Changes in the pulmonary surfactant in patients with mild to moderate COVID-19
et al., PLoS One, doi:10.1371/journal.pone.0325153 , Aug 2025
Observational study of 29 mild to moderate COVID-19 patients and 17 healthy controls in Sweden, showing persistent alterations in pulmonary surfactant lipids months after COVID-19.
Kokelj et al., 7 Aug 2025, peer-reviewed, 10 authors.
Changes in the pulmonary surfactant in patients with mild to moderate COVID-19
PLOS One, doi:10.1371/journal.pone.0325153
Introduction Changes in the pulmonary surfactant have been seen in severe COVID-19, but data on mild to moderate COVID-19 is scarce. The aim of this study was to explore the protein and phospholipid profiles in the small airways in patients with mild to moderate COVID-19.
Methods 29 cases with COVID-19 and 17 healthy controls were examined at baseline. 22 cases were re-examined at follow-up after recovery from COVID-19. Airwave oscillometry was performed and the biological material from the respiratory tract lining fluid was collected with the PExA (Particles in Exhaled Air) method. SOMAscan was used for the analysis of proteins, and liquid chromatography with tandem mass spectrometry (LC-MS/MS) for phospholipids.
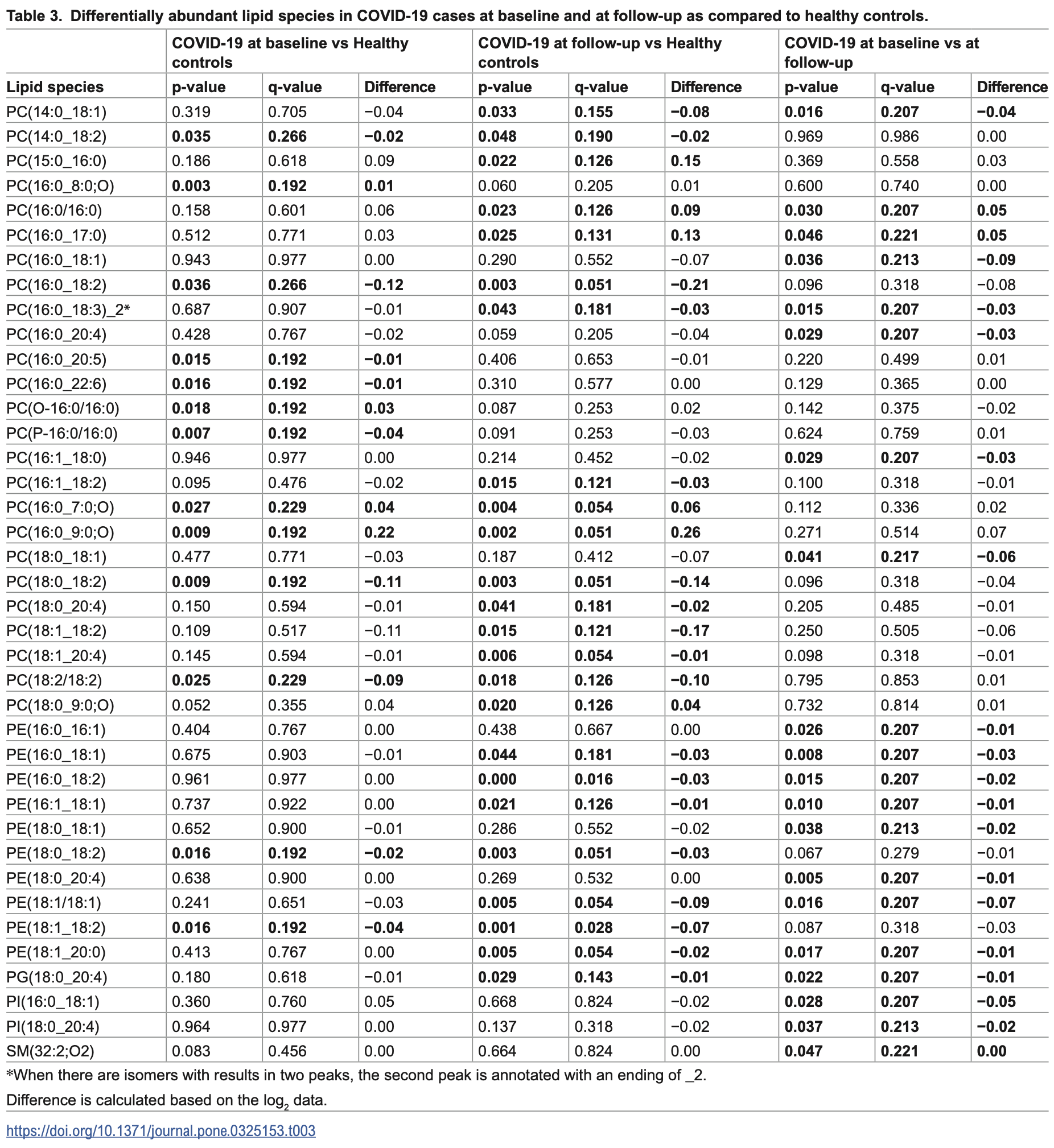
Results 95 lipid species belonging to 8 lipid classes, and 46 proteins were analysed. Relative amounts of 13 lipid species differed between cases and controls at baseline, and of 24 lipid species at follow-up. At follow-up, the phosphatidylethanolamine class (PE) was significantly lower in cases at than in controls, and a significant decrease in PE, as well as a change in 20 lipid species from baseline to follow-up in cases was seen. The protein profile did not differ between cases and controls either at baseline or follow-up, or between repeated measurements in cases.
