Exercise Preferences and Benefits in Patients Hospitalized with COVID-19
et al., Journal of Personalized Medicine, doi:10.3390/jpm12040645, Apr 2022
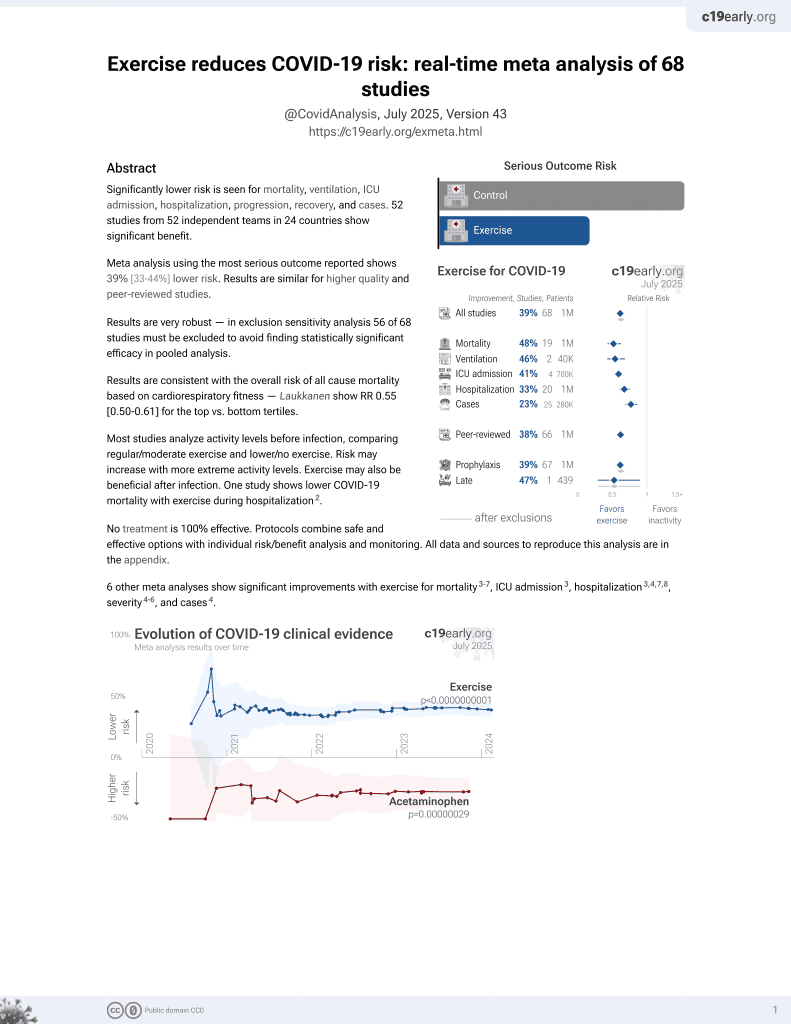
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 66 hospitalized COVID-19 patients in Greece, showing significantly improved recovery with a history of exercise in unadjusted results. Exercise after hospitalization was also associated with lower levels of dyspnea one month post hospitalization.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
|
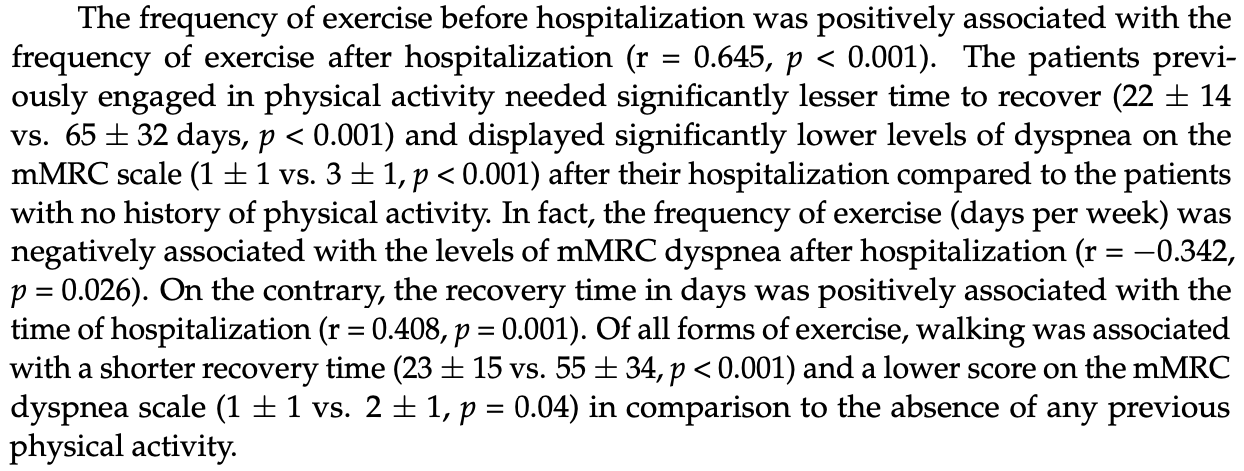
recovery time, 66.2% lower, relative time 0.34, p < 0.001, high activity levels mean 22.0 (±14.0) n=42, low activity levels mean 65.0 (±32.0) n=24.
|
|
relative dyspnea after hospitalization, 66.7% better, RR 0.33, p < 0.001, high activity levels mean 1.0 (±1.0) n=42, low activity levels mean 3.0 (±1.0) n=24, inverted to make RR<1 favor high activity levels.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Kontopoulou et al., 17 Apr 2022, retrospective, Greece, peer-reviewed, survey, 4 authors, study period November 2020 - December 2020.
Contact: raniakotsiou@gmail.com (corresponding author), sevi_kon@hotmail.com, zdaniil@uth.gr, kgourg@med.uth.gr.
Exercise Preferences and Benefits in Patients Hospitalized with COVID-19
Journal of Personalized Medicine, doi:10.3390/jpm12040645
Background: Obese people are at risk of becoming severely ill due to SARS-CoV-2. The exercise benefits on health have been emphasized. Aim: To investigate the correlation of obesity with the length of hospitalization, the pre-and post-hospitalization exercise preferences of COVID-19 patients, and the impact of pre-admission or post-hospitalization physical activity on dyspnea one month after hospitalization and recovery time. Methods: A telephone survey was conducted in patients hospitalized at the
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare no conflict of interest.
References
Albashir, The potential impacts of obesity on COVID-19, Clin. Med, doi:10.7861/clinmed.2020-0239
Berliner, Schneider, Welte, Bauersachs, The Differential Diagnosis of Dyspnea, Dtsch. Arztebl. Int
Bigley, Rezvani, Pistillo, Reed, Agha et al., Acute exercise preferentially redeploys NK-cells with a highly-differentiated phenotype and augments cytotoxicity against lymphoma and multiple myeloma target cells. Part II: Impact of latent cytomegalovirus infection and catecholamine sensitivity, Brain Behav. Immun, doi:10.1016/j.bbi.2014.12.027
Blüher, Obesity: Global epidemiology and pathogenesis, Nat. Rev. Endocrinol, doi:10.1038/s41574-019-0176-8
Bourdas, Zacharakis, Evolution of changes in physical activity over lockdown time: Physical activity datasets of four independent adult sample groups corresponding to each of the last four of the six COVID-19 lockdown weeks in Greece, Data Brief, doi:10.1016/j.dib.2020.106301
Carfì, Bernabei, Landi, Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19, JAMA, doi:10.1001/jama.2020.12603
Cunningham, O'sullivan, Why physical activity matters for older adults in a time of pandemic, Eur. Rev. Aging Phys. Act, doi:10.1186/s11556-020-00249-3
Da Silveira, Da Silva Fagundes, Bizuti, Starck, Rossi et al., Physical exercise as a tool to help the immune system against COVID-19: An integrative review of the current literature, Clin. Exp. Med, doi:10.1007/s10238-020-00650-3
