimer's Disease, Int. J. Mol. Sci, doi:10.3390/ijms22041687
Doshi, Chataway, Multiple sclerosis, a treatable disease, Clin. Med, doi:10.7861/clinmedicine.16-6-s53
Drouet, Fifre, Pinçon-Raymond, Vandekerckhove, Rosseneu et al., ApoE protects cortical neurones against neurotoxicity induced by the non-fibrillar C-terminal domain of the amyloid-beta peptide, J. Neurochem, doi:10.1046/j.1471-4159.2001.00047.x
Ekker, Verhoeven, Schellekens, Boot, Van Alebeek et al., Risk Factors and Causes of Ischemic Stroke in 1322 Young Adults, Stroke, doi:10.1161/STROKEAHA.122.040524
Farooqui, Farooqui, Sun, Lin, Teh et al., Blood Lipid Changes, and Thrombosis, Biomedicines, doi:10.3390/biomedicines11041181
Fernandes De Souza, Fonseca, Sartori, COVID-19 and Multiple Sclerosis: A Complex Relationship Possibly Aggravated by Low Vitamin D Levels, Cells, doi:10.3390/cells12050684
Finsterer, Scorza, Scorza, Fiorini, Ischemic stroke in 455 COVID-19 patients, Clinics, doi:10.1016/j.clinsp.2022.100012
Gain, Song, Angtuaco, Satta, Kelesidis, The role of oxidative stress in the pathogenesis of infections with coronaviruses, Front. Microbiol, doi:10.3389/fmicb.2022.1111930
Gamblin, King, Kuret, Berry, Binder, Oxidative regulation of fatty acid-induced tau polymerization, Biochemistry, doi:10.1021/bi001876l
Garg, Smith, An update on immunopathogenesis, diagnosis, and treatment of multiple sclerosis, Brain Behav, doi:10.1002/brb3.362
Goeijenbier, Van Wissen, Van De Weg, Jong, Gerdes et al., Review: Viral infections and mechanisms of thrombosis and bleeding, J. Med. Virol, doi:10.1002/jmv.23354
Grau, Urbanek, Palm, Common infections and the risk of stroke, Nat. Rev. Neurol, doi:10.1038/nrneurol.2010.163
Gudowska-Sawczuk, Mroczko, Free Light Chains as a Novel Diagnostic Biomarker of Immune System Abnormalities in Multiple Sclerosis and HIV Infection, Biomed. Res. Int, doi:10.1155/2019/8382132
Guo, Cao, Hong, Tan, Chen et al., The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak-An update on the status, Mil. Med. Res, doi:10.1186/s40779-020-00240-0
Guo, Fan, Chen, Wu, Zhang et al., Cardiovascular Implications of Fatal Outcomes of Patients with Coronavirus Disease 2019 (COVID-19), Correction in JAMA Cardiol, doi:10.1001/jamacardio.2020.1017
Gupta, Sahu, Prabhakar, Chatterjee, Tyagi et al., Activation of NLRP3 inflammasome complex potentiates venous thrombosis in response to hypoxia, Proc. Natl. Acad. Sci, doi:10.1073/pnas.1620458114
Hamilton, Van Remmen, Drake, Yang, Guo et al., Does oxidative damage to DNA increase with age?, Proc. Natl. Acad. Sci, doi:10.1073/pnas.171202698
Hamming, Timens, Bulthuis, Lely, Navis et al., Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis, J. Pathol, doi:10.1002/path.1570
Harb, Chen, Chase, Natarajan, Noble, Clinical Features and Outcomes of Patients with Dementia Compared to an Aging Cohort Hospitalized During the Initial New York City COVID-19 Wave, J. Alzheimer's Dis, doi:10.3233/JAD-210050
Hasegawa, Yamaguchi, Omata, Gejyo, Naiki, Interaction between A beta(1-42) and A beta(1-40) in Alzheimer's beta-amyloid fibril formation in vitro, Biochemistry, doi:10.1021/bi991161m
Hauser, Narayanaswami, Ryan, Apolipoprotein, From lipid transport to neurobiology, Prog. Lipid Res, doi:10.1016/j.plipres.2010.09.001
Hellner, Walther, Schubert, Albrecht, Angiotensin-(1-7) enhances LTP in the hippocampus through the G-proteincoupled receptor Mas, Mol. Cell Neurosci, doi:10.1016/j.mcn.2005.03.012
Heneka, Kummer, Stutz, Delekate, Schwartz et al., NLRP3 is activated in Alzheimer's disease and contributes to pathology in APP/PS1 mice, Nature, doi:10.1038/nature11729
Hingorani, Bhadola, Cervantes-Arslanian, COVID-19 and the brain, Trends Cardiovasc. Med, doi:10.1016/j.tcm.2022.04.004
Houen, Trier, Frederiksen, Epstein-Barr, Virus and Multiple Sclerosis, Front. Immunol, doi:10.3389/fimmu.2020.587078
Iyer, Raghavendra, Nooraine, Jaychandran, COVID-19 outcomes in persons with multiple sclerosis treated with rituximab, Mult. Scler. Relat. Disord, doi:10.1016/j.msard.2021.103371
Jiang, Zhang, Zhou, Zhu, Tian et al., Angiotensin-(1-7) is Reduced and Inversely Correlates with Tau Hyperphosphorylation in Animal Models of Alzheimer's Disease, Mol. Neurobiol, doi:10.1007/s12035-015-9260-9
Jose, Manuel, COVID-19 cytokine storm: The interplay between inflammation and coagulation, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30216-2
Kangro, Wolberg, Flick, Fibrinogen, Fibrin, and Fibrin Degradation Products in COVID-19, Curr. Drug Targets, doi:10.2174/1389450123666220826162900
Kim, Lee, Kim, Serum tumour necrosis factor-α and interleukin-6 levels in Alzheimer's disease and mild cognitive impairment, Psychogeriatrics, doi:10.1111/psyg.12218
Kim, Onstead, Randle, Price, Smithson et al., Abeta40 inhibits amyloid deposition in vivo, J. Neurosci, doi:10.1523/JNEUROSCI.4849-06.2007
Kinney, Bemiller, Murtishaw, Leisgang, Salazar et al., Inflammation as a central mechanism in Alzheimer's disease, Alzheimer's Dement, doi:10.1016/j.trci.2018.06.014
Klein, Mechanisms of coronavirus infectious disease 2019-related neurologic diseases, Curr. Opin. Neurol, doi:10.1097/WCO.0000000000001049
Klineova, Lublin, Clinical Course of Multiple Sclerosis, Cold Spring Harb. Perspect. Med, doi:10.1101/cshperspect.a028928
Korwek, Trotter, Ladu, Sullivan, Weeber, ApoE isoform-dependent changes in hippocampal synaptic function, Mol. Neurodegener, doi:10.1186/1750-1326-4-21
Kozlov, Ivanova, Grechko, Wu, Starodubova et al., Involvement of Oxidative Stress and the Innate Immune System in SARS-CoV-2 Infection, Diseases, doi:10.3390/diseases9010017
Kuo, Pilling, Atkins, Masoli, Delgado et al., APOE e4 Genotype Predicts Severe COVID-19 in the UK Biobank Community Cohort, J. Gerontol. A Biol. Sci. Med. Sci, doi:10.1093/gerona/glaa131
Law, Cheung, Ng, Sia, Chan et al., Chemokine up-regulation in SARS-coronavirus-infected, monocyte-derived human dendritic cells, Blood, doi:10.1182/blood-2004-10-4166
Lazaroni, Raslan, Fontes, De Oliveira, Bader et al., Angiotensin-(1-7)/Mas axis integrity is required for the expression of object recognition memory, Neurobiol. Learn Mem, doi:10.1016/j.nlm.2011.10.003
Levine, Leonard, Blauwendraat, Iwaki, Johnson et al., Virus exposure and neurodegenerative disease risk across national biobanks, Neuron, doi:10.1016/j.neuron.2022.12.029
Li, Calingasan, Yu, Mauck, Toidze et al., Increased plaque burden in brains of APP mutant MnSOD heterozygous knockout mice, J. Neurochem, doi:10.1111/j.1471-4159.2004.02455.x
Li, Hearn, Bennett, The role of microbial infection in the pathogenesis of Alzheimer's disease and the opportunity for protection by anti-microbial peptides, Crit. Rev. Microbiol, doi:10.1080/1040841X.2021.1876630
Li, Li, Wang, Zhou, Chang et al., Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study, Stroke Vasc. Neurol, doi:10.1136/svn-2020-000431
Li, Liu, Lin, Shang, COVID-19 and risk of neurodegenerative disorders: A Mendelian randomization study, Transl. Psychiatry, doi:10.1038/s41398-022-02052-3
Liang, Zhang, Wu, Chen, Wang, The Role of NLRP3 Inflammasome in Alzheimer's Disease and Potential Therapeutic Targets, Front. Pharmacol, doi:10.3389/fphar.2022.845185
Lima, Aloizou, Siokas, Bakirtzis, Liampas et al., Coronaviruses and their relationship with multiple sclerosis: Is the prevalence of multiple sclerosis going to increase after the COVID-19 pandemia?, Rev. Neurosci, doi:10.1515/revneuro-2021-0148
Lin, Asfour, Sewell, Hooe, Pryce et al., Neurological issues in children with COVID-19, Neurosci. Lett, doi:10.1016/j.neulet.2020.135567
Lindsberg, Grau, Inflammation and infections as risk factors for ischemic stroke, Stroke, doi:10.1161/01.STR.0000089015.51603.CC
Liu, Liu, Miura, Tanabe, Maeda et al., Conversion of Aβ43 to Aβ40 by the successive action of angiotensin-converting enzyme 2 and angiotensin-converting enzyme, J. Neurosci. Res, doi:10.1002/jnr.23404
Lotz, Blackhurst, Reagin, Funk, Microbial Infections Are a Risk Factor for Neurodegenerative Diseases, Front. Cell Neurosci, doi:10.3389/fncel.2021.691136
Lozano, Naghavi, Foreman, Lim, Shibuya et al., Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010, Correction in Lancet, doi:10.1016/S0140-6736(12)61728-0
Margoni, Preziosa, Filippi, Rocca, Anti-CD20 therapies for multiple sclerosis: Current status and future perspectives, J. Neurol, doi:10.1007/s00415-021-10744-x
Martín-Jiménez, Muñoz-García, Seoane, Roca-Rodríguez, García-Reyne et al., Cognitive Impairment Is a Common Comorbidity in Deceased COVID-19 Patients: A Hospital-Based Retrospective Cohort Study, J. Alzheimer's Dis, doi:10.3233/JAD-200937
Matsuoka, Picciano, La Francois, Duff, Fibrillar beta-amyloid evokes oxidative damage in a transgenic mouse model of Alzheimer's disease, Neuroscience, doi:10.1016/S0306-4522(01)00115-4
