SARS-CoV-2 infection in hiPSC-derived neurons is cathepsin-dependent and causes differential accumulation of HIF1ɑ and phosphorylated tau
et al., Molecular Therapy Nucleic Acids, doi:10.1016/j.omtn.2025.102726, Dec 2025
In vitro study showing that cathepsin B inhibitor CA-074-ME blocks SARS-CoV-2 infection in human induced pluripotent stem cell (hiPSC)-derived neurons.
Kettunen et al., 31 Dec 2025, Finland, peer-reviewed, 17 authors.
Contact: taisia.rolova@helsinki.fi, giuseppe.balistreri@helsinki.fi.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
SARS-CoV-2 infection in hiPSC-derived neurons is cathepsin-dependent and causes differential accumulation of HIF1ɑ and phosphorylated tau
Molecular Therapy Nucleic Acids, doi:10.1016/j.omtn.2025.102726
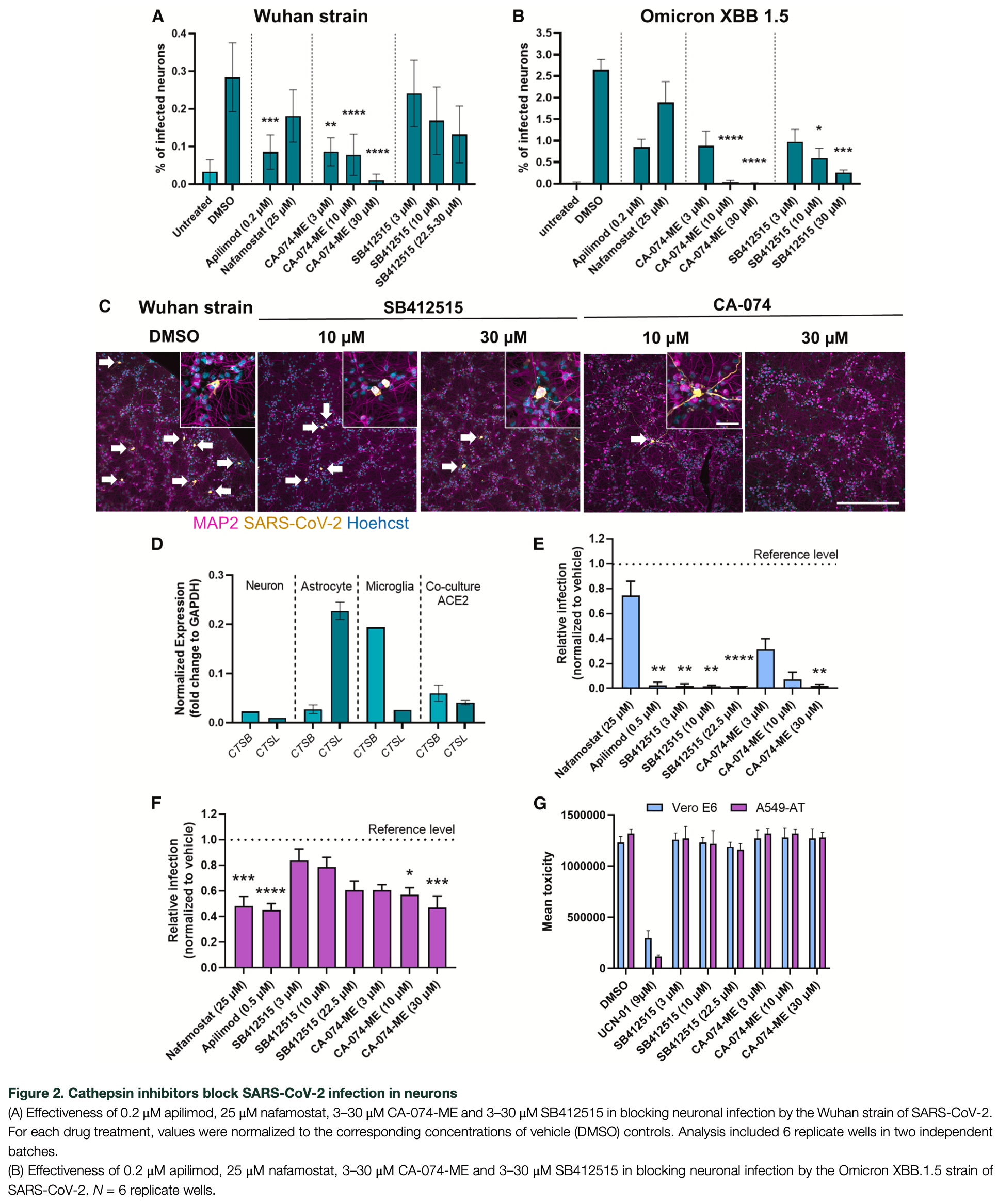
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been shown to infect areas of the human brain and a subset of neurons in vitro. We have previously demonstrated that the virus enters human induced pluripotent stem cell (hiPSC)-derived neurons via an endosomallysosomal pathway. Here, we show that neuronal infection with both SARS-CoV-2 Wuhan and Omicron XBB.1.5 variants is dependent on cathepsins and can be blocked by an inhibitor of cathepsin B. The result was reproducible in non-transgenic hiPSC-derived cortical organoids. We further show that SARS-CoV-2 can replicate in neuron cultures, but the infectivity of the newly produced virions declined at 24 h post-infection despite a further increase in released viral RNA at later time points. The number of infected neurons decreased within five days, suggesting virus-induced neuronal cell death. The infection also caused the accumulation of the hypoxia-inducible stress factor HIF1-α in infected neurons under normoxia. Finally, expanding previous findings, in SARS-CoV-2 infected neurons, the microtubule-associated protein tau was hyperphosphorylated at multiple loci, including S202/T205, and mislocalized to the soma of infected 2D-neuronal cultures, but not in 3D-organotypic models. Hence, the neurodegenerative potential of SARS-CoV-2 infection should be carefully considered in different infection models.
AUTHOR CONTRIBUTIONS P.K.: design, data collection and analysis (2D cultures), interpretation, drafting of the article; J.R.: design, data collection and analysis (2D cultures), drafting of the article; T.Q.: data collection and analysis (2D cultures); R.O.: data collection (2D cultures); S. H.S.: data collection (organoids); S.M.: data collection (organoids); S.M.; image analysis (organoids); L.P.: image analysis of microglial cells; S.D.N.: analysis and data collection of organoid immunohistochemistry; A.K.: guided the work for immunohistochemistry of organoids, provided infrastructures and funding; E.W.: guided the work, provided infrastructures and provided funding (organoids); M.J.: guided the work, provided infrastructures and provided funding (organoids); J.K.: design, interpretation, drafting and commenting of the article, guided the work, provided infrastructures and provided funding; T.R.: design, data collection and analysis (2D cultures), interpretation, drafting and commenting of the article, guided the work; G.B.: design, analysis, interpretation, drafting and commenting of the article, guided the work, provided infrastructures and provided funding.
DECLARATION OF INTERESTS We declare no competing interests.
SUPPLEMENTAL INFORMATION Supplemental information can be found online at https://doi.org/10.1016/j.omtn.2025. 102726 .
