Reduced Sleep in the Week Prior to Diagnosis of COVID-19 is Associated with the Severity of COVID-19
et al., Nature and Science of Sleep, doi:10.2147/NSS.S263488, Nov 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 164 COVID-19 patients and 188 controls in China, showing lower risk of cases with regular exercise.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
Study covers sleep and exercise.
|
risk of severe case, 46.8% lower, RR 0.53, p = 0.18, high activity levels 7 of 74 (9.5%), low activity levels 16 of 90 (17.8%), NNT 12, unadjusted, exercise habit, ≥1 time per week, excluded in exclusion analyses:
unadjusted results with no group details.
|
|
risk of severe case, 8.0% lower, RR 0.92, p = 1.00, high activity levels 3 of 23 (13.0%), low activity levels 20 of 141 (14.2%), NNT 88, unadjusted, ≥30 minutes ≥3 times per week, excluded in exclusion analyses:
unadjusted results with no group details.
|
|
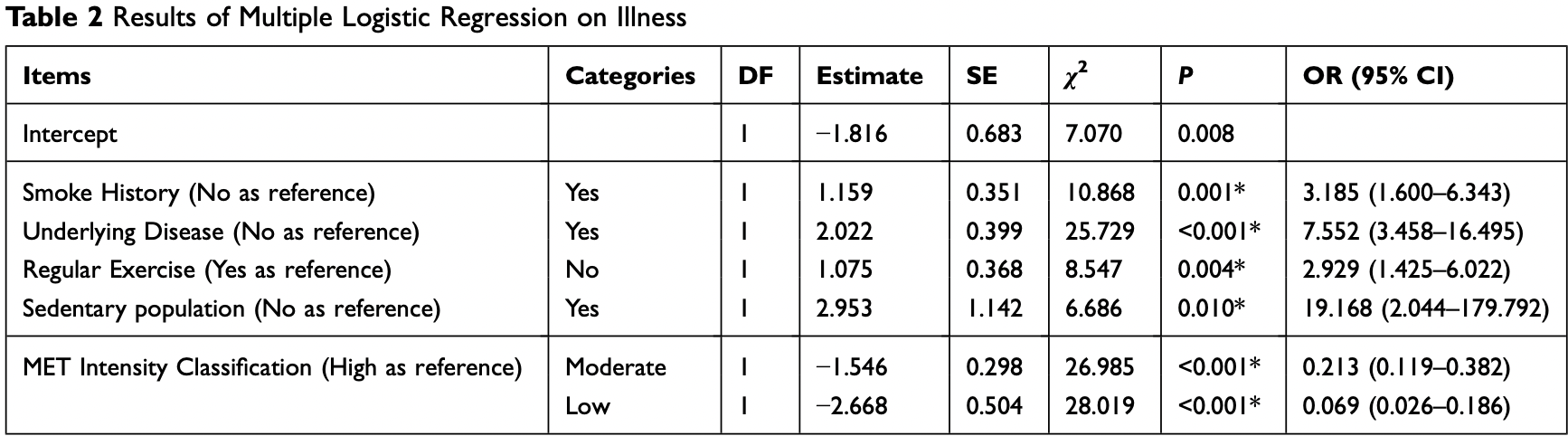
risk of case, 65.9% lower, OR 0.34, p = 0.004, adjusted per study, inverted to make OR<1 favor high activity levels, case control OR, regular exercise, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Huang et al., 30 Nov 2021, retrospective, China, peer-reviewed, survey, 5 authors, study period 10 February, 2020 - 28 March, 2020.
Contact: lidiangeng@126.com, bao03@163.com.
