Bile acids and coronavirus disease 2019
et al., Acta Pharmaceutica Sinica B, doi:10.1016/j.apsb.2024.02.011, Feb 2024
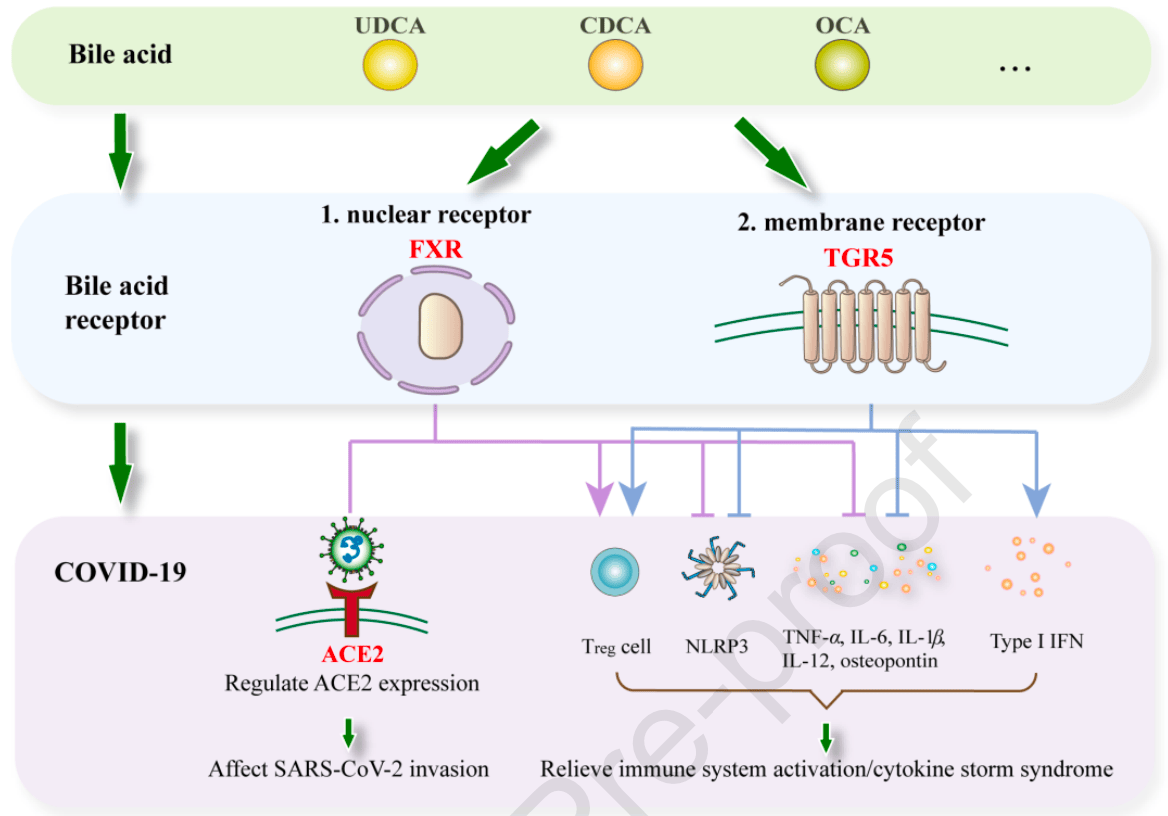
Review of the relationship between bile acids and COVID-19. Authors discuss emerging basic and clinical evidence linking bile acids to COVID-19 infection and potential mechanisms. Functionally, studies indicate that certain bile acids like ursodeoxycholic acid may protect against SARS-CoV-2 infection by modulating ACE2 expression or activity. Mechanistically, bile acids influence pathways involving immunomodulation, inflammation, and metabolism that likely contribute to COVID-19 pathogenesis. Bile acid receptors FXR and TGR5 in particular participate in regulating ACE2 as well as immune responses, making them potential therapeutic targets.
See Fiorucci et al. for another review covering ursodeoxycholic acid for COVID-19.
Huang et al., 13 Feb 2024, peer-reviewed, 3 authors.
Contact: lizijian@bjmu.edu.cn.
Bile acids and coronavirus disease 2019
Acta Pharmaceutica Sinica B, doi:10.1016/j.apsb.2024.02.011
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has been significantly alleviated. However, long-term health effects and prevention strategy remain unresolved. Thus, it is essential to explore the pathophysiological mechanisms and intervention for SARS-CoV-2 infection. Emerging research indicates a link between COVID-19 and bile acids, traditionally known for facilitating dietary fat absorption. The bile acid ursodeoxycholic acid potentially protects against SARS-CoV-2 infection by inhibiting the farnesoid X receptor, a bile acid nuclear receptor. The activation of G-protein-coupled bile acid receptor, another membrane receptor for bile acids, has also been found to regulate the expression of angiotensin-converting enzyme 2, the receptor through which the virus enters human cells. Here, we review the latest basic and clinical evidence linking bile acids to SARS-CoV-2, and reveal their complicated pathophysiological mechanisms.
Author contributions Xiaoru Huang and Xuening Liu contributed equally to this work. Xiaoru Huang and Xuening Liu drafted the manuscript; Xuening Liu prepared figures; Xiaoru Huang, Xuening Liu, and Zijian edited and revised the manuscript.
Conflicts of interest The authors declare no conflicts of interest.
References
Abdulrab, Al-Maweri, Halboub, Ursodeoxycholic acid as a candidate therapeutic to alleviate and/or prevent COVID-19-associated cytokine storm, Med Hypotheses
Ahmad, Haeusler, Bile acids in glucose metabolism and insulin signalling -mechanisms and research needs, Nat Rev Endocrinol
Albrich, Ghosh, Ahearn-Ford, Mikaeloff, Lunjani et al., A high-risk gut microbiota configuration associates with fatal hyperinflammatory immune and metabolic responses to SARS-CoV-2, Gut Microbes
Anderson, Gayer, The pathophysiology of farnesoid X receptor (FXR) in the GI tract: inflammation, barrier function and innate immunity, Cells
Ao, He, Liu, Xu, Strategies for the development and approval of COVID-19 vaccines and therapeutics in the post-pandemic period, Signal Transduct Target Ther
Atchison, Davies, Cooper, Lound, Whitaker et al., Long-term health impacts of COVID-19 among 242,712 adults in England, Nat Commun
Babalghith, Al-Kuraishy, Gareeb, Waard, Sm, The role of berberine in Covid-19: potential adjunct therapy, Inflammopharmacology
Batiha, Al-Kuraishy, Gareeb, Youssef, El-Sherbeni et al., A perspective study of the possible impact of obeticholic acid against SARS-CoV-2 infection, Inflammopharmacology
Bertolini, Fiorotto, Strazzabosco, Bile acids and their receptors: modulators and therapeutic targets in liver inflammation, Semin Immunopathol
Biagioli, Carino, Cipriani, Francisci, Marchianò et al., The bile acid receptor GPBAR1 regulates the M1/M2 phenotype of intestinal macrophages and activation of GPBAR1 rescues mice from murine colitis, J Immunol
Biagioli, Marchianò, Roselli, Giorgio, Bellini et al., GLP-1 mediates regulation of colonic ACE2 expression by the bile acid receptor GPBAR1 in inflammation, Cells
Bian, Li, Angiotensin-converting enzyme 2 (ACE2): SARS-CoV-2 receptor and RAS modulator, Acta Pharm Sin B
Bidault-Jourdainne, Merlen, Glénisson, Doignon, Garcin et al., TGR5 controls bile acid composition and gallbladder function to protect the liver from bile acid overload, JHEP Rep
Bramante, Buse, Tamaritz, Palacio, Cohen et al., Outpatient metformin use is associated with reduced severity of COVID-19 disease in adults with overweight or obesity, J Med Virol
Bramante, Huling, Tignanelli, Buse, Liebovitz et al., Randomized trial of metformin, ivermectin, and fluvoxamine for Covid-19, N Engl J Med
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis, Lancet Healthy Longev
Brevini, Maes, Webb, John, Fuchs et al., FXR inhibition may protect from SARS-CoV-2 infection by reducing ACE2, Nature
Cai, Sun, Gonzalez, Gut microbiota-derived bile acids in intestinal immunity, inflammation, and tumorigenesis, Cell Host Microbe
Campbell, Mckenney, Konstantinovsky, Isaeva, Schizas et al., Bacterial metabolism of bile acids promotes generation of peripheral regulatory T cells, Nature
Cao, Hu, Li, Wang, Xu et al., Anti-SARS-CoV-2 potential of artemisinins in vitro, ACS Infect Dis
Carino, Biagioli, Marchianò, Fiorucci, Zampella et al., Ursodeoxycholic acid is a GPBAR1 agonist and resets liver/intestinal FXR signaling in a model of diet-induced dysbiosis and NASH, Biochim Biophys Acta Mol Cell Biol Lipids
Carino, Moraca, Fiorillo, Marchianò, Sepe et al., Hijacking SARS-CoV-2/ACE2 receptor interaction by natural and semi-synthetic steroidal agents acting on functional pockets on the receptor binding domain, Front Chem
Cariou, Van Harmelen, Duran-Sandoval, Van Dijk, Grefhorst et al., The farnesoid X receptor modulates adiposity and peripheral insulin sensitivity in mice, J Biol Chem
Chen, Gu, Li, Sun, Metabolite reanalysis revealed potential biomarkers for COVID-19: a potential link with immune response, Future Microbiol
Cheng, Liu, Li, Zhang, Lei et al., Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and pre-existing type 2 diabetes, Cell Metab
Chiou, Chen, Chen, Yang, Hwang et al., The inhibitory effects of PGG and EGCG against the SARS-CoV-2 3C-like protease, Biochem Biophys Res Commun
Chourasia, Koppula, Battu, Ouseph, Singh, EGCG, a green tea catechin, as a potential therapeutic agent for symptomatic and asymptomatic SARS-CoV-2 infection, Molecules
Colapietro, Angelotti, Masetti, Shiffer, Pugliese et al., Ursodeoxycholic acid does not improve COVID-19 outcome in hospitalized patients, Viruses
De Aguiar Vallim, Tarling, Edwards, Pleiotropic roles of bile acids in metabolism, Cell Metab
Dejang, Mxu, Kwhite, A SARS-CoV-2 protein interaction map reveals targets for drug repurposing, Nature
Ding, Yang, Zhang, Wang, Sun et al., Notoginsenoside Ft1 acts as a TGR5 agonist but FXR antagonist to alleviate high fat diet-induced obesity and insulin resistance in mice, Acta Pharm Sin B
Duboc, Taché, Hofmann, The bile acid TGR5 membrane receptor: from basic research to clinical application, Dig Liver Dis
Eshraghian, Current and emerging pharmacological therapy for non-alcoholic fatty liver disease, World J Gastroenterol
Fiorillo, Marchianò, Moraca, Sepe, Carino et al., Discovery of bile acid derivatives as potent ACE2 activators by virtual screening and essential dynamics, J Chem Inf Model
Fiorucci, Biagioli, Zampella, Distrutti, Bile acids activated receptors regulate innate immunity, Front Immunol
Forman, Goode, Chen, Oro, Bradley et al., Identification of a nuclear receptor that is activated by farnesol metabolites, Cell
Gonzalez, Jiang, Patterson, An intestinal microbiota-farnesoid X receptor axis modulates metabolic disease, Gastroenterology
Goodwin, Gauthier, Umetani, Watson, Lochansky et al., Identification of bile acid precursors as endogenous ligands for the nuclear xenobiotic pregnane X receptor, Proc Natl Acad Sci U S A