References
Albornoz, Amarilla, Modhiran, Parker, Li et al., SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein, Mol. Psychiatry
Amarilla, Modhiran, Setoh, Peng, Sng et al., An Optimized High-Throughput Immuno-Plaque Assay for SARS-CoV-2, Front. Microbiol
Andrews, Mukhtar, Eze, Simoneau, Ross et al., Tropism of SARS-CoV-2 for human cortical astrocytes, Proc. Natl. Acad. Sci
Baay-Guzman, Bebenek, Zeidler, Hernandez-Pando, Vega et al., HIF-1 expression is associated with CCL2 chemokine expression in airway inflammatory cells: implications in allergic airway inflammation, Respir. Res
Bauer, Lendemeijer, Leijten, Embregts, Rockx et al., Replication Kinetics, Cell Tropism, and Associated Immune Responses in SARS-CoV-2-and H5N1 Virus-Infected Human Induced Pluripotent Stem Cell-Derived Neural Models, mSphere
Beckman, Bonillas, Diniz, Ott, Roh et al., SARS-CoV-2 infects neurons and induces neuroinflammation in a non-human primate model of COVID-19, Cell Rep
Bernhagen, Krohn, Lue, Gregory, Zernecke et al., MIF is a noncognate ligand of CXC chemokine receptors in inflammatory and atherogenic cell recruitment, Nat. Med
Bollavaram, Leeman, Lee, Kulkarni, Upshaw et al., Multiple sites on SARS-CoV -2 spike protein are susceptible to proteolysis by cathepsins B, K, L, S, and V, Protein Sci
Bullen, Hogberg, Bahadirli-Talbott, Bishai, Hartung et al., Infectability of Human BrainSphere Neurons Suggests Neurotropism of SARS-CoV-2, ALTEX
Cambier, Gouwy, Proost, The chemokines CXCL8 and CXCL12: molecular and functional properties, role in disease and efforts towards pharmacological intervention, Cell. Mol. Immunol
Cantuti-Castelvetri, Ojha, Pedro, Djannatian, Franz et al., Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity, Science
Chan, Huang, Hu, Chai, Shi et al., Altered host protease determinants for SARS-CoV-2 Omicron, Sci. Adv
Chen, Wang, Yu, Howard, French et al., The Spatial and Cell-Type Distribution of SARS-CoV-2 Receptor ACE2 in the Human and Mouse Brains, Front. Neurol
Cho, Yoon, Choi, Kang, Jang et al., CA-074Me, a cathepsin B inhibitor, decreases APP accumulation and protects primary rat cortical neurons treated with okadaic acid, Neurosci. Lett
Crunfli, Carregari, Veras, Silva, Nogueira et al., Morphological, cellular, and molecular basis of brain infection in COVID-19 patient, Proc. Natl. Acad. Sci
Di Primio, Quaranta, Mignanelli, Siano, Bimbati et al., Severe acute respiratory syndrome coronavirus 2 infection leads to Tau pathological signature in neurons, PNAS Nexus
Douaud, Lee, Alfaro-Almagro, Arthofer, Wang et al., SARS-CoV-2 is associated with changes in brain structure in UK Biobank, Nature
Duan, Tang, Nair, Zhang, Qiu et al., An airway organoid-based screen identifies a role for the HIF1α-glycolysis axis in SARS-CoV-2 infection, Cell Rep
Duette, Pereyra Gerber, Rubione, Perez, Landay et al., Induction of HIF-1α by HIV-1 Infection in CD4+ T Cells Promotes Viral Replication and Drives Extracellular Vesicle-Mediated Inflammation, mBio
Eberle, Coronado, Gering, Sommerhage, Korostov et al., Tau protein aggregation associated with SARS-CoV-2 main protease, PLoS One
Fink, Kazlauskas, Poellinger, Ebbesen, Zachar, Identification of a tightly regulated hypoxia-response element in the promoter of human plasminogen activator inhibitor-1, Blood
Goshua, Pine, Meizlish, Chang, Zhang et al., Endotheliopathy in COVID-19associated coagulopathy: evidence from a single-centre, cross-sectional study, Lancet. Haematol
Guo, Zhu, Zhang, Meng, Zhu et al., Nuclear translocation of HIF-1α induced by influenza A (H1N1) infection is critical to the production of proinflammatory cytokines, Emerg. Microbes Infect
Hai, Ren, Zhang, Yang, Cao et al., HIF-1α serves as a co-linker between AD and T2DM, Biomed. Pharmacother
Hashimoto, Sakamoto, Deguchi, Yi, Sano et al., Dual inhibition of TMPRSS2 and Cathepsin B prevents SARS-CoV-2 infection in iPS cells, Mol. Ther. Nucleic Acids
Haverty, Mccormack, Evans, Purves, O'reilly et al., SARS-CoV-2 infects neurons, astrocytes, choroid plexus epithelial cells and pericytes of the human central nervous system in vitro, J. Gen. Virol
Hinojosa, Garcia-Bueno, Leza, Madrigal, CCL2/MCP-1 modulation of microglial activation and proliferation, J. Neuroinflammation
Ianevski, Yao, Lysvand, Grødeland, Legrand et al., Nafamostat-Interferon-α Combination Suppresses SARS-CoV-2 Infection In Vitro and In Vivo by Cooperatively Targeting Host TMPRSS2, Viruses
Jackson, Farzan, Chen, Choe, Mechanisms of SARS-CoV-2 entry into cells, Nat. Rev. Mol. Cell Biol
Jacob, Pather, Huang, Zhang, Wong et al., Human Pluripotent Stem Cell-Derived Neural Cells and Brain Organoids Reveal SARS-CoV-2 Neurotropism Predominates in Choroid Plexus Epithelium, Cell Stem Cell
Jahani, Dokaneheifard, Mansouri, Hypoxia: A key feature of COVID-19 launching activation of HIF-1 and cytokine storm, J. Inflamm
Jeon, Kim, Kim, Lee, Lee et al., Plasminogen activator inhibitor type 1 regulates microglial motility and phagocytic activity, J. Neuroinflammation
Jeong, Lyu, Kim, Chung, Yoon et al., SARS-CoV-2 Infection of Microglia Elicits Proinflammatory Activation and Apoptotic Cell Death, Microbiol. Spectr
Jiang, Li, Wang, Chen, Liang et al., SARS-CoV-2 spike S1 protein induces microglial NLRP3-dependent neuroinflammation and cognitive impairment in mice, Exp. Neurol
Jin, Brockmeier, Otterbach, Metzen, New Insight into the SDF-1/CXCR4 Axis in a Breast Carcinoma Model: Hypoxia-Induced Endothelial SDF-1 and Tumor Cell CXCR4 Are Required for Tumor Cell Intravasation, Mol. Cancer Res
Jäntti, Sitnikova, Ishchenko, Shakirzyanova, Giudice et al., Microglial amyloid beta clearance is driven by PIEZO1 channels, J. Neuroinflammation
Kant, Kareinen, Ojha, Strandin, Saber et al., Complete Protection from SARS-CoV-2 Lung Infection in Mice Through Combined Intranasal Delivery of PIKfyve Kinase and TMPRSS2 Protease Inhibitors, doi:10.1101/2023.07.19.549731
Kettunen, Koistinaho, Rolova, Contribution of CNS and extra-CNS infections to neurodegeneration: a narrative review, J. Neuroinflammation
Kettunen, Lesnikova, Räsänen, Ojha, Palmunen et al., SARS-CoV-2 Infection of Human Neurons Is TMPRSS2 Independent, Requires Endosomal Cell Entry, and Can Be Blocked by Inhibitors of Host Phosphoinositol-5 Kinase, J. Virol
Koch, Uckeley, Doldan, Stanifer, Boulant et al., TMPRSS2 expression dictates the entry route used by SARS-CoV-2 to infect host cells, EMBO J
Kong, Montano, Corley, Helmy, Kobayashi et al., Neuropilin-1 Mediates SARS-CoV-2 Infection of Astrocytes in Brain Organoids, Inducing Inflammation Leading to Dysfunction and Death of Neurons, mBio
Lee, Bae, Jeong, Kim, Kim, Hypoxia-inducible factor (HIF-1)α: its protein stability and biological functions, Exp. Mol. Med
Li, Meyerholz, Bartlett, Mccray, The TMPRSS2 Inhibitor Nafamostat Reduces SARS-CoV-2 Pulmonary Infection in Mouse Models of COVID-19, mBio
Liu, Liu, Iqbal, Grundke-Iqbal, Gong, Decreased glucose transporters correlate to abnormal hyperphosphorylation of tau in Alzheimer disease, FEBS Lett
Lopez-Leon, Wegman-Ostrosky, Perelman, Sepulveda, Rebolledo et al., More than 50 long-term effects of COVID-19: a systematic review and meta-analysis, Sci. Rep
Luczo, Edwards, Ardipradja, Suen, Au et al., SARS-CoV and SARS-CoV-2 display limited neuronal infection and lack the ability to transmit within synaptically connected axons in stem cell-derived human neurons, J. Neurovirol
Lukiw, Pogue, Hill, SARS-CoV-2 Infectivity and Neurological Targets in the Brain, Cell. Mol. Neurobiol
López-Rodríguez, Kirillov, Krug, Mesri, Andreansky, A role of hypoxia-inducible factor 1 alpha in Murine Gammaherpesvirus 68 (MHV68) lytic replication and reactivation from latency, PLoS Pathog
Martínez-Mármol, Giordano-Santini, Kaulich, Cho, Przybyla et al., SARS-CoV-2 infection and viral fusogens cause neuronal and glial fusion that compromises neuronal activity, Sci. Adv
Mathys, Davila-Velderrain, Peng, Gao, Mohammadi et al., Single-cell transcriptomic analysis of Alzheimer's disease, Nature
Matschke, Lütgehetmann, Hagel, Sperhake, Schröder et al., Neuropathology of patients with COVID-19 in Germany: a post-mortem case series, Lancet Neurol