Melov, Adlard, Morten, Johnson, Golden et al., Mitochondrial oxidative stress causes hyperphosphorylation of tau, PLoS ONE, doi:10.1371/journal.pone.0000536
Merki-Feld, Aegidius, Bitzer, Canonico, Kurth et al., Hormonal contraceptives and risk of ischemic stroke in women with migraine: A consensus statement from the European Headache Federation (EHF) and the European Society of Contraception and Reproductive Health (ESC), Correction in J. Headache Pain, doi:10.1186/s10194-017-0815-1
Merkler, Parikh, Mir, Gupta, Kamel et al., Risk of Ischemic Stroke in Patients with Coronavirus Disease 2019 (COVID-19) vs. Patients with Influenza, JAMA Neurol, doi:10.1001/jamaneurol.2020.2730
Messinis, Papathanasopoulos, Kosmidis, Nasios, Kambanaros, Neuropsychological Features of Multiple Sclerosis: Impact and Rehabilitation, Behav. Neurol, doi:10.1155/2018/4831647
Motaghinejad, Gholami, Possible Neurological and Mental Outcomes of COVID-19 Infection: A Hypothetical Role of ACE-2\Mas\BDNF Signaling Pathway, Int. J. Prev. Med, doi:10.4103/ijpvm.IJPVM_114_20
Motaghinejad, Motevalian, Falak, Heidari, Sharzad et al., Neuroprotective effects of various doses of topiramate against methylphenidate-induced oxidative stress and inflammation in isolated rat amygdala: The possible role of CREB/BDNF signaling pathway, J. Neural Transm, doi:10.1007/s00702-016-1619-1
Motolese, Rossi, Albergo, Stelitano, Villanova et al., The Psychological Impact of COVID-19 Pandemic on People with Multiple Sclerosis, Front. Neurol, doi:10.3389/fneur.2020.580507
Murphy, Werring, Stroke: Causes and clinical features, Medicine, doi:10.1016/j.mpmed.2020.06.002
Muñoz, Ardiles, Pérez-Espinosa, Núñez-Espinosa, Paula-Lima et al., Redox modifications in synaptic components as biomarkers of cognitive status, in brain aging and disease, Mech. Ageing Dev, doi:10.1016/j.mad.2020.111250
Muñoz-Jurado, Escribano, Caballero-Villarraso, Galván, Agüera et al., Melatonin and multiple sclerosis: Antioxidant, anti-inflammatory and immunomodulator mechanism of action, Inflammopharmacology, doi:10.1007/s10787-022-01011-0
Nichols, Szoeke, Vollset, Abbasi, Abd-Allah et al., regional, and national burden of Alzheimer's disease and other dementias, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016, Lancet Neurol, doi:10.1016/S1474-4422(18)30403-4
O'donnell, Chin, Rangarajan, Xavier, Liu et al., Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): A case-control study, Lancet, doi:10.1016/S0140-6736(16)30506-2
Ousseiran, Fares, Chamoun, Neurological manifestations of COVID-19: A systematic review and detailed comprehension, Int. J. Neurosci, doi:10.1080/00207454.2021.1973000
Pal, Berhanu, Desalegn, Kandi, Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2): An Update, Cureus, doi:10.7759/cureus.7423
Park, Song, Oh, Dementia Risk among Coronavirus Disease Survivors: A Nationwide Cohort Study in South Korea, J. Pers. Med, doi:10.3390/jpm11101015
Patterson, Alzheimer's Disease International
Phillips, De Oliveira, Brain renin angiotensin in disease, J. Mol. Med, doi:10.1007/s00109-008-0331-5
Piekut, Hurła, Banaszek, Szejn, Dorszewska et al., Infectious agents and Alzheimer's disease, J. Integr. Neurosci, doi:10.31083/j.jin2102073
Pozzilli, Pugliatti, Vermersch, Grigoriadis, Alkhawajah et al., Diagnosis and treatment of progressive multiple sclerosis: A position paper, Eur. J. Neurol, doi:10.1111/ene.15593
Pu, Wang, Zhang, Zhao, Jiang et al., Projected Global Trends in Ischemic Stroke Incidence, Deaths and Disability-Adjusted Life Years From 2020 to 2030, Correction in Stroke, doi:10.1161/STROKEAHA.122.040073
Ragab, Salah Eldin, Taeimah, Khattab, Salem, The COVID-19 Cytokine Storm; What We Know So Far, Front. Immunol, doi:10.3389/fimmu.2020.01446
Ramzy, Montrief, Gottlieb, Brady, Singh et al., COVID-19 cardiac arrest management: A review for emergency clinicians, Am. J. Emerg. Med, doi:10.1016/j.ajem.2020.08.011
Rauf, Shariati, Khalil, Bawazeer, Heydari et al., an overview of biochemical and clinical properties, Steroids, doi:10.1016/j.steroids.2020.108661
Reghunathan, Jayapal, Hsu, Chng, Tai et al., Expression profile of immune response genes in patients with Severe Acute Respiratory Syndrome, BMC Immunol, doi:10.1186/1471-2172-6-2
Ren, Shu, Wu, Mu, Wang et al., The ORF3a protein of SARS-CoV-2 induces apoptosis in cells, Cell Mol. Immunol, doi:10.1038/s41423-020-0485-9
Rousseau, Bhaduri-Mcintosh, Inflammation and Epstein-Barr Virus at the Crossroads of Multiple Sclerosis and Post-Acute Sequelae of COVID-19 Infection, Viruses, doi:10.3390/v15040949
Rubio-Perez, Morillas-Ruiz, A review: Inflammatory process in Alzheimer's disease, role of cytokines, Sci. World J, doi:10.1100/2012/756357
Rudnicka-Dro Żak, Dro Żak, Mizerski, Zaborowski, Ślusarska et al., Links between COVID-19 and Alzheimer's Disease-What Do We Already Know?, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph20032146
Ruiz, Vigne, Pot, Resolution of inflammation during multiple sclerosis, Semin. Immunopathol, doi:10.1007/s00281-019-00765-0
Sacco, Kasner, Broderick, Caplan, Connors et al., An updated definition of stroke for the 21st century: A statement for healthcare professionals from the American Heart Association/American Stroke Association, Correction in Stroke, doi:10.1161/STR.0b013e318296aeca
Sacco, on behalf of the European Headache Federation (EHF) and the European Society of Contraception and Reproductive Health
Sadeghmousavi, Rezaei, COVID-19 and Multiple Sclerosis: Predisposition and Precautions in Treatment SN, Compr. Clin. Med, doi:10.1007/s42399-020-00504-9
Satheesh, Salloum-Asfar, Abdulla, The Potential Role of COVID-19 in the Pathogenesis of Multiple Sclerosis-A Preliminary Report, Viruses, doi:10.3390/v13102091
Schiavetti, Carmisciano, Ponzano, Cordioli, Cocco et al., Signs and symptoms of COVID-19 in patients with multiple sclerosis, Eur. J. Neurol, doi:10.1111/ene.15554
Smeeth, Thomas, Hall, Hubbard, Farrington et al., Risk of myocardial infarction and stroke after acute infection or vaccination, N. Engl. J. Med, doi:10.1056/NEJMoa041747
Song, Fan, Tang, Luo, Liu et al., The effects of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on ischemic stroke and the possible underlying mechanisms, Int. J. Neurosci, doi:10.1080/00207454.2021.1897588
Stancu, Cremers, Vanrusselt, Couturier, Vanoosthuyse et al., Aggregated Tau activates NLRP3-ASC inflammasome exacerbating exogenously seeded and non-exogenously seeded Tau pathology in vivo, Acta Neuropathol, doi:10.1007/s00401-018-01957-y
Stoll, Bendszus, Inflammation and atherosclerosis: Novel insights into plaque formation and destabilization, Stroke, doi:10.1161/01.STR.0000226901.34927.10
Tan, Goh, Leow, Tambyah, Ang et al., COVID-19 and ischemic stroke: A systematic review and meta-summary of the literature, J. Thromb. Thrombolysis, doi:10.1007/s11239-020-02228-y
Tejera, Mercan, Sanchez-Caro, Hanan, Greenberg et al., Systemic inflammation impairs microglial Aβ clearance through NLRP3 inflammasome, EMBO J, doi:10.15252/embj.2018101064
Tomassini, Sinclair, Sawlani, Overell, Pearson et al., Diagnosis and management of multiple sclerosis: MRI in clinical practice, J. Neurol, doi:10.1007/s00415-020-09930-0
Trimaille, Bonnet, COVID-19 and venous thromboembolic disease (COVID-19 and venous thromboembolism), Ann. Cardiol. Angeiol, doi:10.1016/j.ancard.2020.09.027
Tsao, Aday, Almarzooq, Anderson, Arora et al., Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association, Correction in Circulation, doi:10.1161/CIR.0000000000001123
Verghese, Castellano, Holtzman, Apolipoprotein E in Alzheimer's disease and other neurological disorders, Lancet Neurol, doi:10.1016/S1474-4422(10)70325-2
Vogrig, Gigli, Bnà, Morassi, Stroke in patients with COVID-19: Clinical and neuroimaging characteristics, Neurosci. Lett, doi:10.1016/j.neulet.2020.135564
Vrillon, Mhanna, Aveneau, Lebozec, Grosset et al., COVID-19 in adults with dementia: Clinical features and risk factors of mortality-A clinical cohort study on 125 patients, Alzheimer's Res. Ther, doi:10.1186/s13195-021-00820-9
Wang, Cui, Leng, Wang, Peng, Cognitive Impairment in the Post-Acute Phases of COVID-19 and Mechanisms: An Introduction and Narrative Review, J. Alzheimer's Dis. Rep, doi:10.3233/ADR-230172
Wang, Iwanami, Min, Tsukuda, Nakaoka et al., Deficiency of angiotensin-converting enzyme 2 causes deterioration of cognitive function, NPJ Aging Mech. Dis, doi:10.1038/npjamd.2016.24
Wang, Kream, Stefano, Long-Term Respiratory and Neurological Sequelae of COVID-19, Med. Sci. Monit, doi:10.12659/MSM.928996
Wang, Qin, Zhang, Chen, Possible immunity, inflammation, and oxidative stress mechanisms of Alzheimer's disease in COVID-19 patients, Clin. Neurol. Neurosurg, doi:10.1016/j.clineuro.2020.106414
Wang, Yao, Ma, Ping, Fan et al., A single-cell transcriptomic landscape of the lungs of patients with COVID-19, Nat. Cell Biol, doi:10.1038/s41556-021-00796-6