Emami, Javanmardi, Pirbonyeh, Akbari, Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: A Systematic Review and Meta-Analysis, Arch. Acad. Emerg. Med
Ferreira, Felippe, Bertuzzi, Bishop, Barreto et al., The Effects of Acute and Chronic Sprint-Interval Training on Cytokine Responses Are Independent of Prior Caffeine Intake, Front. Physiol
Fountoulakis, Apostolidou, Atsiova, Filippidou, Florou et al., Self-reported changes in anxiety, depression and suicidality during the COVID-19 lockdown in Greece, J. Affect Disord, doi:10.1016/j.jad.2020.10.061
Gao, Ding, Dong, Zhang, Kursat Azkur et al., Risk factors for severe and critically ill COVID-19 patients: A review, Allergy, doi:10.1111/all.14657
Gretebeck, Sabatini, Black, Gretebeck, Physical Activity, Functional Ability, and Obesity in Older Adults: A Gender Difference, J. Gerontol. Nurs, doi:10.3928/00989134-20170406-03
Janssen, Fleming, Kirk, Rollins, Young et al., Changes in physical activity, sitting and sleep across the COVID-19 national lockdown period in Scotland, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph17249362
Jimeno-Almazán, Pallarés, Buendía-Romero, Martínez-Cava, Franco-López et al., Post-COVID-19 Syndrome and the Potential Benefits of Exercise, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph18105329
Katzmarzyk, Powell, Jakicic, Troiano, Piercy et al., PHYSICAL ACTIVITY GUIDELINES ADVISORY COMMITTEE. Sedentary Behavior and Health: Update from the 2018 Physical Activity Guidelines Advisory Committee, Med. Sci. Sports Exerc, doi:10.1249/MSS.0000000000001935
Kimura, Kobayashi, Nakayama, Kakihana, Seasonality in physical activity and walking of healthy older adults, J. Physiol. Anthropol, doi:10.1186/s40101-015-0071-5
Lavie, Ozemek, Carbone, Katzmarzyk, Blair, Sedentary Behavior, Exercise, and Cardiovascular Health, Circ. Res, doi:10.1161/CIRCRESAHA.118.312669
Leandro, De Lima, Alba-Loureiro, Do Nascimento, Manhães De Castro et al., Stress-induced downregulation of macrophage phagocytic function is attenuated by exercise training in rats, Neuroimmunomodulation, doi:10.1159/000107282
Leandro, Ferreira, Silva, Lima-Silva, Covid-19 and Exercise-Induced Immunomodulation, Neuroimmunomodulation, doi:10.1159/000508951
Leandro, Martins De Lima, Folador, Alba-Loreiro, Do Nascimento et al., Physical training attenuates the stress-induced changes in rat T-lymphocyte function, Neuroimmunomodulation, doi:10.1159/000096432
Li, Procter-Gray, Churchill, Crouter, Kane et al., Gender and Age Differences in Levels, Types and Locations of Physical Activity among Older Adults Living in Car-Dependent Neighborhoods, J. Frailty Aging, doi:10.14283/cw.2017.4
Molanorouzi, Khoo, Morris, Motives for adult participation in physical activity: Type of activity, age, and gender, BMC Public Health, doi:10.1186/s12889-015-1429-7
Morales, Tauler Riera, Aguiló Pons, García Taibo, Physical activity recommendations during the COVID-19 pandemic: A practical approach for different target groups, Nutr. Hosp
Morley, Kalantar-Zadeh, Anker, COVID-19: A major cause of cachexia and sarcopenia?, J. Cachexia Sarcopenia Muscle, doi:10.1002/jcsm.12589