<p>Reduced Sleep in the Week Prior to Diagnosis of COVID-19 is Associated with the Severity of COVID-19</p>
Nature and Science of Sleep, doi:10.2147/nss.s263488
Background: The rapid outbreak of coronavirus disease 2019 (COVID-19) is a major health concern, in response to which widespread risk factor research is being carried out. Objective: To discover how physical activity and lifestyle affect the epidemic as well as the disease severity and prognosis of COVID-19 patients. Methods: This multicenter, retrospective cohort study included 203 adults infected with COVID-19 and 228 uninfected adults in three Chinese provinces, with 164 (80.7%) of the infected participants and 188 (82.5%) of the uninfected participants answering a doctoradministered telephone questionnaire on lifestyle. The binary logistic regression model and the ordinal logit model were used to observe relevance. Results: Comparing sick and non-sick patients, we found that irregular exercise (P=0.004), sedentary lifestyle (P=0.010), and overexertion (P<0.001) may be associated with the susceptibility to COVID-19. In symptomatic patients, using the recommended status as a reference, risk of severe infection increased with decreased sleep status, being 6.729 (95% CI=2.138-21.181) times higher for potentially appropriate sleep (P=0.001) and peaking at 8.612 (95% CI=1.913-38.760) times higher for lack of sleep (P=0.005). Reduction in average daily sleep time significantly increased the likely severity (P=0.002). Discussion: Through further examination of damage of external lung organs, we found that lack of sleep affected not only disease severity but also prognosis. Based on these findings, the public should prioritize a healthy lifestyle and get adequate sleep in response to the outbreak. The study of life habits may bring new ideas for the prevention and treatment of COVID-19.
Abbreviations COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; RT-PCR, real-time reverse-transcription polymerase-chainreaction; CT, computed tomography; IPAQ, International Physical Activity Questionnaire; NSF, National Sleep Foundation; OR, odds ratio; CI, confidence interval; BMI, body mass index; MET, metabolic equivalent of task.
Ethics Declarations The study complied with the Declaration of Helsinki and the ethical approval in this study was obtained from the Research and Ethics Committee of the Chinese PLA General Hospital (No. S2020-063-01). All patients involved in this study signed informed consent.
Author Contributions Baozhen Huang and Yanlin Niu contributed the same in this study. All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure The authors declare that they have no conflict of interest for this work.
Nature and Science of Sleep
Dovepress
References
Boon, Hamlin, Steel, Ross, Validation of the New Zealand Physical Activity Questionnaire (NZPAQ-LF) and the International Physical Activity Questionnaire (IPAQ-LF) with accelerometry, Br J Sports Med, doi:10.1136/bjsm.2008.052167
Bryant, Trinder, Curtis, Sick and tired: does sleep have a vital role in the immune system?, Nat Rev Immunol, doi:10.1038/nri1369
Cai, Sex difference and smoking predisposition in patients with COVID-19, Lancet Respir Med, doi:10.1016/S2213-2600(20)30117-X
Corman, Landt, Kaiser, Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR, Eurosurveillance, doi:10.2807/1560-7917.ES.2020.25.3.2000045
Fan, Hao, Yang, Clinical characteristics of COVID-19 and establishment of a disease risk prediction model, SSRN J, doi:10.2139/ssrn.3556660
Gleeson, Walsh, The BASES expert statement on exercise, immunity, and infection, J Sports Sci, doi:10.1080/02640414.2011.627371
Guan, Liang, Zhao, Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis, Eur Respir J, doi:10.1183/13993003.00547-2020
Iibarra-Coronado, Pantaleón-Martínez, Velazquéz-Moctezuma, The bidirectional relationship between sleep and immunity against infections, J Immunol Res, doi:10.1155/2015/678164
Irwin, Mcclintick, Costlow, Fortner, White et al., Partial night sleep deprivation reduces natural killer and cellular immune responses in humans, FASEB J, doi:10.1096/fasebj.10.5.8621064
Khair, Nwaneri, Damico, Kolb, Hassoun et al., The minimal important difference in borg dyspnea score in pulmonary arterial hypertension, Ann Am Thorac Soc, doi:10.1513/AnnalsATS.201512-824OC
Krueger, The role of cytokines in sleep regulation, CPD, doi:10.2174/138161208786549281
Lowder, Padgett, Woods, Moderate exercise protects mice from death due to influenza virus, Brain Behav Immun, doi:10.1016/j.bbi.2005.04.002
Martin, Pence, Woods, Exercise and respiratory tract viral infections, Exerc Sport Sci Rev, doi:10.1097/JES.0b013e3181b7b57b
Murthy, Gomersall, Fowler, Care for critically Ill patients with COVID-19, JAMA, doi:10.1001/jama.2020.3633
Patel, Malhotra, Gao, Hu, Neuman et al., A prospective study of sleep duration and pneumonia risk in women, Sleep, doi:10.5665/sleep.1594
