Prevalent Metformin Use in Adults With Diabetes and the Incidence of Long COVID: An EHR-Based Cohort Study From the RECOVER Program
et al., Diabetes Care, doi:10.2337/DCa24-0032, Sep 2024
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
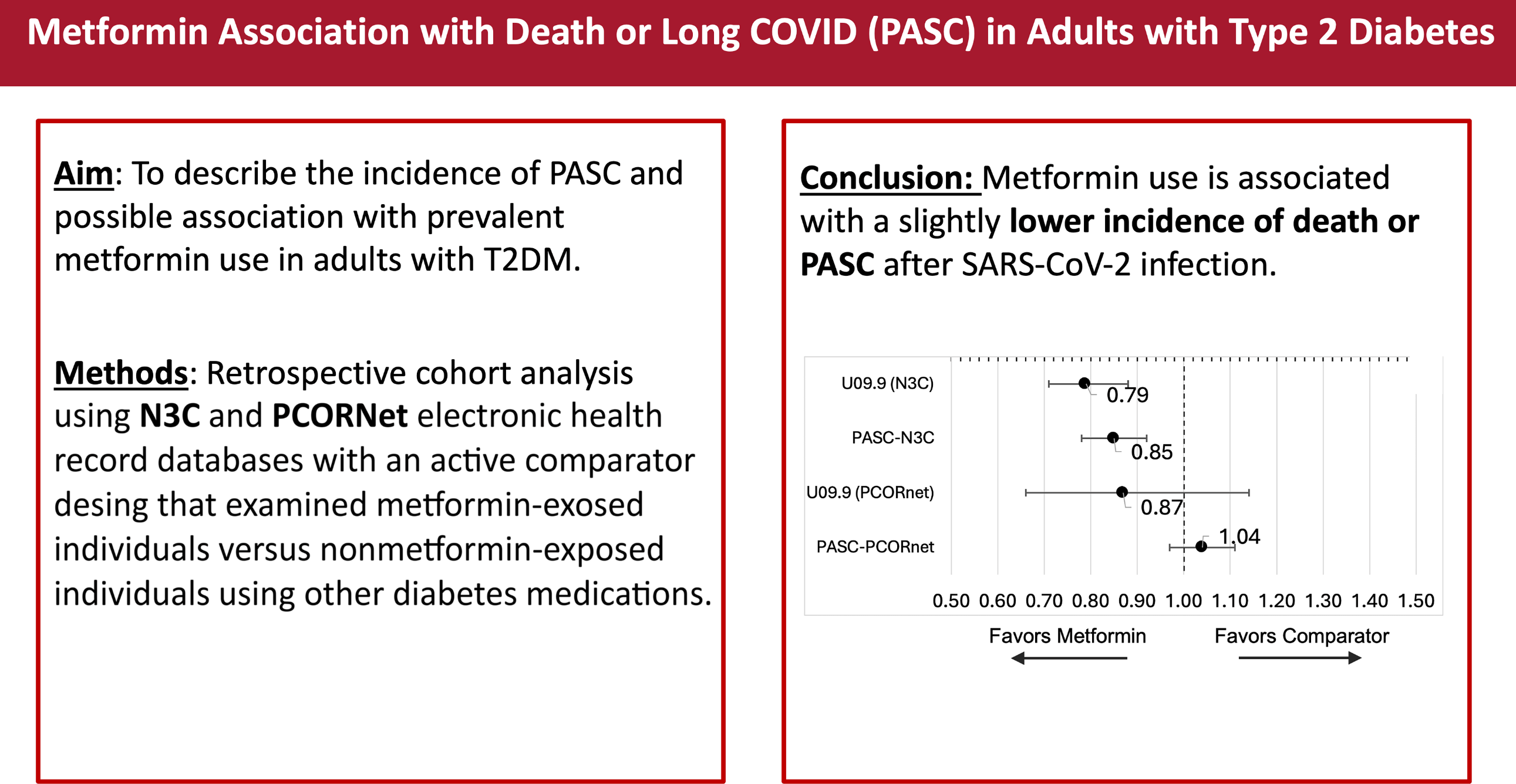
N3C/PCORnet retrospective adults with type 2 diabetes in the USA showing lower incidence of mortality or long COVID with metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
death or long COVID, 11.3% lower, HR 0.89, p = 0.11, treatment 42,275, control 6,713, combined.