May, Chu, Zielinski, Single-Cell RNA Sequencing Reveals HIF1A as a Severity-Sensitive Immunological Scar in Circulating Monocytes of Convalescent Comorbidity-Free COVID-19 Patients, Cells
Mcfarlane, Nicholl, Sutherland, Preston, Interaction of the human cytomegalovirus particle with the host cell induces hypoxia-inducible factor 1 alpha, Virology
Meinhardt, Radke, Dittmayer, Franz, Thomas et al., Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19, Nat. Neurosci
Mellott, Tseng, Drelich, Fajtová, Chenna et al., A Clinical-Stage Cysteine Protease Inhibitor blocks SARS-CoV-2 Infection of Human and Monkey Cells, ACS Chem. Biol
Meng, Abdullahi, Ferreira, Goonawardane, Saito et al., Altered TMPRSS2 usage by SARS-CoV-2 Omicron impacts infectivity and fusogenicity, Nature
Meng, Zhu, Yang, Zhang, Jin et al., HIF-1α promotes virus replication and cytokine storm in H1N1 virusinduced severe pneumonia through cellular metabolic reprogramming, Virol. Sin
Mignolet, Gilloteaux, Halloin, Gueibe, Willemart et al., Viral Entry Inhibitors Protect against SARS-CoV-2-Induced Neurite Shortening in Differentiated SH-SY5Y Cells, Viruses
Montaser, Lalmanach, Mach, CA-074, But Not Its Methyl Ester CA-074Me, Is a Selective Inhibitor of Cathepsin B within Living Cells, Biol. Chem
Muller, Janovjak, Miserez, Dobbie, Processing of gene expression data generated by quantitative real-time RT-PCR, Biotechniques
Neddens, Temmel, Flunkert, Kerschbaumer, Hoeller et al., Phosphorylation of different tau sites during progression of Alzheimer's disease, Acta Neuropathol. Commun
Nyström, Hammarström, Amyloidogenesis of SARS-CoV-2 Spike Protein, J. Am. Chem. Soc
Olajide, Iwuanyanwu, Adegbola, Al-Hindawi, SARS-CoV-2 Spike Glycoprotein S1 Induces Neuroinflammation in BV-2 Microglia, Mol. Neurobiol
Olivarria, Cheng, Furman, Pachow, Hohsfield et al., Microglia Do Not Restrict SARS-CoV-2 Replication following Infection of the Central Nervous System of K18-Human ACE2 Transgenic Mice, J. Virol
Ozkaya, Lalo� Glu, Gul, Çelik, CXCL12/CXCR4 as a potential axis in diagnosis and predicting disease severity in COVID-19 patients: a new perspective, Turk. J. Biochem
Pedrosa, Goto-Silva, Temerozo, Souza, Vitória et al., Non-permissive SARS-CoV-2 infection in human neurospheres, Stem Cell Res
Pellegrini, Albecka, Mallery, Kellner, Paul et al., SARS-CoV-2 Infects the Brain Choroid Plexus and Disrupts the Blood-CSF Barrier in Human Brain Organoids, Cell Stem Cell
Puelles, Lütgehetmann, Lindenmeyer, Sperhake, Wong et al., Multiorgan and Renal Tropism of SARS-CoV-2, N. Engl. J. Med. Overseas. Ed
Ramani, Müller, Ostermann, Gabriel, Abida-Islam et al., SARS-CoV-2 targets neurons of 3D human brain organoids, EMBO J
Ren, Zhang, Han, Zhang, Zhu et al., Influenza A virus (H1N1) triggers a hypoxic response by stabilizing hypoxia-inducible factor-1α via inhibition of proteasome, Virology
Rihn, Merits, Bakshi, Turnbull, Wickenhagen et al., A plasmid DNA-launched SARS-CoV-2 reverse genetics system and coronavirus toolkit for COVID-19 research, PLoS Biol
Rosendal, Mihai, Becker, Das, Frängsmyr et al., Serine Protease Inhibitors Restrict Host Susceptibility to SARS-CoV-2 Infections, mBio
Rusanen, Kareinen, Levanov, Mero, Pakkanen et al., A 10-Minute "Mix and Read" Antibody Assay for SARS-CoV-2, Viruses
Saber, Shaker, Sng, Yak, Morrison et al., Inhibition of host N-myristoylation compromises the infectivity of SARS-CoV-2 due to Golgi-bypassing egress from lysosomes and endoplasmic reticulum, Preprint at bioRxiv, doi:10.1101/2023.03.03.530798
Samudyata, Oliveira, Malwade, Rufino De Sousa, Goparaju et al., SARS-CoV-2 promotes microglial synapse elimination in human brain organoids, Mol. Psychiatry
Shahbaz, Bozorgmehr, Lu, Osman, Sligl et al., Analysis of SARS-CoV-2 isolates, namely the Wuhan strain, Delta variant, and Omicron variant, identifies differential immune profiles, Microbiol. Spectr
Shaker, Slonchak, Al-Mhanawi, Morrison, Sng et al., Choroid plexus defects in Down syndrome brain organoids enhance neurotropism of SARS-CoV-2, Sci. Adv
Shin, Fan, Par-Young, Piecychna, Leng et al., MIF is a common genetic determinant of COVID-19 symptomatic infection and severity, QJM
Singh, Anshita, Ravichandiran, MCP-1: Function, regulation, and involvement in disease, Int. Immunopharmacol
Song, Zhang, Israelow, Lu-Culligan, Prado et al., Neuroinvasion of SARS-CoV-2 in human and mouse brain, J. Exp. Med
Steverding, The Cathepsin B-Selective Inhibitors CA-074 and CA-074Me Inactivate Cathepsin L Under Reducing Conditions, Open Enzym. Inhib. J
Stirling, Swain-Bowden, Lucas, Carpenter, Cimini et al., CellProfiler 4: improvements in speed, utility and usability, BMC Bioinf
Tian, Liu, Li, Zhao, Shereen et al., HIF-1α promotes SARS-CoV-2 infection and aggravates inflammatory responses to COVID-19, Signal Transduct. Target. Ther
Van Acker, Saluja, Bhagat, Singh, Song et al., Cathepsin B inhibition prevents trypsinogen activation and reduces pancreatitis severity, Am. J. Physiol. Gastrointest. Liver Physiol
Wang, Chang, Zhang, Zhang, Pyroptotic cell death in SARS-CoV-2 infection: revealing its roles during the immunopathogenesis of COVID-19, Int. J. Biol. Sci
Wang, Zhang, Garcia, Tian, Cui et al., ApoE-Isoform-Dependent SARS-CoV-2 Neurotropism and Cellular Response, Cell Stem Cell
Welford, Bedogni, Gradin, Poellinger, Broome Powell et al., HIF1α delays premature senescence through the activation of MIF, Genes Dev
Wing, Keeley, Zhuang, Lee, Prange-Barczynska et al., Hypoxic and pharmacological activation of HIF inhibits SARS-CoV-2 infection of lung epithelial cells, Cell Rep
Wise, Xi, Purdy, Hypoxia-Inducible Factor 1α (HIF1α) Suppresses Virus Replication in Human Cytomegalovirus Infection by Limiting Kynurenine Synthesis, mBio
Wu, Wei, Liu, Chen, Lisman et al., Analysis of thrombotic factors in severe acute respiratory syndrome (SARS) patients, Thromb. Haemost
Xu, Wang, Song, Wei, He et al., Protective mechanisms of CA074-me (other than cathepsin-B inhibition) against programmed necrosis induced by global cerebral ischemia/reperfusion injury in rats, Brain Res. Bull
Xu, Xie, Al-Aly, Long-term neurologic outcomes of COVID-19, Nat. Med
Yadati, Houben, Bitorina, Shiri-Sverdlov, The Ins and Outs of Cathepsins: Physiological Function and Role in Disease Management, Cells
Yang, Meng, Li, Yong, Fan et al., Neuronal MCP-1 Mediates Microglia Recruitment and Neurodegeneration Induced by the Mild Impairment of Oxidative Metabolism, Brain Pathol
Zhang, Fu, Yu, Shui, Li et al., Treatment with CA-074Me, a Cathepsin B inhibitor, reduces lung interstitial inflammation and fibrosis in a rat model of polymyositis, Lab. Invest
Zhang, Wu, Yang, Dong, Yu, Tauopathies: new perspectives and challenges, Mol. Neurodegener
Zhao, Chen, Cheng, Xu, Yang et al., Deficiency of HIF-1α enhances influenza A virus replication by promoting autophagy in alveolar type II epithelial cells, Emerg. Microbes Infect
Zhao, Yang, Yang, Zhang, Huang et al., Cathepsin L plays a key role in SARS-CoV-2 infection in humans and humanized mice and is a promising target for new drug development, Signal Transduct. Target. Ther
Zhao, Zhu, Zhang, Zhong, Tai et al., Novel cleavage sites identified in SARS-CoV-2 spike protein reveal mechanism for cathepsin L-facilitated viral infection and treatment strategies, Cell Discov
Zuo, Hou, Jin, Chen, Zhan et al., Inhibition of Cathepsins B Induces Neuroprotection Against Secondary Degeneration in Ipsilateral Substantia Nigra After Focal Cortical Infarction in Adult Male Rats, Front. Aging Neurosci
DOI record:
{
"DOI": "10.1016/j.omtn.2025.102726",
"ISSN": [
"2162-2531"
],
"URL": "http://dx.doi.org/10.1016/j.omtn.2025.102726",
"alternative-id": [
"S216225312500280X"
],
"article-number": "102726",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "SARS-CoV-2 infection in hiPSC-derived neurons is cathepsin-dependent and causes differential accumulation of HIF1ɑ and phosphorylated tau"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Molecular Therapy Nucleic Acids"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.omtn.2025.102726"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2025 Published by Elsevier Inc. on behalf of The American Society of Gene and Cell Therapy."
