Comparison of the cardiovascular system, clinical condition, and laboratory results in COVID-19 patients with and without vitamin D insufficiency
et al., BMC Infectious Diseases, doi:10.1186/s12879-022-07438-8, May 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 202 hospitalized COVID-19 patients in Iran, showing no significant difference in outcomes based on vitamin D levels.
This is the 134th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 75.8% lower, RR 0.24, p = 0.26, high D levels (≥30ng/mL) 1 of 75 (1.3%), low D levels (<30ng/mL) 7 of 127 (5.5%), NNT 24.
|
|
risk of severe case, 4.8% higher, RR 1.05, p = 1.00, high D levels (≥30ng/mL) 13 of 75 (17.3%), low D levels (<30ng/mL) 21 of 127 (16.5%).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Kazemi et al., 7 May 2022, retrospective, Iran, peer-reviewed, mean age 56.0, 4 authors.
Contact: h1a1sheyban@gmail.com (corresponding author), sheybani@shmu.ac.ir.
Comparison of the cardiovascular system, clinical condition, and laboratory results in COVID-19 patients with and without vitamin D insufficiency
BMC Infectious Diseases, doi:10.1186/s12879-022-07438-8
Background: Serum vitamin D levels may have a protective role against severe coronavirus disease 2019 . Studies have shown that deficiency in vitamin D may be a significant risk factor for poor outcomes. This study aims to compare the outcome and clinical condition of patients diagnosed with COVID-19 infection considering serum vitamin D levels.
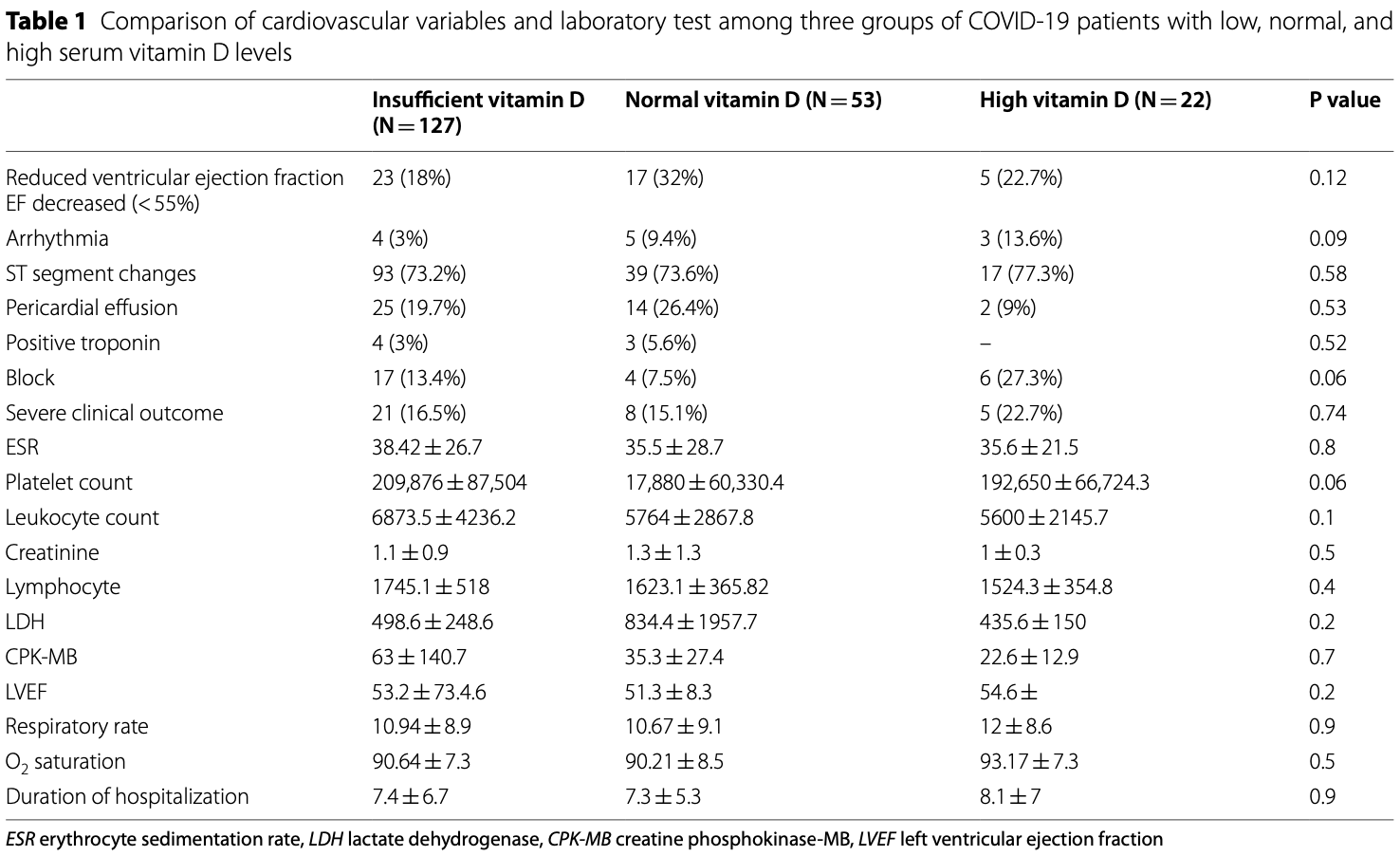
Methods: In this cross-sectional study, 202 COVID-19 patients without known cardiovascular disease (reduced ejection fraction, uncontrolled arrhythmia, pericardial effusion, cardiac block, valvular disease, or hypertension) were included. Patients were divided into three groups of insufficient (< 30 ng/mL), normal (30 to 50 ng/mL), and high (> 50 ng/mL) serum vitamin D levels. Clinical outcome was defined as severe if invasive respiratory intervention and ICU admission was required.