Guo, Peng, Hao, Ji, Zhang et al., Dihydroartemisinin promoted FXR expression independent of YAP1 in hepatocellular carcinoma, FASEB J
Guo, Xie, Chi, Zhang, Liu et al., Bile acids control inflammation and metabolic disorder through inhibition of NLRP3 inflammasome, Immunity
Guzior, Quinn, Review: microbial transformations of human bile acids, Microbiome
Han, Studer, Gupta, Fang, Qiao et al., Bile acids enhance the activity of the insulin receptor and glycogen synthase in primary rodent hepatocytes, Hepatology
Henss, Auste, Schürmann, Schmidt, Von Rhein et al., The green tea catechin epigallocatechin gallate inhibits SARS-CoV-2 infection, J Gen Virol
Heuman, Quantitative estimation of the hydrophilic-hydrophobic balance of mixed bile salt solutions, J Lipid Res
Hofmann, Hagey, Krasowski, Bile salts of vertebrates: structural variation and possible evolutionary significance, J Lipid Res
Hu, He, Gao, Yang, He et al., Virus-induced accumulation of intracellular bile acids activates the TGR5-beta-arrestin-SRC axis to enable innate antiviral immunity, Cell Res
Hu, Wang, Huang, Yi, Pan et al., Gut microbiota-mediated secondary bile acids regulate dendritic cells to attenuate autoimmune uveitis through TGR5 signaling, Cell Rep
Hunyady, Streller, Rüther, Groba, Bettinger et al., Secondary sclerosing cholangitis following coronavirus disease 2019 (COVID-19): a multicenter retrospective study, Clin Infect Dis
Hylemon, Zhou, Pandak, Ren, Gil et al., Bile acids as regulatory molecules, J Lipid Res
J O U R N A L P R E, None
J O U R N A L P R E, None
J O U R N A L P R E, r o o f 56
J O U R N A L P R E, r o o f 67
J O U R N A L P R E, r o o f 78
J O U R N A L P R E, r o o f 89
Jang, Park, Park, Cha, Yamamoto et al., EGCG, a green tea polyphenol, inhibits human coronavirus replication in vitro, Biochem Biophys Res Commun
Ji, Meng, Zhu, He, Cui, Research and development of Chinese anti-COVID-19 drugs, Acta Pharm Sin B
Jia, Wei, Rajani, Zheng, Targeting the alternative bile acid synthetic pathway for metabolic diseases, Protein Cell
John, Bastaich, Webb, Brevini, Moon et al., Ursodeoxycholic acid is associated with a reduction in SARS-CoV-2 infection and reduced severity of COVID-19 in patients with cirrhosis, J Intern Med
Jothimani, Venugopal, Abedin, Kaliamoorthy, Rela, COVID-19 and the liver, J Hepatol
Junqueira, Crespo, Ranjbar, De Lacerda, Lewandrowski et al., FcγR-mediated SARS-CoV-2 infection of monocytes activates inflammation, Nature
Kawamata, Fujii, Hosoya, Harada, Yoshida et al., A G protein-coupled receptor responsive to bile acids, J Biol Chem
Keitel, Cupisti, Ullmer, Knoefel, Kubitz et al., The membrane-bound bile acid receptor TGR5 is localized in the epithelium of human gallbladders, Hepatology
Keitel, Reinehr, Gatsios, Rupprecht, Görg et al., The Gprotein coupled bile salt receptor TGR5 is expressed in liver sinusoidal endothelial cells, Hepatology
Khunti, Knighton, Zaccardi, Bakhai, Barron et al., Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people J o u r n a l P r e -p r o o f with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol
Lasalle, Hoguet, Hennuyer, Leroux, Piveteau et al., Topical intestinal aminoimidazole agonists of G-protein-coupled bile acid receptor 1 promote glucagon like peptide-1 secretion and improve glucose tolerance, J Med Chem
Lefebvre, Cariou, Kuipers, Staels, Role of bile acids and bile acid receptors in metabolic regulation, Physiol Rev
Lew, Zhao, Yu, Huang, Pedro et al., The farnesoid X receptor controls gene expression in a ligand-and promoter-selective fashion, J Biol Chem
Li, Lin, Araya, Chen, Timmermann et al., A tea catechin, epigallocatechin-3-gallate, is a unique modulator of the farnesoid X receptor, Toxicol Appl Pharmacol
Li, Zhu, Cui, Lin, Li, Protective effect of ursodeoxycholic acid on COVID-19 in patients with chronic liver disease, Front Cell Infect Microbiol
Liu, Bodnar, Meng, Khan, Wang et al., Epigallocatechin gallate from green tea effectively blocks infection of SARS-CoV-2 and new variants by inhibiting spike binding to ACE2 receptor, Cell Biosci
Liu, Wang, Ursodeoxycholic acid administration did not reduce susceptibility to SARS-CoV-2 infection in children, Liver Int
Ma, Hu, Wang, Choza, Wang, Drug-repurposing screening identified tropifexor as a SARS-CoV-2 papain-like Protease inhibitor, ACS Infect Dis
Ma, Luo, Deng, Yang, Wang et al., Antibiotic-induced primary biles inhibit SARS-CoV-2 endoribonuclease Nsp15 activity in mouse gut, Front Cell Infect Microbiol
Maio, Cherry, Schultz, Hurst, Linehan et al., TEMPOL inhibits SARS-CoV-2 replication and development of lung disease in the Syrian hamster model, iScience
Maio, Lafont, Sil, Li, Bollinger et al., Fe-S cofactors in the SARS-CoV-2 RNA-dependent RNA polymerase are potential antiviral targets, Science
Makishima, Lu, Xie, Whitfield, Domoto et al., Vitamin D receptor as an intestinal bile acid sensor, Science
Makishima, Okamoto, Repa, Tu, Learned et al., Identification of a nuclear receptor for bile acids, Science
Marrone, Covino, Merra, Piccioni, Amodeo et al., Ursodeoxycholic acid does not affect the clinical outcome of SARS-CoV-2 infection: a retrospective study of propensity score-matched cohorts, Liver Int
Martin, Dumas, Wang, Legido-Quigley, Yap et al., A topdown systems biology view of microbiome-mammalian metabolic interactions in a mouse model, Mol Syst Biol
Maruyama, Miyamoto, Nakamura, Tamai, Okada et al., Identification of membrane-type receptor for bile acids (M-BAR), Biochem Biophys Res Commun
Mathi, Rosenberg-Hasson, Maecker, Carlo, Moss, Brief report: Tempol, a novel antioxidant, inhibits both activated T cell and antigen presenting cell derived cytokines in-vitro from COVID-19 patients, Clin Immunol
Matsubara, Li, Gonzalez, FXR signaling in the enterohepatic system, Mol Cell Endocrinol
Mencarelli, Renga, Migliorati, Cipriani, Distrutti et al., The bile acid sensor farnesoid X receptor is a modulator of liver immunity in a rodent model of acute hepatitis, J Immunol
Meyer, Chiaravalli, Gellenoncourt, Brownridge, Bryne et al., Characterising proteolysis during SARS-CoV-2 infection identifies viral cleavage sites and cellular targets with therapeutic potential, Nat Commun
Nguyen, Ho, Nguyen, Ho, Li et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: a meta-analysis, Metabolism
Ni, Chen, Wei, Lan, Qiu et al., Study on the mechanism of active components of Liupao tea on 3CL(pro) based on HPLC-DAD fingerprint and molecular docking technique, J Food Biochem
Otte, Kranz, Kober, Thompson, Hoefer et al., Identification of farnesoid X receptor beta as a novel mammalian nuclear receptor sensing lanosterol, Mol Cell Biol
Pan, Shen, Yu, Ge, Chen et al., SARS-CoV-2 N protein promotes NLRP3 inflammasome activation to induce hyperinflammation, Nat Commun
Pang, Feng, Commentary: Can FXR serve as a potential target for COVID-19 prevention?, Acta Pharm Sin B
Parks, Blanchard, Bledsoe, Chandra, Consler et al., Bile acids: natural ligands for an orphan nuclear receptor, Science
Parthasarathy, Tandel, Siddiqui, Harshan, Metformin suppresses SARS-CoV-2 in cell culture, Virus Res
Perino, Demagny, Velazquez-Villegas, Schoonjans, Molecular physiology of bile acid signaling in health, disease, and aging, Physiol Rev
Perino, Pols, Nomura, Stein, Pellicciari et al., TGR5 reduces macrophage migration through mTOR-induced C/EBPβ differential translation, J Clin Invest
Pizzorno, Padey, Dubois, Julien, Traversier et al., In vitro evaluation of antiviral activity of single and combined repurposable drugs against SARS-CoV-2, Antiviral Res
Poole, Godfrey, Cattaruzza, Cottrell, Kirkland et al., Expression and function of the bile acid receptor GpBAR1 (TGR5) in the murine enteric nervous system, Neurogastroenterol Motil