}
],
"author": [
{
"affiliation": [],
"family": "Kettunen",
"given": "Pinja",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ruuska",
"given": "Janika",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Quirin",
"given": "Tania",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ojha",
"given": "Ravi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saber",
"given": "Saber H.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sng",
"given": "Julian D.J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Morrison",
"given": "Sean",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Al-Mhanawi",
"given": "Bahaa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shaker",
"given": "Mohammed R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "De Neck",
"given": "Simon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kipar",
"given": "Anja",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Paavolainen",
"given": "Lassi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wolvetang",
"given": "Ernst",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Joensuu",
"given": "Merja",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Koistinaho",
"given": "Jari",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rolova",
"given": "Taisia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Balistreri",
"given": "Giuseppe",
"sequence": "additional"
}
],
"container-title": "Molecular Therapy Nucleic Acids",
"container-title-short": "Molecular Therapy Nucleic Acids",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"cell.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2025,
10,
1
]
],
"date-time": "2025-10-01T07:19:03Z",
"timestamp": 1759303143000
},
"deposited": {
"date-parts": [
[
2026,
1,
20
]
],
"date-time": "2026-01-20T07:59:27Z",
"timestamp": 1768895967000
},
"funder": [
{
"DOI": "10.13039/501100008413",
"award": [
"240024"
],
"award-info": [
{
"award-number": [
"240024"
]
}
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100008413",
"id-type": "DOI"
}
],
"name": "Instrumentariumin Tiedesäätiö"
},
{
"DOI": "10.13039/100004152",
"award": [
"22.00094"
],
"award-info": [
{
"award-number": [
"22.00094"
]
}
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/100004152",
"id-type": "DOI"
}
],
"name": "Spine Education and Research Institute"
},
{
"DOI": "10.13039/501100000925",
"award": [
"2010917"
],
"award-info": [
{
"award-number": [
"2010917"
]
}
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100000925",
"id-type": "DOI"
}
],
"name": "National Health and Medical Research Council"
},
{
"DOI": "10.13039/501100009047",
"award": [
"335527"
],
"award-info": [
{
"award-number": [
"335527"
]
}
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100009047",
"id-type": "DOI"
}
],
"name": "Strategic Research Council"
},
{
"DOI": "10.13039/501100009047",
"award": [
"362468"
],
"award-info": [
{
"award-number": [
"362468"
]
}
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100009047",
"id-type": "DOI"
}
],
"name": "Strategic Research Council"
},
{
"DOI": "10.13039/100007797",
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/100007797",
"id-type": "DOI"
}
],
"name": "Helsingin Yliopisto"
},
{
"DOI": "10.13039/501100001794",
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100001794",
"id-type": "DOI"
}
],
"name": "University of Queensland"
},
{
"DOI": "10.13039/501100013840",
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100013840",
"id-type": "DOI"
}
],
"name": "Biocenter Finland"
},
{
"DOI": "10.13039/501100006306",
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100006306",
"id-type": "DOI"
}
],
"name": "Sigrid Juséliuksen Säätiö"
},
{
"DOI": "10.13039/501100007352",
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100007352",
"id-type": "DOI"
}
],
"name": "Staatssekretariat für Bildung, Forschung und Innovation"
},
{
"DOI": "10.13039/100015735",
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/100015735",
"id-type": "DOI"
}
],
"name": "Helsinki Institute of Life Science, Helsingin Yliopisto"
},
{
"DOI": "10.13039/501100002341",
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100002341",
"id-type": "DOI"
}
],
"name": "Research Council of Finland"
}
],
"indexed": {
"date-parts": [
[
2026,
1,
20
]
],
"date-time": "2026-01-20T21:22:49Z",
"timestamp": 1768944169185,
"version": "3.49.0"
},
"is-referenced-by-count": 0,
"issue": "4",
"issued": {
"date-parts": [
[
2025,
12
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2025,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
12,
1
]
],
"date-time": "2025-12-01T00:00:00Z",
"timestamp": 1764547200000
}
},
{
"URL": "https://www.elsevier.com/legal/tdmrep-license",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
12,
1
]
],
"date-time": "2025-12-01T00:00:00Z",
"timestamp": 1764547200000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
9,
28
]
],
"date-time": "2025-09-28T00:00:00Z",
"timestamp": 1759017600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S216225312500280X?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S216225312500280X?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "102726",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2025,
12
]
]
},
"published-print": {
"date-parts": [
[
2025,
12
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1038/s41598-021-95565-8",
"article-title": "More than 50 long-term effects of COVID-19: a systematic review and meta-analysis",
"author": "Lopez-Leon",
"doi-asserted-by": "crossref",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.omtn.2025.102726_bib1",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1038/s41591-022-02001-z",
"article-title": "Long-term neurologic outcomes of COVID-19",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "2406",
"journal-title": "Nat. Med.",
"key": "10.1016/j.omtn.2025.102726_bib2",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1016/S1474-4422(20)30308-2",
"article-title": "Neuropathology of patients with COVID-19 in Germany: a post-mortem case series",
"author": "Matschke",
"doi-asserted-by": "crossref",
"first-page": "919",
"journal-title": "Lancet Neurol.",
"key": "10.1016/j.omtn.2025.102726_bib3",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1038/s41593-020-00758-5",
"article-title": "Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19",
"author": "Meinhardt",
"doi-asserted-by": "crossref",
"first-page": "168",
"journal-title": "Nat. Neurosci.",
"key": "10.1016/j.omtn.2025.102726_bib4",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1056/NEJMc2011400",
"article-title": "Multiorgan and Renal Tropism of SARS-CoV-2",
"author": "Puelles",
"doi-asserted-by": "crossref",
"first-page": "590",
"journal-title": "N. Engl. J. Med. Overseas. Ed.",
"key": "10.1016/j.omtn.2025.102726_bib5",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2200960119",
"article-title": "Morphological, cellular, and molecular basis of brain infection in COVID-19 patient.",
"author": "Crunfli",
"doi-asserted-by": "crossref",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "10.1016/j.omtn.2025.102726_bib6",
"volume": "119",
"year": "2022"
},
{
"DOI": "10.1038/s41586-022-04569-5",
"article-title": "SARS-CoV-2 is associated with changes in brain structure in UK Biobank",
"author": "Douaud",
"doi-asserted-by": "crossref",
"first-page": "697",
"journal-title": "Nature",
"key": "10.1016/j.omtn.2025.102726_bib7",
"volume": "604",
"year": "2022"
},
{
"DOI": "10.1016/j.stem.2020.09.016",
"article-title": "Human Pluripotent Stem Cell-Derived Neural Cells and Brain Organoids Reveal SARS-CoV-2 Neurotropism Predominates in Choroid Plexus Epithelium",
"author": "Jacob",
"doi-asserted-by": "crossref",
"first-page": "937",
"journal-title": "Cell Stem Cell",
