A Study on Serum Vitamin D3 Level in Patients with Covid-19: A Cross-Sectional Study in Kolkata
et al., National Journal of Medical Research, doi:10.55489/njmr.150220251070, Apr 2025
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Analysis of 100 hospitalized COVID-19 patients in India showing strong association between vitamin D deficiency and COVID-19 severity.
This is the 215th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of severe case, 58.4% lower, RR 0.42, p = 0.002, high D levels (≥20 ng/ml) 8 of 33 (24.2%), low D levels (<20 ng/ml) 39 of 67 (58.2%), NNT 2.9.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Hossain et al., 1 Apr 2025, retrospective, India, peer-reviewed, mean age 51.7, 5 authors, study period January 2021 - January 2022.
Contact: amritajha.1102@gmail.com.
A Study on Serum Vitamin D3 Level in Patients with Covid-19: A Cross-Sectional Study in Kolkata
National Journal of Medical Research, doi:10.55489/njmr.150220251070
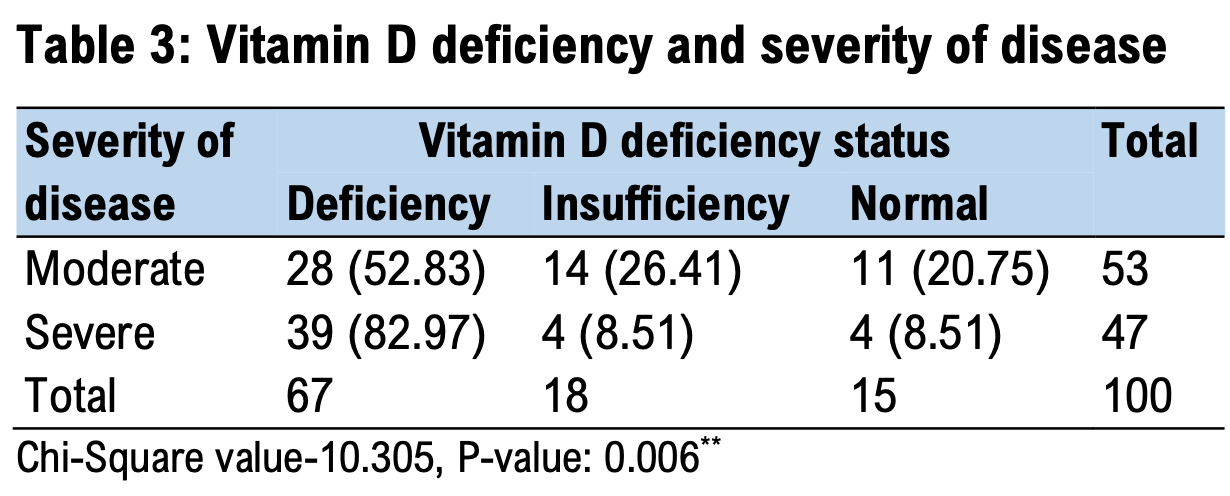
Background: Coronavirus disease (COVID-19) is a global pandemic caused by SARS-CoV-2. Vitamin D has immunomodulatory and anti-inflammatory properties, potentially influencing the disease course. This study assessed the prevalence of 25(OH) vitamin D deficiency in COVID-19 patients and its association with disease severity in the Indian population. Methodology: A hospital-based cross-sectional study was conducted at Medical College, Kolkata, including 100 RT-PCR-confirmed moderate and severe COVID-19 patients. Disease severity was categorized based on oxygen saturation. Serum 25-Hydroxy vitamin D levels were measured on admission, along with other hematological and biochemical parameters. High-resolution CT scans were performed to assess pulmonary involvement. Results: Vitamin D insufficiency and deficiency were observed in 18% and 67% of patients, respectively. Deficiency was more prevalent in severe cases (82.97%) than moderate cases (52.83%). The mean vitamin D levels in moderate and severe disease groups were 23.23±8.74 and 17.17±8.09 ng/ml, respectively. A significant association was found between vitamin D deficiency and COVID-19 severity (P = 0.006). The vitamin D cutoff for predicting severe disease was 18.57 ng/dl.
Conclusion: Vitamin D deficiency is strongly associated with severe COVID-19 in the Indian population. Low vitamin D levels may predict disease severity, suggesting supplementation as a potential preventive strategy.
Conflict of Interest: The authors have declared that no conflicts of interest exist.