Reich, Deutschmann, Sommerfeld, Klindt, Kluge et al., TGR5 is essential for bile acid-dependent cholangiocyte proliferation in vivo and in vitro, Gut
Reich, Spomer, Klindt, Fuchs, Stindt et al., Downregulation of TGR5 (GPBAR1) in biliary epithelial cells contributes to the pathogenesis of sclerosing cholangitis, J Hepatol
Russell, The enzymes, regulation, and genetics of bile acid synthesis, Annu Rev Biochem
Salim, Phillips, Farthing, Pathogenesis of gut virus infection, Baillieres Clin Gastroenterol
Schaap, Trauner, Jansen, Bile acid receptors as targets for drug development, Nat Rev Gastroenterol Hepatol
Schaller, Sharma, Dupee, Nguyen, Urueña et al., Ex vivo SARS-CoV-2 infection of human lung reveals heterogeneous host defense and therapeutic responses, JCI Insight
Schote, Turner, Schiltz, Muller, Nuclear receptors in human immune cells: expression and correlations, Mol Immunol
Seth, Sun, Chen, Antiviral innate immunity pathways, Cell Research
Shen, Yi, Sun, Bi, Du et al., Proteomic and metabolomic characterization of COVID-19 patient sera, Cell
Shi, Su, Zhang, Shi, Zhou et al., TGR5 regulates macrophage inflammation in nonalcoholic steatohepatitis by modulating NLRP3 inflammasome activation, Front Immunol
Shin, Mukherjee, Grewe, Bojkova, Baek et al., Papainlike protease regulates SARS-CoV-2 viral spread and innate immunity, Nature
Shu, Li, Cao, Li, Zhou et al., Berberine alleviates non-alcoholic steatohepatitis through modulating gut microbiota mediated intestinal FXR activation, Front Pharmacol
Simoes E Silva, Silveira, Ferreira, Teixeira, ACE2, angiotensin-(1-7) and Mas receptor axis in inflammation and fibrosis, Br J Pharmacol
Singh, Khera, Allen, Murad, Loomba, Comparative effectiveness of pharmacological interventions for nonalcoholic steatohepatitis: A systematic review and network meta-analysis, Hepatology
Smyth, Truong, Rao, Lin, Foulke-Abel et al., Farnesoid X receptor enhances epithelial ACE2 expression and inhibits virally induced IL-6 secretion: implications for intestinal symptoms of SARS-CoV-2, Am J Physiol Gastrointest Liver Physiol
Sokol, Contreras, Maisonnasse, Desmons, Delache et al., SARS-CoV-2 infection in nonhuman primates alters the composition and functional activity of the gut microbiota, Gut Microbes
Song, Rockwell, Cui, Klaassen, Individual bile acids have differential effects on bile acid signaling in mice, Toxicol Appl Pharmacol
Stutz, Dylla, Pearson, Lecompte-Osorio, Nayak et al., Immunomodulatory fecal metabolites are associated with mortality in COVID-19 patients with respiratory failure, Nat Commun
Sun, Xie, Wang, Wu, Wu et al., Gut microbiota and intestinal FXR mediate the clinical benefits of metformin, Nat Med
Sánchez, Bile acid-microbiota crosstalk in gastrointestinal inflammation and carcinogenesis: a role for bifidobacteria and lactobacilli?, Nat Rev Gastroenterol Hepatol
Tanoue, Atarashi, Honda, Development and maintenance of intestinal regulatory T cells, Nat Rev Immunol
Thomas, Gioiello, Noriega, Strehle, Oury et al., TGR5mediated bile acid sensing controls glucose homeostasis, Cell Metab
Thomas, Pellicciari, Pruzanski, Auwerx, Schoonjans, Targeting bileacid signalling for metabolic diseases, Nat Rev Drug Discov
Thuy, Bao, Moon, Ursodeoxycholic acid ameliorates cell migration retarded by the SARS-CoV-2 spike protein in BEAS-2B human bronchial epithelial cells, Biomed Pharmacother
Urizar, Liverman, Dodds, Silva, Ordentlich et al., A natural product that lowers cholesterol as an antagonist ligand for FXR, Science
Varghese, Van Woudenbergh, Overheul, Eleveld, Kurver et al., Berberine and obatoclax inhibit SARS-Cov-2 replication in primary human nasal epithelial cells in vitro, Viruses
Vassileva, Golovko, Markowitz, Abbondanzo, Zeng et al., Targeted deletion of Gpbar1 protects mice from cholesterol gallstone formation, Biochem J
Wang, Chen, Hollister, Sowers, Forman, Endogenous bile acids are ligands for the nuclear receptor FXR/BAR, Mol Cell
Wang, Chen, Moore, Huang, FXR: a metabolic regulator and cell protector, Cell Res
Wang, Chen, Yu, Forman, Huang, The G-protein-coupled bile acid receptor, Gpbar1 (TGR5), negatively regulates hepatic inflammatory response through antagonizing nuclear factor κ light-chain enhancer of activated B cells (NF-κB) in mice, Hepatology
Wang, Li, Maskey, Huang, Toutov et al., A small molecule compound berberine as an orally active therapeutic candidate against COVID-19 and SARS: a computational and mechanistic study, FASEB J
Wang, Qiao, Li, New insights into modes of GPCR activation, Trends Pharmacol Sci
Wang, Wu, Chapter 55-Ursodeoxycholic acid for the treatment of liver diseases
Wang, Yan, Li, Gong, Mai et al., Clinical and antibody characteristics reveal diverse signatures of severe and non-severe SARS-CoV-2 patients, Infect Dis Poverty
Watanabe, Houten, Mataki, Christoffolete, Kim et al., Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation, Nature
Watanabe, Houten, Wang, Moschetta, Mangelsdorf et al., Bile acids lower triglyceride levels via a pathway involving FXR, SHP, and SREBP-1c, J Clin Invest
Xian, Liu, Nilsson, Gatchalian, Crother et al., Metformin inhibition of mitochondrial ATP and DNA synthesis abrogates NLRP3 inflammasome activation and pulmonary inflammation, Immunity
Xiong, Huang, Wang, Chen, Chen et al., Metabolite-sensing G protein coupled receptor TGR5 protects host from viral infection through amplifying type I interferon responses, Front Immunol
Xu, Huang, Gong, Zhou, Zhao et al., FXR ligands protect against hepatocellular inflammation via SOCS3 induction, Cell Signal
Xu, Yuan, Chen, Xiong, Zhang et al., Carboxylic submetabolome-driven signature characterization of COVID-19 asymptomatic infection, Talanta
Yan, Yan, Xia, Hao, Wang et al., The pathophysiological function of non-gastrointestinal farnesoid X receptor, Pharmacol Ther
Zhang, Chen, Chen, Cao, You et al., Berberine reduces circulating inflammatory mediators in patients with severe COVID-19, Br J Surg
Zhang, Hao, Zhang, He, Chen et al., Potential of green tea EGCG in neutralizing SARS-CoV-2 Omicron variant with greater tropism toward the upper respiratory tract, Trends Food Sci Technol
Zhang, Huang, Qatanani, Evans, Moore, The constitutive androstane receptor and pregnane X receptor function coordinately to prevent bile acidinduced hepatotoxicity, J Biol Chem
Zhang, Kast-Woelbern, Edwards, Natural structural variants of the nuclear receptor farnesoid X receptor affect transcriptional activation, J Biol Chem
Zhang, Lau, Liu, Su, Chan et al., Gut microbiota in COVID-19: key microbial changes, potential mechanisms and clinical applications, Nat Rev Gastroenterol Hepatol
Zhang, Yu, Zhang, Wang, Zhao et al., Mechanism of SARS-CoV-2 Invasion into the Liver and Hepatic Injury in Patients with COVID-19, Mediterr J Hematol Infect Dis
Zhang, Zhang, Bi, He, Yang, Potential protective mechanisms of green tea polyphenol EGCG against COVID-19, Trends Food Sci Technol
Zhao, Ni, Gao, Wang, Yang et al., Recapitulation of SARS-CoV-2 infection and cholangiocyte damage with human liver ductal organoids, Protein Cell
Zhou, Cao, Jiang, Xie, Cheng et al., PPARα-UGT axis activation represses intestinal FXR-FGF15 feedback signalling and exacerbates experimental colitis, Nat Commun
DOI record:
{
"DOI": "10.1016/j.apsb.2024.02.011",
"ISSN": [
"2211-3835"
],
"URL": "http://dx.doi.org/10.1016/j.apsb.2024.02.011",
"alternative-id": [
"S2211383524000492"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Bile acids and coronavirus disease 2019"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Acta Pharmaceutica Sinica B"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.apsb.2024.02.011"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2024 Published by Elsevier B.V. on behalf of Chinese Pharmaceutical Association and Institute of Materia Medica, Chinese Academy of Medical Sciences."