Results: The patients were divided into three groups based on their vitamin D level: 127 cases in the insufficient vitamin D group, 53 cases in the normal vitamin D group, and 22 cases in the high vitamin D group. The mean age of the population study was 56 years. Thirty-four patients had severe clinical outcomes. The distribution of this group was as follows: 21 patients in the insufficient vitamin D group (16.5%), eight patients in the normal vitamin D group (15.1%), and five patients in the high vitamin D group (22.7%); P = 0.74. No significant differences were found between the groups in terms of mortality rate (P = 0.46). Moreover, the mean of leukocytes (mean ± SD = 6873.5 ± 4236.2), ESR (mean ± SD = 38.42 ± 26.7), and CPK-MB (mean ± SD = 63 ± 140.7) were higher in the insufficient vitamin D group, but it was not statistically significant (P > 0.05).
Conclusion: The finding of the present study showed that vitamin D could not make a significant difference in cardiovascular systems, laboratory results, and severity of the disease in COVID-19 patients.
Abbreviations Author contributions EK and AM gathered the required data. AM, EK, and HSh reviewed the literature. HSh and MRR interpreted the laboratory and clinical findings. All authors participated in writing the manuscript. All authors read and approved the final manuscript.
Declarations Ethics approval and consent to participate This project was approved by the Ethical Committee of Shahroud University of Medical Sciences, Shahroud, Iran. The study was conducted according to the guidelines of the Declaration of Helsinki. Informed consent was waived by the Ethics Committee as no intervention was done, and informed consent is routinely obtained from the patients at our hospital upon admission to receive medical care and diagnostic procedures.
Consent for publication Not applicable.
Competing interests The authors declare no competing interests.
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Abrishami, Possible association of vitamin D status with lung involvement and outcome in patients with COVID-19: a retrospective study, Eur J Nutr
Annweiler, Vitamin D and survival in COVID-19 patients: a quasiexperimental study, J Steroid Biochem Mol Biol
Azadeh, Serum Vitamin D concentrations in CoVID19 patients, J Mazand Univ Med Sci
Azevedo, Covid-19 and the cardiovascular system: a comprehensive review, J Hum Hypertens
Bae, Impact of cardiovascular disease and risk factors on fatal outcomes in patients with COVID-19 according to age: a systematic review and meta-analysis, Heart
Baktash, Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med J
Banerjee, Vitamin D and immuno-pathology of COVID-19: many interactions but uncertain therapeutic benefits, Expert Rev Anti Infect Ther
Batsi, Vitamin D deficiency as a risk factor for myocardial ischemia, Medicina
Bie, The status and research progress on vitamin D deficiency and atrial fibrillation, Braz J Cardiovasc Surg
Butler-Laporte, Vitamin D and COVID-19 susceptibility and severity in the COVID-19 host genetics initiative: a Mendelian randomization study, PLoS Med
Cereda, Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital, Clin Nutr
Cereda, Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy, Nutrition
Da Rocha, Insufficient evidence for vitamin D use in COVID-19: A rapid systematic review, Int J Clin Pract
Davoudi, Lack of association between vitamin D insufficiency and clinical outcomes of patients with COVID-19 infection, BMC Infect Dis
Diaz-Curiel, The relationship between 25(OH) vitamin D levels and COVID-19 onset and disease course in Spanish patients, J Steroid Biochem Mol Biol
Flack, Adekola, Blood pressure and the new ACC/AHA hypertension guidelines, Trends Cardiovasc Med
Garcia-Zamora, Arrhythmias and electrocardiographic findings in Coronavirus disease 2019: A systematic review and meta-analysis, Pacing Clin Electrophysiol
Grant, Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients
Hadizadeh, Supplementation with vitamin D in the COVID-19 pandemic?, Nutr Rev
Hastie, Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr
Hernández, Vitamin D status in hospitalized patients with SARS-CoV-2 infection, J Clin Endocrinol Metab
Honardoost, Ghavideldarestani, Khamseh, Role of vitamin D in pathogenesis and severity of COVID-19 infection, Arch Physiol Biochem, doi:10.1080/13813455.2020.1792505
Jain, Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci Rep
Kazemi, Association of vitamin D status with SARS-CoV-2 infection or COVID-19 severity: a systematic review and meta-analysis, Adv Nutr
Kendrick, 25-Hydroxyvitamin D deficiency is independently associated with cardiovascular disease in the third national health and nutrition examination survey, Atherosclerosis
Lakkireddy, Impact of daily high dose oral vitamin D therapy on the inflammatory markers in patients with COVID 19 disease, Sci Rep
Latic, Erben, Vitamin D and cardiovascular disease, with emphasis on hypertension, atherosclerosis, and heart failure, Int J Mol Sci