Wang, Yuan, Pavel, Jablonski, Jablonski et al., The role of high cholesterol in age-related COVID19 lethality, bioRxiv, doi:10.1101/2020.05.09.086249
Weatherley, Araujo, Dando, Jenner, Could Mathematics be the Key to Unlocking the Mysteries of Multiple Sclerosis?, Bull. Math. Biol, doi:10.1007/s11538-023-01181-0
Who, WHO Coronavirus (COVID-19) Dashboard
Winblad, Amouyel, Andrieu, Ballard, Brayne et al., Defeating Alzheimer's disease and other dementias: A priority for European science and society, Lancet Neurol, doi:10.1016/S1474-4422(16)00062-4
Wouk, Rechenchoski, Rodrigues, Ribelato, Faccin-Galhardi, Viral infections and their relationship to neurological disorders, Arch. Virol, doi:10.1007/s00705-021-04959-6
Xia, Wang, Zheng, COVID-19 and Alzheimer's disease: How one crisis worsens the other, Transl. Neurodegener, doi:10.1186/s40035-021-00237-2
Yan, Wang, Abeta40 protects non-toxic Abeta42 monomer from aggregation, J. Mol. Biol, doi:10.1016/j.jmb.2007.04.014
Yeo, Siew, Gulam, Tye, Aw et al., COVID-19 infection after SARS-CoV-2 mRNA vaccination in Multiple Sclerosis, AQP4-antibody NMOSD and MOGAD patients during the Omicron subvariant BA.1/2 wave in Singapore, J. Neurol, doi:10.1007/s00415-023-11692-4
Zafar, Al-Khamis, Al-Bakr, Alsulaiman, Msmar, Risk factors and subtypes of acute ischemic stroke. A study at King Fahd Hospital of the University, Neurosciences, doi:10.17712/nsj.2016.3.20150731
Zanza, Romenskaya, Manetti, Franceschi, La Russa et al., Cytokine Storm in COVID-19: Immunopathogenesis and Therapy, Medicina, doi:10.3390/medicina58020144
Zhang, Tian, Wang, Ma, Tan et al., The Epidemiology of Alzheimer's Disease Modifiable Risk Factors and Prevention, J. Prev. Alzheimer's Dis, doi:10.14283/jpad.2021.15
Zhang, Xiao, Zhang, Xia, Cao et al., Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19, N. Engl. J. Med, doi:10.1056/NEJMc2007575
Zhang, Zhang, Wang, Chen, Zhao et al., COVID-19 and ischemic stroke: Mechanisms of hypercoagulability (Review), Int. J. Mol. Med, doi:10.3892/ijmm.2021.4854
Zhao, Li, Lukiw, Ubiquity of the SARS-CoV-2 receptor ACE2 and upregulation in limbic regions of Alzheimer's disease brain, Folia Neuropathol, doi:10.5114/fn.2021.109495
Zhao, Zhao, Oxidative stress and the pathogenesis of Alzheimer's disease, Oxid. Med. Cell. Longev, doi:10.1155/2013/316523
Zhou, Yang, Wang, Hu, Zhang et al., A pneumonia outbreak associated with a new coronavirus of probable bat origin, Erratum in Nature, doi:10.1038/s41586-020-2012-7
Zmasek, Lefkowitz, Niewiadomska, Scheuermann, Genomic evolution of the Coronaviridae family, Virology, doi:10.1016/j.virol.2022.03.005
Zou, Liu, Watanabe, Hiraga, Liu et al., Aβ43 is the earliest-depositing Aβ species in APP transgenic mouse brain and is converted to Aβ41 by two active domains of ACE, Am. J. Pathol, doi:10.1016/j.ajpath.2013.01.053
Zubair, Mcalpine, Gardin, Farhadian, Kuruvilla et al., Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review, JAMA Neurol, doi:10.1001/jamaneurol.2020.2065
DOI record:
{
"DOI": "10.3390/ijms25168715",
"ISSN": [
"1422-0067"
],
"URL": "http://dx.doi.org/10.3390/ijms25168715",
"abstract": "<jats:p>In 2024, over 775 million cases of COVID-19 were recorded, including approximately 7 million deaths, indicating its widespread and dangerous nature. The disease is caused by the SARS-CoV-2 virus, which can manifest a wide spectrum of symptoms, from mild infection to respiratory failure and even death. Neurological symptoms, such as headaches, confusion, and impaired consciousness, have also been reported in some COVID-19 patients. These observations suggest the potential of SARS-CoV-2 to invade the central nervous system and induce neuroinflammation during infection. This review specifically explores the relationship between SARS-CoV-2 infection and selected neurological diseases such as multiple sclerosis (MS), ischemic stroke (IS), and Alzheimer’s disease (AD). It has been observed that the SARS-CoV-2 virus increases the production of cytokines whose action can cause the destruction of the myelin sheaths of nerve cells. Subsequently, the body may synthesize autoantibodies that attack nerve cells, resulting in damage to the brain’s anatomical elements, potentially contributing to the onset of multiple sclerosis. Additionally, SARS-CoV-2 exacerbates inflammation, worsening the clinical condition in individuals already suffering from MS. Moreover, the secretion of pro-inflammatory cytokines may lead to an escalation in blood clot formation, which can result in thrombosis, obstructing blood flow to the brain and precipitating an ischemic stroke. AD is characterized by intense inflammation and heightened oxidative stress, both of which are exacerbated during SARS-CoV-2 infection. It has been observed that the SARS-CoV-2 demonstrates enhanced cell entry in the presence of both the ACE2 receptor, which is already elevated in AD and the ApoE ε4 allele. Consequently, the condition worsens and progresses more rapidly, increasing the mortality rate among AD patients. The above information underscores the numerous connections between SARS-CoV-2 infection and neurological diseases.</jats:p>",
"alternative-id": [
"ijms25168715"
],
"author": [
{
"affiliation": [
{
"name": "Department of Biochemical Diagnostics, Medical University of Bialystok, Waszyngtona 15A St., 15-269 Bialystok, Poland"
}
],
"family": "Kryńska",
"given": "Klaudia",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Biochemical Diagnostics, Medical University of Bialystok, Waszyngtona 15A St., 15-269 Bialystok, Poland"
}
],
"family": "Kuliś",
"given": "Katarzyna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Biochemical Diagnostics, Medical University of Bialystok, Waszyngtona 15A St., 15-269 Bialystok, Poland"
}
],
"family": "Mazurek",
"given": "Wiktoria",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4854-7155",
"affiliation": [
{
"name": "Department of Biochemical Diagnostics, Medical University of Bialystok, Waszyngtona 15A St., 15-269 Bialystok, Poland"
}
],
"authenticated-orcid": false,
"family": "Gudowska-Sawczuk",
"given": "Monika",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5179-0722",
"affiliation": [
{
"name": "Department of Neurodegeneration Diagnostics, Medical University of Bialystok, Waszyngtona 15A St., 15-269 Bialystok, Poland"
}
],
"authenticated-orcid": false,
"family": "Zajkowska",
"given": "Monika",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4075-8479",
"affiliation": [
{
"name": "Department of Biochemical Diagnostics, Medical University of Bialystok, Waszyngtona 15A St., 15-269 Bialystok, Poland"
},
{
"name": "Department of Neurodegeneration Diagnostics, Medical University of Bialystok, Waszyngtona 15A St., 15-269 Bialystok, Poland"
}
],
"authenticated-orcid": false,
"family": "Mroczko",
"given": "Barbara",
"sequence": "additional"
}
],
"container-title": "International Journal of Molecular Sciences",
"container-title-short": "IJMS",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
8,
14
]
],
"date-time": "2024-08-14T07:46:36Z",
"timestamp": 1723621596000
},
"deposited": {
"date-parts": [
[
2024,
8,
14
]
],
"date-time": "2024-08-14T07:53:20Z",
"timestamp": 1723622000000
},
"funder": [
{
"award": [
"B.SUB.23.378"
],
"name": "Medical University of Bialystok, Poland"
}
],
"indexed": {
"date-parts": [
[
2024,
8,
15
]
],
"date-time": "2024-08-15T00:18:02Z",
"timestamp": 1723681082210
},
"is-referenced-by-count": 0,
"issue": "16",
"issued": {
"date-parts": [
[
2024,
8,
9
]
]
},
"journal-issue": {
"issue": "16",
"published-online": {
"date-parts": [
[
2024,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
8,
9
]
],
"date-time": "2024-08-09T00:00:00Z",
"timestamp": 1723161600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1422-0067/25/16/8715/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "8715",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
8,
9
]
]
},
"published-online": {
"date-parts": [
[
2024,
8,
9
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1038/s41579-018-0118-9",
"article-title": "Origin and evolution of pathogenic coronaviruses",
"author": "Cui",
"doi-asserted-by": "crossref",
"first-page": "181",
"journal-title": "Nat. Rev. Microbiol.",
"key": "ref_1",
"volume": "17",
"year": "2019"
},
{
"DOI": "10.1038/s41591-020-0820-9",
"article-title": "The proximal origin of SARS-CoV-2",
"author": "Andersen",
"doi-asserted-by": "crossref",
"first-page": "450",
"journal-title": "Nat. Med.",
"key": "ref_2",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1136/postgradmedj-2020-138386",
"article-title": "SARS-CoV-2 and the pandemic of COVID-19",
"author": "Adil",
"doi-asserted-by": "crossref",
"first-page": "110",
"journal-title": "Postgrad. Med. J.",
"key": "ref_3",
"volume": "97",
"year": "2021"
},
{
"key": "ref_4",
"unstructured": "WHO (2024, May 02). WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/."