}
],
"author": [
{
"affiliation": [],
"family": "Huang",
"given": "Xiaoru",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0009-0007-3969-3093",
"affiliation": [],
"authenticated-orcid": false,
"family": "Liu",
"given": "Xuening",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8057-2257",
"affiliation": [],
"authenticated-orcid": false,
"family": "Li",
"given": "Zijian",
"sequence": "additional"
}
],
"container-title": "Acta Pharmaceutica Sinica B",
"container-title-short": "Acta Pharmaceutica Sinica B",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2024,
2,
13
]
],
"date-time": "2024-02-13T05:41:01Z",
"timestamp": 1707802861000
},
"deposited": {
"date-parts": [
[
2024,
2,
13
]
],
"date-time": "2024-02-13T05:42:36Z",
"timestamp": 1707802956000
},
"indexed": {
"date-parts": [
[
2024,
2,
14
]
],
"date-time": "2024-02-14T01:18:26Z",
"timestamp": 1707873506058
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
2
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
2,
1
]
],
"date-time": "2024-02-01T00:00:00Z",
"timestamp": 1706745600000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 9,
"start": {
"date-parts": [
[
2024,
2,
10
]
],
"date-time": "2024-02-10T00:00:00Z",
"timestamp": 1707523200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2211383524000492?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2211383524000492?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"prefix": "10.1016",
"published": {
"date-parts": [
[
2024,
2
]
]
},
"published-print": {
"date-parts": [
[
2024,
2
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/j.apsb.2020.10.006",
"article-title": "Angiotensin-converting enzyme 2 (ACE2): SARS-CoV-2 receptor and RAS modulator",
"author": "Bian",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Acta Pharm Sin B",
"key": "10.1016/j.apsb.2024.02.011_bib1",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1038/s41467-023-41879-2",
"article-title": "Long-term health impacts of COVID-19 among 242,712 adults in England",
"author": "Atchison",
"doi-asserted-by": "crossref",
"first-page": "6588",
"journal-title": "Nat Commun",
"key": "10.1016/j.apsb.2024.02.011_bib2",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1038/s41392-023-01724-w",
"article-title": "Strategies for the development and approval of COVID-19 vaccines and therapeutics in the post-pandemic period",
"author": "Ao",
"doi-asserted-by": "crossref",
"first-page": "466",
"journal-title": "Signal Transduct Target Ther",
"key": "10.1016/j.apsb.2024.02.011_bib3",
"volume": "8",
"year": "2023"
},
{
"DOI": "10.1038/s41586-022-05594-0",
"article-title": "FXR inhibition may protect from SARS-CoV-2 infection by reducing ACE2",
"author": "Brevini",
"doi-asserted-by": "crossref",
"first-page": "134",
"journal-title": "Nature",
"key": "10.1016/j.apsb.2024.02.011_bib4",
"volume": "615",
"year": "2023"
},
{
"DOI": "10.3390/cells11071187",
"article-title": "GLP-1 mediates regulation of colonic ACE2 expression by the bile acid receptor GPBAR1 in inflammation",
"author": "Biagioli",
"doi-asserted-by": "crossref",
"first-page": "1187",
"journal-title": "Cells",
"key": "10.1016/j.apsb.2024.02.011_bib5",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1007/s00281-022-00935-7",
"article-title": "Bile acids and their receptors: modulators and therapeutic targets in liver inflammation",
"author": "Bertolini",
"doi-asserted-by": "crossref",
"first-page": "547",
"journal-title": "Semin Immunopathol",
"key": "10.1016/j.apsb.2024.02.011_bib6",
"volume": "44",
"year": "2022"
},
{
"DOI": "10.1016/j.chom.2022.02.004",
"article-title": "Gut microbiota-derived bile acids in intestinal immunity, inflammation, and tumorigenesis",
"author": "Cai",
"doi-asserted-by": "crossref",
"first-page": "289",
"journal-title": "Cell Host Microbe",
"key": "10.1016/j.apsb.2024.02.011_bib7",
"volume": "30",
"year": "2022"
},
{
"DOI": "10.2217/fmb-2021-0047",
"article-title": "Metabolite reanalysis revealed potential biomarkers for COVID-19: a potential link with immune response",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "577",
"journal-title": "Future Microbiol",
"key": "10.1016/j.apsb.2024.02.011_bib8",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1007/s10787-022-01111-x",
"article-title": "A perspective study of the possible impact of obeticholic acid against SARS-CoV-2 infection",
"author": "Batiha",
"doi-asserted-by": "crossref",
"first-page": "9",
"journal-title": "Inflammopharmacology",
"key": "10.1016/j.apsb.2024.02.011_bib9",
"volume": "31",
"year": "2023"
},
{
"DOI": "10.1146/annurev.biochem.72.121801.161712",
"article-title": "The enzymes, regulation, and genetics of bile acid synthesis",
"author": "Russell",
"doi-asserted-by": "crossref",
"first-page": "137",
"journal-title": "Annu Rev Biochem",
"key": "10.1016/j.apsb.2024.02.011_bib10",
"volume": "72",
"year": "2003"
},
{
"DOI": "10.1007/s13238-020-00804-9",
"article-title": "Targeting the alternative bile acid synthetic pathway for metabolic diseases",
"author": "Jia",
"doi-asserted-by": "crossref",
"first-page": "411",
"journal-title": "Protein Cell",
"key": "10.1016/j.apsb.2024.02.011_bib11",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1194/jlr.R000042",
"article-title": "Bile salts of vertebrates: structural variation and possible evolutionary significance",
"author": "Hofmann",
"doi-asserted-by": "crossref",
"first-page": "226",
"journal-title": "J Lipid Res",
"key": "10.1016/j.apsb.2024.02.011_bib12",
"volume": "51",
"year": "2010"
},
{
"DOI": "10.1186/s40168-021-01101-1",
"article-title": "Review: microbial transformations of human bile acids",
"author": "Guzior",
"doi-asserted-by": "crossref",
"first-page": "140",
"journal-title": "Microbiome",
"key": "10.1016/j.apsb.2024.02.011_bib13",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1038/msb4100153",
"article-title": "A top-down systems biology view of microbiome-mammalian metabolic interactions in a mouse model",
"author": "Martin",
"doi-asserted-by": "crossref",
"first-page": "112",
"journal-title": "Mol Syst Biol",
"key": "10.1016/j.apsb.2024.02.011_bib14",
"volume": "3",
"year": "2007"
},
{
"DOI": "10.1126/science.284.5418.1362",
"article-title": "Identification of a nuclear receptor for bile acids",
"author": "Makishima",
"doi-asserted-by": "crossref",
"first-page": "1362",
"journal-title": "Science",
"key": "10.1016/j.apsb.2024.02.011_bib15",
"volume": "284",
"year": "1999"
},
{
"DOI": "10.1126/science.284.5418.1365",
"article-title": "Bile acids: natural ligands for an orphan nuclear receptor",
"author": "Parks",
"doi-asserted-by": "crossref",
"first-page": "1365",
"journal-title": "Science",
"key": "10.1016/j.apsb.2024.02.011_bib16",
"volume": "284",
"year": "1999"
},
{
"DOI": "10.1016/S1097-2765(00)80348-2",
"article-title": "Endogenous bile acids are ligands for the nuclear receptor FXR/BAR",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "543",
"journal-title": "Mol Cell",
"key": "10.1016/j.apsb.2024.02.011_bib17",
"volume": "3",
"year": "1999"
},
{
"DOI": "10.1073/pnas.0237082100",
"article-title": "Identification of bile acid precursors as endogenous ligands for the nuclear xenobiotic pregnane X receptor",
"author": "Goodwin",
"doi-asserted-by": "crossref",
"first-page": "223",
"journal-title": "Proc Natl Acad Sci U S A",
"key": "10.1016/j.apsb.2024.02.011_bib18",
"volume": "100",
"year": "2003"
},
{
"DOI": "10.1126/science.1070477",
"article-title": "Vitamin D receptor as an intestinal bile acid sensor",
"author": "Makishima",
"doi-asserted-by": "crossref",
"first-page": "1313",
"journal-title": "Science",
"key": "10.1016/j.apsb.2024.02.011_bib19",
"volume": "296",
"year": "2002"
},
{
"DOI": "10.1074/jbc.M409041200",
"article-title": "The constitutive androstane receptor and pregnane X receptor function coordinately to prevent bile acid-induced hepatotoxicity",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "49517",
"journal-title": "J Biol Chem",
"key": "10.1016/j.apsb.2024.02.011_bib20",
"volume": "279",
"year": "2004"
},
{
"DOI": "10.1074/jbc.M209706200",
"article-title": "A G protein-coupled receptor responsive to bile acids",
"author": "Kawamata",
"doi-asserted-by": "crossref",
"first-page": "9435",
"journal-title": "J Biol Chem",
"key": "10.1016/j.apsb.2024.02.011_bib21",
"volume": "278",
"year": "2003"
},
{
"DOI": "10.1038/nrgastro.2013.151",
"article-title": "Bile acid receptors as targets for drug development",
"author": "Schaap",
"doi-asserted-by": "crossref",
"first-page": "55",
"journal-title": "Nat Rev Gastroenterol Hepatol",
"key": "10.1016/j.apsb.2024.02.011_bib22",
"volume": "11",
"year": "2014"
},
{
"DOI": "10.1016/S0022-2275(20)38331-0",
"article-title": "Quantitative estimation of the hydrophilic-hydrophobic balance of mixed bile salt solutions",
"author": "Heuman",
"doi-asserted-by": "crossref",
"first-page": "719",
"journal-title": "J Lipid Res",
"key": "10.1016/j.apsb.2024.02.011_bib23",
"volume": "30",
"year": "1989"
},
{
"DOI": "10.1016/j.cmet.2013.03.013",
"article-title": "Pleiotropic roles of bile acids in metabolism",
