Multidrug-Resistant Infections and Outcome of Critically Ill Patients with Coronavirus Disease 2019: A Single Center Experience
et al., Microbial Drug Resistance, doi:10.1089/mdr.2020.0489, Sep 2021
Retrospective 32 ICU patients showing lower mortality with aspirin treatment, without statistical significance.
Study covers HCQ and aspirin.
|
risk of death, 46.3% lower, RR 0.54, p = 0.63, treatment 1 of 5 (20.0%), control 22 of 27 (81.5%), NNT 1.6, adjusted per study, odds ratio converted to relative risk, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Karruli et al., 1 Sep 2021, retrospective, Italy, peer-reviewed, 13 authors, study period March 2020 - May 2020.
Multidrug-Resistant Infections and Outcome of Critically Ill Patients with Coronavirus Disease 2019: A Single Center Experience
Microbial Drug Resistance, doi:10.1089/mdr.2020.0489
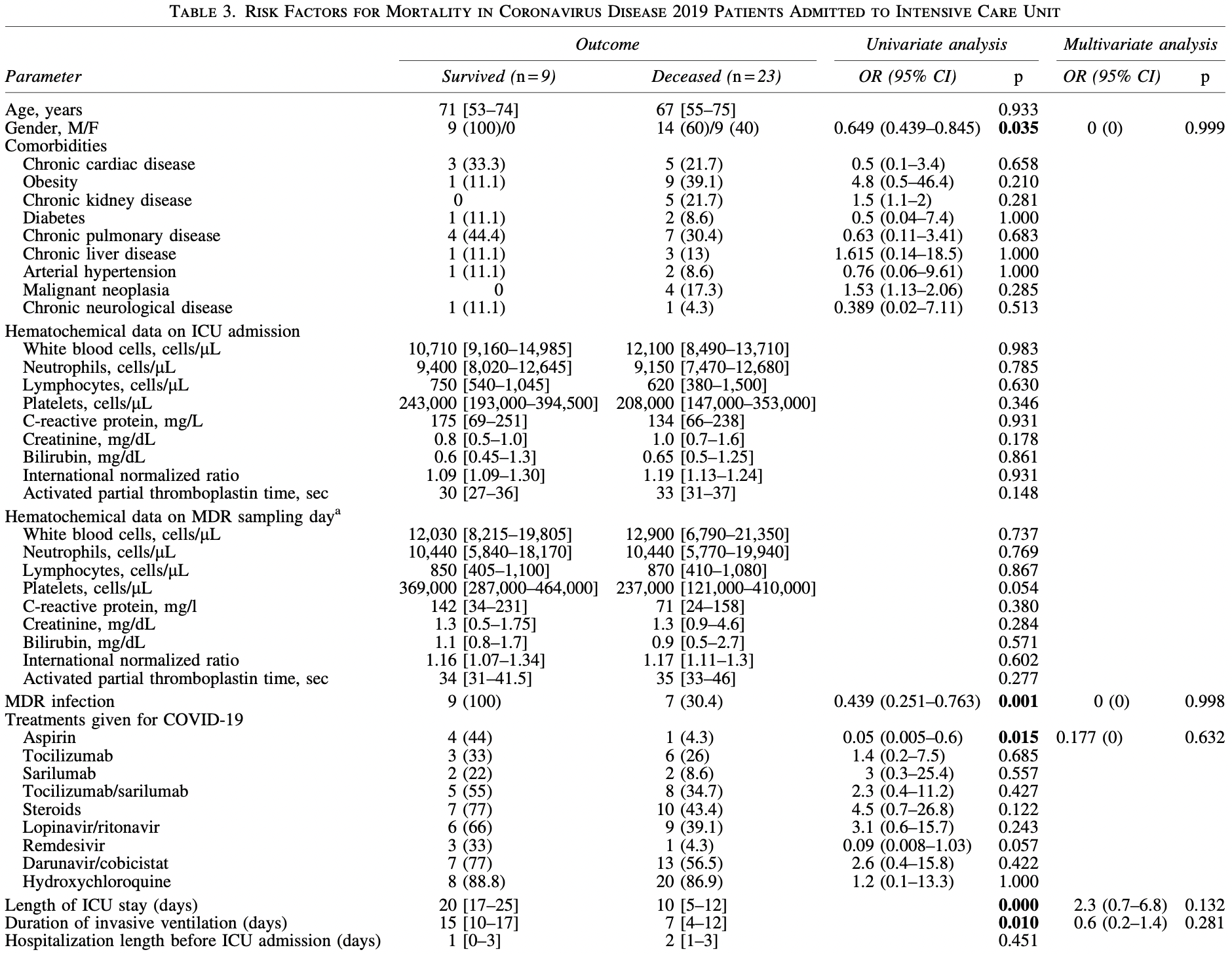
Background: The aim of this study was to assess the drivers of multidrug-resistant (MDR) bacterial infection development in coronavirus disease 2019 (COVID-19) and its impact on patient outcome. Methods: Retrospective analysis on data from 32 consecutive patients with COVID-19, admitted to our intensive care unit (ICU) from March to May 2020. Outcomes considered were MDR infection and ICU mortality. Results: Fifty percent of patients developed an MDR infection during ICU stay after a median time of 8 [4-11] days. Most common MDR pathogens were carbapenem-resistant Klebsiella pneumoniae and Acinetobacter baumannii, causing bloodstream infections and pneumonia. MDR infections were linked to a higher length of ICU stay ( p = 0.002), steroid therapy ( p = 0.011), and associated with a lower ICU mortality (odds ratio: 0.439, 95% confidence interval: 0.251-0.763; p < 0.001). Low-dose aspirin intake was associated with both MDR infection ( p = 0.043) and survival ( p = 0.015). Among MDR patients, mortality was related with piperacillintazobactam use ( p = 0.035) and an earlier onset of MDR infection ( p = 0.042). Conclusions: MDR infections were a common complication in critically ill COVID-19 patients at our center. MDR risk was higher among those dwelling longer in the ICU and receiving steroids. However, MDR infections were not associated with a worse outcome.