References
Cereda, Bogliolo, Klersy, Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital, Clinical nutrition, doi:10.1016/j.clnu.2020.10.055PMid:33187772PMCid
Chan, Rout, Use of neutrophil-to-lymphocyte and platelet-tolymphocyte ratios in COVID-19, Journal of clinical medicine research, doi:10.14740/jocmr4240PMid:32655740PMCid:PMC7331861
Chan, Rout, Use of neutrophil-to-lymphocyte and platelet-tolymphocyte ratios in COVID-19, Journal of clinical medicine research, doi:10.14740/jocmr4240PMid:32655740PMCid:PMC7331861
Cheng, Luo, Wang, Kidney impairment is associated with in-hospital death of COVID-19 patients, MedRxiv, doi:10.1101/2020.02.18.20023242
Cheng, Luo, Wang, Kidney impairment is associated with in-hospital death of COVID-19 patients, MedRxiv, doi:10.1101/2020.02.18.20023242
Francone, Iafrate, Masci, Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis, European radiology, doi:10.1007/s00330-020-07033-yPMid:32623505
Ginde, Mansbach, Camargo, Vitamin D, respiratory infections, and asthma. Current allergy and asthma reports, doi:10.1007/s11882-009-0012-7
Hamming, Timens, Bulthuis, Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis, J Pathol, doi:10.1002/path.1570PMid:15141377
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Scientific reports, doi:10.1038/s41598-020-77093-zPMid:33214648PMCid:PMC7677378
Lemire, Adams, Sakai, Jordan, 1 alpha, 25-dihydroxyvitamin D3 suppresses proliferation and immunoglobulin production by normal human peripheral blood mononuclear cells, The Journal of clinical investigation, doi:10.1172/JCI111465PMid:6611355PMCid:PMC370520
Li, Ye, Chen, Elevated Lactate Dehydrogenase (LDH) level as an independent risk factor for the severity and mortality of COVID-19, Aging, doi:10.18632/aging.103770PMid:32805722
Li, Ye, Chen, Elevated Lactate Dehydrogenase (LDH) level as an independent risk factor for the severity and mortality of COVID-19, Aging, doi:10.18632/aging.103770PMid:32805722
Lin, Long, Yang, Chen, Xu et al., Serum ferritin as an independent risk factor for severity in COVID-19 patients, Journal of infection, doi:10.1016/j.jinf.2020.06.053PMid:32592705PMCid
Lin, Long, Yang, Chen, Xu et al., Serum ferritin as an independent risk factor for severity in COVID-19 patients, Journal of infection, doi:10.1016/j.jinf.2020.06.053PMid:32592705PMCid
Luo, Liao, Shen, Li, Cheng, Vitamin D deficiency is associated with COVID-19 incidence and disease severity in Chinese people, The Journal of nutrition, doi:10.1093/jn/nxaa332PMid:33188401
Nimavat, Singh, Singh, Singh, Sinha, Vitamin D deficiency and COVID-19: A case-control study at a tertiary care hospital in India, Annals of Medicine and Surgery, doi:10.1016/j.amsu.2021.102661PMid:34377451
Prietl, Treiber, Pieber, Amrein, Vitamin D and immune function, Nutrients, doi:10.3390/nu5072502PMid:23857223PMCid:PMC3738984
Radujkovic, Hippchen, Tiwari-Heckler, Vitamin D deficiency and outcome of COVID-19 patients, Nutrients, doi:10.3390/nu12092757
Smet, Smet, Herroelen, Gryspeerdt, Martens, Serum 25 (OH) D level on hospital admission associated with COVID-19 stage and mortality, American journal of clinical pathology, doi:10.1093/ajcp/aqaa252PMid:33236114PMCid:PMC7717135
Teama, Abdelhakam, Elmohamadi, Badr, Vitamin D deficiency as a predictor of severity in patients with COVID-19 infection, Science Progress, doi:10.1177/00368504211036854
Teama, Abdelhakam, Elmohamadi, Badr, Vitamin D deficiency as a predictor of severity in patients with COVID-19 infection, Science Progress, doi:10.1177/00368504211036854PMid:34347528PMCid:PMC10450705
Wang, Hu, Hu, Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, JAMA, doi:10.1001/jama.2020.1585PMid:32031570PMCid:PMC7042881