"key": "10.1016/j.omtn.2025.102726_bib8",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1016/j.stem.2020.10.001",
"article-title": "SARS-CoV-2 Infects the Brain Choroid Plexus and Disrupts the Blood-CSF Barrier in Human Brain Organoids",
"author": "Pellegrini",
"doi-asserted-by": "crossref",
"first-page": "951",
"journal-title": "Cell Stem Cell",
"key": "10.1016/j.omtn.2025.102726_bib9",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1128/mbio.02308-22",
"article-title": "Neuropilin-1 Mediates SARS-CoV-2 Infection of Astrocytes in Brain Organoids, Inducing Inflammation Leading to Dysfunction and Death of Neurons",
"author": "Kong",
"doi-asserted-by": "crossref",
"journal-title": "mBio",
"key": "10.1016/j.omtn.2025.102726_bib10",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1084/jem.20202135",
"article-title": "Neuroinvasion of SARS-CoV-2 in human and mouse brain",
"author": "Song",
"doi-asserted-by": "crossref",
"journal-title": "J. Exp. Med.",
"key": "10.1016/j.omtn.2025.102726_bib11",
"volume": "218",
"year": "2021"
},
{
"DOI": "10.1128/jvi.00144-23",
"article-title": "SARS-CoV-2 Infection of Human Neurons Is TMPRSS2 Independent, Requires Endosomal Cell Entry, and Can Be Blocked by Inhibitors of Host Phosphoinositol-5 Kinase",
"author": "Kettunen",
"doi-asserted-by": "crossref",
"journal-title": "J. Virol.",
"key": "10.1016/j.omtn.2025.102726_bib12",
"volume": "97",
"year": "2023"
},
{
"DOI": "10.1016/j.stem.2020.12.018",
"article-title": "ApoE-Isoform-Dependent SARS-CoV-2 Neurotropism and Cellular Response",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "331",
"journal-title": "Cell Stem Cell",
"key": "10.1016/j.omtn.2025.102726_bib13",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1128/spectrum.01091-22",
"article-title": "SARS-CoV-2 Infection of Microglia Elicits Proinflammatory Activation and Apoptotic Cell Death",
"author": "Jeong",
"doi-asserted-by": "crossref",
"journal-title": "Microbiol. Spectr.",
"key": "10.1016/j.omtn.2025.102726_bib14",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.7150/ijbs.77561",
"article-title": "Pyroptotic cell death in SARS-CoV-2 infection: revealing its roles during the immunopathogenesis of COVID-19",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "5827",
"journal-title": "Int. J. Biol. Sci.",
"key": "10.1016/j.omtn.2025.102726_bib15",
"volume": "18",
"year": "2022"
},
{
"DOI": "10.1038/s41380-022-01786-2",
"article-title": "SARS-CoV-2 promotes microglial synapse elimination in human brain organoids",
"author": "Samudyata",
"doi-asserted-by": "crossref",
"first-page": "3939",
"journal-title": "Mol. Psychiatry",
"key": "10.1016/j.omtn.2025.102726_bib16",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1038/s41380-022-01831-0",
"article-title": "SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein",
"author": "Albornoz",
"doi-asserted-by": "crossref",
"first-page": "2878",
"journal-title": "Mol. Psychiatry",
"key": "10.1016/j.omtn.2025.102726_bib17",
"volume": "28",
"year": "2023"
},
{
"DOI": "10.1007/s12035-021-02593-6",
"article-title": "SARS-CoV-2 Spike Glycoprotein S1 Induces Neuroinflammation in BV-2 Microglia",
"author": "Olajide",
"doi-asserted-by": "crossref",
"first-page": "445",
"journal-title": "Mol. Neurobiol.",
"key": "10.1016/j.omtn.2025.102726_bib18",
"volume": "59",
"year": "2022"
},
{
"DOI": "10.1016/j.expneurol.2024.115020",
"article-title": "SARS-CoV-2 spike S1 protein induces microglial NLRP3-dependent neuroinflammation and cognitive impairment in mice",
"author": "Jiang",
"doi-asserted-by": "crossref",
"journal-title": "Exp. Neurol.",
"key": "10.1016/j.omtn.2025.102726_bib19",
"volume": "383",
"year": "2025"
},
{
"DOI": "10.1073/pnas.2122236119",
"article-title": "Tropism of SARS-CoV-2 for human cortical astrocytes",
"author": "Andrews",
"doi-asserted-by": "crossref",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "10.1016/j.omtn.2025.102726_bib20",
"volume": "119",
"year": "2022"
},
{
"DOI": "10.1016/j.celrep.2022.111573",
"article-title": "SARS-CoV-2 infects neurons and induces neuroinflammation in a non-human primate model of COVID-19",
"author": "Beckman",
"doi-asserted-by": "crossref",
"journal-title": "Cell Rep.",
"key": "10.1016/j.omtn.2025.102726_bib21",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.1126/sciadv.add3867",
"article-title": "Altered host protease determinants for SARS-CoV-2 Omicron",
"author": "Chan",
"doi-asserted-by": "crossref",
"journal-title": "Sci. Adv.",
"key": "10.1016/j.omtn.2025.102726_bib22",
"volume": "9",
"year": "2023"
},
{
"DOI": "10.1038/s41580-021-00418-x",
"article-title": "Mechanisms of SARS-CoV-2 entry into cells",
"author": "Jackson",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "Nat. Rev. Mol. Cell Biol.",
"key": "10.1016/j.omtn.2025.102726_bib23",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.3390/cells9071679",
"article-title": "The Ins and Outs of Cathepsins: Physiological Function and Role in Disease Management",
"author": "Yadati",
"doi-asserted-by": "crossref",
"first-page": "1679",
"journal-title": "Cells",
"key": "10.1016/j.omtn.2025.102726_bib24",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1002/pro.4073",
"article-title": "Multiple sites on SARS-CoV -2 spike protein are susceptible to proteolysis by cathepsins B, K, L, S, and V",
"author": "Bollavaram",
"doi-asserted-by": "crossref",
"first-page": "1131",
"journal-title": "Protein Sci.",
"key": "10.1016/j.omtn.2025.102726_bib25",
"volume": "30",
"year": "2021"
},
{
"DOI": "10.1038/s41392-021-00558-8",
"article-title": "Cathepsin L plays a key role in SARS-CoV-2 infection in humans and humanized mice and is a promising target for new drug development",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "134",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "10.1016/j.omtn.2025.102726_bib26",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1038/s41421-022-00419-w",
"article-title": "Novel cleavage sites identified in SARS-CoV-2 spike protein reveal mechanism for cathepsin L-facilitated viral infection and treatment strategies",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "53",
"journal-title": "Cell Discov.",
"key": "10.1016/j.omtn.2025.102726_bib27",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.3389/fneur.2020.573095",
"article-title": "The Spatial and Cell-Type Distribution of SARS-CoV-2 Receptor ACE2 in the Human and Mouse Brains",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "573095",
"journal-title": "Front. Neurol.",
"key": "10.1016/j.omtn.2025.102726_bib28",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1007/s10571-020-00947-7",
"article-title": "SARS-CoV-2 Infectivity and Neurological Targets in the Brain",
"author": "Lukiw",
"doi-asserted-by": "crossref",
"first-page": "217",
"journal-title": "Cell. Mol. Neurobiol.",
"key": "10.1016/j.omtn.2025.102726_bib29",
"volume": "42",
"year": "2022"
},
{
"article-title": "Inhibition of host N-myristoylation compromises the infectivity of SARS-CoV-2 due to Golgi-bypassing egress from lysosomes and endoplasmic reticulum",
"author": "Saber",
"journal-title": "bioRxiv",
"key": "10.1016/j.omtn.2025.102726_bib30",
"year": "2023"
},
{
"DOI": "10.1126/sciadv.adj4735",
"article-title": "Choroid plexus defects in Down syndrome brain organoids enhance neurotropism of SARS-CoV-2",
"author": "Shaker",
"doi-asserted-by": "crossref",
"journal-title": "Sci. Adv.",
"key": "10.1016/j.omtn.2025.102726_bib31",
"volume": "10",
"year": "2024"
},
{
"DOI": "10.1186/s13024-022-00533-z",
"article-title": "Tauopathies: new perspectives and challenges",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "28",
"journal-title": "Mol. Neurodegener.",