Ethics Approval The study and its observational procedures were approved by our institutional ethics committee.
Authors' Contributions All authors have contributed to and agreed on the content of the article, and the respective roles of each author are as follows: A.K., F.B., R.Z., and E.D.-M. worked on concept of the study; M.G., F.P., M.P.U., and P.S. worked on data collection and data interpretation; A.K., R.Z., and E.D.-M. drafted the article. All authors read, critically revised, and approved the final version of the article.
Disclosure Statement Authors have no conflict of interest to disclose relevant to the content of this study. E.D.-M. received grant support and personal fees, outside of this study, from Roche, Pfizer, MSD, Angelini, Bio-Merieux, Abbvie, Nordic Pharma, Sanofi-Aventis, Medtronic, and DiaSorin. R.Z. and R.A. received personal fees, outside of this study, from Nordic Pharma.
Supplementary Material Supplementary Table S1
References
Abelha, Castro, Landeiro, Neves, Santos, Mortality and length of stay in a surgical intensive care unit, Rev. Bras. Anestesiol
Choudhuri, Ahuja, Biswas, Uppal, Epidemiology of multidrug resistant infections after inter-ICU transfer in India, Indian J. Crit. Care Med
Docherty, Harrison, Green, Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study, BMJ
Du, Liang, Yang, Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study, Eur. Respir. J
Garcia, Fumeaux, Guerci, Prognostic factors associated with mortality risk and disease progression in 639 critically ill patients with COVID-19 in Europe: initial report of the international RISC-19-ICU prospective observational cohort, EClinicalMedicine
Grasselli, Greco, Zanella, Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy, JAMA Intern. Med
Grasselli, Zangrillo, Zanella, Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy, JAMA
Gudiol, Tubau, Calatayud, Bacteraemia due to multidrug-resistant Gram-negative bacilli in cancer patients: risk factors, antibiotic therapy and outcomes, J. Antimicrob. Chemother
Horan, Andrus, Dudeck, CDC/NHSN surveillance definition of health careassociated infection and criteria for specific types of infections in the acute care setting, Am. J. Infect. Control
Hotchkiss, Monneret, Payen, Immunosuppression in sepsis: a novel understanding of the disorder and a new therapeutic approach, Lancet Infect. Dis
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, Lancet
Humphreys, Fitzpatick, Harvey, Gender differences in rates of carriage and bloodstream infection caused by methicillin-resistant Staphylococcus aureus: are they real, do they matter and why?, Clin. Infect. Dis
Kang, Lee, Lee, Hwang, Han, Prevalence of and risk factors for multidrugresistant bacteria in urine cultures of spinal cord injury patients, Ann. Rehabil. Med
Lat, Daley, Shewale, A multicenter, prospective, observational study to determine predictive factors for multidrug-resistant pneumonia in critically Ill adults: the DEFINE Study, Pharmacotherapy
Li, Huang, Zou, Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes, J. Med. Virol, doi:10.1002/jmv.26424
Magiorakos, Srinivasan, Carey, Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance, Clin. Microbiol. Infect
Phua, Weng, Ling, Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations, Lancet Respir. Med
Qin, Zhou, Hu, Dysregulation of immune response in patients with COVID-19 in Wuhan, China, Clin. Infect. Dis
Siwakoti, Subedi, Sharma, Baral, Bhattarai et al., Incidence and outcomes of multidrug-resistant gram-negative bacteria infections in intensive care unit from Nepal-a prospective cohort study, Antimicrob. Resist. Infect. Control