Prather, Leung, Association of insufficient sleep with respiratory infection among adults in the United States, JAMA Intern Med, doi:10.1001/jamainternmed.2016.0787
Scholes, Bridges, Ng Fat, Mindell, Brucki, Comparison of the physical activity and sedentary behaviour assessment questionnaire and the short-form international physical activity questionnaire: an analysis of health survey for England data. Brucki S, PLoS One, doi:10.1371/journal.pone.0151647
Who, None
Zhao, Zhao, Wang, Zhou, Ma et al., Single-cell RNA expression profiling of ACE2, the receptor of SARS-CoV-2, Bioinformatics, doi:10.1101/2020.01.26.919985
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
Zhu, Zhao, Lai, Dose-response association between risk factors and incidence of COVID-19 in 325 hospitalized patients: a Multicenter Retrospective Cohort Study, doi:10.2139/ssrn.3562478
DOI record:
{
"DOI": "10.2147/nss.s263488",
"ISSN": [
"1179-1608"
],
"URL": "http://dx.doi.org/10.2147/NSS.S263488",
"author": [
{
"affiliation": [],
"family": "Huang",
"given": "Baozhen",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-4946-3028",
"affiliation": [],
"authenticated-orcid": true,
"family": "Niu",
"given": "Yanlin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhao",
"given": "Weiguo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bao",
"given": "Pengtao",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8698-4746",
"affiliation": [],
"authenticated-orcid": true,
"family": "Li",
"given": "Diangeng",
"sequence": "additional"
}
],
"container-title": "Nature and Science of Sleep",
"container-title-short": "NSS",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
11,
12
]
],
"date-time": "2020-11-12T02:46:14Z",
"timestamp": 1605149174000
},
"deposited": {
"date-parts": [
[
2020,
11,
12
]
],
"date-time": "2020-11-12T02:46:24Z",
"timestamp": 1605149184000
},
"indexed": {
"date-parts": [
[
2022,
4,
29
]
],
"date-time": "2022-04-29T15:06:41Z",
"timestamp": 1651244801500
},
"is-referenced-by-count": 11,
"issued": {
"date-parts": [
[
2020,
11
]
]
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/3.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
11,
1
]
],
"date-time": "2020-11-01T00:00:00Z",
"timestamp": 1604188800000
}
}
],
"link": [
{
"URL": "https://www.dovepress.com/getfile.php?fileID=63655",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.dovepress.com/getfile.php?fileID=63655",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "999-1007",
"prefix": "10.2147",
"published": {
"date-parts": [
[
2020,
11
]
]
},
"published-online": {
"date-parts": [
[
2020,
11
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"key": "ref1",
"unstructured": "WHO. Available from: https://www.who.int. Accessed March 31, 2020."
},
{
"DOI": "10.2139/ssrn.3556660",
"author": "Fan",
"doi-asserted-by": "publisher",
"journal-title": "SSRN J",
"key": "ref2",
"year": "2020"
},
{
"DOI": "10.2139/ssrn.3562478",
"author": "Zhu",
"doi-asserted-by": "publisher",
"journal-title": "SSRN J",
"key": "ref3",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"journal-title": "Lancet",
"key": "ref4",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.3633",
"author": "Murthy",
"doi-asserted-by": "publisher",
"first-page": "1499",
"journal-title": "JAMA",
"key": "ref5",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30117-X",
"author": "Cai",
"doi-asserted-by": "publisher",
"first-page": "e20",
"journal-title": "Lancet Respir Med",
"key": "ref6",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1101/2020.01.26.919985",
"author": "Zhao",
"doi-asserted-by": "publisher",
"journal-title": "Bioinformatics",
"key": "ref7",
"year": "2020"
},
{
"DOI": "10.1080/02640414.2011.627371",
"author": "Gleeson",
"doi-asserted-by": "publisher",
"first-page": "321",
"journal-title": "J Sports Sci",
"key": "ref8",
"volume": "30",
"year": "2012"
},
{
"DOI": "10.1016/j.bbi.2005.04.002",
"author": "Lowder",
"doi-asserted-by": "publisher",
"first-page": "377",
"journal-title": "Brain Behav Immun",
"key": "ref9",
"volume": "19",
"year": "2005"
},
{
"DOI": "10.1097/JES.0b013e3181b7b57b",
"author": "Martin",
"doi-asserted-by": "publisher",
"first-page": "157",
"journal-title": "Exerc Sport Sci Rev",
"key": "ref10",
"volume": "37",
"year": "2009"
},
{
"DOI": "10.1155/2015/678164",
"author": "IIbarra-Coronado",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Immunol Res",
"key": "ref11",
"volume": "2015",
"year": "2015"
},
{
"DOI": "10.2807/1560-7917.ES.2020.25.3.2000045",
"author": "Corman",
"doi-asserted-by": "publisher",
"first-page": "3",
"journal-title": "Eurosurveillance",
"key": "ref12",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1513/AnnalsATS.201512-824OC",
"author": "Khair",
"doi-asserted-by": "publisher",
"first-page": "842",
"journal-title": "Ann Am Thorac Soc",
"key": "ref13",
"volume": "13",
"year": "2016"
},
{
"DOI": "10.4103/2311-8571.281609",
"doi-asserted-by": "crossref",
"key": "ref14",
"unstructured": "Diagnosis and treatment plan for COVID-19 (trial version 6). Chin Med J. 2020."