"key": "10.1016/j.omtn.2025.102726_bib32",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1007/s13365-023-01187-3",
"article-title": "SARS-CoV and SARS-CoV-2 display limited neuronal infection and lack the ability to transmit within synaptically connected axons in stem cell–derived human neurons",
"author": "Luczo",
"doi-asserted-by": "crossref",
"first-page": "39",
"journal-title": "J. Neurovirol.",
"key": "10.1016/j.omtn.2025.102726_bib33",
"volume": "30",
"year": "2024"
},
{
"DOI": "10.1126/sciadv.adg2248",
"article-title": "SARS-CoV-2 infection and viral fusogens cause neuronal and glial fusion that compromises neuronal activity",
"author": "Martínez-Mármol",
"doi-asserted-by": "crossref",
"journal-title": "Sci. Adv.",
"key": "10.1016/j.omtn.2025.102726_bib34",
"volume": "9",
"year": "2023"
},
{
"DOI": "10.3390/v15102020",
"article-title": "Viral Entry Inhibitors Protect against SARS-CoV-2-Induced Neurite Shortening in Differentiated SH-SY5Y Cells",
"author": "Mignolet",
"doi-asserted-by": "crossref",
"first-page": "2020",
"journal-title": "Viruses",
"key": "10.1016/j.omtn.2025.102726_bib35",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.15252/embj.2021107821",
"article-title": "TMPRSS2 expression dictates the entry route used by SARS-CoV-2 to infect host cells",
"author": "Koch",
"doi-asserted-by": "crossref",
"journal-title": "EMBO J.",
"key": "10.1016/j.omtn.2025.102726_bib36",
"volume": "40",
"year": "2021"
},
{
"article-title": "Complete Protection from SARS-CoV-2 Lung Infection in Mice Through Combined Intranasal Delivery of PIKfyve Kinase and TMPRSS2 Protease Inhibitors",
"author": "Kant",
"journal-title": "bioRxiv",
"key": "10.1016/j.omtn.2025.102726_bib37",
"year": "2023"
},
{
"DOI": "10.1021/acschembio.0c00875",
"article-title": "A Clinical-Stage Cysteine Protease Inhibitor blocks SARS-CoV-2 Infection of Human and Monkey Cells",
"author": "Mellott",
"doi-asserted-by": "crossref",
"first-page": "642",
"journal-title": "ACS Chem. Biol.",
"key": "10.1016/j.omtn.2025.102726_bib38",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.15252/embj.2020106230",
"article-title": "SARS-CoV-2 targets neurons of 3D human brain organoids",
"author": "Ramani",
"doi-asserted-by": "crossref",
"journal-title": "EMBO J.",
"key": "10.1016/j.omtn.2025.102726_bib39",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.1016/j.brainresbull.2015.11.007",
"article-title": "Protective mechanisms of CA074-me (other than cathepsin-B inhibition) against programmed necrosis induced by global cerebral ischemia/reperfusion injury in rats",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "97",
"journal-title": "Brain Res. Bull.",
"key": "10.1016/j.omtn.2025.102726_bib40",
"volume": "120",
"year": "2016"
},
{
"DOI": "10.1016/j.neulet.2013.05.056",
"article-title": "CA-074Me, a cathepsin B inhibitor, decreases APP accumulation and protects primary rat cortical neurons treated with okadaic acid",
"author": "Cho",
"doi-asserted-by": "crossref",
"first-page": "222",
"journal-title": "Neurosci. Lett.",
"key": "10.1016/j.omtn.2025.102726_bib41",
"volume": "548",
"year": "2013"
},
{
"DOI": "10.3389/fnagi.2018.00125",
"article-title": "Inhibition of Cathepsins B Induces Neuroprotection Against Secondary Degeneration in Ipsilateral Substantia Nigra After Focal Cortical Infarction in Adult Male Rats",
"author": "Zuo",
"doi-asserted-by": "crossref",
"first-page": "125",
"journal-title": "Front. Aging Neurosci.",
"key": "10.1016/j.omtn.2025.102726_bib42",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1186/s12974-024-03139-y",
"article-title": "Contribution of CNS and extra-CNS infections to neurodegeneration: a narrative review",
"author": "Kettunen",
"doi-asserted-by": "crossref",
"first-page": "152",
"journal-title": "J. Neuroinflammation",
"key": "10.1016/j.omtn.2025.102726_bib43",
"volume": "21",
"year": "2024"
},
{
"DOI": "10.1016/j.biopha.2024.116158",
"article-title": "HIF-1α serves as a co-linker between AD and T2DM",
"author": "Hai",
"doi-asserted-by": "crossref",
"journal-title": "Biomed. Pharmacother.",
"key": "10.1016/j.omtn.2025.102726_bib44",
"volume": "171",
"year": "2024"
},
{
"DOI": "10.3390/v13091768",
"article-title": "Nafamostat–Interferon-α Combination Suppresses SARS-CoV-2 Infection In Vitro and In Vivo by Cooperatively Targeting Host TMPRSS2",
"author": "Ianevski",
"doi-asserted-by": "crossref",
"first-page": "1768",
"journal-title": "Viruses",
"key": "10.1016/j.omtn.2025.102726_bib45",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/j.intimp.2021.107598",
"article-title": "MCP-1: Function, regulation, and involvement in disease",
"author": "Singh",
"doi-asserted-by": "crossref",
"journal-title": "Int. Immunopharmacol.",
"key": "10.1016/j.omtn.2025.102726_bib46",
"volume": "101",
"year": "2021"
},
{
"article-title": "Infectability of Human BrainSphere Neurons Suggests Neurotropism of SARS-CoV-2",
"author": "Bullen",
"first-page": "665",
"journal-title": "ALTEX",
"key": "10.1016/j.omtn.2025.102726_bib47",
"volume": "37",
"year": "2020"
},
{
"DOI": "10.1128/mSphere.00270-21",
"article-title": "Replication Kinetics, Cell Tropism, and Associated Immune Responses in SARS-CoV-2- and H5N1 Virus-Infected Human Induced Pluripotent Stem Cell-Derived Neural Models",
"author": "Bauer",
"doi-asserted-by": "crossref",
"journal-title": "mSphere",
"key": "10.1016/j.omtn.2025.102726_bib48",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1016/j.scr.2021.102436",
"article-title": "Non-permissive SARS-CoV-2 infection in human neurospheres",
"author": "Pedrosa",
"doi-asserted-by": "crossref",
"journal-title": "Stem Cell Res.",
"key": "10.1016/j.omtn.2025.102726_bib49",
"volume": "54",
"year": "2021"
},
{
"DOI": "10.1099/jgv.0.002009",
"article-title": "SARS-CoV-2 infects neurons, astrocytes, choroid plexus epithelial cells and pericytes of the human central nervous system in vitro",
"author": "Haverty",
"doi-asserted-by": "crossref",
"journal-title": "J. Gen. Virol.",
"key": "10.1016/j.omtn.2025.102726_bib50",
"volume": "105",
"year": "2024"
},
{
"DOI": "10.1016/j.omtn.2021.10.016",
"article-title": "Dual inhibition of TMPRSS2 and Cathepsin B prevents SARS-CoV-2 infection in iPS cells",
"author": "Hashimoto",
"doi-asserted-by": "crossref",
"first-page": "1107",
"journal-title": "Mol. Ther. Nucleic Acids",
"key": "10.1016/j.omtn.2025.102726_bib51",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1038/s41586-019-1195-2",
"article-title": "Single-cell transcriptomic analysis of Alzheimer’s disease",
"author": "Mathys",
"doi-asserted-by": "crossref",
"first-page": "332",
"journal-title": "Nature",
"key": "10.1016/j.omtn.2025.102726_bib52",
"volume": "570",
"year": "2019"
},
{
"DOI": "10.2174/1874940201104010011",
"article-title": "The Cathepsin B-Selective Inhibitors CA-074 and CA-074Me Inactivate Cathepsin L Under Reducing Conditions",
"author": "Steverding",
"doi-asserted-by": "crossref",
"first-page": "11",
"journal-title": "Open Enzym. Inhib. J.",
"key": "10.1016/j.omtn.2025.102726_bib53",
"volume": "4",
"year": "2011"
},
{
"DOI": "10.1515/BC.2002.147",
"article-title": "CA-074, But Not Its Methyl Ester CA-074Me, Is a Selective Inhibitor of Cathepsin B within Living Cells",
"author": "Montaser",
"doi-asserted-by": "crossref",
"first-page": "1305",
"journal-title": "Biol. Chem.",
"key": "10.1016/j.omtn.2025.102726_bib54",
"volume": "383",
"year": "2002"
},
{
"DOI": "10.1152/ajpgi.00363.2001",
"article-title": "Cathepsin B inhibition prevents trypsinogen activation and reduces pancreatitis severity",
"author": "van Acker",
"doi-asserted-by": "crossref",
"first-page": "G794",
"journal-title": "Am. J. Physiol. Gastrointest. Liver Physiol.",
"key": "10.1016/j.omtn.2025.102726_bib55",