Wang, Shi, Wang, Duan, Yang, Albumin and total bilirubin for severity and mortality in coronavirus disease 2019 patients, Journal of Clinical Laboratory Analysis, doi:10.1002/jcla.23412PMid:32745325PMCid:PMC7323086
Wang, Shi, Wang, Duan, Yang, Albumin and total bilirubin for severity and mortality in coronavirus disease 2019 patients, Journal of Clinical Laboratory Analysis, doi:10.1002/jcla.23412PMid:32745325PMCid:PMC7323086
Yang, Liu, Liu, COVID-19: immunopathogenesis and Immunotherapeutics, Signal transduction and targeted therapy, doi:10.1038/s41392-020-00243-2PMid:32712629PMCid:PMC7381863
Yao, Cao, Wang, Shi, Liu et al., D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: a case control study, Journal of intensive care, doi:10.1186/s40560-020-00466-zPMid:32665858PMCid:PMC7348129
Yao, Cao, Wang, Shi, Liu et al., D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: a case control study, Journal of intensive care, doi:10.1186/s40560-020-00466-zPMid:32665858PMCid:PMC7348129
Ye, Tang, Liao, Does serum vitamin D level affect COVID-19 infection and its severity? -A case-control study, Journal of the American College of Nutrition, doi:10.1080/07315724.2020.1826005PMid:33048028
DOI record:
{
"DOI": "10.55489/njmr.150220251070",
"ISSN": [
"2277-8810",
"2249-4995"
],
"URL": "http://dx.doi.org/10.55489/njmr.150220251070",
"abstract": "<jats:p>Background: Coronavirus disease (COVID-19) is a global pandemic caused by SARS-CoV-2. Vitamin D has immunomodulatory and anti-inflammatory properties, potentially influencing the disease course. This study assessed the prevalence of 25(OH) vitamin D deficiency in COVID-19 patients and its association with disease severity in the Indian population.\nMethodology: A hospital-based cross-sectional study was conducted at Medical College, Kolkata, including 100 RT-PCR-confirmed moderate and severe COVID-19 patients. Disease severity was categorized based on oxygen saturation. Serum 25-Hydroxy vitamin D levels were measured on admission, along with other hematological and biochemical parameters. High-resolution CT scans were performed to assess pulmonary involvement.\nResults: Vitamin D insufficiency and deficiency were observed in 18% and 67% of patients, respectively. Deficiency was more prevalent in severe cases (82.97%) than moderate cases (52.83%). The mean vitamin D levels in moderate and severe disease groups were 23.23±8.74 and 17.17±8.09 ng/ml, respectively. A significant association was found between vitamin D deficiency and COVID-19 severity (P = 0.006). The vitamin D cutoff for predicting severe disease was 18.57 ng/dl.\nConclusion: Vitamin D deficiency is strongly associated with severe COVID-19 in the Indian population. Low vitamin D levels may predict disease severity, suggesting supplementation as a potential preventive strategy.</jats:p>",
"author": [
{
"ORCID": "https://orcid.org/0000-0002-6283-1665",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hossain",
"given": "Enamul",
"sequence": "first"
},
{
"ORCID": "https://orcid.org/0000-0002-2925-056X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mandal",
"given": "Sanjay K",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-0662-6333",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sarkar",
"given": "Souvik",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0009-0001-8331-8131",
"affiliation": [],
"authenticated-orcid": false,
"family": "Jha",
"given": "Amrita",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0009-0001-4207-5233",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mondal",
"given": "Ranjan",
"sequence": "additional"
}
],
"container-title": "National Journal of Medical Research",
"container-title-short": "Natl J Med Res",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2025,
4,
1
]
],