Lee, Vitamin D deficiency an important, common, and easily treatable cardiovascular risk factor?, J Am Coll Cardiol
Liu, Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta-analysis, Int J Infect Dis
Maghbooli, Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PLoS ONE
Mariani, Association between vitamin D Deficiency and COVID-19 incidence, complications, and mortality in 46 countries: an ecological study, Health Secur
Mathyssen, Local expression profiles of vitamin D-related genes in airways of COPD patients, Respir Res
Meltzer, Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw Open
Mesquita, Cardiac arrhythmias in patients presenting with COVID-19 treated in Portuguese hospitals: A national registry from the Portuguese association of arrhythmology, pacing and electrophysiology, Rev Port Cardiol
Mirmoeeni, Cardiovascular manifestations in COVID-19 patients: a systematic review and meta-analysis, J Cardiovasc Thorac Res
Mozos, Marginean, Links between vitamin D deficiency and cardiovascular diseases, Biomed Res Int
Murdaca, Pioggia, Negrini, Vitamin D and Covid-19: an update on evidence and potential therapeutic implications, Clin Mol Allergy
Naghedi, Effect of vitamin D supplements on left ventricular ejection fraction in patients with heart failure: A systematic review and meta-analysis of randomized controlled trials, Rev Port Cardiol
Pereira, Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis, Crit Rev Food Sci Nutr
Pilz, Vitamin D and cardiovascular disease prevention, Nat Rev Cardiol
Pimentel, Vega, Pichard, Low vitamin D levels and increased neutrophil in patients admitted at ICU with COVID-19, Clin Nutr ESPEN
Pizzini, Impact of vitamin D deficiency on COVID-19-a prospective analysis from the CovILD Registry, Nutrients
Rastogi, Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study), Postgrad Med J
Saponaro, Marcocci, Zucchi, Vitamin D status and cardiovascular outcome, J Endocrinol Invest
Schleithoff, Vitamin D supplementation improves cytokine profiles in patients with congestive heart failure: a double-blind, randomized, placebo-controlled trial, Am J Clin Nutr
Stroehlein, Vitamin D supplementation for the treatment of COVID-19: a living systematic review, Cochrane Database Syst Rev, doi:10.1002/14651858.CD015043
Szeto, Vitamin D status and COVID-19 clinical outcomes in hospitalized patients, Endocr Res
Tadj, Lahbib, Our overall current knowledge of Covid 19: an overview, Microbes Infect Chemother
Tan, Cohort study to evaluate the effect of vitamin D, magnesium, and vitamin B(12) in combination on progression to severe outcomes in older patients with coronavirus (COVID-19), Nutrition
Turin, Interactions among vitamin D, atrial fibrillation, and the renin-angiotensin-aldosterone system, Am J Cardiol
Wang, The vitamin D for COVID-19 (VIVID) trial: a pragmatic cluster-randomized design, Contemp Clin Trials
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) Outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention, JAMA
Xie, HMGB1 regulates P-glycoprotein expression in status epilepticus rat brains via the RAGE/NF-κB signaling pathway, Mol Med Rep
Ye, Does serum vitamin D level affect COVID-19 infection and its severity? A case-control study, J Am Coll Nutr
Zelzer, Vitamin D metabolites and clinical outcome in hospitalized COVID-19 patients, Nutrients
Zheng, COVID-19 and the cardiovascular system, Nat Rev Cardiol
DOI record:
{
"DOI": "10.1186/s12879-022-07438-8",
"ISSN": [
"1471-2334"
],
"URL": "http://dx.doi.org/10.1186/s12879-022-07438-8",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>Serum vitamin D levels may have a protective role against severe coronavirus disease 2019 (COVID-19). Studies have shown that deficiency in vitamin D may be a significant risk factor for poor outcomes. This study aims to compare the outcome and clinical condition of patients diagnosed with COVID-19 infection considering serum vitamin D levels.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>In this cross-sectional study, 202 COVID-19 patients without known cardiovascular disease (reduced ejection fraction, uncontrolled arrhythmia, pericardial effusion, cardiac block, valvular disease, or hypertension) were included. Patients were divided into three groups of insufficient (< 30 ng/mL), normal (30 to 50 ng/mL), and high (> 50 ng/mL) serum vitamin D levels. Clinical outcome was defined as severe if invasive respiratory intervention and ICU admission was required.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>The patients were divided into three groups based on their vitamin D level: 127 cases in the insufficient vitamin D group, 53 cases in the normal vitamin D group, and 22 cases in the high vitamin D group. The mean age of the population study was 56 years. Thirty-four patients had severe clinical outcomes. The distribution of this group was as follows: 21 patients in the insufficient vitamin D group (16.5%), eight patients in the normal vitamin D group (15.1%), and five patients in the high vitamin D group (22.7%); P = 0.74. No significant differences were found between the groups in terms of mortality rate (P = 0.46). Moreover, the mean of leukocytes (mean ± SD = 6873.5 ± 4236.2), ESR (mean ± SD = 38.42 ± 26.7), and CPK-MB (mean ± SD = 63 ± 140.7) were higher in the insufficient vitamin D group, but it was not statistically significant (P > 0.05).</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusion</jats:title>\n <jats:p>The finding of the present study showed that vitamin D could not make a significant difference in cardiovascular systems, laboratory results, and severity of the disease in COVID-19 patients.</jats:p>\n </jats:sec>",