Conclusions The observed alterations in the surfactant phospholipids in the RTLF indicate that surfactant homeostasis is affected already in mild to moderate COVID-19, and these changes appear to persist over time.
Supporting information S1 Fig. Flow chart on the inclusion and drop out of patients. (TIF) S1 Table . List of all the lipid species analysed and included in the study. (PDF)
S2 Table. Correlations between lipids and proteins and indices of small airway function. (PDF)
S3
References
Adinolfi, Lehner, C9 and factor B as acute phase proteins and their diagnostic and prognostic value in disease, Exp Clin Immunogenet
Afzali, Noris, Lambrecht, Kemper, The state of complement in COVID-19, Nat Rev Immunol, doi:10.1038/s41577-021-00665-1
Almstrand, Bake, Ljungström, Larsson, Bredberg et al., Effect of airway opening on production of exhaled particles, J Appl Physiol, doi:10.1152/japplphysiol.00873.2009
Almstrand, Ljungstrom, Lausmaa, Bake, Sjovall et al., Airway monitoring by collection and mass spectrometric analysis of exhaled particles, Anal Chem
Beyerstedt, Casaro, Rangel, COVID-19: angiotensin-converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection, Eur J Clin Microbiol Infect Dis, doi:10.1007/s10096-020-04138-6
Bredberg, Gobom, Almstrand, Larsson, Blennow et al., Exhaled endogenous particles contain lung proteins, Clin Chem, doi:10.1373/clinchem.2011.169235
Cervia-Hasler, Brüningk, Hoch, Fan, Muzio et al., Persistent complement dysregulation with signs of thromboinflammation in active Long Covid, Science, doi:10.1126/science.adg7942
De Lima, Moraes, Barbosa, Bombassaro, Palma et al., Association of heme-oxygenase 1, hemopexin, and heme levels with markers of disease severity in COVID-19, Exp Biol Med, doi:10.1177/15353702221139185
Erickson, Huang, Allen, Ireland, Roth et al., SARS-CoV-2 infection of human lung epithelial cells induces TMPRSS-mediated acute fibrin deposition, Nat Commun
Fessler, Summer, Surfactant lipids at the host-environment interface. Metabolic sensors, suppressors, and effectors of inflammatory lung disease, Am J Respir Cell Mol Biol
Gandhi, Lynch, Rio, Mild or Moderate Covid-19, New England Journal of Medicine
Gao, Ji, Burla, Wenk, Torta et al., LICAR: An Application for Isotopic Correction of Targeted Lipidomic Data Acquired with Class-Based Chromatographic Separations Using Multiple Reaction Monitoring, Anal Chem, doi:10.1021/acs.analchem.0c04565
Günther, Siebert, Schmidt, Ziegler, Grimminger et al., Surfactant alterations in severe pneumonia, acute respiratory distress syndrome, and cardiogenic lung edema, Am J Respir Crit Care Med, doi:10.1164/ajrccm.153.1.8542113
He, Deng, Li, Coronavirus disease 2019: What we know?, J Med Virol, doi:10.1002/jmv.25766
Hirdman, Bodén, Kjellström, Fraenkel, Olm et al., Proteomic characteristics and diagnostic potential of exhaled breath particles in patients with COVID-19, Clin Proteomics, doi:10.1186/s12014-023-09403-2
Karki, Birukov, Oxidized phospholipids in healthy and diseased lung endothelium, Cells
King, Bates, Berger, Calverley, De Melo et al., Technical standards for respiratory oscillometry, Eur Respir J, doi:10.1183/13993003.00753-2019
Kjellberg, Holm, Berguerand, Sandén, Schiöler et al., Impaired function in the lung periphery following COVID-19 is associated with lingering breathing difficulties, Physiol Rep, doi:10.14814/phy2.15918
Kokelj, Östling, Georgi, Fromell, Ekdahl et al., Smoking induces sex-specific changes in the small airway proteome, Respir Res, doi:10.1186/s12931-021-01825-6
Larsson, Bake, Wallin, Hammar, Almstrand et al., The effect of exhalation flow on endogenous particle emission and phospholipid composition, Respiratory Physiology & Neurobiology
Larsson, Holz, Koster, Postle, Olin et al., Exhaled breath particles as a novel tool to study lipid composition of epithelial lining fluid from the distal lung, BMC Pulmonary Medicine
