The Relationship Between Zinc Levels, Length of Hospital Stay, and Mortality in Intensive Care Unit of COVID-19 Patients
et al., Ain Shams Medical Journal, doi:10.21608/asmj.2024.311563.1297, Dec 2024
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Cross-sectional study of 153 COVID-19 patients and 78 healthy controls showing significantly lower serum zinc levels in COVID-19 patients compared to healthy individuals, and an inverse relationship between zinc levels and ICU admission.
Kızılet et al., 1 Dec 2024, retrospective, Turkey, peer-reviewed, 4 authors.
Contact: halitkizilet@adu.edu.tr.
The Relationship Between Zinc Levels, Length of Hospital Stay, and Mortality in Intensive Care Unit of COVID-19 Patients
Ain Shams Medical Journal, doi:10.21608/asmj.2024.311563.1297
Aim: The aim of this study is to evaluate the relationship between disease severity and serum Zinc(Zn) levels in COVID-19 patients.
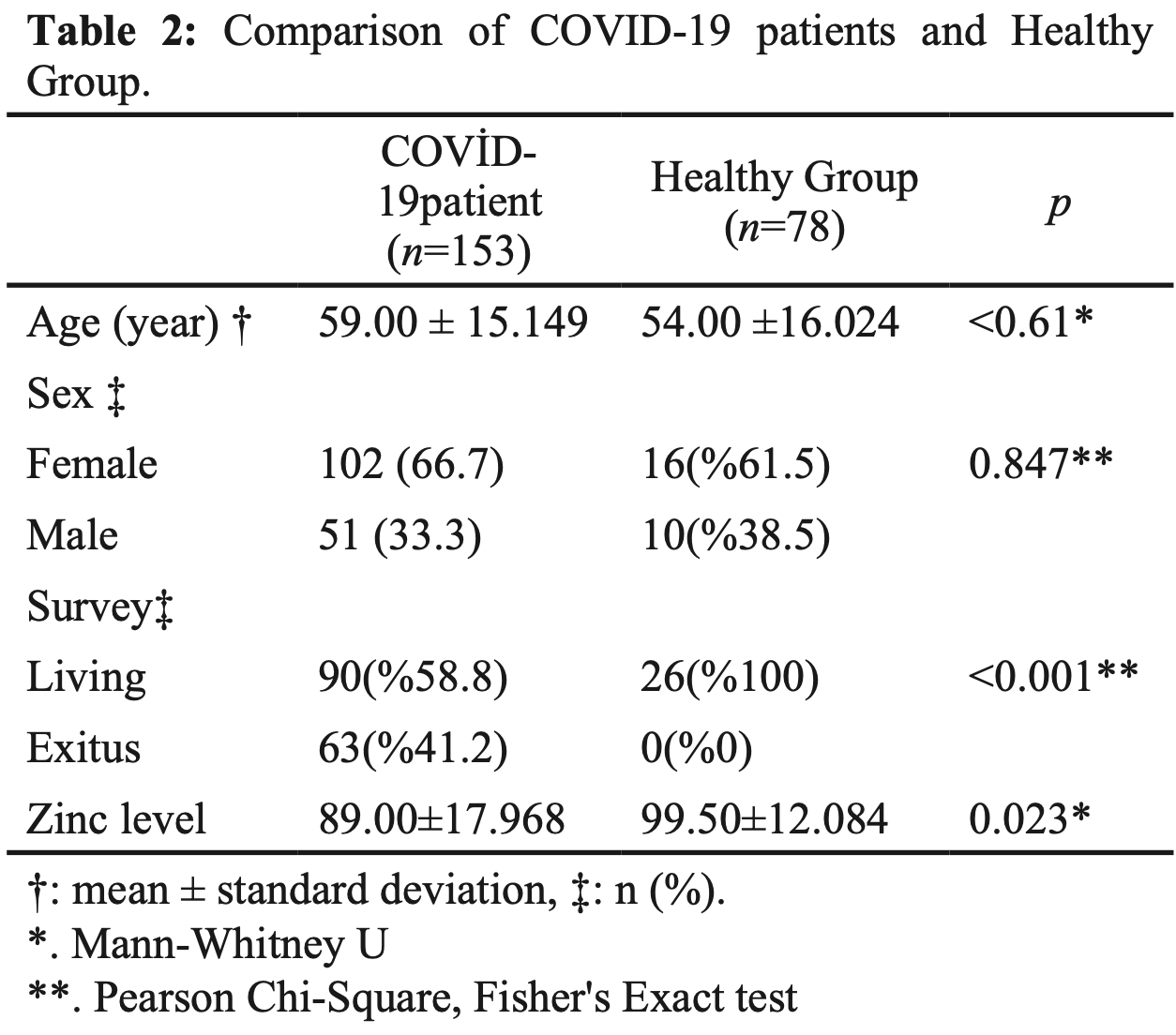
Materials and Methods: The study included 153 COVID-19 patients confirmed by RT-PCR test, were divided into two groups according to the severity of the disease: hospitalized COVID-19 patients (n=81) and intensive care unit patients (n=72). Additionally, 78 healthy controls were included. Serum levels of various biomarkers, including WBC, Neutrophil, Lymphocyte, Monocyte, Platelet, PT, APTT, INR, D-Dimer, CRP, PCT, Ferritin, and Zinc, were measured for all participants. Demographic data and length of hospitalization were also recorded.