"alternative-id": [
"7438"
],
"article-number": "441",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "5 November 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "3 May 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "7 May 2022"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "This project was approved by the Ethical Committee of Shahroud University of Medical Sciences, Shahroud, Iran. The study was conducted according to the guidelines of the Declaration of Helsinki. Informed consent was waived by the Ethics Committee as no intervention was done, and informed consent is routinely obtained from the patients at our hospital upon admission to receive medical care and diagnostic procedures."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "Not applicable."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-3886-0466",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kazemi",
"given": "Erfan",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-7206-2858",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mansursamaei",
"given": "Ali",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7945-7542",
"affiliation": [],
"authenticated-orcid": false,
"family": "Rohani-Rasaf",
"given": "Marzieh",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1632-0511",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sheibani",
"given": "Hossein",
"sequence": "additional"
}
],
"container-title": "BMC Infectious Diseases",
"container-title-short": "BMC Infect Dis",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
5,
7
]
],
"date-time": "2022-05-07T12:05:08Z",
"timestamp": 1651925108000
},
"deposited": {
"date-parts": [
[
2022,
5,
7
]
],
"date-time": "2022-05-07T13:02:44Z",
"timestamp": 1651928564000
},
"indexed": {
"date-parts": [
[
2022,
5,
7
]
],
"date-time": "2022-05-07T13:41:29Z",
"timestamp": 1651930889269
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2022,
5,
7
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2022,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
5,
7
]
],
"date-time": "2022-05-07T00:00:00Z",
"timestamp": 1651881600000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
5,
7
]
],
"date-time": "2022-05-07T00:00:00Z",
"timestamp": 1651881600000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12879-022-07438-8.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1186/s12879-022-07438-8/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12879-022-07438-8.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2022,
5,
7
]
]
},
"published-online": {
"date-parts": [
[
2022,
5,
7
]
]
},
"published-print": {
"date-parts": [
[
2022,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1371/journal.pone.0239799",
"author": "Z Maghbooli",
"doi-asserted-by": "publisher",
"issue": "9",
"journal-title": "PLoS ONE",
"key": "7438_CR1",
"unstructured": "Maghbooli Z, et al. Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PLoS ONE. 2020;15(9): e0239799.",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1080/07435800.2020.1867162",
"author": "B Szeto",
"doi-asserted-by": "publisher",
"first-page": "66",
"issue": "2",
"journal-title": "Endocr Res",
"key": "7438_CR2",
"unstructured": "Szeto B, et al. Vitamin D status and COVID-19 clinical outcomes in hospitalized patients. Endocr Res. 2021;46(2):66–73.",
"volume": "46",
"year": "2021"
},
{
"DOI": "10.54034/mic.e1262",
"author": "A Tadj",
"doi-asserted-by": "publisher",
"journal-title": "Microbes Infect Chemother",
"key": "7438_CR3",
"unstructured": "Tadj A, Lahbib SS. Our overall current knowledge of Covid 19: an overview. Microbes Infect Chemother. 2021;1: e1262.",
"volume": "1",
"year": "2021"
},
{
"key": "7438_CR4",
"unstructured": "World health organization. Weekly epidemiological update on COVID-19, 14 December 2021. 2021;70. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---14-december-2021. Accessed 15 Dec 2021."
},
{
"DOI": "10.1016/j.nut.2020.111017",
"author": "CW Tan",
"doi-asserted-by": "publisher",
"journal-title": "Nutrition",
"key": "7438_CR5",
"unstructured": "Tan CW, et al. Cohort study to evaluate the effect of vitamin D, magnesium, and vitamin B(12) in combination on progression to severe outcomes in older patients with coronavirus (COVID-19). Nutrition. 2020;79–80: 111017.",
"volume": "79–80",
"year": "2020"
},
{