"volume": "283",
"year": "2002"
},
{
"DOI": "10.1038/labinvest.2014.135",
"article-title": "Treatment with CA-074Me, a Cathepsin B inhibitor, reduces lung interstitial inflammation and fibrosis in a rat model of polymyositis",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "65",
"journal-title": "Lab. Invest.",
"key": "10.1016/j.omtn.2025.102726_bib56",
"volume": "95",
"year": "2015"
},
{
"DOI": "10.1038/s41586-022-04474-x",
"article-title": "Altered TMPRSS2 usage by SARS-CoV-2 Omicron impacts infectivity and fusogenicity",
"author": "Meng",
"doi-asserted-by": "crossref",
"first-page": "706",
"journal-title": "Nature",
"key": "10.1016/j.omtn.2025.102726_bib57",
"volume": "603",
"year": "2022"
},
{
"DOI": "10.1038/emm.2004.1",
"article-title": "Hypoxia-inducible factor (HIF-1)α: its protein stability and biological functions",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Exp. Mol. Med.",
"key": "10.1016/j.omtn.2025.102726_bib58",
"volume": "36",
"year": "2004"
},
{
"DOI": "10.1016/j.febslet.2007.12.035",
"article-title": "Decreased glucose transporters correlate to abnormal hyperphosphorylation of tau in Alzheimer disease",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "359",
"journal-title": "FEBS Lett.",
"key": "10.1016/j.omtn.2025.102726_bib59",
"volume": "582",
"year": "2008"
},
{
"DOI": "10.1016/j.virol.2019.02.010",
"article-title": "Influenza A virus (H1N1) triggers a hypoxic response by stabilizing hypoxia-inducible factor-1α via inhibition of proteasome",
"author": "Ren",
"doi-asserted-by": "crossref",
"first-page": "51",
"journal-title": "Virology",
"key": "10.1016/j.omtn.2025.102726_bib60",
"volume": "530",
"year": "2019"
},
{
"DOI": "10.1016/j.virol.2011.03.005",
"article-title": "Interaction of the human cytomegalovirus particle with the host cell induces hypoxia-inducible factor 1 alpha",
"author": "McFarlane",
"doi-asserted-by": "crossref",
"first-page": "83",
"journal-title": "Virology",
"key": "10.1016/j.omtn.2025.102726_bib61",
"volume": "414",
"year": "2011"
},
{
"DOI": "10.1128/mBio.02956-20",
"article-title": "Hypoxia-Inducible Factor 1α (HIF1α) Suppresses Virus Replication in Human Cytomegalovirus Infection by Limiting Kynurenine Synthesis",
"author": "Wise",
"doi-asserted-by": "crossref",
"journal-title": "mBio",
"key": "10.1016/j.omtn.2025.102726_bib62",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1128/mBio.00757-18",
"article-title": "Induction of HIF-1α by HIV-1 Infection in CD4+ T Cells Promotes Viral Replication and Drives Extracellular Vesicle-Mediated Inflammation",
"author": "Duette",
"doi-asserted-by": "crossref",
"journal-title": "mBio",
"key": "10.1016/j.omtn.2025.102726_bib63",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1186/s12950-020-00263-3",
"article-title": "Hypoxia: A key feature of COVID-19 launching activation of HIF-1 and cytokine storm",
"author": "Jahani",
"doi-asserted-by": "crossref",
"first-page": "33",
"journal-title": "J. Inflamm.",
"key": "10.1016/j.omtn.2025.102726_bib64",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.celrep.2021.109920",
"article-title": "An airway organoid-based screen identifies a role for the HIF1α-glycolysis axis in SARS-CoV-2 infection",
"author": "Duan",
"doi-asserted-by": "crossref",
"journal-title": "Cell Rep.",
"key": "10.1016/j.omtn.2025.102726_bib65",
"volume": "37",
"year": "2021"
},
{
"DOI": "10.3390/cells13040300",
"article-title": "Single-Cell RNA Sequencing Reveals HIF1A as a Severity-Sensitive Immunological Scar in Circulating Monocytes of Convalescent Comorbidity-Free COVID-19 Patients",
"author": "May",
"doi-asserted-by": "crossref",
"first-page": "300",
"journal-title": "Cells",
"key": "10.1016/j.omtn.2025.102726_bib66",
"volume": "13",
"year": "2024"
},
{
"DOI": "10.1016/j.celrep.2021.109020",
"article-title": "Hypoxic and pharmacological activation of HIF inhibits SARS-CoV-2 infection of lung epithelial cells",
"author": "Wing",
"doi-asserted-by": "crossref",
"journal-title": "Cell Rep.",
"key": "10.1016/j.omtn.2025.102726_bib67",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1038/s41392-021-00726-w",
"article-title": "HIF-1α promotes SARS-CoV-2 infection and aggravates inflammatory responses to COVID-19",
"author": "Tian",
"doi-asserted-by": "crossref",
"first-page": "308",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "10.1016/j.omtn.2025.102726_bib68",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1038/emi.2017.21",
"article-title": "Nuclear translocation of HIF-1α induced by influenza A (H1N1) infection is critical to the production of proinflammatory cytokines",
"author": "Guo",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Emerg. Microbes Infect.",
"key": "10.1016/j.omtn.2025.102726_bib69",
"volume": "6",
"year": "2017"
},
{
"DOI": "10.1080/22221751.2020.1742585",
"article-title": "Deficiency of HIF-1α enhances influenza A virus replication by promoting autophagy in alveolar type II epithelial cells",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "691",
"journal-title": "Emerg. Microbes Infect.",
"key": "10.1016/j.omtn.2025.102726_bib70",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.virs.2023.11.010",
"article-title": "HIF-1α promotes virus replication and cytokine storm in H1N1 virus-induced severe pneumonia through cellular metabolic reprogramming",
"author": "Meng",
"doi-asserted-by": "crossref",
"first-page": "81",
"journal-title": "Virol. Sin.",
"key": "10.1016/j.omtn.2025.102726_bib71",
"volume": "39",
"year": "2024"
},
{
"DOI": "10.1371/journal.ppat.1008192",
"article-title": "A role of hypoxia-inducible factor 1 alpha in Murine Gammaherpesvirus 68 (MHV68) lytic replication and reactivation from latency",
"author": "López-Rodríguez",
"doi-asserted-by": "crossref",
"journal-title": "PLoS Pathog.",
"key": "10.1016/j.omtn.2025.102726_bib72",
"volume": "15",
"year": "2019"
},
{
"DOI": "10.1186/1742-2094-9-149",
"article-title": "Plasminogen activator inhibitor type 1 regulates microglial motility and phagocytic activity",
"author": "Jeon",
"doi-asserted-by": "crossref",
"first-page": "149",
"journal-title": "J. Neuroinflammation",
"key": "10.1016/j.omtn.2025.102726_bib73",
"volume": "9",
"year": "2012"
},
{
"DOI": "10.1186/1742-2094-8-77",
"article-title": "CCL2/MCP-1 modulation of microglial activation and proliferation",
"author": "Hinojosa",
"doi-asserted-by": "crossref",
"first-page": "77",
"journal-title": "J. Neuroinflammation",
"key": "10.1016/j.omtn.2025.102726_bib74",
"volume": "8",
"year": "2011"
},
{
"DOI": "10.1038/nm1567",
"article-title": "MIF is a noncognate ligand of CXC chemokine receptors in inflammatory and atherogenic cell recruitment",
"author": "Bernhagen",
"doi-asserted-by": "crossref",
"first-page": "587",
"journal-title": "Nat. Med.",
"key": "10.1016/j.omtn.2025.102726_bib75",
"volume": "13",
"year": "2007"
},
{
"DOI": "10.1111/j.1750-3639.2010.00445.x",
"article-title": "Neuronal MCP-1 Mediates Microglia Recruitment and Neurodegeneration Induced by the Mild Impairment of Oxidative Metabolism",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "279",
"journal-title": "Brain Pathol.",
"key": "10.1016/j.omtn.2025.102726_bib76",
"volume": "21",
"year": "2011"
},
{
"DOI": "10.1038/s41423-023-00974-6",
"article-title": "The chemokines CXCL8 and CXCL12: molecular and functional properties, role in disease and efforts towards pharmacological intervention",
"author": "Cambier",
"doi-asserted-by": "crossref",
"first-page": "217",
"journal-title": "Cell. Mol. Immunol.",
"key": "10.1016/j.omtn.2025.102726_bib77",
"volume": "20",
"year": "2023"
},
{
"DOI": "10.1128/spectrum.01256-23",