|
|
death or long COVID, 21.0% lower, HR 0.79, p < 0.001, treatment 42,275, control 6,713, N3C, EHR code.
|
|
death or long COVID, 15.0% lower, HR 0.85, p < 0.001, treatment 42,275, control 6,713, N3C, phenotype.
|
|
death or long COVID, 13.0% lower, HR 0.87, p = 0.32, treatment 30,748, control 5,933, PCORnet, EHR code.
|
|
death or long COVID, 4.0% higher, HR 1.04, p = 0.26, treatment 30,748, control 5,933, PCORnet, phenotype.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Johnson et al., 17 Sep 2024, retrospective, USA, peer-reviewed, 19 authors.
DOI record:
{
"DOI": "10.2337/dca24-0032",
"ISSN": [
"0149-5992",
"1935-5548"
],
"URL": "http://dx.doi.org/10.2337/DCa24-0032",
"abstract": "<jats:sec>\n <jats:title>OBJECTIVE</jats:title>\n <jats:p>Studies show metformin use before and during SARS-CoV-2 infection reduces severe COVID-19 and postacute sequelae of SARS-CoV-2 (PASC) in adults. Our objective was to describe the incidence of PASC and possible associations with prevalent metformin use in adults with type 2 diabetes mellitus (T2DM).</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>RESEARCH DESIGN AND METHODS</jats:title>\n <jats:p>This is a retrospective cohort analysis using the National COVID Cohort Collaborative (N3C) and Patient-Centered Clinical Research Network (PCORnet) electronic health record (EHR) databases with an active comparator design that examined metformin-exposed individuals versus nonmetformin-exposed individuals who were taking other diabetes medications. T2DM was defined by HbA1C ≥6.5 or T2DM EHR diagnosis code. The outcome was death or PASC within 6 months, defined by EHR code or computable phenotype.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>RESULTS</jats:title>\n <jats:p>In the N3C, the hazard ratio (HR) for death or PASC with a U09.9 diagnosis code (PASC-U09.0) was 0.79 (95% CI 0.71–0.88; P &lt; 0.001), and for death or N3C computable phenotype PASC (PASC-N3C) was 0.85 (95% CI 0.78–0.92; P &lt; 0.001). In PCORnet, the HR for death or PASC-U09.9 was 0.87 (95% CI 0.66–1.14; P = 0.08), and for death or PCORnet computable phenotype PASC (PASC-PCORnet) was 1.04 (95% CI 0.97–1.11; P = 0.58). Incident PASC by diagnosis code was 1.6% metformin vs. 2.0% comparator in the N3C, and 2.1% metformin vs. 2.5% comparator in PCORnet. By computable phenotype, incidence was 4.8% metformin and 5.2% comparator in the N3C and 24.7% metformin vs. 26.1% comparator in PCORnet.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>CONCLUSIONS</jats:title>\n <jats:p>Prevalent metformin use is associated with a slightly lower incidence of death or PASC after SARS-CoV-2 infection. PASC incidence by computable phenotype is higher than by EHR code, especially in PCORnet. These data are consistent with other observational analyses showing prevalent metformin is associated with favorable outcomes after SARS-CoV-2 infection in adults with T2DM.</jats:p>\n </jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-2983-6384",
"affiliation": [
{
"name": "1Institute for Health Informatics, University of Minnesota, Minneapolis, MN"
}
],
"authenticated-orcid": false,
"family": "Johnson",
"given": "Steven G.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "2Information Technologies and Services Department, Weill Cornell Medicine, New York, NY"
}
],
"family": "Abedian",
"given": "Sajjad",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "3Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC"
}
],
"family": "Stürmer",
"given": "Til",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "4Division of Biostatistics and Health Data Science, University of Minnesota School of Public Health, Minneapolis, MN"
}
],
"family": "Huling",
"given": "Jared D.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "5Department of Population Health Sciences, Weill Cornell Medicine, New York, NY"
}
],
"family": "Lewis V",
"given": "Colby",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9723-3876",
"affiliation": [
{
"name": "6Division of Endocrinology, Department of Medicine, University of North Carolina School of Medicine, Chapel Hill, NC"
}
],
"authenticated-orcid": false,
"family": "Buse",
"given": "John B.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "7Department of Medicine, New York University Grossman School of Medicine, New York, NY"
}
],
"family": "Brosnahan",
"given": "Shari B.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "8Department of Population Health, New York University Grossman School of Medicine, New York, NY"
}
],