"DOI": "10.1007/s00394-020-02411-0",
"author": "A Abrishami",
"doi-asserted-by": "publisher",
"first-page": "2249",
"issue": "4",
"journal-title": "Eur J Nutr",
"key": "7438_CR6",
"unstructured": "Abrishami A, et al. Possible association of vitamin D status with lung involvement and outcome in patients with COVID-19: a retrospective study. Eur J Nutr. 2021;60(4):2249–57.",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1016/j.jsbmb.2020.105771",
"author": "C Annweiler",
"doi-asserted-by": "publisher",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "7438_CR7",
"unstructured": "Annweiler C, et al. Vitamin D and survival in COVID-19 patients: a quasi-experimental study. J Steroid Biochem Mol Biol. 2020;204: 105771.",
"volume": "204",
"year": "2020"
},
{
"DOI": "10.1210/clinem/dgaa733",
"author": "JL Hernández",
"doi-asserted-by": "publisher",
"first-page": "e1343",
"issue": "3",
"journal-title": "J Clin Endocrinol Metab",
"key": "7438_CR8",
"unstructured": "Hernández JL, et al. Vitamin D status in hospitalized patients with SARS-CoV-2 infection. J Clin Endocrinol Metab. 2021;106(3):e1343–53.",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1080/07315724.2020.1826005",
"author": "K Ye",
"doi-asserted-by": "publisher",
"first-page": "724",
"issue": "8",
"journal-title": "J Am Coll Nutr",
"key": "7438_CR9",
"unstructured": "Ye K, et al. Does serum vitamin D level affect COVID-19 infection and its severity? A case–control study. J Am Coll Nutr. 2020;40(8):724–31.",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.12.077",
"author": "N Liu",
"doi-asserted-by": "publisher",
"first-page": "58",
"journal-title": "Int J Infect Dis",
"key": "7438_CR10",
"unstructured": "Liu N, et al. Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta-analysis. Int J Infect Dis. 2021;104:58–64.",
"volume": "104",
"year": "2021"
},
{
"DOI": "10.1186/s12948-020-00139-0",
"author": "G Murdaca",
"doi-asserted-by": "publisher",
"first-page": "23",
"issue": "1",
"journal-title": "Clin Mol Allergy",
"key": "7438_CR11",
"unstructured": "Murdaca G, Pioggia G, Negrini S. Vitamin D and Covid-19: an update on evidence and potential therapeutic implications. Clin Mol Allergy. 2020;18(1):23.",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1016/j.cct.2020.106176",
"author": "R Wang",
"doi-asserted-by": "publisher",
"first-page": "106176",
"journal-title": "Contemp Clin Trials",
"key": "7438_CR12",
"unstructured": "Wang R, et al. The vitamin D for COVID-19 (VIVID) trial: a pragmatic cluster-randomized design. Contemp Clin Trials. 2021;100:106176–106176.",
"volume": "100",
"year": "2021"
},
{
"DOI": "10.3892/mmr.2017.6772",
"author": "Y Xie",
"doi-asserted-by": "publisher",
"first-page": "1691",
"issue": "2",
"journal-title": "Mol Med Rep",
"key": "7438_CR13",
"unstructured": "Xie Y, et al. HMGB1 regulates P-glycoprotein expression in status epilepticus rat brains via the RAGE/NF-κB signaling pathway. Mol Med Rep. 2017;16(2):1691–700.",
"volume": "16",
"year": "2017"
},
{
"DOI": "10.1080/13813455.2020.1792505",
"author": "M Honardoost",
"doi-asserted-by": "publisher",
"journal-title": "Arch Physiol Biochem",
"key": "7438_CR14",
"unstructured": "Honardoost M, Ghavideldarestani M, Khamseh ME. Role of vitamin D in pathogenesis and severity of COVID-19 infection. Arch Physiol Biochem. 2020. https://doi.org/10.1080/13813455.2020.1792505.",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"author": "DO Meltzer",
"doi-asserted-by": "publisher",
"issue": "9",
"journal-title": "JAMA Netw Open",
"key": "7438_CR15",
"unstructured": "Meltzer DO, et al. Association of vitamin D status and other clinical characteristics with COVID-19 test results. JAMA Netw Open. 2020;3(9): e2019722.",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1089/hs.2020.0137",
"author": "J Mariani",
"doi-asserted-by": "publisher",
"first-page": "302",
"issue": "3",
"journal-title": "Health Secur",
"key": "7438_CR16",
"unstructured": "Mariani J, et al. Association between vitamin D Deficiency and COVID-19 incidence, complications, and mortality in 46 countries: an ecological study. Health Secur. 2021;19(3):302–8.",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1093/nutrit/nuaa081",
"author": "F Hadizadeh",
"doi-asserted-by": "publisher",
"first-page": "200",
"issue": "2",
"journal-title": "Nutr Rev",
"key": "7438_CR17",
"unstructured": "Hadizadeh F. Supplementation with vitamin D in the COVID-19 pandemic? Nutr Rev. 2021;79(2):200–8.",
"volume": "79",
"year": "2021"
},
{
"DOI": "10.1038/s41598-019-56847-4",
"author": "A Jain",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "Sci Rep",
"key": "7438_CR18",
"unstructured": "Jain A, et al. Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers. Sci Rep. 2020;10(1):1–8.",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1016/j.nut.2020.111055",
"author": "E Cereda",
"doi-asserted-by": "publisher",
"journal-title": "Nutrition",
"key": "7438_CR19",
"unstructured": "Cereda E, et al. Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy. Nutrition. 2021;82: 111055.",