Nigg, Fuchs, Gerber, Jekauc, Koch et al., Assessing physical activity through questionnaires-A consensus of best practices and future directions, Psychol. Sport Exerc, doi:10.1016/j.psychsport.2020.101715
Orlandi, Rosselli, Pellegrino, Boddi, Stefani et al., Gender differences in the impact on physical activity and lifestyle in Italy during the lockdown, due to the COVID-19 pandemic, Nutr. Metab. Cardiovasc. Dis, doi:10.1016/j.numecd.2021.03.011
Papazisis, Nikolaidis, Trakada, Sleep, Physical Activity, and Diet of Adults during the Second Lockdown of the COVID-19 Pandemic in Greece, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph18147292
Petrilli, Jones, Yang, Rajagopalan, O'donnell et al., Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study, BMJ, doi:10.1136/bmj.m1966
Pitsavos, Panagiotakos, Lentzas, Stefanadis, Epidemiology of leisure-time physical activity in socio-demographic, lifestyle and psychological characteristics of men and women in Greece: The ATTICA Study, BMC Public Health, doi:10.1186/1471-2458-5-37
Sallis, Hovell, Hofstetter, Predictors of adoption and maintenance of vigorous physical activity in men and women, Prev. Med, doi:10.1016/0091-7435(92)90022-A
Sattar, Mcinnes, Mcmurray, Obesity Is a Risk Factor for Severe COVID-19 Infection: Multiple Potential Mechanisms, Circulation, doi:10.1161/CIRCULATIONAHA.120.047659
Scartoni, Sant'ana, Murillo-Rodriguez, Yamamoto, Imperatori et al., Physical Exercise and Immune System in the Elderly: Implications and Importance in COVID-19 Pandemic Period, Front. Psychol, doi:10.3389/fpsyg.2020.593903
Senna, Torres, Lopes, Alheiros-Lira, De Moura et al., Moderate physical training attenuates perinatal low-protein-induced spleen lymphocyte apoptosis in endotoxemic adult offspring rats, Eur. J. Nutr, doi:10.1007/s00394-015-0925-y
Simpson, Campbell, Gleeson, Krüger, Nieman et al., Can exercise affect immune function to increase susceptibility to infection?, Exerc. Immunol. Rev
Trabelsi, Ammar, Masmoudi, Boukhris, Chtourou et al., Sleep Quality and Physical Activity as Predictors of Mental Wellbeing Variance in Older Adults during COVID-19 Lockdown: ECLB COVID-19 International Online Survey, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph18084329
Van Uffelen, Khan, Burton, Gender differences in physical activity motivators and context preferences: A population-based study in people in their sixties, BMC Public Health, doi:10.1186/s12889-017-4540-0
Wiersinga, Rhodes, Cheng, Peacock, Prescott, Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review, JAMA, doi:10.1001/jama.2020.12839
Wynants, Van Calster, Collins, Riley, Heinze et al., Prediction models for diagnosis and prognosis of covid-19: Systematic review and critical appraisal, BMJ, doi:10.1136/bmj.m1328
DOI record:
{
"DOI": "10.3390/jpm12040645",
"ISSN": [
"2075-4426"
],
"URL": "http://dx.doi.org/10.3390/jpm12040645",