"author": "de Aguiar Vallim",
"doi-asserted-by": "crossref",
"first-page": "657",
"journal-title": "Cell Metab",
"key": "10.1016/j.apsb.2024.02.011_bib24",
"volume": "17",
"year": "2013"
},
{
"DOI": "10.1152/physrev.00010.2008",
"article-title": "Role of bile acids and bile acid receptors in metabolic regulation",
"author": "Lefebvre",
"doi-asserted-by": "crossref",
"first-page": "147",
"journal-title": "Physiol Rev",
"key": "10.1016/j.apsb.2024.02.011_bib25",
"volume": "89",
"year": "2009"
},
{
"DOI": "10.1038/nrd2619",
"article-title": "Targeting bile-acid signalling for metabolic diseases",
"author": "Thomas",
"doi-asserted-by": "crossref",
"first-page": "678",
"journal-title": "Nat Rev Drug Discov",
"key": "10.1016/j.apsb.2024.02.011_bib26",
"volume": "7",
"year": "2008"
},
{
"DOI": "10.1194/jlr.R900007-JLR200",
"article-title": "Bile acids as regulatory molecules",
"author": "Hylemon",
"doi-asserted-by": "crossref",
"first-page": "1509",
"journal-title": "J Lipid Res",
"key": "10.1016/j.apsb.2024.02.011_bib27",
"volume": "50",
"year": "2009"
},
{
"DOI": "10.1016/0092-8674(95)90530-8",
"article-title": "Identification of a nuclear receptor that is activated by farnesol metabolites",
"author": "Forman",
"doi-asserted-by": "crossref",
"first-page": "687",
"journal-title": "Cell",
"key": "10.1016/j.apsb.2024.02.011_bib28",
"volume": "81",
"year": "1995"
},
{
"DOI": "10.1016/j.molimm.2006.04.021",
"article-title": "Nuclear receptors in human immune cells: expression and correlations",
"author": "Schote",
"doi-asserted-by": "crossref",
"first-page": "1436",
"journal-title": "Mol Immunol",
"key": "10.1016/j.apsb.2024.02.011_bib29",
"volume": "44",
"year": "2007"
},
{
"DOI": "10.1016/j.pharmthera.2021.107867",
"article-title": "The pathophysiological function of non-gastrointestinal farnesoid X receptor",
"author": "Yan",
"doi-asserted-by": "crossref",
"journal-title": "Pharmacol Ther",
"key": "10.1016/j.apsb.2024.02.011_bib30",
"volume": "226",
"year": "2021"
},
{
"DOI": "10.1074/jbc.M209505200",
"article-title": "Natural structural variants of the nuclear receptor farnesoid X receptor affect transcriptional activation",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "104",
"journal-title": "J Biol Chem",
"key": "10.1016/j.apsb.2024.02.011_bib31",
"volume": "278",
"year": "2003"
},
{
"DOI": "10.1128/MCB.23.3.864-872.2003",
"article-title": "Identification of farnesoid X receptor beta as a novel mammalian nuclear receptor sensing lanosterol",
"author": "Otte",
"doi-asserted-by": "crossref",
"first-page": "864",
"journal-title": "Mol Cell Biol",
"key": "10.1016/j.apsb.2024.02.011_bib32",
"volume": "23",
"year": "2003"
},
{
"DOI": "10.1038/nrgastro.2018.23",
"article-title": "Bile acid-microbiota crosstalk in gastrointestinal inflammation and carcinogenesis: a role for bifidobacteria and lactobacilli?",
"author": "Sánchez",
"doi-asserted-by": "crossref",
"first-page": "205",
"journal-title": "Nat Rev Gastroenterol Hepatol",
"key": "10.1016/j.apsb.2024.02.011_bib33",
"volume": "15",
"year": "2018"
},
{
"DOI": "10.1016/j.taap.2014.12.005",
"article-title": "Individual bile acids have differential effects on bile acid signaling in mice",
"author": "Song",
"doi-asserted-by": "crossref",
"first-page": "57",
"journal-title": "Toxicol Appl Pharmacol",
"key": "10.1016/j.apsb.2024.02.011_bib34",
"volume": "283",
"year": "2015"
},
{
"DOI": "10.1038/s41591-018-0222-4",
"article-title": "Gut microbiota and intestinal FXR mediate the clinical benefits of metformin",
"author": "Sun",
"doi-asserted-by": "crossref",
"first-page": "1919",
"journal-title": "Nat Med",
"key": "10.1016/j.apsb.2024.02.011_bib35",
"volume": "24",
"year": "2018"
},
{
"DOI": "10.1074/jbc.M306422200",
"article-title": "The farnesoid X receptor controls gene expression in a ligand- and promoter-selective fashion",
"author": "Lew",
"doi-asserted-by": "crossref",
"first-page": "8856",
"journal-title": "J Biol Chem",
"key": "10.1016/j.apsb.2024.02.011_bib36",
"volume": "279",
"year": "2004"
},
{
"DOI": "10.1038/cr.2008.289",
"article-title": "FXR: a metabolic regulator and cell protector",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1087",
"journal-title": "Cell Res",
"key": "10.1016/j.apsb.2024.02.011_bib37",
"volume": "18",
"year": "2008"
},
{
"DOI": "10.1016/j.mce.2012.05.004",
"article-title": "FXR signaling in the enterohepatic system",
"author": "Matsubara",
"doi-asserted-by": "crossref",
"first-page": "17",
"journal-title": "Mol Cell Endocrinol",
"key": "10.1016/j.apsb.2024.02.011_bib38",
"volume": "368",
"year": "2013"
},
{
"DOI": "10.1172/JCI21025",
"article-title": "Bile acids lower triglyceride levels via a pathway involving FXR, SHP, and SREBP-1c",
"author": "Watanabe",
"doi-asserted-by": "crossref",
"first-page": "1408",
"journal-title": "J Clin Invest",
"key": "10.1016/j.apsb.2024.02.011_bib39",
"volume": "113",
"year": "2004"
},
{
"DOI": "10.1002/hep.20043",
"article-title": "Bile acids enhance the activity of the insulin receptor and glycogen synthase in primary rodent hepatocytes",
"author": "Han",
"doi-asserted-by": "crossref",
"first-page": "456",
"journal-title": "Hepatology",
"key": "10.1016/j.apsb.2024.02.011_bib40",
"volume": "39",
"year": "2004"
},
{
"DOI": "10.1074/jbc.M510258200",
"article-title": "The farnesoid X receptor modulates adiposity and peripheral insulin sensitivity in mice",
"author": "Cariou",
"doi-asserted-by": "crossref",
"first-page": "11039",
"journal-title": "J Biol Chem",
"key": "10.1016/j.apsb.2024.02.011_bib41",
"volume": "281",
"year": "2006"
},
{
"DOI": "10.1038/s41574-019-0266-7",
"article-title": "Bile acids in glucose metabolism and insulin signalling - mechanisms and research needs",
"author": "Ahmad",
"doi-asserted-by": "crossref",
"first-page": "701",
"journal-title": "Nat Rev Endocrinol",
"key": "10.1016/j.apsb.2024.02.011_bib42",
"volume": "15",
"year": "2019"
},
{
"DOI": "10.1016/S0006-291X(02)02550-0",
"article-title": "Identification of membrane-type receptor for bile acids (M-BAR)",
"author": "Maruyama",
"doi-asserted-by": "crossref",
"first-page": "714",
"journal-title": "Biochem Biophys Res Commun",
"key": "10.1016/j.apsb.2024.02.011_bib43",
"volume": "298",
"year": "2002"
},
{
"DOI": "10.1002/hep.23032",
"article-title": "The membrane-bound bile acid receptor TGR5 is localized in the epithelium of human gallbladders",
"author": "Keitel",
"doi-asserted-by": "crossref",
"first-page": "861",
"journal-title": "Hepatology",
"key": "10.1016/j.apsb.2024.02.011_bib44",
"volume": "50",
"year": "2009"
},
{
"article-title": "Expression and function of the bile acid receptor GpBAR1 (TGR5) in the murine enteric nervous system",
"author": "Poole",
"first-page": "e227",
"issue": "814-25",
"journal-title": "Neurogastroenterol Motil",
"key": "10.1016/j.apsb.2024.02.011_bib45",
"volume": "22",
"year": "2010"
},
{
"DOI": "10.1152/physrev.00049.2019",
"article-title": "Molecular physiology of bile acid signaling in health, disease, and aging",
"author": "Perino",
"doi-asserted-by": "crossref",
"first-page": "683",
"journal-title": "Physiol Rev",
"key": "10.1016/j.apsb.2024.02.011_bib46",
"volume": "101",
"year": "2021"
},
{
"DOI": "10.1016/j.apsb.2021.03.038",
"article-title": "Notoginsenoside Ft1 acts as a TGR5 agonist but FXR antagonist to alleviate high fat diet-induced obesity and insulin resistance in mice",
"author": "Ding",
"doi-asserted-by": "crossref",
"first-page": "1541",
"journal-title": "Acta Pharm Sin B",
"key": "10.1016/j.apsb.2024.02.011_bib47",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.dld.2013.10.021",
"article-title": "The bile acid TGR5 membrane receptor: from basic research to clinical application",
"author": "Duboc",
"doi-asserted-by": "crossref",
"first-page": "302",
"journal-title": "Dig Liver Dis",
"key": "10.1016/j.apsb.2024.02.011_bib48",
"volume": "46",
"year": "2014"
},
{
"article-title": "TGR5 regulates macrophage inflammation in nonalcoholic steatohepatitis by modulating NLRP3 inflammasome activation",
"author": "Shi",
"journal-title": "Front Immunol",
"key": "10.1016/j.apsb.2024.02.011_bib49",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2009.08.001",
"article-title": "TGR5-mediated bile acid sensing controls glucose homeostasis",
"author": "Thomas",
"doi-asserted-by": "crossref",
"first-page": "167",
"journal-title": "Cell Metab",
"key": "10.1016/j.apsb.2024.02.011_bib50",
"volume": "10",
"year": "2009"
},
{
"DOI": "10.1021/acs.jmedchem.6b01873",
"article-title": "Topical intestinal aminoimidazole agonists of G-protein-coupled bile acid receptor 1 promote glucagon like peptide-1 secretion and improve glucose tolerance",
"author": "Lasalle",
"doi-asserted-by": "crossref",
"first-page": "4185",
"journal-title": "J Med Chem",
"key": "10.1016/j.apsb.2024.02.011_bib51",
"volume": "60",
"year": "2017"
},
{
"DOI": "10.1172/JCI76289",
"article-title": "TGR5 reduces macrophage migration through mTOR-induced C/EBPβ differential translation",
"author": "Perino",
"doi-asserted-by": "crossref",