"date-time": "2025-04-01T10:28:11Z",
"timestamp": 1743503291000
},
"deposited": {
"date-parts": [
[
2025,
4,
1
]
],
"date-time": "2025-04-01T10:36:49Z",
"timestamp": 1743503809000
},
"indexed": {
"date-parts": [
[
2025,
4,
1
]
],
"date-time": "2025-04-01T11:10:08Z",
"timestamp": 1743505808339,
"version": "3.40.3"
},
"is-referenced-by-count": 0,
"issue": "02",
"issued": {
"date-parts": [
[
2025,
4,
1
]
]
},
"journal-issue": {
"issue": "02",
"published-online": {
"date-parts": [
[
2025,
4,
1
]
]
}
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by-sa/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
4,
1
]
],
"date-time": "2025-04-01T00:00:00Z",
"timestamp": 1743465600000
}
}
],
"link": [
{
"URL": "https://njmr.in/index.php/file/article/download/1070/890",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://njmr.in/index.php/file/article/download/1070/890",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "34154",
"original-title": [],
"page": "126-131",
"prefix": "10.55489",
"published": {
"date-parts": [
[
2025,
4,
1
]
]
},
"published-online": {
"date-parts": [
[
2025,
4,
1
]
]
},
"publisher": "Medsci Publications",
"reference": [
{
"DOI": "10.1002/path.1570",
"doi-asserted-by": "crossref",
"key": "3875",
"unstructured": "Hamming I, Timens W, Bulthuis ML, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631-637. DOI: https://doi.org/10.1002/path.1570 PMid:15141377 PMCid:PMC7167720"
},
{
"DOI": "10.1001/jama.2020.1585",
"doi-asserted-by": "crossref",
"key": "3876",
"unstructured": "Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061. DOI: https://doi.org/10.1001/jama.2020.1585 PMid:32031570 PMCid:PMC7042881"
},
{
"DOI": "10.1038/s41392-020-00243-2",
"doi-asserted-by": "crossref",
"key": "3877",
"unstructured": "Yang L, Liu S, Liu J, et al. COVID-19: immunopathogenesis and Immunotherapeutics. Signal transduction and targeted therapy. 2020 Jul 25;5(1):1-8. DOI: https://doi.org/10.1038/s41392-020-00243-2 PMid:32712629 PMCid:PMC7381863"
},
{
"DOI": "10.3390/nu5072502",
"doi-asserted-by": "crossref",
"key": "3878",
"unstructured": "Prietl B, Treiber G, Pieber TR, Amrein K. Vitamin D and immune function. Nutrients. 2013 Jul 5;5(7):2502-21. DOI: https://doi.org/10.3390/nu5072502 PMid:23857223 PMCid:PMC3738984"
},
{
"DOI": "10.1172/JCI111465",
"doi-asserted-by": "crossref",
"key": "3879",
"unstructured": "Lemire JM, Adams JS, Sakai R, Jordan SC. 1 alpha, 25-dihydroxyvitamin D3 suppresses proliferation and immunoglobulin production by normal human peripheral blood mononuclear cells. The Journal of clinical investigation. 1984 Aug 1;74(2):657-61. DOI: https://doi.org/10.1172/JCI111465 PMid:6611355 PMCid:PMC370520"
},
{
"DOI": "10.1007/s11882-009-0012-7",
"doi-asserted-by": "crossref",
"key": "3880",
"unstructured": "Ginde AA, Mansbach JM, Camargo CA. Vitamin D, respiratory infections, and asthma. Current allergy and asthma reports. 2009 Jan;9(1):81-7. DOI: https://doi.org/10.1007/s11882-009-0012-7 PMid:19063829"
},
{
"DOI": "10.1016/j.amsu.2021.102661",
"doi-asserted-by": "crossref",
"key": "3881",
"unstructured": "Nimavat N, Singh S, Singh P, Singh SK, Sinha N. Vitamin D deficiency and COVID-19: A case-control study at a tertiary care hospital in India. Annals of Medicine and Surgery. 2021 Aug 1;68:102661. DOI: https://doi.org/10.1016/j.amsu.2021.102661 PMid:34377451 PMCid:PMC8339450"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"doi-asserted-by": "crossref",
"key": "3882",
"unstructured": "Jain A, Chaurasia R, Sengar NS, Singh M, Mahor S, Narain S. Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers. Scientific reports. 2020 Nov 19;10(1):1-8. DOI: https://doi.org/10.1038/s41598-020-77093-z PMid:33214648 PMCid:PMC7677378"
},
{
"DOI": "10.1093/jn/nxaa332",
"doi-asserted-by": "crossref",