Tabah, Koulenti, Laupland, Characteristics and determinants of outcome of hospitalacquired bloodstream infections in intensive care units: the EUROBACT International Cohort Study, Intensive Care Med
Tosi, Roat, Biasi, Multidrug resistant bacteria in critically ill patients: a step further antibiotic therapy, J. Emerg. Crit. Care Med
Tumbarello, Repetto, Trecarichi, Multidrug-resistant Pseudomonas aeruginosa bloodstream infections: risk factors and mortality, Epidemiol. Infect
Vincent, Rello, Marshall, International study of the prevalence and outcomes of infection in intensive care units, JAMA
Wang, Hu, Hu, Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, JAMA
Wei, Zhao, Analysis of multidrug-resistant bacteria in 3223 patients with hospitalacquired infections (HAI) from a tertiary general hospital in China, Bosn. J. Basic Med. Sci
Yu, Xu, Fu, Patients with COVID-19 in 19 ICUs in Wuhan, China: a cross-sectional study, Crit. Care
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.1089/mdr.2020.0489",
"ISSN": [
"1076-6294",
"1931-8448"
],
"URL": "http://dx.doi.org/10.1089/mdr.2020.0489",
"alternative-id": [
"10.1089/mdr.2020.0489"
],
"author": [
{
"affiliation": [
{
"name": "Department of Precision Medicine, University of Campania “L. Vanvitelli”, Napoli, Italy."
}
],
"family": "Karruli",
"given": "Arta",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Precision Medicine, University of Campania “L. Vanvitelli”, Napoli, Italy."
}
],
"family": "Boccia",
"given": "Filomena",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Precision Medicine, University of Campania “L. Vanvitelli”, Napoli, Italy."
}
],
"family": "Gagliardi",
"given": "Massimo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Precision Medicine, University of Campania “L. Vanvitelli”, Napoli, Italy."
}
],
"family": "Patauner",
"given": "Fabian",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Precision Medicine, University of Campania “L. Vanvitelli”, Napoli, Italy."
}
],
"family": "Ursi",
"given": "Maria Paola",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Precision Medicine, University of Campania “L. Vanvitelli”, Napoli, Italy."
}
],
"family": "Sommese",
"given": "Pino",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Intensive Care Unit, AORN Ospedali dei Colli-Monaldi Hospital, Napoli, Italy."
}
],
"family": "De Rosa",
"given": "Rosanna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Intensive Care Unit, AORN Ospedali dei Colli-Monaldi Hospital, Napoli, Italy."
}
],
"family": "Murino",
"given": "Patrizia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Microbiology and Virology Laboratory, AORN Ospedali dei Colli-Monaldi Hospital, Napoli, Italy."
}
],
"family": "Ruocco",
"given": "Giuseppe",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Intensive Care Unit, AORN Ospedali dei Colli-Monaldi Hospital, Napoli, Italy."
}
],
"family": "Corcione",
"given": "Antonio",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Unit of Infectious and Transplant Medicine, AORN Ospedali dei Colli-Monaldi Hospital, Napoli, Italy."
}
],
"family": "Andini",
"given": "Roberto",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Unit of Infectious and Transplant Medicine, AORN Ospedali dei Colli-Monaldi Hospital, Napoli, Italy."
},
{
"name": "Department of Advanced Medical and Surgical Sciences, University of Campania “L. Vanvitelli”, Napoli, Italy."
}
],
"family": "Zampino",
"given": "Rosa",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Precision Medicine, University of Campania “L. Vanvitelli”, Napoli, Italy."
},
{
"name": "Unit of Infectious and Transplant Medicine, AORN Ospedali dei Colli-Monaldi Hospital, Napoli, Italy."