"volume": "82",
"year": "2021"
},
{
"DOI": "10.3390/nu12092775",
"author": "A Pizzini",
"doi-asserted-by": "publisher",
"first-page": "2775",
"issue": "9",
"journal-title": "Nutrients",
"key": "7438_CR20",
"unstructured": "Pizzini A, et al. Impact of vitamin D deficiency on COVID-19—a prospective analysis from the CovILD Registry. Nutrients. 2020;12(9):2775.",
"volume": "12",
"year": "2020"
},
{
"author": "V Baktash",
"first-page": "442",
"issue": "1149",
"journal-title": "Postgrad Med J",
"key": "7438_CR21",
"unstructured": "Baktash V, et al. Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgrad Med J. 2021;97(1149):442–7.",
"volume": "97",
"year": "2021"
},
{
"DOI": "10.1007/s40618-019-01057-y",
"author": "F Saponaro",
"doi-asserted-by": "publisher",
"first-page": "1285",
"issue": "11",
"journal-title": "J Endocrinol Invest",
"key": "7438_CR22",
"unstructured": "Saponaro F, Marcocci C, Zucchi R. Vitamin D status and cardiovascular outcome. J Endocrinol Invest. 2019;42(11):1285–90.",
"volume": "42",
"year": "2019"
},
{
"DOI": "10.3390/ijms21186483",
"author": "N Latic",
"doi-asserted-by": "publisher",
"first-page": "6483",
"issue": "18",
"journal-title": "Int J Mol Sci",
"key": "7438_CR23",
"unstructured": "Latic N, Erben RG. Vitamin D and cardiovascular disease, with emphasis on hypertension, atherosclerosis, and heart failure. Int J Mol Sci. 2020;21(18):6483.",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1038/nrcardio.2016.73",
"author": "S Pilz",
"doi-asserted-by": "publisher",
"first-page": "404",
"issue": "7",
"journal-title": "Nat Rev Cardiol",
"key": "7438_CR24",
"unstructured": "Pilz S, et al. Vitamin D and cardiovascular disease prevention. Nat Rev Cardiol. 2016;13(7):404–17.",
"volume": "13",
"year": "2016"
},
{
"DOI": "10.1038/s41371-020-0387-4",
"author": "RB Azevedo",
"doi-asserted-by": "publisher",
"first-page": "4",
"issue": "1",
"journal-title": "J Hum Hypertens",
"key": "7438_CR25",
"unstructured": "Azevedo RB, et al. Covid-19 and the cardiovascular system: a comprehensive review. J Hum Hypertens. 2021;35(1):4–11.",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1136/heartjnl-2020-317901",
"author": "S Bae",
"doi-asserted-by": "publisher",
"first-page": "373",
"issue": "5",
"journal-title": "Heart",
"key": "7438_CR26",
"unstructured": "Bae S, et al. Impact of cardiovascular disease and risk factors on fatal outcomes in patients with COVID-19 according to age: a systematic review and meta-analysis. Heart. 2021;107(5):373.",
"volume": "107",
"year": "2021"
},
{
"DOI": "10.1186/s12879-021-06168-7",
"author": "A Davoudi",
"doi-asserted-by": "publisher",
"first-page": "450",
"issue": "1",
"journal-title": "BMC Infect Dis",
"key": "7438_CR27",
"unstructured": "Davoudi A, et al. Lack of association between vitamin D insufficiency and clinical outcomes of patients with COVID-19 infection. BMC Infect Dis. 2021;21(1):450.",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1016/j.tcm.2019.05.003",
"author": "JM Flack",
"doi-asserted-by": "publisher",
"first-page": "160",
"issue": "3",
"journal-title": "Trends Cardiovasc Med",
"key": "7438_CR28",
"unstructured": "Flack JM, Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med. 2020;30(3):160–4.",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1186/s12931-020-01405-0",
"author": "C Mathyssen",
"doi-asserted-by": "publisher",
"first-page": "137",
"issue": "1",
"journal-title": "Respir Res",
"key": "7438_CR29",
"unstructured": "Mathyssen C, et al. Local expression profiles of vitamin D-related genes in airways of COPD patients. Respir Res. 2020;21(1):137.",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"author": "CE Hastie",
"doi-asserted-by": "publisher",
"first-page": "561",
"issue": "4",
"journal-title": "Diabetes Metab Syndr",
"key": "7438_CR30",
"unstructured": "Hastie CE, et al. Vitamin D concentrations and COVID-19 infection in UK Biobank. Diabetes Metab Syndr. 2020;14(4):561–5.",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1080/14787210.2021.1905519",
"author": "A Banerjee",
"doi-asserted-by": "publisher",
"first-page": "1245",
"issue": "10",
"journal-title": "Expert Rev Anti Infect Ther",
"key": "7438_CR31",
"unstructured": "Banerjee A, et al. Vitamin D and immuno-pathology of COVID-19: many interactions but uncertain therapeutic benefits. Expert Rev Anti Infect Ther. 2021;19(10):1245–58.",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1002/14651858.CD015043",
"author": "JK Stroehlein",
"doi-asserted-by": "publisher",
"journal-title": "Cochrane Database Syst Rev",
"key": "7438_CR32",
"unstructured": "Stroehlein JK, et al. Vitamin D supplementation for the treatment of COVID-19: a living systematic review. Cochrane Database Syst Rev. 2021. https://doi.org/10.1002/14651858.CD015043.",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.2648",
"author": "Z Wu",
"doi-asserted-by": "publisher",
"first-page": "1239",
"issue": "13",
"journal-title": "JAMA",