"family": "Mudumbi",
"given": "Praveen C.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "9University of Colorado, Anschutz Medical Campus, Aurora, CO"
}
],
"family": "Erlandson",
"given": "Kristine M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "10Case Western Reserve University, Cleveland, OH"
}
],
"family": "McComsey",
"given": "Grace A.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "11Division of General Internal Medicine, University of Pittsburgh School of Medicine, Pittsburgh, PA"
}
],
"family": "Arnold",
"given": "Jonathan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "1Institute for Health Informatics, University of Minnesota, Minneapolis, MN"
}
],
"family": "Wiggen",
"given": "Talia D.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "12Department of Biomedical Informatics and the Department of Internal Medicine, Stony Brook University, Stony Brook, NY"
}
],
"family": "Wong",
"given": "Rachel",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "13Mass General Brigham, Boston, MA"
}
],
"family": "Murphy",
"given": "Shawn",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "14MaineHealth Institute for Research, Scarborough, ME"
}
],
"family": "Rosen",
"given": "Clifford",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "5Department of Population Health Sciences, Weill Cornell Medicine, New York, NY"
}
],
"family": "Kaushal",
"given": "Rainu",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "5Department of Population Health Sciences, Weill Cornell Medicine, New York, NY"
}
],
"family": "Weiner",
"given": "Mark G.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "15Division of General Internal Medicine, Department of Medicine, University of Minnesota Medical School, Minneapolis, MN"
}
],
"family": "Bramante",
"given": "Carolyn",
"sequence": "additional"
},
{
"affiliation": [],
"name": "RECOVER PCORnet EHR Cohort and the N3C Consortium",
"sequence": "additional"
}
],
"container-title": "Diabetes Care",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"diabetesjournals.org"
]
},
"created": {
"date-parts": [
[
2024,
9,
17
]
],
"date-time": "2024-09-17T17:58:16Z",
"timestamp": 1726595896000
},
"deposited": {
"date-parts": [
[
2024,
9,
17
]
],
"date-time": "2024-09-17T17:58:18Z",
"timestamp": 1726595898000
},
"funder": [
{
"DOI": "10.13039/100006108",
"award": [
"UM1TR004406",
"UM1TR004528"
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/100006108",
"id-type": "DOI"
}
],
"name": "National Center for Advancing Translational Sciences"
},
{
"DOI": "10.13039/100000062",
"award": [
"DK124654"
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/100000062",
"id-type": "DOI"
}
],
"name": "National Institute of Diabetes and Digestive and Kidney Diseases"
},
{
"award": [
"P30DK124723"
],
"name": "NC Diabetes Research Center"
},
{
"DOI": "10.13039/100000050",
"award": [
"OT2HL16184701"
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/100000050",
"id-type": "DOI"
}
],
"name": "National Heart, Lung, and Blood Institute"
},
{
"DOI": "10.13039/100000049",
"award": [
"AG056479"
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/100000049",
"id-type": "DOI"
}
],
"name": "National Institute on Aging"
}
],
"indexed": {
"date-parts": [
[
2024,
9,
17
]
],
"date-time": "2024-09-17T18:40:21Z",
"timestamp": 1726598421108
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
9,
17
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.diabetesjournals.org/journals/pages/license",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
9,
17
]
],
"date-time": "2024-09-17T00:00:00Z",
"timestamp": 1726531200000
}
}
],
"link": [
{
"URL": "https://diabetesjournals.org/care/article-pdf/doi/10.2337/DCa24-0032/781872/dca240032.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://diabetesjournals.org/care/article-pdf/doi/10.2337/DCa24-0032/781872/dca240032.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1167",
"original-title": [],
"prefix": "10.2337",
"published": {
"date-parts": [
[
2024,
9,
17
]
]
},
"published-online": {
"date-parts": [
[
2024,
9,
17
]
]
},
"publisher": "American Diabetes Association",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://diabetesjournals.org/care/article/doi/10.2337/DCa24-0032/157171/Prevalent-Metformin-Use-in-Adults-With-Diabetes"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Prevalent Metformin Use in Adults With Diabetes and the Incidence of Long COVID: An EHR-Based Cohort Study From the RECOVER Program",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.2337/ada-journal-policies"
}