Results: The study found significant differences between the groups in age, hospitalizations, chronic disease, and length of hospital stay (p≤0.001). COVID-19 patients had lower median zinc levels (89μg/dl) compared to healthy individuals (99.50μg/ dl), and this difference was statistically significant (p=0.023). As zinc levels increased, the CORADS score decreased (r=-0.248, p=0.031). There was an inverse relationship between zinc level and intensive care unit admission, indicating that lower zinc levels were associated with a higher probability of intensive care hospitalization (r=-0.260, p=0.023).
Conclusion: This study showed that COVID-19 patients had significantly lower zinc levels than healthy individuals. The difference between the average zinc level of COVID-19 patients and the average zinc level of healthy individuals were found to be statistically significant. Additionally, a significant inverse relationship were found between zinc level and intensive care unit hospitalization; As the zinc level decreases, the likelihood of being hospitalized in intensive care increases.
ETHICS COMMITTEE APPROVAL The study design and the consent form were approved by the clinical research ethics committee of Samsun University under protocols (2021/4/8).
INFORMED CONSENT Written informed consent was obtained from all the participants in the study.
CONFLICT OF INTEREST No conflict of interest was declared by the authors.
References
Aci, Erdem, Üstün, Duran, Keskin et al., The Relationship Between Inflammatory Indicators and the Severity of the Disease in Coronavirus Disease, Meandros Med. Dental J, doi:10.4274/meandros.galenos.2021.65477
Aci, Keskin, The impact of COVID-19 on some aspects of laboratory activities, Riv Ital Med Lab, doi:10.23736/S1825-859X.22.00143-8
Bailey, Jr, Black, The epidemiology of global micronutrient deficiencies, Ann Nutr Metab, doi:.org/10.1159/000371618
Barnard, Wong, Bailey, Day, Sidwell et al., Effect of oral gavage treatment with ZnAL42 and other metallo-ion formulations on influenza A H5N1 and H1N1 virus infections in mice, Antivir Chem Chemother, doi:.org/10.1177/095632020701800302
Bilgin, Basbulut, Baklacioglu, Keskin, Aci, Could SARS-CoV-2 Trigger the Formation of Antinuclear Antibodies?, Turk J Immunol, doi:10.4274/tji.galenos.2022.25238
Chou, Cheng, Lai, Chou, Differential domain structure stability of the severe acute respiratory syndrome coronavirus papain-like protease, Arch Biochem Biophys, doi:.org/10.1016/j.abb.2012.02.015
Doğan, Bal, Çabalak, Dikmen, Yaqoobi et al., Oxidative stress index can be a new marker related to disease severity in COVID-19, Turkish J Biochem, doi:.org/10.1515/tjb-2021-0013
Elham, Azam, Azam, Mostafa, Nasrin et al., Serum vitamin D, calcium, and zinc levels in patients with COVID-19, Clin Nutr ESPEN, doi:.org/10.1016/j.clnesp.2021.03.040
Finzi, Treatment of SARS-CoV-2 with high dose oral zinc salts: A report on four patients, Int J Infect Dis, doi:.org/10.1016/j.ijid.2020.06.006
Gammoh, Rink, Zinc in infection and inflammation, Nutrients, doi:.org/10.3390/nu9060624
Gasmi, Tippairote, Mujawdiya, Peana, Menzel et al., Micronutrients as immunomodulatory tools for COVID-19 management, Clinical Immunology, doi:.org/10.1016/j.clim.2020.108545
Gorji, Ghadiri, Potential roles of micronutrient deficiency and immune system dysfunction in the coronavirus disease 2019 (COVID-19) pandemic, Nutrition, doi:.org/10.1016/j.nut.2020.111047
Güven, Köseoğlu, Lohmann, Samancı, Şahin et al., Peripheral Expression of IL-6, TNF-α and TGF-β1 in Alzheimer's Disease Patients, Turk J Immunol, doi:10.4274/tji.galenos.2024.76598
Haryanto, Suksmasari, Wintergerst, Maggini, Multivitamin supplementation supports immune function and ameliorates conditions triggered by reduced air quality, Vitam Min, doi:10.4172/2376-1318.1000128
Heller, Sun, Hackler, Seelig, Seibert et al., Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker, Redox Biol, doi:.org/10.1016/j.redox.2020.101764