"key": "3883",
"unstructured": "Luo X, Liao Q, Shen Y, Li H, Cheng L. Vitamin D deficiency is associated with COVID-19 incidence and disease severity in Chinese people. The Journal of nutrition. 2021 Jan;151(1):98-103. DOI: https://doi.org/10.1093/jn/nxaa332 PMid:33188401 PMCid:PMC7890671"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "crossref",
"key": "3884",
"unstructured": "Radujkovic A, Hippchen T, Tiwari-Heckler S, et al. Vitamin D deficiency and outcome of COVID-19 patients. Nutrients. 2020 Sep 10;12(9):2757. DOI: https://doi.org/10.3390/nu12092757 PMid:32927735 PMCid:PMC7551780"
},
{
"DOI": "10.1080/07315724.2020.1826005",
"doi-asserted-by": "crossref",
"key": "3885",
"unstructured": "Ye K, Tang F, Liao X, et al. Does serum vitamin D level affect COVID-19 infection and its severity? -A case-control study. Journal of the American College of Nutrition. 2021 Nov 10;40(8):724-31. DOI: https://doi.org/10.1080/07315724.2020.1826005 PMid:33048028"
},
{
"DOI": "10.1093/ajcp/aqaa252",
"doi-asserted-by": "crossref",
"key": "3886",
"unstructured": "De Smet D, De Smet K, Herroelen P, Gryspeerdt S, Martens GA. Serum 25 (OH) D level on hospital admission associated with COVID-19 stage and mortality. American journal of clinical pathology. 2021 Mar;155(3):381-8. DOI: https://doi.org/10.1093/ajcp/aqaa252 PMid:33236114 PMCid:PMC7717135"
},
{
"DOI": "10.1007/s00330-020-07033-y",
"doi-asserted-by": "crossref",
"key": "3887",
"unstructured": "Francone M, Iafrate F, Masci GM, et al. Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. European radiology. 2020 Dec;30(12):6808-17. DOI: https://doi.org/10.1007/s00330-020-07033-y PMid:32623505 PMCid:PMC7334627"
},
{
"DOI": "10.1016/j.clnu.2020.10.055",
"doi-asserted-by": "crossref",
"key": "3888",
"unstructured": "Cereda E, Bogliolo L, Klersy C, et al. Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital. Clinical nutrition. 2021 Apr 1;40(4):2469-72. DOI: https://doi.org/10.1016/j.clnu.2020.10.055 PMid:33187772 PMCid:PMC7605851"
},
{
"DOI": "10.1177/00368504211036854",
"doi-asserted-by": "crossref",
"key": "3889",
"unstructured": "Teama MA, Abdelhakam DA, Elmohamadi MA, Badr FM. Vitamin D deficiency as a predictor of severity in patients with COVID-19 infection. Science Progress. 2021 Aug;104(3):00368504211036854. DOI: https://doi.org/10.1177/00368504211036854 PMid:34347528 PMCid:PMC10450705"
},
{
"DOI": "10.14740/jocmr4240",
"doi-asserted-by": "crossref",
"key": "3890",
"unstructured": "Chan AS, Rout A. Use of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in COVID-19. Journal of clinical medicine research. 2020 Jul;12(7):448. DOI: https://doi.org/10.14740/jocmr4240 PMid:32655740 PMCid:PMC7331861"
},
{
"DOI": "10.1016/j.kint.2020.03.005",
"doi-asserted-by": "crossref",
"key": "3891",
"unstructured": "Cheng Y, Luo R, Wang K, et al. Kidney impairment is associated with in-hospital death of COVID-19 patients. MedRxiv. 2020 Jan 1. DOI: https://doi.org/10.1101/2020.02.18.20023242"
},
{
"DOI": "10.1002/jcla.23412",
"doi-asserted-by": "crossref",
"key": "3892",
"unstructured": "Wang Y, Shi L, Wang Y, Duan G, Yang H. Albumin and total bilirubin for severity and mortality in coronavirus disease 2019 patients. Journal of Clinical Laboratory Analysis. 2020 Jul;34(7). DOI: https://doi.org/10.1002/jcla.23412 PMid:32745325 PMCid:PMC7323086"
},
{
"DOI": "10.1186/s40560-020-00466-z",
"doi-asserted-by": "crossref",
"key": "3893",
"unstructured": "Yao Y, Cao J, Wang Q, Shi Q, Liu K, Luo Z, Chen X, Chen S, Yu K, Huang Z, Hu B. D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: a case control study. Journal of intensive care. 2020 Dec;8(1):1-1. DOI: https://doi.org/10.1186/s40560-020-00466-z PMid:32665858 PMCid:PMC7348129"
},
{