"key": "7438_CR33",
"unstructured": "Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) Outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239–42.",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.3390/nu12040988",
"author": "WB Grant",
"doi-asserted-by": "publisher",
"first-page": "988",
"issue": "4",
"journal-title": "Nutrients",
"key": "7438_CR34",
"unstructured": "Grant WB, et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12(4):988.",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.jsbmb.2021.105928",
"author": "M Diaz-Curiel",
"doi-asserted-by": "publisher",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "7438_CR35",
"unstructured": "Diaz-Curiel M, et al. The relationship between 25(OH) vitamin D levels and COVID-19 onset and disease course in Spanish patients. J Steroid Biochem Mol Biol. 2021;212: 105928.",
"volume": "212",
"year": "2021"
},
{
"DOI": "10.1016/j.clnesp.2021.05.021",
"author": "GD Pimentel",
"doi-asserted-by": "publisher",
"first-page": "466",
"journal-title": "Clin Nutr ESPEN",
"key": "7438_CR36",
"unstructured": "Pimentel GD, Dela Vega MCM, Pichard C. Low vitamin D levels and increased neutrophil in patients admitted at ICU with COVID-19. Clin Nutr ESPEN. 2021;44:466–8.",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-90189-4",
"author": "M Lakkireddy",
"doi-asserted-by": "publisher",
"first-page": "10641",
"issue": "1",
"journal-title": "Sci Rep",
"key": "7438_CR37",
"unstructured": "Lakkireddy M, et al. Impact of daily high dose oral vitamin D therapy on the inflammatory markers in patients with COVID 19 disease. Sci Rep. 2021;11(1):10641.",
"volume": "11",
"year": "2021"
},
{
"author": "A Rastogi",
"first-page": "87",
"issue": "1156",
"journal-title": "Postgrad Med J",
"key": "7438_CR38",
"unstructured": "Rastogi A, et al. Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study). Postgrad Med J. 2020;98(1156):87–90.",
"volume": "98",
"year": "2020"
},
{
"DOI": "10.3390/nu13072129",
"author": "S Zelzer",
"doi-asserted-by": "publisher",
"first-page": "2129",
"issue": "7",
"journal-title": "Nutrients",
"key": "7438_CR39",
"unstructured": "Zelzer S, et al. Vitamin D metabolites and clinical outcome in hospitalized COVID-19 patients. Nutrients. 2021;13(7):2129.",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1186/s12967-021-02838-x",
"author": "NM Al-Daghri",
"doi-asserted-by": "publisher",
"first-page": "166",
"issue": "1",
"journal-title": "J Transl Med",
"key": "7438_CR40",
"unstructured": "Al-Daghri NM, et al. Vitamin D status of Arab Gulf residents screened for SARS-CoV-2 and its association with COVID-19 infection: a multi-centre case–control study. J Transl Med. 2021;19(1):166.",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1371/journal.pmed.1003605",
"author": "G Butler-Laporte",
"doi-asserted-by": "publisher",
"issue": "6",
"journal-title": "PLoS Med",
"key": "7438_CR41",
"unstructured": "Butler-Laporte G, et al. Vitamin D and COVID-19 susceptibility and severity in the COVID-19 host genetics initiative: a Mendelian randomization study. PLoS Med. 2021;18(6): e1003605.",
"volume": "18",
"year": "2021"
},
{
"author": "H Azadeh",
"first-page": "30",
"issue": "195",
"journal-title": "J Mazand Univ Med Sci",
"key": "7438_CR42",
"unstructured": "Azadeh H, et al. Serum Vitamin D concentrations in CoVID19 patients. J Mazand Univ Med Sci. 2021;31(195):30–6.",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.1016/j.clnu.2020.10.055",
"author": "E Cereda",
"doi-asserted-by": "publisher",
"first-page": "2469",
"issue": "4",
"journal-title": "Clin Nutr",
"key": "7438_CR43",
"unstructured": "Cereda E, et al. Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital. Clin Nutr. 2021;40(4):2469–72.",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1111/ijcp.14649",
"author": "AP da Rocha",
"doi-asserted-by": "publisher",
"issue": "11",
"journal-title": "Int J Clin Pract",
"key": "7438_CR44",
"unstructured": "da Rocha AP, et al. Insufficient evidence for vitamin D use in COVID-19: A rapid systematic review. Int J Clin Pract. 2021;75(11): e14649.",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.1093/advances/nmab012",
"author": "A Kazemi",
"doi-asserted-by": "publisher",
"first-page": "1636",
"issue": "5",
"journal-title": "Adv Nutr",
"key": "7438_CR45",
"unstructured": "Kazemi A, et al. Association of vitamin D status with SARS-CoV-2 infection or COVID-19 severity: a systematic review and meta-analysis. Adv Nutr. 2021;12(5):1636–58.",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1080/10408398.2020.1841090",
"author": "M Pereira",
"doi-asserted-by": "publisher",
"first-page": "1308",
"issue": "5",
"journal-title": "Crit Rev Food Sci Nutr",
"key": "7438_CR46",
"unstructured": "Pereira M, et al. Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2020;62(5):1308–16.",
"volume": "62",
"year": "2020"
},
{
"author": "I Mozos",
"journal-title": "Biomed Res Int",
"key": "7438_CR47",