},
{
"DOI": "10.1016/j.virol.2022.03.005",
"article-title": "Genomic evolution of the Coronaviridae family",
"author": "Zmasek",
"doi-asserted-by": "crossref",
"first-page": "123",
"journal-title": "Virology",
"key": "ref_5",
"volume": "570",
"year": "2022"
},
{
"article-title": "Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2): An Update",
"author": "Pal",
"first-page": "e7423",
"journal-title": "Cureus",
"key": "ref_6",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.ajem.2020.08.011",
"article-title": "COVID-19 cardiac arrest management: A review for emergency clinicians",
"author": "Ramzy",
"doi-asserted-by": "crossref",
"first-page": "2693",
"journal-title": "Am. J. Emerg. Med.",
"key": "ref_7",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.1080/00207454.2021.1973000",
"article-title": "Neurological manifestations of COVID-19: A systematic review and detailed comprehension",
"author": "Ousseiran",
"doi-asserted-by": "crossref",
"first-page": "754",
"journal-title": "Int. J. Neurosci.",
"key": "ref_8",
"volume": "133",
"year": "2023"
},
{
"DOI": "10.1016/j.neulet.2020.135567",
"article-title": "Neurological issues in children with COVID-19",
"author": "Lin",
"doi-asserted-by": "crossref",
"first-page": "135567",
"journal-title": "Neurosci. Lett.",
"key": "ref_9",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1016/j.tcm.2022.04.004",
"article-title": "COVID-19 and the brain",
"author": "Hingorani",
"doi-asserted-by": "crossref",
"first-page": "323",
"journal-title": "Trends Cardiovasc. Med.",
"key": "ref_10",
"volume": "32",
"year": "2022"
},
{
"DOI": "10.1097/WCO.0000000000001049",
"article-title": "Mechanisms of coronavirus infectious disease 2019-related neurologic diseases",
"author": "Klein",
"doi-asserted-by": "crossref",
"first-page": "392",
"journal-title": "Curr. Opin. Neurol.",
"key": "ref_11",
"volume": "35",
"year": "2022"
},
{
"article-title": "A Comprehensive Review on Navigating the Neurological Landscape of COVID-19: Insights into Etiopathogenesis and Clinical Management",
"author": "Chavhan",
"first-page": "e60079",
"journal-title": "Cureus",
"key": "ref_12",
"volume": "16",
"year": "2024"
},
{
"DOI": "10.3233/ADR-230172",
"article-title": "Cognitive Impairment in the Post-Acute Phases of COVID-19 and Mechanisms: An Introduction and Narrative Review",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "647",
"journal-title": "J. Alzheimer’s Dis. Rep.",
"key": "ref_13",
"volume": "8",
"year": "2024"
},
{
"DOI": "10.3390/ijms24119231",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Bazylewicz, M., Gudowska-Sawczuk, M., Mroczko, B., Kochanowicz, J., and Kułakowska, A. (2023). COVID-19: The Course, Vaccination and Immune Response in People with Multiple Sclerosis: Systematic Review. Int. J. Mol. Sci., 24."
},
{
"DOI": "10.7861/clinmedicine.16-6-s53",
"article-title": "Multiple sclerosis, a treatable disease",
"author": "Doshi",
"doi-asserted-by": "crossref",
"first-page": "s53",
"journal-title": "Clin. Med.",
"key": "ref_15",
"volume": "16",
"year": "2016"
},
{
"DOI": "10.1097/WCO.0000000000000319",
"article-title": "Multiple sclerosis: Genetics, biomarkers, treatments",
"author": "Axisa",
"doi-asserted-by": "crossref",
"first-page": "345",
"journal-title": "Curr. Opin. Neurol.",
"key": "ref_16",
"volume": "29",
"year": "2016"
},
{
"DOI": "10.1007/s00281-019-00765-0",
"article-title": "Resolution of inflammation during multiple sclerosis",
"author": "Ruiz",
"doi-asserted-by": "crossref",
"first-page": "711",
"journal-title": "Semin. Immunopathol.",
"key": "ref_17",
"volume": "41",
"year": "2019"
},
{
"DOI": "10.1016/B978-0-444-64076-5.00046-6",
"article-title": "Multiple sclerosis",
"author": "Cotsapas",
"doi-asserted-by": "crossref",
"first-page": "723",
"journal-title": "Handb. Clin. Neurol.",
"key": "ref_18",
"volume": "148",
"year": "2018"
},
{
"DOI": "10.1111/ene.15593",
"article-title": "Diagnosis and treatment of progressive multiple sclerosis: A position paper",
"author": "Pozzilli",
"doi-asserted-by": "crossref",
"first-page": "9",
"journal-title": "Eur. J. Neurol.",
"key": "ref_19",
"volume": "30",
"year": "2023"
},
{
"DOI": "10.1002/brb3.362",
"article-title": "An update on immunopathogenesis, diagnosis, and treatment of multiple sclerosis",
"author": "Garg",
"doi-asserted-by": "crossref",
"first-page": "e00362",
"journal-title": "Brain Behav.",
"key": "ref_20",
"volume": "5",
"year": "2015"
},
{
"DOI": "10.1155/2018/4831647",
"article-title": "Neuropsychological Features of Multiple Sclerosis: Impact and Rehabilitation",
"author": "Messinis",
"doi-asserted-by": "crossref",
"first-page": "4831647",
"journal-title": "Behav. Neurol.",
"key": "ref_21",
"volume": "2018",
"year": "2018"
},
{
"DOI": "10.1101/cshperspect.a028928",
"article-title": "Clinical Course of Multiple Sclerosis",
"author": "Klineova",
"doi-asserted-by": "crossref",
"first-page": "a028928",
"journal-title": "Cold Spring Harb. Perspect. Med.",
"key": "ref_22",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.1007/s00415-020-09930-0",
"article-title": "Diagnosis and management of multiple sclerosis: MRI in clinical practice",
"author": "Tomassini",
"doi-asserted-by": "crossref",
"first-page": "2917",
"journal-title": "J. Neurol.",
"key": "ref_23",
"volume": "267",
"year": "2020"
},
{
"DOI": "10.1155/2019/8382132",
"doi-asserted-by": "crossref",
"key": "ref_24",
"unstructured": "Gudowska-Sawczuk, M., and Mroczko, B. (2019). Free Light Chains as a Novel Diagnostic Biomarker of Immune System Abnormalities in Multiple Sclerosis and HIV Infection. Biomed. Res. Int., 2019."
},
{
"DOI": "10.1007/s11538-023-01181-0",
"doi-asserted-by": "crossref",
"key": "ref_25",
"unstructured": "Weatherley, G., Araujo, R.P., Dando, S.J., and Jenner, A.L. (2023). Could Mathematics be the Key to Unlocking the Mysteries of Multiple Sclerosis?. Bull. Math. Biol., 85."
},
{
"DOI": "10.3389/fimmu.2020.587078",
"doi-asserted-by": "crossref",
"key": "ref_26",
"unstructured": "Houen, G., Trier, N.H., and Frederiksen, J.L. (2020). Epstein-Barr Virus and Multiple Sclerosis. Front. Immunol., 11."
},
{
"DOI": "10.3390/v15040949",
"doi-asserted-by": "crossref",
"key": "ref_27",
"unstructured": "Rousseau, B.A., and Bhaduri-McIntosh, S. (2023). Inflammation and Epstein-Barr Virus at the Crossroads of Multiple Sclerosis and Post-Acute Sequelae of COVID-19 Infection. Viruses, 15."
},
{
"article-title": "Long-Term Respiratory and Neurological Sequelae of COVID-19",
"author": "Wang",
"first-page": "e928996",
"journal-title": "Med. Sci. Monit.",
"key": "ref_28",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1007/s42399-020-00504-9",
"article-title": "COVID-19 and Multiple Sclerosis: Predisposition and Precautions in Treatment SN",
"author": "Sadeghmousavi",
"doi-asserted-by": "crossref",
"first-page": "1802",
"journal-title": "Compr. Clin. Med.",
"key": "ref_29",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1007/s00415-023-11692-4",
"article-title": "COVID-19 infection after SARS-CoV-2 mRNA vaccination in Multiple Sclerosis, AQP4-antibody NMOSD and MOGAD patients during the Omicron subvariant BA.1/2 wave in Singapore",
"author": "Yeo",
"doi-asserted-by": "crossref",
"first-page": "2817",
"journal-title": "J. Neurol.",
"key": "ref_30",
"volume": "270",
"year": "2023"
},
{
"DOI": "10.3390/v13102091",
"doi-asserted-by": "crossref",
"key": "ref_31",
"unstructured": "Satheesh, N.J., Salloum-Asfar, S., and Abdulla, S.A. (2021). The Potential Role of COVID-19 in the Pathogenesis of Multiple Sclerosis—A Preliminary Report. Viruses, 13."