"abstract": "<jats:p>Background: Obese people are at risk of becoming severely ill due to SARS-CoV-2. The exercise benefits on health have been emphasized. Aim: To investigate the correlation of obesity with the length of hospitalization, the pre- and post-hospitalization exercise preferences of COVID-19 patients, and the impact of pre-admission or post-hospitalization physical activity on dyspnea one month after hospitalization and recovery time. Methods: A telephone survey was conducted in patients hospitalized at the Respiratory Medicine Department, University of Thessaly, Greece, from November to December 2020. Results: Two-thirds of the patients were obese. Obesity was not associated with the hospitalization time. Two-thirds of the patients used to engage in physical activity before hospitalization. Males exercised in a higher percentage and more frequently than women before and after hospitalization. The methodical pre-hospitalization exercise was associated with lower levels of dyspnea one month after hospitalization. In-hospital weight loss, comorbidities, and dyspnea on admission independently predicted longer recovery time. Lockdown had boosted men’s desire to exercise than females who were negatively affected. Conclusions: Obesity is common in COVID-19 hospitalized patients. In-hospital weight loss, comorbidities, and dyspnea on admission predicted a longer post-hospitalization recovery time. The pre-hospitalization exercise was associated with less post-hospitalization dyspnea and recovery time.</jats:p>",
"alternative-id": [
"jpm12040645"
],
"author": [
{
"affiliation": [],
"family": "Kontopoulou",
"given": "Sevasti",
"sequence": "first"
},
{
"affiliation": [],
"family": "Daniil",
"given": "Zoe",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9541-1010",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gourgoulianis",
"given": "Konstantinos I.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5219-6971",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kotsiou",
"given": "Ourania S.",
"sequence": "additional"
}
],
"container-title": "Journal of Personalized Medicine",
"container-title-short": "JPM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
4,
18
]
],
"date-time": "2022-04-18T08:21:28Z",
"timestamp": 1650270088000
},
"deposited": {
"date-parts": [
[
2022,
4,
18
]
],
"date-time": "2022-04-18T09:19:53Z",
"timestamp": 1650273593000
},
"indexed": {
"date-parts": [
[
2022,
4,
18
]
],
"date-time": "2022-04-18T09:41:50Z",
"timestamp": 1650274910614
},
"is-referenced-by-count": 0,
"issue": "4",
"issued": {
"date-parts": [
[
2022,
4,
17
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2022,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
4,
17
]
],
"date-time": "2022-04-17T00:00:00Z",
"timestamp": 1650153600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2075-4426/12/4/645/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "645",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
4,
17
]
]
},
"published-online": {
"date-parts": [
[
2022,
4,
17
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1136/bmj.m1328",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1038/s41574-019-0176-8",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047659",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1136/bmj.m1966",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"key": "ref5",
"unstructured": "COVID-19 Pandemic in Greece\nhttps://en.wikipedia.org/wiki/COVID-19_pandemic_in_Greece"
},
{
"DOI": "10.3390/ijerph17249362",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1016/j.jad.2020.10.061",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1186/s11556-020-00249-3",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"article-title": "Physical activity recommendations during the COVID-19 pandemic: A practical approach for different target groups",