"unstructured": "Mozos I, Marginean O. Links between vitamin D deficiency and cardiovascular diseases. Biomed Res Int. 2015;2015: 109275.",
"volume": "2015",
"year": "2015"
},
{
"DOI": "10.1016/j.jacc.2008.08.050",
"author": "JH Lee",
"doi-asserted-by": "publisher",
"first-page": "1949",
"issue": "24",
"journal-title": "J Am Coll Cardiol",
"key": "7438_CR48",
"unstructured": "Lee JH, et al. Vitamin D deficiency an important, common, and easily treatable cardiovascular risk factor? J Am Coll Cardiol. 2008;52(24):1949–56.",
"volume": "52",
"year": "2008"
},
{
"DOI": "10.1016/j.repc.2020.10.014",
"author": "A Naghedi",
"doi-asserted-by": "publisher",
"first-page": "447",
"issue": "6",
"journal-title": "Rev Port Cardiol",
"key": "7438_CR49",
"unstructured": "Naghedi A, et al. Effect of vitamin D supplements on left ventricular ejection fraction in patients with heart failure: A systematic review and meta-analysis of randomized controlled trials. Rev Port Cardiol. 2021;40(6):447–55.",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.3390/medicina57080774",
"author": "C Batsi",
"doi-asserted-by": "publisher",
"first-page": "774",
"issue": "8",
"journal-title": "Medicina",
"key": "7438_CR50",
"unstructured": "Batsi C, et al. Vitamin D deficiency as a risk factor for myocardial ischemia. Medicina. 2021;57(8):774.",
"volume": "57",
"year": "2021"
},
{
"DOI": "10.1093/ajcn/83.4.754",
"author": "SS Schleithoff",
"doi-asserted-by": "publisher",
"first-page": "754",
"issue": "4",
"journal-title": "Am J Clin Nutr",
"key": "7438_CR51",
"unstructured": "Schleithoff SS, et al. Vitamin D supplementation improves cytokine profiles in patients with congestive heart failure: a double-blind, randomized, placebo-controlled trial. Am J Clin Nutr. 2006;83(4):754–9.",
"volume": "83",
"year": "2006"
},
{
"DOI": "10.1016/j.amjcard.2018.05.013",
"author": "A Turin",
"doi-asserted-by": "publisher",
"first-page": "780",
"issue": "5",
"journal-title": "Am J Cardiol",
"key": "7438_CR52",
"unstructured": "Turin A, et al. Interactions among vitamin D, atrial fibrillation, and the renin–angiotensin–aldosterone system. Am J Cardiol. 2018;122(5):780–4.",
"volume": "122",
"year": "2018"
},
{
"DOI": "10.21470/1678-9741-2018-0322",
"author": "L Bie",
"doi-asserted-by": "publisher",
"first-page": "605",
"issue": "5",
"journal-title": "Braz J Cardiovasc Surg",
"key": "7438_CR53",
"unstructured": "Bie L. The status and research progress on vitamin D deficiency and atrial fibrillation. Braz J Cardiovasc Surg. 2019;34(5):605–9.",
"volume": "34",
"year": "2019"
},
{
"DOI": "10.1038/s41569-020-0360-5",
"author": "YY Zheng",
"doi-asserted-by": "publisher",
"first-page": "259",
"issue": "5",
"journal-title": "Nat Rev Cardiol",
"key": "7438_CR54",
"unstructured": "Zheng YY, et al. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259–60.",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.repc.2020.11.007",
"author": "D Mesquita",
"doi-asserted-by": "publisher",
"first-page": "573",
"issue": "8",
"journal-title": "Rev Port Cardiol",
"key": "7438_CR55",
"unstructured": "Mesquita D, et al. Cardiac arrhythmias in patients presenting with COVID-19 treated in Portuguese hospitals: A national registry from the Portuguese association of arrhythmology, pacing and electrophysiology. Rev Port Cardiol. 2021;40(8):573–80.",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1111/pace.14247",
"author": "S Garcia-Zamora",
"doi-asserted-by": "publisher",
"first-page": "1062",
"issue": "6",
"journal-title": "Pacing Clin Electrophysiol",
"key": "7438_CR56",
"unstructured": "Garcia-Zamora S, et al. Arrhythmias and electrocardiographic findings in Coronavirus disease 2019: A systematic review and meta-analysis. Pacing Clin Electrophysiol. 2021;44(6):1062–74.",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1016/j.atherosclerosis.2008.10.033",
"author": "J Kendrick",
"doi-asserted-by": "publisher",
"first-page": "255",
"issue": "1",
"journal-title": "Atherosclerosis",
"key": "7438_CR57",
"unstructured": "Kendrick J, et al. 25-Hydroxyvitamin D deficiency is independently associated with cardiovascular disease in the third national health and nutrition examination survey. Atherosclerosis. 2009;205(1):255–60.",
"volume": "205",
"year": "2009"
},
{
"DOI": "10.34172/jcvtr.2021.30",
"author": "S Mirmoeeni",
"doi-asserted-by": "publisher",
"first-page": "181",
"issue": "3",
"journal-title": "J Cardiovasc Thorac Res.",
"key": "7438_CR58",
"unstructured": "Mirmoeeni S, et al. Cardiovascular manifestations in COVID-19 patients: a systematic review and meta-analysis. J Cardiovasc Thorac Res. 2021;13(3):181.",
"volume": "13",
"year": "2021"
}
],
"reference-count": 58,
"references-count": 58,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-022-07438-8"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases"
],
"subtitle": [],
"title": "Comparison of the cardiovascular system, clinical condition, and laboratory results in COVID-19 patients with and without vitamin D insufficiency",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "22"
}