},
{
"DOI": "10.1007/s10787-022-01011-0",
"article-title": "Melatonin and multiple sclerosis: Antioxidant, anti-inflammatory and immunomodulator mechanism of action",
"author": "Escribano",
"doi-asserted-by": "crossref",
"first-page": "1569",
"journal-title": "Inflammopharmacology",
"key": "ref_32",
"volume": "30",
"year": "2022"
},
{
"DOI": "10.1515/revneuro-2021-0148",
"article-title": "Coronaviruses and their relationship with multiple sclerosis: Is the prevalence of multiple sclerosis going to increase after the Covid-19 pandemia?",
"author": "Lima",
"doi-asserted-by": "crossref",
"first-page": "703",
"journal-title": "Rev. Neurosci.",
"key": "ref_33",
"volume": "33",
"year": "2022"
},
{
"DOI": "10.1007/s00415-021-10744-x",
"article-title": "Anti-CD20 therapies for multiple sclerosis: Current status and future perspectives",
"author": "Margoni",
"doi-asserted-by": "crossref",
"first-page": "1316",
"journal-title": "J. Neurol.",
"key": "ref_34",
"volume": "269",
"year": "2022"
},
{
"DOI": "10.3389/fimmu.2021.755333",
"doi-asserted-by": "crossref",
"key": "ref_35",
"unstructured": "Bellucci, G., Rinaldi, V., Buscarinu, M.C., Reniè, R., Bigi, R., Pellicciari, G., Morena, E., Romano, C., Marrone, A., and Mechelli, R. (2021). Multiple Sclerosis and SARS-CoV-2: Has the Interplay Started?. Front. Immunol., 12."
},
{
"DOI": "10.3390/cells12050684",
"doi-asserted-by": "crossref",
"key": "ref_36",
"unstructured": "Fernandes de Souza, W.D., Fonseca, D.M.D., and Sartori, A. (2023). COVID-19 and Multiple Sclerosis: A Complex Relationship Possibly Aggravated by Low Vitamin D Levels. Cells, 12."
},
{
"DOI": "10.1111/ene.15554",
"article-title": "Signs and symptoms of COVID-19 in patients with multiple sclerosis",
"author": "Schiavetti",
"doi-asserted-by": "crossref",
"first-page": "3728",
"journal-title": "Eur. J. Neurol.",
"key": "ref_37",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.1016/j.msard.2021.103371",
"article-title": "COVID-19 outcomes in persons with multiple sclerosis treated with rituximab",
"author": "Iyer",
"doi-asserted-by": "crossref",
"first-page": "103371",
"journal-title": "Mult. Scler. Relat. Disord.",
"key": "ref_38",
"volume": "57",
"year": "2022"
},
{
"DOI": "10.3389/fneur.2020.580507",
"doi-asserted-by": "crossref",
"key": "ref_39",
"unstructured": "Motolese, F., Rossi, M., Albergo, G., Stelitano, D., Villanova, M., Di Lazzaro, V., and Capone, F. (2020). The Psychological Impact of COVID-19 Pandemic on People with Multiple Sclerosis. Front. Neurol., 11."
},
{
"DOI": "10.1161/STR.0b013e318296aeca",
"article-title": "An updated definition of stroke for the 21st century: A statement for healthcare professionals from the American Heart Association/American Stroke Association",
"author": "Sacco",
"doi-asserted-by": "crossref",
"first-page": "2064",
"journal-title": "Stroke",
"key": "ref_40",
"volume": "44",
"year": "2013"
},
{
"DOI": "10.5005/jp-journals-10071-23192",
"article-title": "Acute Ischemic Stroke: Management Approach",
"author": "Chugh",
"doi-asserted-by": "crossref",
"first-page": "S140",
"journal-title": "Indian J. Crit. Care Med.",
"key": "ref_41",
"volume": "23",
"year": "2019"
},
{
"DOI": "10.1016/S0140-6736(12)61728-0",
"article-title": "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010",
"author": "Lozano",
"doi-asserted-by": "crossref",
"first-page": "2095",
"journal-title": "Lancet",
"key": "ref_42",
"volume": "380",
"year": "2012"
},
{
"DOI": "10.1161/CIR.0000000000001123",
"article-title": "Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association",
"author": "Tsao",
"doi-asserted-by": "crossref",
"first-page": "e93",
"journal-title": "Circulation",
"key": "ref_43",
"volume": "147",
"year": "2023"
},
{
"DOI": "10.1161/STROKEAHA.122.040073",
"article-title": "Projected Global Trends in Ischemic Stroke Incidence, Deaths and Disability-Adjusted Life Years From 2020 to 2030",
"author": "Pu",
"doi-asserted-by": "crossref",
"first-page": "1330",
"journal-title": "Stroke",
"key": "ref_44",
"volume": "54",
"year": "2023"
},
{
"DOI": "10.17712/nsj.2016.3.20150731",
"article-title": "Risk factors and subtypes of acute ischemic stroke. A study at King Fahd Hospital of the University",
"author": "Zafar",
"doi-asserted-by": "crossref",
"first-page": "246",
"journal-title": "Neurosciences",
"key": "ref_45",
"volume": "21",
"year": "2016"
},
{
"DOI": "10.1016/j.bbadis.2018.09.012",
"doi-asserted-by": "crossref",
"key": "ref_46",
"unstructured": "Barthels, D., and Das, H. (2020). Current advances in ischemic stroke research and therapies. Biochim. Biophys. Acta Mol. Basis Dis., 1866."
},
{
"DOI": "10.1016/j.mpmed.2020.06.002",
"article-title": "Stroke: Causes and clinical features",
"author": "Murphy",
"doi-asserted-by": "crossref",
"first-page": "561",
"journal-title": "Medicine",
"key": "ref_47",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.1161/STROKEAHA.122.040524",
"article-title": "Risk Factors and Causes of Ischemic Stroke in 1322 Young Adults",
"author": "Ekker",
"doi-asserted-by": "crossref",
"first-page": "439",
"journal-title": "Stroke",
"key": "ref_48",
"volume": "54",
"year": "2023"
},
{
"DOI": "10.1186/s10194-017-0815-1",
"article-title": "Hormonal contraceptives and risk of ischemic stroke in women with migraine: A consensus statement from the European Headache Federation (EHF) and the European Society of Contraception and Reproductive Health (ESC)",
"author": "Sacco",
"doi-asserted-by": "crossref",
"first-page": "108",
"journal-title": "J. Headache Pain",
"key": "ref_49",
"volume": "18",
"year": "2017"
},
{
"DOI": "10.1016/S0140-6736(16)30506-2",
"article-title": "Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): A case-control study",
"author": "Chin",
"doi-asserted-by": "crossref",
"first-page": "761",
"journal-title": "Lancet",
"key": "ref_50",
"volume": "388",
"year": "2016"
},
{
"DOI": "10.1056/NEJMoa041747",
"article-title": "Risk of myocardial infarction and stroke after acute infection or vaccination",
"author": "Smeeth",
"doi-asserted-by": "crossref",
"first-page": "2611",
"journal-title": "N. Engl. J. Med.",
"key": "ref_51",
"volume": "351",
"year": "2004"
},
{
"DOI": "10.1038/nrneurol.2010.163",
"article-title": "Common infections and the risk of stroke",
"author": "Grau",
"doi-asserted-by": "crossref",
"first-page": "681",
"journal-title": "Nat. Rev. Neurol.",
"key": "ref_52",
"volume": "6",
"year": "2010"
},
{
"DOI": "10.1161/STROKEAHA.120.030630",
"article-title": "Acute Viral Illnesses and Ischemic Stroke: Pathophysiological Considerations in the Era of the COVID-19 Pandemic",
"author": "Bahouth",
"doi-asserted-by": "crossref",
"first-page": "1885",
"journal-title": "Stroke",
"key": "ref_53",
"volume": "52",
"year": "2021"
},
{
"DOI": "10.1161/01.STR.0000226901.34927.10",
"article-title": "Inflammation and atherosclerosis: Novel insights into plaque formation and destabilization",
"author": "Stoll",
"doi-asserted-by": "crossref",
"first-page": "1923",
"journal-title": "Stroke",
"key": "ref_54",
"volume": "37",
"year": "2006"
},
{
"DOI": "10.1002/jmv.23354",
"article-title": "Review: Viral infections and mechanisms of thrombosis and bleeding",
"author": "Goeijenbier",
"doi-asserted-by": "crossref",
"first-page": "1680",
"journal-title": "J. Med. Virol.",
"key": "ref_55",
"volume": "84",
"year": "2012"
},
{
"DOI": "10.1161/01.STR.0000089015.51603.CC",
"article-title": "Inflammation and infections as risk factors for ischemic stroke",
"author": "Lindsberg",
"doi-asserted-by": "crossref",
"first-page": "2518",
"journal-title": "Stroke",
"key": "ref_56",
"volume": "34",
"year": "2003"
},
{
"DOI": "10.1016/j.jocn.2020.05.017",
"article-title": "Neurological manifestations and complications of COVID-19: A literature review",
"author": "Ahmad",
"doi-asserted-by": "crossref",
"first-page": "8",
"journal-title": "J. Clin. Neurosci.",
"key": "ref_57",
"volume": "77",
"year": "2020"
},
{
"DOI": "10.1007/s43440-022-00424-6",
"article-title": "Neurological consequences of COVID-19",
"author": "Brola",
"doi-asserted-by": "crossref",
"first-page": "1208",
"journal-title": "Pharmacol. Rep.",
"key": "ref_58",
"volume": "74",
"year": "2022"
},
{
"DOI": "10.1016/j.neulet.2020.135564",
"article-title": "Stroke in patients with COVID-19: Clinical and neuroimaging characteristics",
"author": "Vogrig",
"doi-asserted-by": "crossref",
"first-page": "135564",
"journal-title": "Neurosci. Lett.",
"key": "ref_59",
"volume": "743",
"year": "2021"
},
{
"DOI": "10.1007/s11239-020-02228-y",
"article-title": "COVID-19 and ischemic stroke: A systematic review and meta-summary of the literature",
"author": "Tan",
"doi-asserted-by": "crossref",
"first-page": "587",
"journal-title": "J. Thromb. Thrombolysis",
"key": "ref_60",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1136/svn-2020-000431",
"article-title": "Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "279",
"journal-title": "Stroke Vasc. Neurol.",
"key": "ref_61",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1001/jamaneurol.2020.2730",
"article-title": "Risk of Ischemic Stroke in Patients with Coronavirus Disease 2019 (COVID-19) vs. Patients with Influenza",
"author": "Merkler",
"doi-asserted-by": "crossref",
"first-page": "1366",
"journal-title": "JAMA Neurol.",
"key": "ref_62",
"volume": "77",
"year": "2020"
},
{
"article-title": "The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—An update on the status",
"author": "Guo",
"first-page": "11",
"journal-title": "Mil. Med. Res.",
"key": "ref_63",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1002/path.1570",
"article-title": "Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis",
"author": "Hamming",
"doi-asserted-by": "crossref",
"first-page": "631",
"journal-title": "J. Pathol.",
"key": "ref_64",
"volume": "203",
"year": "2004"
},
{
"DOI": "10.1093/bib/bbac045",
"doi-asserted-by": "crossref",
"key": "ref_65",
"unstructured": "Bartas, M., Volná, A., A Beaudoin, C., Poulsen, E.T., Červeň, J., Brázda, V., Špunda, V., Blundell, T.L., and Pečinka, P. (2022). Unheeded SARS-CoV-2 proteins? A deep look into negative-sense RNA. Brief Bioinform., 23."