"author": "Baena Morales",
"first-page": "194",
"journal-title": "Nutr. Hosp.",
"key": "ref9",
"volume": "38",
"year": "2021"
},
{
"DOI": "10.1161/CIRCRESAHA.118.312669",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.3390/ijerph18084329",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.3390/ijerph18147292",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1016/j.dib.2020.106301",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.3389/fpsyg.2020.593903",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1001/jama.2020.12839",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1111/all.14657",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"article-title": "Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: A Systematic Review and Meta-Analysis",
"author": "Emami",
"first-page": "e35",
"journal-title": "Arch. Acad. Emerg. Med.",
"key": "ref17",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.3238/arztebl.2016.0834",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1001/jama.2020.12603",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.7861/clinmed.2020-0239",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1249/MSS.0000000000001935",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1159/000508951",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"article-title": "Can exercise affect immune function to increase susceptibility to infection?",
"author": "Simpson",
"first-page": "8",
"journal-title": "Exerc. Immunol. Rev.",
"key": "ref23",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2014.12.027",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1007/s00394-015-0925-y",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.3389/fphys.2018.00671",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1159/000096432",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1159/000107282",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.3928/00989134-20170406-03",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.14283/cw.2017.4",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1186/s12889-017-4540-0",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1186/s12889-015-1429-7",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1016/j.numecd.2021.03.011",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1016/0091-7435(92)90022-A",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1186/1471-2458-5-37",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1186/s40101-015-0071-5",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1007/s10238-020-00650-3",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.3390/ijerph18105329",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1002/jcsm.12589",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1016/j.psychsport.2020.101715",
"doi-asserted-by": "publisher",
"key": "ref40"
}
],
"reference-count": 40,
"references-count": 40,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2075-4426/12/4/645"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Medicine (miscellaneous)"
],
"subtitle": [],
"title": "Exercise Preferences and Benefits in Patients Hospitalized with COVID-19",
"type": "journal-article",
"volume": "12"
}