Lindahl, Reijula, Malmberg, Aro, Vasankari et al., Small airway function in Finnish COVID-19 survivors, Respir Res, doi:10.1186/s12931-021-01830-9
Lipcsey, Persson, Eriksson, Blom, Fromell et al., The Outcome of Critically Ill COVID-19 Patients Is Linked to Thromboinflammation Dominated by the Kallikrein/Kinin System, Front Immunol
Marion-Letellier, Savoye, Ghosh, Polyunsaturated fatty acids and inflammation, IUBMB Life, doi:10.1002/iub.1428
Martens, Van Mol, Wauters, Wauters, Gangnus et al., Dysregulation of the kallikrein-kinin system in bronchoalveolar lavage fluid of patients with severe COVID-19, EBioMedicine, doi:10.1016/j.ebiom.2022.104195
Mcdonnell, Wincup, Buchholz, Pericleous, Giles et al., The role of beta-2-glycoprotein I in health and disease associating structure with function: More than just APS, Blood Rev, doi:10.1016/j.blre.2019.100610
Meletis, Tychala, Ntritsos, Verrou, Savvidou et al., Variant-Related Differences in Laboratory Biomarkers among Patients Affected with Alpha, Delta and Omicron: A Retrospective Whole Viral Genome Sequencing and Hospital-Setting Cohort Study, Biomedicines, doi:10.3390/biomedicines11041143
Mendoza, Saha, Momeni, Gabutan, Alawad et al., Ephrin-A1 and the sheddase ADAM12 are upregulated in COVID-19, Heliyon, doi:10.1016/j.heliyon.2021.e07200
Nilsson, Sim, Lea, Fremeaux-Bacchi, Blom, Complement factor I in health and disease, Mol Immunol, doi:10.1016/j.molimm.2011.04.004
Numata, Kandasamy, Voelker, The anti-inflammatory and antiviral properties of anionic pulmonary surfactant phospholipids, Immunol Rev, doi:10.1111/imr.13207
Numata, Voelker, Anti-inflammatory and anti-viral actions of anionic pulmonary surfactant phospholipids, Biochim Biophys Acta Mol Cell Biol Lipids, doi:10.1016/j.bbalip.2022.159139
Oostveen, Boda, Van Der Grinten, James, Young et al., Respiratory impedance in healthy subjects: baseline values and bronchodilator response, Eur Respir J, doi:10.1183/09031936.00126212
Ousaka, Nishibori, Is hemolysis a novel therapeutic target in COVID-19?, Front Immunol
Pierce, Shen, Cintron, Hiebert, Post-COVID-19 Syndrome, Nurs Res
Rezaie, Giri, Antithrombin: An anticoagulant, anti-inflammatory and antibacterial serpin, J Thromb Haemost, doi:10.1111/jth.14724
Schousboe, Ronit, Nielsen, Benfield, Wiese et al., Reduced levels of pulmonary surfactant in COVID-19 ARDS, Sci Rep
Sinkovits, Mező, Réti, Müller, Iványi et al., Complement Overactivation and Consumption Predicts In-Hospital Mortality in SARS-CoV-2 Infection, Front Immunol
Tamminen, Kerimov, Viskari, Aittoniemi, Syrjänen et al., Lung function during and after acute respiratory infection in COVID-19 positive and negative outpatients, Eur Respir J, doi:10.1183/13993003.02837-2021
Taube, Thurman, Takeda, Joetham, Miyahara et al., Factor B of the alternative complement pathway regulates development of airway hyperresponsiveness and inflammation, Proc Natl Acad Sci U S A, doi:10.1073/pnas.0602357103
Tolosano, Altruda, Hemopexin: Structure, Function, and Regulation, DNA and Cell Biology
Vijayakumar, Boustani, Ogger, Papadaki, Tonkin et al., Immuno-proteomic profiling reveals aberrant immune cell regulation in the airways of individuals with ongoing post-COVID-19 respiratory disease, Immunity, doi:10.1016/j.immuni.2022.01.017
Viklund, Bake, Hussain-Alkhateeb, Akdeva, Larsson et al., Current smoking alters phospholipid-and surfactant protein A levels in small airway lining fluid: An explorative study on exhaled breath, PLoS One, doi:10.1371/journal.pone.0253825
Östling, Van Geest, Olsson, Dahlen, Viklund et al., A novel non-invasive method allowing for discovery of pathologically relevant proteins from small airways, Clin Proteomics, doi:10.1186/s12014-022-09348-y