},
{
"DOI": "10.1001/jamacardio.2020.1017",
"article-title": "Cardiovascular Implications of Fatal Outcomes of Patients with Coronavirus Disease 2019 (COVID-19)",
"author": "Guo",
"doi-asserted-by": "crossref",
"first-page": "811",
"journal-title": "JAMA Cardiol.",
"key": "ref_66",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1080/00207454.2021.1897588",
"article-title": "The effects of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on ischemic stroke and the possible underlying mechanisms",
"author": "Song",
"doi-asserted-by": "crossref",
"first-page": "176",
"journal-title": "Int. J. Neurosci.",
"key": "ref_67",
"volume": "133",
"year": "2023"
},
{
"DOI": "10.4081/cp.2020.1271",
"article-title": "COVID-19: Hemoglobin, iron, and hypoxia beyond inflammation. A narrative review",
"author": "Cavezzi",
"doi-asserted-by": "crossref",
"first-page": "1271",
"journal-title": "Clin. Pract.",
"key": "ref_68",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1016/j.steroids.2020.108661",
"article-title": "Hepcidin, an overview of biochemical and clinical properties",
"author": "Rauf",
"doi-asserted-by": "crossref",
"first-page": "108661",
"journal-title": "Steroids",
"key": "ref_69",
"volume": "160",
"year": "2020"
},
{
"DOI": "10.1073/pnas.1620458114",
"article-title": "Activation of NLRP3 inflammasome complex potentiates venous thrombosis in response to hypoxia",
"author": "Gupta",
"doi-asserted-by": "crossref",
"first-page": "4763",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_70",
"volume": "114",
"year": "2017"
},
{
"DOI": "10.1016/S2213-2600(20)30216-2",
"article-title": "COVID-19 cytokine storm: The interplay between inflammation and coagulation",
"author": "Jose",
"doi-asserted-by": "crossref",
"first-page": "e46",
"journal-title": "Lancet Respir. Med.",
"key": "ref_71",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.3892/ijmm.2021.4854",
"article-title": "COVID-19 and ischemic stroke: Mechanisms of hypercoagulability (Review)",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "21",
"journal-title": "Int. J. Mol. Med.",
"key": "ref_72",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2020.01446",
"doi-asserted-by": "crossref",
"key": "ref_73",
"unstructured": "Ragab, D., Salah Eldin, H., Taeimah, M., Khattab, R., and Salem, R. (2020). The COVID-19 Cytokine Storm; What We Know So Far. Front. Immunol., 11."
},
{
"DOI": "10.3390/biomedicines11041181",
"doi-asserted-by": "crossref",
"key": "ref_74",
"unstructured": "Farooqui, A.A., Farooqui, T., Sun, G.Y., Lin, T.N., Teh, D.B.L., and Ong, W.Y. (2023). COVID-19, Blood Lipid Changes, and Thrombosis. Biomedicines, 11."
},
{
"DOI": "10.1016/j.cytogfr.2021.11.001",
"article-title": "SARS-CoV-2 infection and oxidative stress: Pathophysiological insight into thrombosis and therapeutic opportunities",
"author": "Alam",
"doi-asserted-by": "crossref",
"first-page": "44",
"journal-title": "Cytokine Growth Factor Rev.",
"key": "ref_75",
"volume": "63",
"year": "2022"
},
{
"DOI": "10.3389/fmicb.2022.1111930",
"doi-asserted-by": "crossref",
"key": "ref_76",
"unstructured": "Gain, C., Song, S., Angtuaco, T., Satta, S., and Kelesidis, T. (2023). The role of oxidative stress in the pathogenesis of infections with coronaviruses. Front. Microbiol., 13."
},
{
"DOI": "10.2174/1389450123666220826162900",
"article-title": "Fibrinogen, Fibrin, and Fibrin Degradation Products in COVID-19",
"author": "Kangro",
"doi-asserted-by": "crossref",
"first-page": "1593",
"journal-title": "Curr. Drug Targets",
"key": "ref_77",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1016/j.ancard.2020.09.027",
"article-title": "COVID-19 and venous thromboembolic disease (COVID-19 and venous thromboembolism)",
"author": "Trimaille",
"doi-asserted-by": "crossref",
"first-page": "370",
"journal-title": "Ann. Cardiol. Angeiol.",
"key": "ref_78",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/j.clinsp.2022.100012",
"article-title": "Ischemic stroke in 455 COVID-19 patients",
"author": "Finsterer",
"doi-asserted-by": "crossref",
"first-page": "100012",
"journal-title": "Clinics",
"key": "ref_79",
"volume": "77",
"year": "2022"
},
{
"DOI": "10.3389/fimmu.2023.1129201",
"doi-asserted-by": "crossref",
"key": "ref_80",
"unstructured": "Capozzi, A., Riitano, G., Recalchi, S., Manganelli, V., Longo, A., Falcou, A., De Michele, M., Garofalo, T., Pulcinelli, F.M., and Sorice, M. (2023). Antiphospholipid antibodies in patients with stroke during COVID-19: A role in the signaling pathway leading to platelet activation. Front. Immunol., 14."
},
{
"DOI": "10.1056/NEJMc2007575",
"article-title": "Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "e38",
"journal-title": "N. Engl. J. Med.",
"key": "ref_81",
"volume": "382",
"year": "2020"
},
{
"article-title": "The Epidemiology of Alzheimer’s Disease Modifiable Risk Factors and Prevention",
"author": "Zhang",
"first-page": "313",
"journal-title": "J. Prev. Alzheimer’s Dis.",
"key": "ref_82",
"volume": "8",
"year": "2021"
},
{
"key": "ref_83",
"unstructured": "Patterson, C. (2018). World Alzheimer Report 2018, Alzheimer’s Disease International."
},
{
"DOI": "10.1016/S1474-4422(18)30403-4",
"article-title": "Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016",
"author": "Nichols",
"doi-asserted-by": "crossref",
"first-page": "88",
"journal-title": "Lancet Neurol.",
"key": "ref_84",
"volume": "18",
"year": "2019"
},
{
"DOI": "10.1016/S1474-4422(16)00062-4",
"article-title": "Defeating Alzheimer’s disease and other dementias: A priority for European science and society",
"author": "Winblad",
"doi-asserted-by": "crossref",
"first-page": "455",
"journal-title": "Lancet Neurol.",
"key": "ref_85",
"volume": "15",
"year": "2016"
},
{
"DOI": "10.3389/fncel.2021.691136",
"doi-asserted-by": "crossref",
"key": "ref_86",
"unstructured": "Lotz, S.K., Blackhurst, B.M., Reagin, K.L., and Funk, K.E. (2021). Microbial Infections Are a Risk Factor for Neurodegenerative Diseases. Front. Cell Neurosci., 15."