"first-page": "5424",
"journal-title": "J Clin Invest",
"key": "10.1016/j.apsb.2024.02.011_bib52",
"volume": "124",
"year": "2014"
},
{
"DOI": "10.1038/nature04330",
"article-title": "Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation",
"author": "Watanabe",
"doi-asserted-by": "crossref",
"first-page": "484",
"journal-title": "Nature",
"key": "10.1016/j.apsb.2024.02.011_bib53",
"volume": "439",
"year": "2006"
},
{
"DOI": "10.1042/BJ20060537",
"article-title": "Targeted deletion of Gpbar1 protects mice from cholesterol gallstone formation",
"author": "Vassileva",
"doi-asserted-by": "crossref",
"first-page": "423",
"journal-title": "Biochem J",
"key": "10.1016/j.apsb.2024.02.011_bib54",
"volume": "398",
"year": "2006"
},
{
"DOI": "10.1002/hep.21458",
"article-title": "The G‐protein coupled bile salt receptor TGR5 is expressed in liver sinusoidal endothelial cells",
"author": "Keitel",
"doi-asserted-by": "crossref",
"first-page": "695",
"journal-title": "Hepatology",
"key": "10.1016/j.apsb.2024.02.011_bib55",
"volume": "45",
"year": "2007"
},
{
"DOI": "10.1016/j.talanta.2021.123086",
"article-title": "Carboxylic submetabolome-driven signature characterization of COVID-19 asymptomatic infection",
"author": "Xu",
"doi-asserted-by": "crossref",
"journal-title": "Talanta",
"key": "10.1016/j.apsb.2024.02.011_bib56",
"volume": "239",
"year": "2022"
},
{
"DOI": "10.1186/s40249-022-00940-w",
"article-title": "Clinical and antibody characteristics reveal diverse signatures of severe and non-severe SARS-CoV-2 patients",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "Infect Dis Poverty",
"key": "10.1016/j.apsb.2024.02.011_bib57",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1016/j.cell.2020.05.032",
"article-title": "Proteomic and metabolomic characterization of COVID-19 patient sera",
"author": "Shen",
"doi-asserted-by": "crossref",
"first-page": "59",
"journal-title": "Cell",
"key": "10.1016/j.apsb.2024.02.011_bib58",
"volume": "182",
"year": "2020"
},
{
"DOI": "10.1038/s41467-022-34260-2",
"article-title": "Immunomodulatory fecal metabolites are associated with mortality in COVID-19 patients with respiratory failure",
"author": "Stutz",
"doi-asserted-by": "crossref",
"first-page": "6615",
"journal-title": "Nat Commun",
"key": "10.1016/j.apsb.2024.02.011_bib59",
"volume": "13",
"year": "2022"
},
{
"article-title": "Protective effect of ursodeoxycholic acid on COVID-19 in patients with chronic liver disease",
"author": "Li",
"journal-title": "Front Cell Infect Microbiol",
"key": "10.1016/j.apsb.2024.02.011_bib60",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1093/cid/ciac565",
"article-title": "Secondary sclerosing cholangitis following coronavirus disease 2019 (COVID-19): a multicenter retrospective study",
"author": "Hunyady",
"doi-asserted-by": "crossref",
"first-page": "e179",
"journal-title": "Clin Infect Dis",
"key": "10.1016/j.apsb.2024.02.011_bib61",
"volume": "76",
"year": "2023"
},
{
"DOI": "10.1111/joim.13630",
"article-title": "Ursodeoxycholic acid is associated with a reduction in SARS-CoV-2 infection and reduced severity of COVID-19 in patients with cirrhosis",
"author": "John",
"doi-asserted-by": "crossref",
"first-page": "636",
"journal-title": "J Intern Med",
"key": "10.1016/j.apsb.2024.02.011_bib62",
"volume": "293",
"year": "2023"
},
{
"DOI": "10.3390/v15081738",
"article-title": "Ursodeoxycholic acid does not improve COVID-19 outcome in hospitalized patients",
"author": "Colapietro",
"doi-asserted-by": "crossref",
"first-page": "1738",
"journal-title": "Viruses",
"key": "10.1016/j.apsb.2024.02.011_bib63",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1111/liv.15736",
"article-title": "Ursodeoxycholic acid does not affect the clinical outcome of SARS-CoV-2 infection: a retrospective study of propensity score-matched cohorts",
"author": "Marrone",
"doi-asserted-by": "crossref",
"first-page": "83",
"journal-title": "Liver Int",
"key": "10.1016/j.apsb.2024.02.011_bib64",
"volume": "44",
"year": "2024"
},
{
"DOI": "10.1111/liv.15660",
"article-title": "Ursodeoxycholic acid administration did not reduce susceptibility to SARS-CoV-2 infection in children",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "1950",
"journal-title": "Liver Int",
"key": "10.1016/j.apsb.2024.02.011_bib65",
"volume": "43",
"year": "2023"
},
{
"DOI": "10.1016/j.apsb.2023.01.023",
"article-title": "Commentary: Can FXR serve as a potential target for COVID-19 prevention?",
"author": "Pang",
"doi-asserted-by": "crossref",
"first-page": "1786",
"journal-title": "Acta Pharm Sin B",
"key": "10.1016/j.apsb.2024.02.011_bib66",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1080/19490976.2021.1893113",
"article-title": "SARS-CoV-2 infection in nonhuman primates alters the composition and functional activity of the gut microbiota",
"author": "Sokol",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Gut Microbes",
"key": "10.1016/j.apsb.2024.02.011_bib67",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/j.jhep.2020.06.006",
"article-title": "COVID-19 and the liver",
"author": "Jothimani",
"doi-asserted-by": "crossref",
"first-page": "1231",
"journal-title": "J Hepatol",
"key": "10.1016/j.apsb.2024.02.011_bib68",
"volume": "73",
"year": "2020"
},
{
"DOI": "10.4084/MJHID.2022.003",
"article-title": "Mechanism of SARS-CoV-2 Invasion into the Liver and Hepatic Injury in Patients with COVID-19",
"author": "Zhang",
"doi-asserted-by": "crossref",
"journal-title": "Mediterr J Hematol Infect Dis",
"key": "10.1016/j.apsb.2024.02.011_bib69",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1080/19490976.2022.2073131",
"article-title": "A high-risk gut microbiota configuration associates with fatal hyperinflammatory immune and metabolic responses to SARS-CoV-2",
"author": "Albrich",
"doi-asserted-by": "crossref",
"journal-title": "Gut Microbes",
"key": "10.1016/j.apsb.2024.02.011_bib70",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1038/s41575-022-00698-4",
"article-title": "Gut microbiota in COVID-19: key microbial changes, potential mechanisms and clinical applications",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "323",
"journal-title": "Nat Rev Gastroenterol Hepatol",
"key": "10.1016/j.apsb.2024.02.011_bib71",
"volume": "20",
"year": "2023"
},
{
"DOI": "10.1152/ajpgi.00099.2023",
"article-title": "Farnesoid X receptor enhances epithelial ACE2 expression and inhibits virally induced IL-6 secretion: implications for intestinal symptoms of SARS-CoV-2",
"author": "Smyth",
"doi-asserted-by": "crossref",
"first-page": "G446",
"journal-title": "Am J Physiol Gastrointest Liver Physiol",
"key": "10.1016/j.apsb.2024.02.011_bib72",
"volume": "325",
"year": "2023"
},
{
"DOI": "10.3389/fcimb.2022.896504",
"article-title": "Antibiotic-induced primary biles inhibit SARS-CoV-2 endoribonuclease Nsp15 activity in mouse gut",
"author": "Ma",
"doi-asserted-by": "crossref",
"journal-title": "Front Cell Infect Microbiol",
"key": "10.1016/j.apsb.2024.02.011_bib73",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3389/fchem.2020.572885",
"article-title": "Hijacking SARS-CoV-2/ACE2 receptor interaction by natural and semi-synthetic steroidal agents acting on functional pockets on the receptor binding domain",
"author": "Carino",
"doi-asserted-by": "crossref",
"journal-title": "Front Chem",
"key": "10.1016/j.apsb.2024.02.011_bib74",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1002/hep.27999",
"article-title": "Comparative effectiveness of pharmacological interventions for nonalcoholic steatohepatitis: A systematic review and network meta-analysis",
"author": "Singh",
"doi-asserted-by": "crossref",
"first-page": "1417",
"journal-title": "Hepatology",
"key": "10.1016/j.apsb.2024.02.011_bib75",
"volume": "62",
"year": "2015"
},
{
"DOI": "10.3748/wjg.v23.i42.7495",
"article-title": "Current and emerging pharmacological therapy for non-alcoholic fatty liver disease",
"author": "Eshraghian",
"doi-asserted-by": "crossref",
"first-page": "7495",
"journal-title": "World J Gastroenterol",
"key": "10.1016/j.apsb.2024.02.011_bib76",
"volume": "23",
"year": "2017"
},
{
"DOI": "10.1016/0950-3528(90)90051-H",
"article-title": "Pathogenesis of gut virus infection",
"author": "Salim",
"doi-asserted-by": "crossref",
"first-page": "593",
"journal-title": "Baillieres Clin Gastroenterol",
"key": "10.1016/j.apsb.2024.02.011_bib77",
"volume": "4",
"year": "1990"
},
{
"DOI": "10.1111/bph.12159",
"article-title": "ACE2, angiotensin-(1-7) and Mas receptor axis in inflammation and fibrosis",
"author": "Simoes e Silva",
"doi-asserted-by": "crossref",
"first-page": "477",
"journal-title": "Br J Pharmacol",
"key": "10.1016/j.apsb.2024.02.011_bib78",
"volume": "169",
"year": "2013"
},
{
"DOI": "10.1016/B978-0-12-804274-8.00055-2",
"doi-asserted-by": "crossref",
"key": "10.1016/j.apsb.2024.02.011_bib79",
"unstructured": "Wang JY, Wu SD. Chapter 55—Ursodeoxycholic acid for the treatment of liver diseases. In: Muriel P, editor. Liver pathophysiology. London: Elsevier Science; 2017. p. 767–779."