"article-title": "Analysis of SARS-CoV-2 isolates, namely the Wuhan strain, Delta variant, and Omicron variant, identifies differential immune profiles",
"author": "Shahbaz",
"doi-asserted-by": "crossref",
"journal-title": "Microbiol. Spectr.",
"key": "10.1016/j.omtn.2025.102726_bib78",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.1016/S2352-3026(20)30216-7",
"article-title": "Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study",
"author": "Goshua",
"doi-asserted-by": "crossref",
"first-page": "e575",
"journal-title": "Lancet. Haematol.",
"key": "10.1016/j.omtn.2025.102726_bib79",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1160/TH05-12-0827",
"article-title": "Analysis of thrombotic factors in severe acute respiratory syndrome (SARS) patients",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "100",
"journal-title": "Thromb. Haemost.",
"key": "10.1016/j.omtn.2025.102726_bib80",
"volume": "96",
"year": "2006"
},
{
"DOI": "10.1093/qjmed/hcac234",
"article-title": "MIF is a common genetic determinant of COVID-19 symptomatic infection and severity",
"author": "Shin",
"doi-asserted-by": "crossref",
"first-page": "205",
"journal-title": "QJM",
"key": "10.1016/j.omtn.2025.102726_bib81",
"volume": "116",
"year": "2023"
},
{
"DOI": "10.1515/tjb-2023-0193",
"article-title": "CXCL12/CXCR4 as a potential axis in diagnosis and predicting disease severity in COVID-19 patients: a new perspective",
"author": "Ozkaya",
"doi-asserted-by": "crossref",
"first-page": "578",
"journal-title": "Turk. J. Biochem.",
"key": "10.1016/j.omtn.2025.102726_bib82",
"volume": "49",
"year": "2024"
},
{
"DOI": "10.1182/blood.V99.6.2077",
"article-title": "Identification of a tightly regulated hypoxia-response element in the promoter of human plasminogen activator inhibitor–1",
"author": "Fink",
"doi-asserted-by": "crossref",
"first-page": "2077",
"journal-title": "Blood",
"key": "10.1016/j.omtn.2025.102726_bib83",
"volume": "99",
"year": "2002"
},
{
"DOI": "10.1101/gad.1471106",
"article-title": "HIF1α delays premature senescence through the activation of MIF",
"author": "Welford",
"doi-asserted-by": "crossref",
"first-page": "3366",
"journal-title": "Genes Dev.",
"key": "10.1016/j.omtn.2025.102726_bib84",
"volume": "20",
"year": "2006"
},
{
"DOI": "10.1158/1541-7786.MCR-11-0498",
"article-title": "New Insight into the SDF-1/CXCR4 Axis in a Breast Carcinoma Model: Hypoxia-Induced Endothelial SDF-1 and Tumor Cell CXCR4 Are Required for Tumor Cell Intravasation",
"author": "Jin",
"doi-asserted-by": "crossref",
"first-page": "1021",
"journal-title": "Mol. Cancer Res.",
"key": "10.1016/j.omtn.2025.102726_bib85",
"volume": "10",
"year": "2012"
},
{
"DOI": "10.1186/1465-9921-13-60",
"article-title": "HIF-1 expression is associated with CCL2 chemokine expression in airway inflammatory cells: implications in allergic airway inflammation",
"author": "Baay-Guzman",
"doi-asserted-by": "crossref",
"first-page": "60",
"journal-title": "Respir. Res.",
"key": "10.1016/j.omtn.2025.102726_bib86",
"volume": "13",
"year": "2012"
},
{
"DOI": "10.1128/mbio.00892-22",
"article-title": "Serine Protease Inhibitors Restrict Host Susceptibility to SARS-CoV-2 Infections",
"author": "Rosendal",
"doi-asserted-by": "crossref",
"journal-title": "mBio",
"key": "10.1016/j.omtn.2025.102726_bib87",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1128/mBio.00970-21",
"article-title": "The TMPRSS2 Inhibitor Nafamostat Reduces SARS-CoV-2 Pulmonary Infection in Mouse Models of COVID-19",
"author": "Li",
"doi-asserted-by": "crossref",
"journal-title": "mBio",
"key": "10.1016/j.omtn.2025.102726_bib88",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1128/jvi.01969-21",
"article-title": "Microglia Do Not Restrict SARS-CoV-2 Replication following Infection of the Central Nervous System of K18-Human ACE2 Transgenic Mice",
"author": "Olivarria",
"doi-asserted-by": "crossref",
"journal-title": "J. Virol.",
"key": "10.1016/j.omtn.2025.102726_bib89",
"volume": "96",
"year": "2022"
},
{
"DOI": "10.1021/jacs.2c03925",
"article-title": "Amyloidogenesis of SARS-CoV-2 Spike Protein",
"author": "Nyström",
"doi-asserted-by": "crossref",
"first-page": "8945",
"journal-title": "J. Am. Chem. Soc.",
"key": "10.1016/j.omtn.2025.102726_bib90",
"volume": "144",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0288138",
"article-title": "Tau protein aggregation associated with SARS-CoV-2 main protease",
"author": "Eberle",
"doi-asserted-by": "crossref",
"journal-title": "PLoS One",
"key": "10.1016/j.omtn.2025.102726_bib91",
"volume": "18",
"year": "2023"
},
{
"DOI": "10.1093/pnasnexus/pgad282",
"article-title": "Severe acute respiratory syndrome coronavirus 2 infection leads to Tau pathological signature in neurons",
"author": "Di Primio",
"doi-asserted-by": "crossref",
"journal-title": "PNAS Nexus",
"key": "10.1016/j.omtn.2025.102726_bib92",
"volume": "2",
"year": "2023"
},
{
"DOI": "10.1186/s40478-018-0557-6",
"article-title": "Phosphorylation of different tau sites during progression of Alzheimer’s disease",
"author": "Neddens",
"doi-asserted-by": "crossref",
"first-page": "52",
"journal-title": "Acta Neuropathol. Commun.",
"key": "10.1016/j.omtn.2025.102726_bib93",
"volume": "6",
"year": "2018"
},
{
"DOI": "10.1186/s12974-022-02486-y",
"article-title": "Microglial amyloid beta clearance is driven by PIEZO1 channels",
"author": "Jäntti",
"doi-asserted-by": "crossref",
"first-page": "147",
"journal-title": "J. Neuroinflammation",
"key": "10.1016/j.omtn.2025.102726_bib94",
"volume": "19",
"year": "2022"
},
{
"DOI": "10.1126/science.abd2985",
"article-title": "Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity",
"author": "Cantuti-Castelvetri",
"doi-asserted-by": "crossref",
"first-page": "856",
"journal-title": "Science",
"key": "10.1016/j.omtn.2025.102726_bib95",
"volume": "370",
"year": "2020"
},
{
"DOI": "10.1371/journal.pbio.3001091",
"article-title": "A plasmid DNA-launched SARS-CoV-2 reverse genetics system and coronavirus toolkit for COVID-19 research",
"author": "Rihn",
"doi-asserted-by": "crossref",
"journal-title": "PLoS Biol.",
"key": "10.1016/j.omtn.2025.102726_bib96",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.3389/fmicb.2021.625136",
"article-title": "An Optimized High-Throughput Immuno-Plaque Assay for SARS-CoV-2",
"author": "Amarilla",
"doi-asserted-by": "crossref",
"first-page": "625136",
"journal-title": "Front. Microbiol.",
"key": "10.1016/j.omtn.2025.102726_bib97",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.3390/v13020143",
"article-title": "A 10-Minute “Mix and Read” Antibody Assay for SARS-CoV-2",
"author": "Rusanen",
"doi-asserted-by": "crossref",
"first-page": "143",
"journal-title": "Viruses",
"key": "10.1016/j.omtn.2025.102726_bib98",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1186/s12859-021-04344-9",
"article-title": "CellProfiler 4: improvements in speed, utility and usability",
"author": "Stirling",
"doi-asserted-by": "crossref",
"first-page": "433",
"journal-title": "BMC Bioinf.",
"key": "10.1016/j.omtn.2025.102726_bib99",
"volume": "22",
"year": "2021"
},
{
"article-title": "Processing of gene expression data generated by quantitative real-time RT-PCR",
"author": "Muller",
"first-page": "1372",
"journal-title": "Biotechniques",
"key": "10.1016/j.omtn.2025.102726_bib100",
"volume": "32",
"year": "2002"
}
],
"reference-count": 100,
"references-count": 100,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S216225312500280X"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "SARS-CoV-2 infection in hiPSC-derived neurons is cathepsin-dependent and causes differential accumulation of HIF1ɑ and phosphorylated tau",
"type": "journal-article",
"update-policy": "https://doi.org/10.1016/elsevier_cm_policy",
"volume": "36"
}