},
{
"DOI": "10.1007/s00705-021-04959-6",
"article-title": "Viral infections and their relationship to neurological disorders",
"author": "Wouk",
"doi-asserted-by": "crossref",
"first-page": "733",
"journal-title": "Arch. Virol.",
"key": "ref_87",
"volume": "166",
"year": "2021"
},
{
"DOI": "10.1016/j.neuron.2022.12.029",
"article-title": "Virus exposure and neurodegenerative disease risk across national biobanks",
"author": "Levine",
"doi-asserted-by": "crossref",
"first-page": "1086",
"journal-title": "Neuron",
"key": "ref_88",
"volume": "111",
"year": "2023"
},
{
"DOI": "10.31083/j.jin2102073",
"article-title": "Infectious agents and Alzheimer’s disease",
"author": "Piekut",
"doi-asserted-by": "crossref",
"first-page": "73",
"journal-title": "J. Integr. Neurosci.",
"key": "ref_89",
"volume": "21",
"year": "2022"
},
{
"DOI": "10.1080/1040841X.2021.1876630",
"article-title": "The role of microbial infection in the pathogenesis of Alzheimer’s disease and the opportunity for protection by anti-microbial peptides",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "240",
"journal-title": "Crit. Rev. Microbiol.",
"key": "ref_90",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1186/s40035-021-00237-2",
"article-title": "COVID-19 and Alzheimer’s disease: How one crisis worsens the other",
"author": "Xia",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "Transl. Neurodegener.",
"key": "ref_91",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2012-7",
"article-title": "A pneumonia outbreak associated with a new coronavirus of probable bat origin",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "270",
"journal-title": "Nature",
"key": "ref_92",
"volume": "579",
"year": "2020"
},
{
"DOI": "10.1001/jamaneurol.2020.2065",
"article-title": "Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review",
"author": "Zubair",
"doi-asserted-by": "crossref",
"first-page": "1018",
"journal-title": "JAMA Neurol.",
"key": "ref_93",
"volume": "77",
"year": "2020"
},
{
"DOI": "10.1093/ibd/izaa131",
"article-title": "Temporal Correlation Between Neurological and Gastrointestinal Symptoms of SARS-CoV-2",
"doi-asserted-by": "crossref",
"first-page": "e89",
"journal-title": "Inflamm. Bowel Dis.",
"key": "ref_94",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1038/s41398-022-02052-3",
"article-title": "COVID-19 and risk of neurodegenerative disorders: A Mendelian randomization study",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "283",
"journal-title": "Transl. Psychiatry",
"key": "ref_95",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1038/s41556-021-00796-6",
"article-title": "A single-cell transcriptomic landscape of the lungs of patients with COVID-19",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1314",
"journal-title": "Nat. Cell Biol.",
"key": "ref_96",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1002/jmv.28107",
"article-title": "Causal effect of COVID-19 on Alzheimer’s disease: A Mendelian randomization study",
"author": "Baranova",
"doi-asserted-by": "crossref",
"first-page": "e28107",
"journal-title": "J. Med. Virol.",
"key": "ref_97",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.1093/gerona/glaa183",
"article-title": "Preexisting Comorbidities Predicting Severe COVID-19 in Older Adults in the UK Biobank Community Cohort",
"author": "Atkins",
"doi-asserted-by": "crossref",
"first-page": "2224",
"journal-title": "J. Gerontol. Ser. A",
"key": "ref_98",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.3233/JAD-200937",
"article-title": "Cognitive Impairment Is a Common Comorbidity in Deceased COVID-19 Patients: A Hospital-Based Retrospective Cohort Study",
"author": "Seoane",
"doi-asserted-by": "crossref",
"first-page": "1367",
"journal-title": "J. Alzheimer’s Dis.",
"key": "ref_99",
"volume": "78",
"year": "2020"
},
{
"DOI": "10.3390/jpm11101015",
"doi-asserted-by": "crossref",
"key": "ref_100",
"unstructured": "Park, H.Y., Song, I.A., and Oh, T.K. (2021). Dementia Risk among Coronavirus Disease Survivors: A Nationwide Cohort Study in South Korea. J. Pers. Med., 11."
},
{
"DOI": "10.3233/JAD-210050",
"article-title": "Clinical Features and Outcomes of Patients with Dementia Compared to an Aging Cohort Hospitalized During the Initial New York City COVID-19 Wave",
"author": "Harb",
"doi-asserted-by": "crossref",
"first-page": "679",
"journal-title": "J. Alzheimer’s Dis.",
"key": "ref_101",
"volume": "81",
"year": "2021"
},
{
"DOI": "10.1186/s13195-021-00820-9",
"article-title": "COVID-19 in adults with dementia: Clinical features and risk factors of mortality—A clinical cohort study on 125 patients",
"author": "Vrillon",
"doi-asserted-by": "crossref",
"first-page": "77",
"journal-title": "Alzheimer’s Res. Ther.",
"key": "ref_102",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1007/s12603-020-1389-1",
"article-title": "Clinical Presentation of COVID19 in Dementia Patients",
"author": "Bianchetti",
"doi-asserted-by": "crossref",
"first-page": "560",
"journal-title": "J. Nutr. Health Aging",
"key": "ref_103",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1016/j.mcn.2005.03.012",
"article-title": "Angiotensin-(1-7) enhances LTP in the hippocampus through the G-protein-coupled receptor Mas",
"author": "Hellner",
"doi-asserted-by": "crossref",
"first-page": "427",
"journal-title": "Mol. Cell Neurosci.",
"key": "ref_104",
"volume": "29",
"year": "2005"
},
{
"DOI": "10.1016/j.nlm.2011.10.003",
"article-title": "Angiotensin-(1-7)/Mas axis integrity is required for the expression of object recognition memory",
"author": "Lazaroni",
"doi-asserted-by": "crossref",
"first-page": "113",
"journal-title": "Neurobiol. Learn Mem.",
"key": "ref_105",
"volume": "97",
"year": "2012"
},
{
"DOI": "10.1007/s00109-008-0331-5",
"article-title": "Brain renin angiotensin in disease",
"author": "Phillips",
"doi-asserted-by": "crossref",
"first-page": "715",
"journal-title": "J. Mol. Med.",
"key": "ref_106",
"volume": "86",
"year": "2008"
},
{
"DOI": "10.1007/s12035-015-9260-9",
"article-title": "Angiotensin-(1-7) is Reduced and Inversely Correlates with Tau Hyperphosphorylation in Animal Models of Alzheimer’s Disease",
"author": "Jiang",
"doi-asserted-by": "crossref",
"first-page": "2489",
"journal-title": "Mol. Neurobiol.",
"key": "ref_107",
"volume": "53",
"year": "2016"
},
{
"DOI": "10.1002/jnr.23404",
"article-title": "Conversion of Aβ43 to Aβ40 by the successive action of angiotensin-converting enzyme 2 and angiotensin-converting enzyme",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "1178",
"journal-title": "J. Neurosci. Res.",
"key": "ref_108",
"volume": "92",
"year": "2014"
},
{
"DOI": "10.3390/ijms22041687",
"doi-asserted-by": "crossref",
"key": "ref_109",
"unstructured": "Ding, Q., Shults, N.V., Gychka, S.G., Harris, B.T., and Suzuki, Y.J. (2021). Protein Expression of Angiotensin-Converting Enzyme 2 (ACE2) is Upregulated in Brains with Alzheimer’s Disease. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.1016/j.ajpath.2013.01.053",
"article-title": "Aβ43 is the earliest-depositing Aβ species in APP transgenic mouse brain and is converted to Aβ41 by two active domains of ACE",
"author": "Zou",
"doi-asserted-by": "crossref",
"first-page": "2322",
"journal-title": "Am. J. Pathol.",
"key": "ref_110",
"volume": "182",
"year": "2013"
},
{
"DOI": "10.1523/JNEUROSCI.4849-06.2007",
"article-title": "Abeta40 inhibits amyloid deposition in vivo",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "627",
"journal-title": "J. Neurosci.",
"key": "ref_111",
"volume": "27",
"year": "2007"
},
{
"DOI": "10.1016/j.jmb.2007.04.014",
"article-title": "Abeta40 protects non-toxic Abeta42 monomer from aggregation",
"author": "Yan",
"doi-asserted-by": "crossref",
"first-page": "909",
"journal-title": "J. Mol. Biol.",
"key": "ref_112",
"volume": "369",
"year": "2007"
},
{
"DOI": "10.1021/bi991161m",
"article-title": "Interaction between A beta(1-42) and A beta(1-40) in Alzheimer’s beta-amyloid fibril formation in vitro",
"author": "Hasegawa",
"doi-asserted-by": "crossref",
"first-page": "15514",
"journal-title": "Biochemistry",
"key": "ref_113",
"volume": "38",
"year": "1999"
},
{
"DOI": "10.3390/ijerph20032146",
"doi-asserted-by": "crossref",
"key": "ref_114",
"unstructured": "Rudnicka-Drożak, E., Drożak, P., Mizerski, G., Zaborowski, T., Ślusarska, B., Nowicki, G., and Drożak, M. (2023). Links between COVID-19 and Alzheimer’s Disease—What Do We Already Know?. Int. J. Environ. Res. Public Health, 20."
},
{
"DOI": "10.5114/fn.2021.109495",
"article-title": "Ubiquity of the SARS-CoV-2 receptor ACE2 and upregulation in limbic regions of Alzheimer’s disease brain",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "232",
"journal-title": "Folia Neuropathol.",
"key": "ref_115",
"volume": "59",
"year": "2021"
},
{
"DOI": "10.1038/npjamd.2016.24",
"article-title": "Deficiency of angiotensin-converting enzyme 2 causes deterioration of cognitive function",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "16024",
"journal-title": "NPJ Aging Mech. Dis.",
"key": "ref_116",
"volume": "2",
"year": "2016"
},
{
"DOI": "10.4103/ijpvm.IJPVM_114_20",
"article-title": "Possible Neurological and Mental Outcomes of COVID-19 Infection: A Hypothetical Role of ACE-2\\Mas\\BDNF Signaling Pathway",
"author": "Motaghinejad",
"doi-asserted-by": "crossref",
"first-page": "84",
"journal-title": "Int. J. Prev. Med.",
"key": "ref_117",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.plipres.2010.09.001",
"article-title": "Apolipoprotein E: From lipid transport to neurobiology",
"author": "Hauser",
"doi-asserted-by": "crossref",
"first-page": "62",
"journal-title": "Prog. Lipid Res.",
"key": "ref_118",
"volume": "50",
"year": "2011"
},
{
"DOI": "10.1186/1750-1326-4-21",
"article-title": "ApoE isoform-dependent changes in hippocampal synaptic function",
"author": "Korwek",
"doi-asserted-by": "crossref",
"first-page": "21",
"journal-title": "Mol. Neurodegener.",
"key": "ref_119",
"volume": "4",
"year": "2009"
},
{
"DOI": "10.1046/j.1471-4159.2001.00047.x",
"article-title": "ApoE protects cortical neurones against neurotoxicity induced by the non-fibrillar C-terminal domain of the amyloid-beta peptide",
"author": "Drouet",
"doi-asserted-by": "crossref",
"first-page": "117",
"journal-title": "J. Neurochem.",
"key": "ref_120",
"volume": "76",
"year": "2001"
},
{
"DOI": "10.1016/S1474-4422(10)70325-2",
"article-title": "Apolipoprotein E in Alzheimer’s disease and other neurological disorders",
"author": "Verghese",
"doi-asserted-by": "crossref",
"first-page": "241",
"journal-title": "Lancet Neurol.",
"key": "ref_121",
"volume": "10",
"year": "2011"
},
{
"DOI": "10.1093/gerona/glaa131",
"article-title": "APOE e4 Genotype Predicts Severe COVID-19 in the UK Biobank Community Cohort",
"author": "Kuo",
"doi-asserted-by": "crossref",
"first-page": "2231",
"journal-title": "J. Gerontol. A Biol. Sci. Med. Sci.",
"key": "ref_122",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1101/2020.05.09.086249",
"doi-asserted-by": "crossref",
"key": "ref_123",
"unstructured": "Wang, H., Yuan, Z., Pavel, M.A., Jablonski, S.M., Jablonski, J., Hobson, R., Valente, S., Reddy, C.B., and Hansen, S.B. (2021). The role of high cholesterol in age-related COVID19 lethality. bioRxiv."