},
{
"DOI": "10.1016/j.biopha.2022.113021",
"article-title": "Ursodeoxycholic acid ameliorates cell migration retarded by the SARS-CoV-2 spike protein in BEAS-2B human bronchial epithelial cells",
"author": "Thuy",
"doi-asserted-by": "crossref",
"journal-title": "Biomed Pharmacother",
"key": "10.1016/j.apsb.2024.02.011_bib80",
"volume": "150",
"year": "2022"
},
{
"DOI": "10.1016/j.bbalip.2019.07.006",
"article-title": "Ursodeoxycholic acid is a GPBAR1 agonist and resets liver/intestinal FXR signaling in a model of diet-induced dysbiosis and NASH",
"author": "Carino",
"doi-asserted-by": "crossref",
"first-page": "1422",
"journal-title": "Biochim Biophys Acta Mol Cell Biol Lipids",
"key": "10.1016/j.apsb.2024.02.011_bib81",
"volume": "1864",
"year": "2019"
},
{
"DOI": "10.1021/acs.jcim.1c01126",
"article-title": "Discovery of bile acid derivatives as potent ACE2 activators by virtual screening and essential dynamics",
"author": "Fiorillo",
"doi-asserted-by": "crossref",
"first-page": "196",
"journal-title": "J Chem Inf Model",
"key": "10.1016/j.apsb.2024.02.011_bib82",
"volume": "62",
"year": "2022"
},
{
"DOI": "10.1016/j.mehy.2020.109897",
"article-title": "Ursodeoxycholic acid as a candidate therapeutic to alleviate and/or prevent COVID-19-associated cytokine storm",
"author": "Abdulrab",
"doi-asserted-by": "crossref",
"journal-title": "Med Hypotheses",
"key": "10.1016/j.apsb.2024.02.011_bib83",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.3390/cells10113206",
"article-title": "The pathophysiology of farnesoid X receptor (FXR) in the GI tract: inflammation, barrier function and innate immunity",
"author": "Anderson",
"doi-asserted-by": "crossref",
"first-page": "3206",
"journal-title": "Cells",
"key": "10.1016/j.apsb.2024.02.011_bib84",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2018.01853",
"article-title": "Bile acids activated receptors regulate innate immunity",
"author": "Fiorucci",
"doi-asserted-by": "crossref",
"first-page": "1853",
"journal-title": "Front Immunol",
"key": "10.1016/j.apsb.2024.02.011_bib85",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1038/nri.2016.36",
"article-title": "Development and maintenance of intestinal regulatory T cells",
"author": "Tanoue",
"doi-asserted-by": "crossref",
"first-page": "295",
"journal-title": "Nat Rev Immunol",
"key": "10.1016/j.apsb.2024.02.011_bib86",
"volume": "16",
"year": "2016"
},
{
"DOI": "10.1038/s41586-020-2193-0",
"article-title": "Bacterial metabolism of bile acids promotes generation of peripheral regulatory T cells",
"author": "Campbell",
"doi-asserted-by": "crossref",
"first-page": "475",
"journal-title": "Nature",
"key": "10.1016/j.apsb.2024.02.011_bib87",
"volume": "581",
"year": "2020"
},
{
"DOI": "10.4049/jimmunol.0901347",
"article-title": "The bile acid sensor farnesoid X receptor is a modulator of liver immunity in a rodent model of acute hepatitis",
"author": "Mencarelli",
"doi-asserted-by": "crossref",
"first-page": "6657",
"journal-title": "J Immunol",
"key": "10.1016/j.apsb.2024.02.011_bib88",
"volume": "183",
"year": "2009"
},
{
"DOI": "10.1016/j.cellsig.2012.04.015",
"article-title": "FXR ligands protect against hepatocellular inflammation via SOCS3 induction",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "1658",
"journal-title": "Cell Signal",
"key": "10.1016/j.apsb.2024.02.011_bib89",
"volume": "24",
"year": "2012"
},
{
"DOI": "10.1038/ncomms5573",
"article-title": "PPARα–UGT axis activation represses intestinal FXR-FGF15 feedback signalling and exacerbates experimental colitis",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "4573",
"journal-title": "Nat Commun",
"key": "10.1016/j.apsb.2024.02.011_bib90",
"volume": "5",
"year": "2014"
},
{
"DOI": "10.3389/fphar.2021.750826",
"article-title": "Berberine alleviates non-alcoholic steatohepatitis through modulating gut microbiota mediated intestinal FXR activation",
"author": "Shu",
"doi-asserted-by": "crossref",
"journal-title": "Front Pharmacol",
"key": "10.1016/j.apsb.2024.02.011_bib91",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1007/s10787-022-01080-1",
"article-title": "The role of berberine in Covid-19: potential adjunct therapy",
"author": "Babalghith",
"doi-asserted-by": "crossref",
"first-page": "2003",
"journal-title": "Inflammopharmacology",
"key": "10.1016/j.apsb.2024.02.011_bib92",
"volume": "30",
"year": "2022"
},
{
"DOI": "10.1016/j.antiviral.2020.104878",
"article-title": "In vitro evaluation of antiviral activity of single and combined repurposable drugs against SARS-CoV-2",
"author": "Pizzorno",
"doi-asserted-by": "crossref",
"journal-title": "Antiviral Res",
"key": "10.1016/j.apsb.2024.02.011_bib93",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.3390/v13020282",
"article-title": "Berberine and obatoclax inhibit SARS-Cov-2 replication in primary human nasal epithelial cells in vitro",
"author": "Varghese",
"doi-asserted-by": "crossref",
"first-page": "282",
"journal-title": "Viruses",
"key": "10.1016/j.apsb.2024.02.011_bib94",
"volume": "13",
"year": "2021"
},
{
"article-title": "A small molecule compound berberine as an orally active therapeutic candidate against COVID-19 and SARS: a computational and mechanistic study",
"author": "Wang",
"journal-title": "FASEB J",
"key": "10.1016/j.apsb.2024.02.011_bib95",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1093/bjs/znaa021",
"article-title": "Berberine reduces circulating inflammatory mediators in patients with severe COVID-19",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "e9",
"journal-title": "Br J Surg",
"key": "10.1016/j.apsb.2024.02.011_bib96",
"volume": "108",
"year": "2021"
},
{
"DOI": "10.1016/j.apsb.2022.09.002",
"article-title": "Research and development of Chinese anti-COVID-19 drugs",
"author": "Ji",
"doi-asserted-by": "crossref",
"first-page": "4271",
"journal-title": "Acta Pharm Sin B",
"key": "10.1016/j.apsb.2024.02.011_bib97",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.taap.2011.11.006",
"article-title": "A tea catechin, epigallocatechin-3-gallate, is a unique modulator of the farnesoid X receptor",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "268",
"journal-title": "Toxicol Appl Pharmacol",
"key": "10.1016/j.apsb.2024.02.011_bib98",
"volume": "258",
"year": "2012"
},
{
"DOI": "10.3390/molecules26051200",
"article-title": "EGCG, a green tea catechin, as a potential therapeutic agent for symptomatic and asymptomatic SARS-CoV-2 infection",
"author": "Chourasia",
"doi-asserted-by": "crossref",
"first-page": "1200",
"journal-title": "Molecules",
"key": "10.1016/j.apsb.2024.02.011_bib99",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1099/jgv.0.001574",
"article-title": "The green tea catechin epigallocatechin gallate inhibits SARS-CoV-2 infection",
"author": "Henss",
"doi-asserted-by": "crossref",
"journal-title": "J Gen Virol",
"key": "10.1016/j.apsb.2024.02.011_bib100",
"volume": "102",
"year": "2021"
},
{
"DOI": "10.1186/s13578-021-00680-8",
"article-title": "Epigallocatechin gallate from green tea effectively blocks infection of SARS-CoV-2 and new variants by inhibiting spike binding to ACE2 receptor",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "168",
"journal-title": "Cell Biosci",
"key": "10.1016/j.apsb.2024.02.011_bib101",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.tifs.2022.12.012",
"article-title": "Potential of green tea EGCG in neutralizing SARS-CoV-2 Omicron variant with greater tropism toward the upper respiratory tract",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "40",
"journal-title": "Trends Food Sci Technol",
"key": "10.1016/j.apsb.2024.02.011_bib102",
"volume": "132",
"year": "2023"
},
{
"DOI": "10.1016/j.bbrc.2021.02.016",
"article-title": "EGCG, a green tea polyphenol, inhibits human coronavirus replication in vitro",
"author": "Jang",
"doi-asserted-by": "crossref",
"first-page": "23",
"journal-title": "Biochem Biophys Res Commun",
"key": "10.1016/j.apsb.2024.02.011_bib103",
"volume": "547",
"year": "2021"
},
{
"DOI": "10.1111/jfbc.13707",
"article-title": "Study on the mechanism of active components of Liupao tea on 3CL(pro) based on HPLC-DAD fingerprint and molecular docking technique",
"author": "Ni",
"doi-asserted-by": "crossref",
"journal-title": "J Food Biochem",
"key": "10.1016/j.apsb.2024.02.011_bib104",
"volume": "45",
"year": "2021"
},
{
"DOI": "10.1016/j.bbrc.2020.12.106",
"article-title": "The inhibitory effects of PGG and EGCG against the SARS-CoV-2 3C-like protease",
"author": "Chiou",
"doi-asserted-by": "crossref",
"first-page": "130",
"journal-title": "Biochem Biophys Res Commun",
"key": "10.1016/j.apsb.2024.02.011_bib105",
"volume": "591",
"year": "2022"
},
{
"DOI": "10.1016/j.tifs.2021.05.023",
"article-title": "Potential protective mechanisms of green tea polyphenol EGCG against COVID-19",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "11",
"journal-title": "Trends Food Sci Technol",
"key": "10.1016/j.apsb.2024.02.011_bib106",
"volume": "114",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2601-5",
"article-title": "Papain-like protease regulates SARS-CoV-2 viral spread and innate immunity",
"author": "Shin",
"doi-asserted-by": "crossref",
"first-page": "657",
"journal-title": "Nature",
"key": "10.1016/j.apsb.2024.02.011_bib107",
"volume": "587",
"year": "2020"
},
{
"DOI": "10.1038/s41467-021-25796-w",
"article-title": "Characterising proteolysis during SARS-CoV-2 infection identifies viral cleavage sites and cellular targets with therapeutic potential",
"author": "Meyer",
"doi-asserted-by": "crossref",
"first-page": "5553",
"journal-title": "Nat Commun",
"key": "10.1016/j.apsb.2024.02.011_bib108",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1021/acsinfecdis.1c00629",
"article-title": "Drug-repurposing screening identified tropifexor as a SARS-CoV-2 papain-like Protease inhibitor",
"author": "Ma",
"doi-asserted-by": "crossref",
"first-page": "1022",
"journal-title": "ACS Infect Dis",
"key": "10.1016/j.apsb.2024.02.011_bib109",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1096/fj.202200171R",
"article-title": "Dihydroartemisinin promoted FXR expression independent of YAP1 in hepatocellular carcinoma",
"author": "Guo",
"doi-asserted-by": "crossref",