Ibs, Rink, Zinc-Altered Immune function, J Nutr, doi:.org/10.1093/jn/133.5.1452S
Jothimani, Kailasam, Danielraj, Nallathambi, Ramachandran et al., COVID-19: Poor outcomes in patients with zinc deficiency, Int J Infect Dis, doi:.org/10.1016/j.ijid.2020.09.014
Junaid, Ejaz, Abdalla, Abosalif, Ullah et al., Effective immune functions of micronutrients against SARS-CoV-2, Nutrients, doi:.org/10.3390/nu12102992
Keskin, Aci, The Relationship Between Some Laboratory Findings and the Prognostic Significance of Phosphorus and 25-(OH) Vitamin D3 Values in SARS-CoV-2 Cases, Avicenna J Med Biochem, doi:10.34172/ajmb.2022.2387
Kitabayashi, Fukada, Kanamoto, Ohashi, Hojyo et al., Zinc suppresses Th17 development via inhibition of STAT3 activation, Int Immunol
Maggini, Beveridge, Sorbara, Senatore, Feeding the immune system: The role of micronutrients in restoring resistance to infections, CAB Rev, doi:10.1079/PAVSNNR20083098
Maggini, Pierre, Calder, Immune function and micronutrient requirements change over the life course, Nutrients, doi:.org/10.3390/nu10101531
Majkowska-Wojciechowska, Kowalski, Allergens, air pollutants and immune system function in the era of global warming. Air pollution-monitoring, modelling, health and control
Maywald, Wang, Rink, Zinc supplementation plays a crucial role in T helper 9 differentiation in allogeneic immune reactions and non-activated T cells, J Trace Elem Med Biol, doi:.org/10.1016/j.jtemb.2018.02.004
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., COVID-19: consider cytokine storm syndromes and immunosuppression, Lancet, doi:10.1016/S0140-6736(20)30628-0
Mossink, Zinc as nutritional intervention and prevention measure for COVID-19 disease, BMJ Nutr Prev Heal, doi:10.1136/bmjnph-2020-000095
Ms, Mottaleb, In search for effective and safe drugs against SARS-CoV-2: Part II] The role of selected salts and organometallics of copper, zinc, selenium, and iodine food supplements, ChemRxiv, doi:10.26434/chemrxiv.12234743.v1
Pal, Squitti, Picozza, Pawar, Rongioletti et al., Zinc and COVID-19: basis of current clinical trials, Biol Trace Elem Res, doi:.org/10.1007/s12011-020-02437-9
Ponti, Maccaferri, Ruini, Tomasi, Ozben, Biomarkers associated with COVID-19 disease progression, Crit Rev Clin Lab Sci, doi:.org/10.1080/10408363.2020.1770685
Prompetchara, Ketloy, Palaga, Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic, Asian Pac J Allergy Immunol, doi:10.12932/ap-200220-0772
Quiles, Rivas-Garcia, Varela-López, Llopis, Battino et al., Do nutrients and other bioactive molecules from foods have anything to say in the treatment against COVID-19?, Environ Res, doi:.org/10.1016/j.envres.2020.110053
Rosenkranz, Maywald, Hilgers, Brieger, Clarner et al., Induction of regulatory T cells in Th1-/Th17-driven experimental autoimmune encephalomyelitis by zinc administration, J Nutr Biochem, doi:.org/10.1016/j.jnutbio.2015.11.010
Rosenkranz, Metz, Maywald, Hilgers, Weßels et al., Zinc supplementation induces regulatory T cells by inhibition of Sirt-1 deacetylase in mixed lymphocyte cultures, Mol Nutr Food Res, doi:.org/10.1002/mnfr.201500524
Shankar, Prasad, Zinc and immune function: The biological basis of altered resistance to infection, Am J Clin Nutr, doi:.org/10.1093/ajcn/68.2.447S
Shanmugaraj, Siriwattananon, Wangkanont, Phoolcharoen, Perspectives on monoclonal antibody therapy as potential therapeutic intervention for Coronavirus disease-19 (COVID-19), Asian Pac J Allergy Immunol, doi:10.12932/ap-200220-0773
Shi, Wang, Shao, Huang, Gan et al., COVID-19 infection: the perspectives on immune responses, Cell Death Differ, doi:10.1038/s41418-020-0530-3
Skalny, Rink, Ajsuvakova, Aschner, Gritsenko et al., Zinc and respiratory tract infections: Perspectives for COVID-19, Int J Mol Med, doi:.org/10.3892/ijmm.2020.4575