},
{
"DOI": "10.1016/j.trci.2018.06.014",
"article-title": "Inflammation as a central mechanism in Alzheimer’s disease",
"author": "Kinney",
"doi-asserted-by": "crossref",
"first-page": "575",
"journal-title": "Alzheimer’s Dement.",
"key": "ref_124",
"volume": "4",
"year": "2018"
},
{
"article-title": "A review: Inflammatory process in Alzheimer’s disease, role of cytokines",
"first-page": "756357",
"journal-title": "Sci. World J.",
"key": "ref_125",
"volume": "2012",
"year": "2012"
},
{
"DOI": "10.1111/psyg.12218",
"article-title": "Serum tumour necrosis factor-α and interleukin-6 levels in Alzheimer’s disease and mild cognitive impairment",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "224",
"journal-title": "Psychogeriatrics",
"key": "ref_126",
"volume": "17",
"year": "2017"
},
{
"DOI": "10.3390/medicina58020144",
"doi-asserted-by": "crossref",
"key": "ref_127",
"unstructured": "Zanza, C., Romenskaya, T., Manetti, A.C., Franceschi, F., La Russa, R., Bertozzi, G., Maiese, A., Savioli, G., Volonnino, G., and Longhitano, Y. (2022). Cytokine Storm in COVID-19: Immunopathogenesis and Therapy. Medicina, 58."
},
{
"DOI": "10.1186/1471-2172-6-2",
"doi-asserted-by": "crossref",
"key": "ref_128",
"unstructured": "Reghunathan, R., Jayapal, M., Hsu, L.Y., Chng, H.H., Tai, D., Leung, B.P., and Melendez, A.J. (2005). Expression profile of immune response genes in patients with Severe Acute Respiratory Syndrome. BMC Immunol., 6."
},
{
"DOI": "10.1182/blood-2004-10-4166",
"article-title": "Chemokine up-regulation in SARS-coronavirus-infected, monocyte-derived human dendritic cells",
"author": "Law",
"doi-asserted-by": "crossref",
"first-page": "2366",
"journal-title": "Blood",
"key": "ref_129",
"volume": "106",
"year": "2005"
},
{
"DOI": "10.1038/s41423-020-0485-9",
"article-title": "The ORF3a protein of SARS-CoV-2 induces apoptosis in cells",
"author": "Ren",
"doi-asserted-by": "crossref",
"first-page": "881",
"journal-title": "Cell Mol. Immunol.",
"key": "ref_130",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.ijbiomac.2020.12.142",
"article-title": "SARS-Cov-2 ORF3a: Mutability and function",
"author": "Bianchi",
"doi-asserted-by": "crossref",
"first-page": "820",
"journal-title": "Int. J. Biol. Macromol.",
"key": "ref_131",
"volume": "170",
"year": "2021"
},
{
"DOI": "10.1007/s00401-018-01957-y",
"article-title": "Aggregated Tau activates NLRP3-ASC inflammasome exacerbating exogenously seeded and non-exogenously seeded Tau pathology in vivo",
"author": "Stancu",
"doi-asserted-by": "crossref",
"first-page": "599",
"journal-title": "Acta Neuropathol.",
"key": "ref_132",
"volume": "137",
"year": "2019"
},
{
"DOI": "10.1038/nature11729",
"article-title": "NLRP3 is activated in Alzheimer’s disease and contributes to pathology in APP/PS1 mice",
"author": "Heneka",
"doi-asserted-by": "crossref",
"first-page": "674",
"journal-title": "Nature",
"key": "ref_133",
"volume": "493",
"year": "2013"
},
{
"DOI": "10.15252/embj.2018101064",
"article-title": "Systemic inflammation impairs microglial Aβ clearance through NLRP3 inflammasome",
"author": "Tejera",
"doi-asserted-by": "crossref",
"first-page": "e101064",
"journal-title": "EMBO J.",
"key": "ref_134",
"volume": "38",
"year": "2019"
},
{
"DOI": "10.3389/fphar.2022.845185",
"doi-asserted-by": "crossref",
"key": "ref_135",
"unstructured": "Liang, T., Zhang, Y., Wu, S., Chen, Q., and Wang, L. (2022). The Role of NLRP3 Inflammasome in Alzheimer’s Disease and Potential Therapeutic Targets. Front. Pharmacol., 13."
},
{
"DOI": "10.1007/s00702-016-1619-1",
"article-title": "Neuroprotective effects of various doses of topiramate against methylphenidate-induced oxidative stress and inflammation in isolated rat amygdala: The possible role of CREB/BDNF signaling pathway",
"author": "Motaghinejad",
"doi-asserted-by": "crossref",
"first-page": "1463",
"journal-title": "J. Neural Transm.",
"key": "ref_136",
"volume": "123",
"year": "2016"
},
{
"DOI": "10.1155/2013/316523",
"article-title": "Oxidative stress and the pathogenesis of Alzheimer’s disease",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "316523",
"journal-title": "Oxid. Med. Cell. Longev.",
"key": "ref_137",
"volume": "2013",
"year": "2013"
},
{
"DOI": "10.1111/j.1471-4159.2004.02455.x",
"article-title": "Increased plaque burden in brains of APP mutant MnSOD heterozygous knockout mice",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "1308",
"journal-title": "J. Neurochem.",
"key": "ref_138",
"volume": "89",
"year": "2004"
},
{
"DOI": "10.1016/S0306-4522(01)00115-4",
"article-title": "Fibrillar beta-amyloid evokes oxidative damage in a transgenic mouse model of Alzheimer’s disease",
"author": "Matsuoka",
"doi-asserted-by": "crossref",
"first-page": "609",
"journal-title": "Neuroscience",
"key": "ref_139",
"volume": "104",
"year": "2001"
},
{
"DOI": "10.1021/bi001876l",
"article-title": "Oxidative regulation of fatty acid-induced tau polymerization",
"author": "Gamblin",
"doi-asserted-by": "crossref",
"first-page": "14203",
"journal-title": "Biochemistry",
"key": "ref_140",
"volume": "39",
"year": "2000"
},
{
"DOI": "10.1371/journal.pone.0000536",
"doi-asserted-by": "crossref",
"key": "ref_141",
"unstructured": "Melov, S., Adlard, P.A., Morten, K., Johnson, F., Golden, T.R., Hinerfeld, D., Schilling, B., Mavros, C., Masters, C.L., and Volitakis, I. (2007). Mitochondrial oxidative stress causes hyperphosphorylation of tau. PLoS ONE, 2."
},
{
"DOI": "10.1073/pnas.171202698",
"article-title": "Does oxidative damage to DNA increase with age?",
"author": "Hamilton",
"doi-asserted-by": "crossref",
"first-page": "10469",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_142",
"volume": "98",
"year": "2001"
},
{
"DOI": "10.3390/diseases9010017",
"doi-asserted-by": "crossref",
"key": "ref_143",
"unstructured": "Kozlov, E.M., Ivanova, E., Grechko, A.V., Wu, W.K., Starodubova, A.V., and Orekhov, A.N. (2021). Involvement of Oxidative Stress and the Innate Immune System in SARS-CoV-2 Infection. Diseases, 9."
},
{
"DOI": "10.1016/j.mehy.2020.110102",
"article-title": "SARS-CoV-2 infection pathogenesis is related to oxidative stress as a response to aggression",
"author": "Cecchini",
"doi-asserted-by": "crossref",
"first-page": "110102",
"journal-title": "Med. Hypotheses",
"key": "ref_144",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.1016/j.clineuro.2020.106414",
"article-title": "Possible immunity, inflammation, and oxidative stress mechanisms of Alzheimer’s disease in COVID-19 patients",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "106414",
"journal-title": "Clin. Neurol. Neurosurg.",
"key": "ref_145",
"volume": "201",
"year": "2021"
},
{
"DOI": "10.1016/j.mad.2020.111250",
"article-title": "Redox modifications in synaptic components as biomarkers of cognitive status, in brain aging and disease",
"author": "Ardiles",
"doi-asserted-by": "crossref",
"first-page": "111250",
"journal-title": "Mech. Ageing Dev.",
"key": "ref_146",
"volume": "189",
"year": "2020"
}
],
"reference-count": 146,
"references-count": 146,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1422-0067/25/16/8715"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "The Influence of SARS-CoV-2 Infection on the Development of Selected Neurological Diseases",
"type": "journal-article",
"volume": "25"
}