"journal-title": "FASEB J",
"key": "10.1016/j.apsb.2024.02.011_bib110",
"volume": "36",
"year": "2022"
},
{
"DOI": "10.1021/acsinfecdis.0c00522",
"article-title": "Anti-SARS-CoV-2 potential of artemisinins in vitro",
"author": "Cao",
"doi-asserted-by": "crossref",
"first-page": "2524",
"journal-title": "ACS Infect Dis",
"key": "10.1016/j.apsb.2024.02.011_bib111",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1126/science.1072891",
"article-title": "A natural product that lowers cholesterol as an antagonist ligand for FXR",
"author": "Urizar",
"doi-asserted-by": "crossref",
"first-page": "1703",
"journal-title": "Science",
"key": "10.1016/j.apsb.2024.02.011_bib112",
"volume": "296",
"year": "2002"
},
{
"DOI": "10.1053/j.gastro.2016.08.057",
"article-title": "An intestinal microbiota-farnesoid X receptor axis modulates metabolic disease",
"author": "Gonzalez",
"doi-asserted-by": "crossref",
"first-page": "845",
"journal-title": "Gastroenterology",
"key": "10.1016/j.apsb.2024.02.011_bib113",
"volume": "151",
"year": "2016"
},
{
"DOI": "10.1126/science.abi5224",
"article-title": "Fe-S cofactors in the SARS-CoV-2 RNA-dependent RNA polymerase are potential antiviral targets",
"author": "Maio",
"doi-asserted-by": "crossref",
"first-page": "236",
"journal-title": "Science",
"key": "10.1016/j.apsb.2024.02.011_bib114",
"volume": "373",
"year": "2021"
},
{
"DOI": "10.1016/j.isci.2022.105074",
"article-title": "TEMPOL inhibits SARS-CoV-2 replication and development of lung disease in the Syrian hamster model",
"author": "Maio",
"doi-asserted-by": "crossref",
"journal-title": "iScience",
"key": "10.1016/j.apsb.2024.02.011_bib115",
"volume": "25",
"year": "2022"
},
{
"DOI": "10.1016/j.clim.2021.108828",
"article-title": "Brief report: Tempol, a novel antioxidant, inhibits both activated T cell and antigen presenting cell derived cytokines in-vitro from COVID-19 patients",
"author": "Mathi",
"doi-asserted-by": "crossref",
"journal-title": "Clin Immunol",
"key": "10.1016/j.apsb.2024.02.011_bib116",
"volume": "231",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2286-9",
"article-title": "A SARS-CoV-2 protein interaction map reveals targets for drug repurposing",
"author": "Gordon",
"doi-asserted-by": "crossref",
"first-page": "459",
"journal-title": "Nature",
"key": "10.1016/j.apsb.2024.02.011_bib117",
"volume": "583",
"year": "2020"
},
{
"DOI": "10.1172/jci.insight.148003",
"article-title": "Ex vivo SARS-CoV-2 infection of human lung reveals heterogeneous host defense and therapeutic responses",
"author": "Schaller",
"doi-asserted-by": "crossref",
"journal-title": "JCI Insight",
"key": "10.1016/j.apsb.2024.02.011_bib118",
"volume": "6",
"year": "2021"
},
{
"article-title": "Metformin suppresses SARS-CoV-2 in cell culture",
"author": "Parthasarathy",
"journal-title": "Virus Res",
"key": "10.1016/j.apsb.2024.02.011_bib119",
"volume": "323",
"year": "2022"
},
{
"DOI": "10.1016/j.immuni.2021.05.004",
"article-title": "Metformin inhibition of mitochondrial ATP and DNA synthesis abrogates NLRP3 inflammasome activation and pulmonary inflammation",
"author": "Xian",
"doi-asserted-by": "crossref",
"first-page": "1463",
"journal-title": "Immunity",
"key": "10.1016/j.apsb.2024.02.011_bib120",
"volume": "54",
"year": "2021"
},
{
"DOI": "10.1016/S2666-7568(20)30033-7",
"article-title": "Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis",
"author": "Bramante",
"doi-asserted-by": "crossref",
"first-page": "e34",
"journal-title": "Lancet Healthy Longev",
"key": "10.1016/j.apsb.2024.02.011_bib121",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"article-title": "Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England",
"author": "Khunti",
"doi-asserted-by": "crossref",
"first-page": "293",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "10.1016/j.apsb.2024.02.011_bib122",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.metabol.2022.155196",
"article-title": "Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: a meta-analysis",
"author": "Nguyen",
"doi-asserted-by": "crossref",
"journal-title": "Metabolism",
"key": "10.1016/j.apsb.2024.02.011_bib123",
"volume": "131",
"year": "2022"
},
{
"DOI": "10.1002/jmv.26873",
"article-title": "Outpatient metformin use is associated with reduced severity of COVID-19 disease in adults with overweight or obesity",
"author": "Bramante",
"doi-asserted-by": "crossref",
"first-page": "4273",
"journal-title": "J Med Virol",
"key": "10.1016/j.apsb.2024.02.011_bib124",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1016/j.cmet.2020.08.013",
"article-title": "Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and pre-existing type 2 diabetes",
"author": "Cheng",
"doi-asserted-by": "crossref",
"first-page": "537",
"journal-title": "Cell Metab",
"key": "10.1016/j.apsb.2024.02.011_bib125",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2201662",
"article-title": "Randomized trial of metformin, ivermectin, and fluvoxamine for Covid-19",
"author": "Bramante",
"doi-asserted-by": "crossref",
"first-page": "599",
"journal-title": "N Engl J Med",
"key": "10.1016/j.apsb.2024.02.011_bib126",
"volume": "387",
"year": "2022"
},
{
"DOI": "10.3389/fimmu.2018.02289",
"article-title": "Metabolite-sensing G protein coupled receptor TGR5 protects host from viral infection through amplifying type I interferon responses",
"author": "Xiong",
"doi-asserted-by": "crossref",
"first-page": "2289",
"journal-title": "Front Immunol",
"key": "10.1016/j.apsb.2024.02.011_bib127",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1038/sj.cr.7310019",
"article-title": "Antiviral innate immunity pathways",
"author": "Seth",
"doi-asserted-by": "crossref",
"first-page": "141",
"journal-title": "Cell Research",
"key": "10.1016/j.apsb.2024.02.011_bib128",
"volume": "16",
"year": "2006"
},
{
"DOI": "10.1038/s41467-021-25015-6",
"article-title": "SARS-CoV-2 N protein promotes NLRP3 inflammasome activation to induce hyperinflammation",
"author": "Pan",
"doi-asserted-by": "crossref",
"first-page": "4664",
"journal-title": "Nat Commun",
"key": "10.1016/j.apsb.2024.02.011_bib129",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41586-022-04702-4",
"article-title": "FcγR-mediated SARS-CoV-2 infection of monocytes activates inflammation",
"author": "Junqueira",
"doi-asserted-by": "crossref",
"first-page": "576",
"journal-title": "Nature",
"key": "10.1016/j.apsb.2024.02.011_bib130",
"volume": "606",
"year": "2022"
},
{
"DOI": "10.1016/j.immuni.2016.09.008",
"article-title": "Bile acids control inflammation and metabolic disorder through inhibition of NLRP3 inflammasome",
"author": "Guo",
"doi-asserted-by": "crossref",
"first-page": "802",
"journal-title": "Immunity",
"key": "10.1016/j.apsb.2024.02.011_bib131",
"volume": "45",
"year": "2016"
},
{
"DOI": "10.1002/hep.24525",
"article-title": "The G-protein-coupled bile acid receptor, Gpbar1 (TGR5), negatively regulates hepatic inflammatory response through antagonizing nuclear factor κ light-chain enhancer of activated B cells (NF-κB) in mice",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1421",
"journal-title": "Hepatology",
"key": "10.1016/j.apsb.2024.02.011_bib132",
"volume": "54",
"year": "2011"
},
{
"DOI": "10.1016/j.celrep.2021.109726",
"article-title": "Gut microbiota-mediated secondary bile acids regulate dendritic cells to attenuate autoimmune uveitis through TGR5 signaling",
"author": "Hu",
"doi-asserted-by": "crossref",
"journal-title": "Cell Rep",
"key": "10.1016/j.apsb.2024.02.011_bib133",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.4049/jimmunol.1700183",
"article-title": "The bile acid receptor GPBAR1 regulates the M1/M2 phenotype of intestinal macrophages and activation of GPBAR1 rescues mice from murine colitis",
"author": "Biagioli",
"doi-asserted-by": "crossref",
"first-page": "718",
"journal-title": "J Immunol",
"key": "10.1016/j.apsb.2024.02.011_bib134",
"volume": "199",
"year": "2017"
},
{
"DOI": "10.1007/s13238-020-00718-6",
"article-title": "Recapitulation of SARS-CoV-2 infection and cholangiocyte damage with human liver ductal organoids",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "771",
"journal-title": "Protein Cell",
"key": "10.1016/j.apsb.2024.02.011_bib135",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1136/gutjnl-2015-309458",
"article-title": "TGR5 is essential for bile acid-dependent cholangiocyte proliferation in vivo and in vitro",
"author": "Reich",
"doi-asserted-by": "crossref",
"first-page": "487",
"journal-title": "Gut",
"key": "10.1016/j.apsb.2024.02.011_bib136",
"volume": "65",
"year": "2016"
},
{
"DOI": "10.1016/j.jhep.2021.03.029",
"article-title": "Downregulation of TGR5 (GPBAR1) in biliary epithelial cells contributes to the pathogenesis of sclerosing cholangitis",
"author": "Reich",
"doi-asserted-by": "crossref",
"first-page": "634",
"journal-title": "J Hepatol",
"key": "10.1016/j.apsb.2024.02.011_bib137",
"volume": "75",
"year": "2021"
},
{
"article-title": "TGR5 controls bile acid composition and gallbladder function to protect the liver from bile acid overload",
"author": "Bidault-Jourdainne",
"journal-title": "JHEP Rep",
"key": "10.1016/j.apsb.2024.02.011_bib138",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.1016/j.tips.2018.01.001",
"article-title": "New insights into modes of GPCR activation",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "367",
"journal-title": "Trends Pharmacol Sci",
"key": "10.1016/j.apsb.2024.02.011_bib139",
"volume": "39",
"year": "2018"
},
{
"DOI": "10.1038/s41422-018-0136-1",
"article-title": "Virus-induced accumulation of intracellular bile acids activates the TGR5-beta-arrestin-SRC axis to enable innate antiviral immunity",
"author": "Hu",
"doi-asserted-by": "crossref",
"first-page": "193",
"journal-title": "Cell Res",
"key": "10.1016/j.apsb.2024.02.011_bib140",
"volume": "29",
"year": "2019"
}
],
"reference-count": 140,
"references-count": 140,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2211383524000492"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Pharmacology, Toxicology and Pharmaceutics"
],
"subtitle": [],
"title": "Bile acids and coronavirus disease 2019",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}