}
],
"family": "Durante-Mangoni",
"given": "Emanuele",
"sequence": "additional"
}
],
"container-title": [
"Microbial Drug Resistance"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
2,
18
]
],
"date-time": "2021-02-18T17:03:51Z",
"timestamp": 1613667831000
},
"deposited": {
"date-parts": [
[
2021,
9,
14
]
],
"date-time": "2021-09-14T16:14:16Z",
"timestamp": 1631636056000
},
"indexed": {
"date-parts": [
[
2021,
12,
22
]
],
"date-time": "2021-12-22T21:42:51Z",
"timestamp": 1640209371261
},
"is-referenced-by-count": 12,
"issn-type": [
{
"type": "print",
"value": "1076-6294"
},
{
"type": "electronic",
"value": "1931-8448"
}
],
"issue": "9",
"issued": {
"date-parts": [
[
2021,
9,
1
]
]
},
"journal-issue": {
"issue": "9",
"published-print": {
"date-parts": [
[
2021,
9,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.liebertpub.com/nv/resources-tools/text-and-data-mining-policy/121/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
1
]
],
"date-time": "2021-09-01T00:00:00Z",
"timestamp": 1630454400000
}
}
],
"link": [
{
"URL": "https://www.liebertpub.com/doi/full-xml/10.1089/mdr.2020.0489",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.liebertpub.com/doi/pdf/10.1089/mdr.2020.0489",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "278",
"original-title": [],
"page": "1167-1175",
"prefix": "10.1089",
"published": {
"date-parts": [
[
2021,
9,
1
]
]
},
"published-print": {
"date-parts": [
[
2021,
9,
1
]
]
},
"publisher": "Mary Ann Liebert Inc",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"doi-asserted-by": "publisher",
"key": "B2"
},
{
"DOI": "10.1002/jmv.26424",
"doi-asserted-by": "publisher",
"key": "B3"
},
{
"DOI": "10.1136/bmj.m1985",
"doi-asserted-by": "publisher",
"key": "B4"
},
{
"author": "Wang D.",
"key": "B5",
"volume-title": "et al",
"year": "1069"
},
{
"DOI": "10.1016/S2213-2600(20)30161-2",
"doi-asserted-by": "publisher",
"key": "B6"
},
{
"DOI": "10.1001/jamainternmed.2020.3539",
"doi-asserted-by": "publisher",
"key": "B7"
},
{
"DOI": "10.1016/j.eclinm.2020.100449",
"doi-asserted-by": "publisher",
"key": "B8"
},
{
"DOI": "10.1183/13993003.00524-2020",
"doi-asserted-by": "publisher",
"key": "B9"
},
{
"author": "Zhou F.",
"key": "B10",
"volume-title": "et al",
"year": "1062"
},
{
"DOI": "10.1001/jama.2020.5394",
"doi-asserted-by": "publisher",
"key": "B11"
},
{
"DOI": "10.1002/phar.2171",
"doi-asserted-by": "publisher",
"key": "B12"
},
{
"DOI": "10.1007/s00134-012-2695-9",
"doi-asserted-by": "publisher",
"key": "B13"
},
{
"DOI": "10.1001/jama.2009.1754",
"doi-asserted-by": "publisher",
"key": "B14"
},
{
"DOI": "10.21037/jeccm.2018.11.08",
"doi-asserted-by": "publisher",
"key": "B15"
},
{
"DOI": "10.17305/bjbms.2018.3826",
"doi-asserted-by": "publisher",
"key": "B16"
},
{
"DOI": "10.1016/S1473-3099(13)70001-X",
"doi-asserted-by": "publisher",
"key": "B17"
},
{
"DOI": "10.1093/cid/ciaa248",
"doi-asserted-by": "publisher",
"key": "B18"
},
{
"DOI": "10.1186/s13054-020-02939-x",
"doi-asserted-by": "publisher",
"key": "B20"
},
{
"DOI": "10.1111/j.1469-0691.2011.03570.x",
"doi-asserted-by": "publisher",
"key": "B21"
},
{
"DOI": "10.1016/j.ajic.2008.03.002",
"doi-asserted-by": "publisher",
"key": "B22"
},
{
"DOI": "10.1186/s13756-018-0404-3",
"doi-asserted-by": "publisher",
"key": "B23"
},
{
"DOI": "10.5005/jp-journals-10071-23103",
"doi-asserted-by": "publisher",
"key": "B24"
},
{
"DOI": "10.1590/S0034-70942006000100005",
"doi-asserted-by": "publisher",
"key": "B25"
},
{
"DOI": "10.1017/S0950268810003055",
"doi-asserted-by": "publisher",
"key": "B26"
},
{
"DOI": "10.1093/jac/dkq494",
"doi-asserted-by": "publisher",
"key": "B27"
},
{
"DOI": "10.5535/arm.2015.39.5.686",
"doi-asserted-by": "publisher",
"key": "B28"
},
{
"author": "Humphreys H.",
"first-page": "1708",
"journal-title": "Infect. Dis",
"key": "B29",
"volume": "61",
"year": "2015"
}
],
"reference-count": 27,
"references-count": 27,
"relation": {},
"score": 1,
"short-container-title": [
"Microbial Drug Resistance"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Microbiology (medical)",
"Pharmacology",
"Immunology",
"Microbiology"
],
"subtitle": [],
"title": [
"Multidrug-Resistant Infections and Outcome of Critically Ill Patients with Coronavirus Disease 2019: A Single Center Experience"
],
"type": "journal-article",
"volume": "27"
}