Skalny, Timashev, Aschner, Aaseth, Chernova et al., Serum zinc, copper, and other biometals are associated with COVID-19 severity markers, Metabolites, doi:10.3390/metabo11040244
Vallee, Falchuk, The biochemical basis of zinc physiology, Physiological reviews, doi:.org/10.1152/physrev.1993.73.1.79
Velthuis, Van Den Worm, She, Sims, Baric et al., Zn2+ inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture, PLoS Pathog, doi:.org/10.1371/journal.ppat.1001176
Vogel-González, Talló-Parra, Herrera-Fernández, Pérez-Vilaró, Chillón et al., Low zinc levels at admission associates with poor clinical outcomes in SARS-CoV-2 infection, Nutrients, doi:.org/10.3390/nu13020562
Warnes, Little, Keevil, Human coronavirus 229E remains infectious on common touch surface materials, mBio, doi:10.1128/mBio.01697-15
Wintergerst, Maggini, Hornig, Contribution of selected vitamins and trace elements to immune function, Ann Nutr Metab, doi:10.1159/000107673
Wintergerst, Maggini, Hornig, Dh, Immuneenhancing role of vitamin C and zinc and effect on clinical conditions, Ann Nutr Metab, doi:.org/10.1159/000090495
Wu, Lewis, Pae, Meydani, Nutritional modulation of immune function: Analysis of evidence, mechanisms, and clinical relevance, Front Immunol, doi:10.3389/fimmu.2018.03160
Yasui, Yasui, Suzuki, Saitou, Yamamoto et al., Analysis of the predictive factors for a critical illness of COVID-19 during treatmentrelationship between serum zinc level and critical illness of COVID-19, Int J Infect Dis, doi:.org/10.1016/j.ijid.2020.09.008
Yigit, Tural, Aci, Sezer, Vascular endothelial growth factor gene insertion/deletion polymorphism is associated with Vitamin D level in Turkish patients with coronavirus disease 2019, Rev. Assoc. Med. Bras
Zhang, Wu, Li, Zhao, Wang, Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality, Int J Antimicrob Agents, doi:.org/10.1016/j.ijantimicag.2020.105954
DOI record:
{
"DOI": "10.21608/asmj.2024.311563.1297",
"ISSN": [
"2735-3540"
],
"URL": "http://dx.doi.org/10.21608/asmj.2024.311563.1297",
"author": [
{
"affiliation": [],
"family": "Kızılet",
"given": "Halit",
"sequence": "first"
},
{
"affiliation": [],
"family": "ACİ",
"given": "RECAİ",
"sequence": "additional"
},
{
"affiliation": [],
"family": "KESKIN",
"given": "ADEM",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Duran",
"given": "Utku",
"sequence": "additional"
}
],
"container-title": "Ain Shams Medical Journal",
"container-title-short": "Ain Shams Medical Journal",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"asmj.journals.ekb.eg"
]
},
"created": {
"date-parts": [
[
2025,
2,
2
]
],
"date-time": "2025-02-02T09:36:06Z",
"timestamp": 1738488966000
},
"deposited": {
"date-parts": [
[
2025,
2,
2
]
],
"date-time": "2025-02-02T09:52:49Z",
"timestamp": 1738489969000
},
"indexed": {
"date-parts": [
[
2025,
2,
3
]
],
"date-time": "2025-02-03T05:12:42Z",
"timestamp": 1738559562326,
"version": "3.35.0"
},
"is-referenced-by-count": 0,
"issue": "4",
"issued": {
"date-parts": [
[
2024,
12,
1
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2024,
12,
1
]
]
},
"published-print": {
"date-parts": [
[
2024,
12,
1
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://asmj.journals.ekb.eg/article_407430_51863f97053930980d1247aa6b0c1b34.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "9060",
"original-title": [],
"page": "822-830",
"prefix": "10.21608",
"published": {
"date-parts": [
[
2024,
12,
1
]
]
},
"published-online": {
"date-parts": [
[
2024,
12,
1
]
]
},
"published-print": {
"date-parts": [
[
2024,
12,
1
]
]
},
"publisher": "Egyptian Knowledge Bank",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://asmj.journals.ekb.eg/article_407430.html"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "The Relationship Between Zinc Levels, Length of Hospital Stay, and Mortality in Intensive Care Unit of COVID-19 Patients",
"type": "journal-article",
"update-policy": "https://doi.org/10.21608/crossmark_policy",
"volume": "75"
}