},
{
"DOI": "10.1183/13993003.00547-2020",
"author": "Guan",
"doi-asserted-by": "publisher",
"first-page": "2000547",
"journal-title": "Eur Respir J",
"key": "ref15",
"volume": "55",
"year": "2020"
},
{
"key": "ref16",
"unstructured": "US Department of Health and Human Services, & National Institutes of Health. Your Guide to Physical Activity and Your Heart (No. 06-5714). NIH Publication; 2006."
},
{
"DOI": "10.1136/bjsm.2008.052167",
"author": "Boon",
"doi-asserted-by": "publisher",
"first-page": "741",
"journal-title": "Br J Sports Med",
"key": "ref17",
"volume": "44",
"year": "2010"
},
{
"key": "ref18",
"unstructured": "IPAQ committee. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ). November, 2005. Available from: http://www.ipaq.ki.se/scoring.html. Accessed September 23, 2020."
},
{
"DOI": "10.1371/journal.pone.0151647",
"author": "Scholes",
"doi-asserted-by": "publisher",
"first-page": "e0151647",
"journal-title": "PLoS One",
"key": "ref19",
"volume": "11",
"year": "2016"
},
{
"key": "ref20",
"unstructured": "National Sleep Foundation. National sleep foundation recommends new sleep times. February 2, 2015. Available from: https://www.sleepfoundation.org/press-release/national-sleep-foundation-recommends-new-sleep-times. Accessed September 23, 2020."
},
{
"DOI": "10.1038/nri1369",
"author": "Bryant",
"doi-asserted-by": "publisher",
"first-page": "457",
"journal-title": "Nat Rev Immunol",
"key": "ref21",
"volume": "4",
"year": "2004"
},
{
"DOI": "10.2174/138161208786549281",
"author": "Krueger",
"doi-asserted-by": "publisher",
"first-page": "3408",
"journal-title": "CPD",
"key": "ref22",
"volume": "14",
"year": "2008"
},
{
"DOI": "10.1096/fasebj.10.5.8621064",
"author": "Irwin",
"doi-asserted-by": "publisher",
"first-page": "643",
"journal-title": "FASEB J",
"key": "ref23",
"volume": "10",
"year": "1996"
},
{
"DOI": "10.5665/sleep.1594",
"author": "Patel",
"doi-asserted-by": "publisher",
"first-page": "97",
"journal-title": "Sleep",
"key": "ref24",
"volume": "35",
"year": "2012"
},
{
"DOI": "10.1001/jamainternmed.2016.0787",
"author": "Prather",
"doi-asserted-by": "publisher",
"first-page": "850",
"journal-title": "JAMA Intern Med",
"key": "ref25",
"volume": "176",
"year": "2016"
}
],
"reference-count": 25,
"references-count": 25,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.dovepress.com/reduced-sleep-in-the-week-prior-to-diagnosis-of-covid-19-is-associated-peer-reviewed-article-NSS"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Behavioral Neuroscience",
"Applied Psychology"
],
"subtitle": [],
"title": "<p>Reduced Sleep in the Week Prior to Diagnosis of COVID-19 is Associated with the Severity of COVID-19</p>",
"type": "journal-article",
"volume": "Volume 12"
}