"DOI": "10.1016/j.jinf.2020.06.053",
"doi-asserted-by": "crossref",
"key": "3894",
"unstructured": "Lin Z, Long F, Yang Y, Chen X, Xu L, Yang M. Serum ferritin as an independent risk factor for severity in COVID-19 patients. Journal of infection. 2020 Oct 1;81(4):647-79. DOI: https://doi.org/10.1016/j.jinf.2020.06.053 PMid:32592705 PMCid:PMC7313486"
},
{
"DOI": "10.18632/aging.103770",
"doi-asserted-by": "crossref",
"key": "3895",
"unstructured": "Li C, Ye J, Chen Q, et al. Elevated Lactate Dehydrogenase (LDH) level as an independent risk factor for the severity and mortality of COVID-19. Aging (Albany NY). 2020 Aug 8;12(15):15670. DOI: https://doi.org/10.18632/aging.103770 PMid:32805722 PMCid:PMC7467395"
},
{
"DOI": "10.1016/j.clnu.2020.10.055",
"doi-asserted-by": "crossref",
"key": "3896",
"unstructured": "a tertiary referral hospital. Clinical nutrition. 2021 Apr 1;40(4):2469-72. DOI: https://doi.org/10.1016/j.clnu.2020.10.055 PMid:33187772 PMCid:PMC7605851"
},
{
"DOI": "10.1177/00368504211036854",
"doi-asserted-by": "crossref",
"key": "3897",
"unstructured": "Teama MA, Abdelhakam DA, Elmohamadi MA, Badr FM. Vitamin D deficiency as a predictor of severity in patients with COVID-19 infection. Science Progress. 2021 Aug;104(3):00368504211036854. DOI: https://doi.org/10.1177/00368504211036854 PMid:34347528 PMCid:PMC10450705"
},
{
"DOI": "10.14740/jocmr4240",
"doi-asserted-by": "crossref",
"key": "3898",
"unstructured": "Chan AS, Rout A. Use of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in COVID-19. Journal of clinical medicine research. 2020 Jul;12(7):448. DOI: https://doi.org/10.14740/jocmr4240 PMid:32655740 PMCid:PMC7331861"
},
{
"DOI": "10.1016/j.kint.2020.03.005",
"doi-asserted-by": "crossref",
"key": "3899",
"unstructured": "Cheng Y, Luo R, Wang K, et al. Kidney impairment is associated with in-hospital death of COVID-19 patients. MedRxiv. 2020 Jan 1. DOI: https://doi.org/10.1101/2020.02.18.20023242"
},
{
"DOI": "10.1002/jcla.23412",
"doi-asserted-by": "crossref",
"key": "3900",
"unstructured": "Wang Y, Shi L, Wang Y, Duan G, Yang H. Albumin and total bilirubin for severity and mortality in coronavirus disease 2019 patients. Journal of Clinical Laboratory Analysis. 2020 Jul;34(7). DOI: https://doi.org/10.1002/jcla.23412 PMid:32745325 PMCid:PMC7323086"
},
{
"DOI": "10.1186/s40560-020-00466-z",
"doi-asserted-by": "crossref",
"key": "3901",
"unstructured": "Yao Y, Cao J, Wang Q, Shi Q, Liu K, Luo Z, Chen X, Chen S, Yu K, Huang Z, Hu B. D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: a case control study. Journal of intensive care. 2020 Dec;8(1):1-1. DOI: https://doi.org/10.1186/s40560-020-00466-z PMid:32665858 PMCid:PMC7348129"
},
{
"DOI": "10.1016/j.jinf.2020.06.053",
"doi-asserted-by": "crossref",
"key": "3902",
"unstructured": "Lin Z, Long F, Yang Y, Chen X, Xu L, Yang M. Serum ferritin as an independent risk factor for severity in COVID-19 patients. Journal of infection. 2020 Oct 1;81(4):647-79. DOI: https://doi.org/10.1016/j.jinf.2020.06.053 PMid:32592705 PMCid:PMC7313486"
},
{
"DOI": "10.18632/aging.103770",
"doi-asserted-by": "crossref",
"key": "3903",
"unstructured": "Li C, Ye J, Chen Q, et al. Elevated Lactate Dehydrogenase (LDH) level as an independent risk factor for the severity and mortality of COVID-19. Aging (Albany NY). 2020 Aug 8;12(15):15670. DOI: https://doi.org/10.18632/aging.103770 PMid:32805722 PMCid:PMC7467395"
}
],
"reference-count": 29,
"references-count": 29,
"relation": {},
"resource": {
"primary": {
"URL": "https://njmr.in/index.php/file/article/view/1070"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "A Study on Serum Vitamin D3 Level in Patients with Covid-19: A Cross-Sectional Study in Kolkata",
"type": "journal-article",
"volume": "15"
}
